Peritonitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Peritonitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
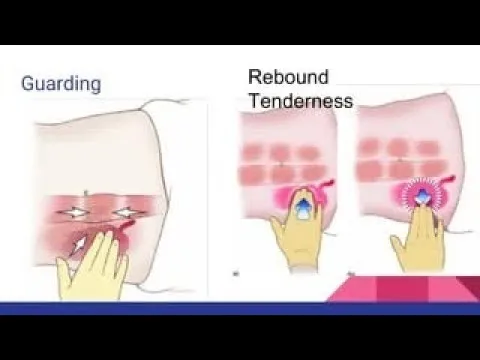
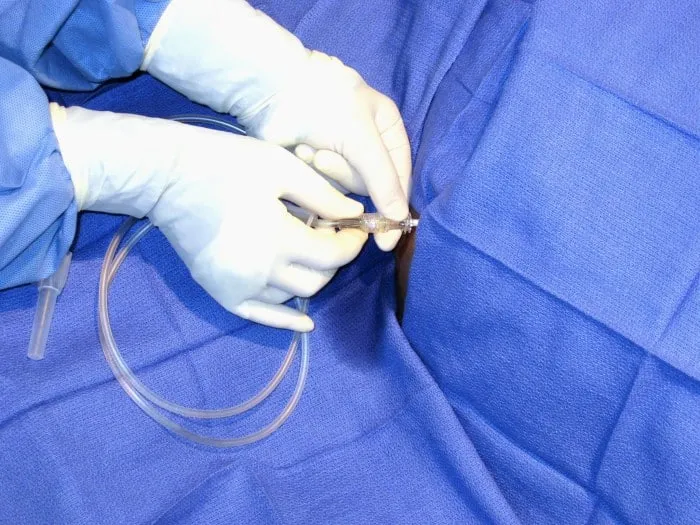
Peritonitis US Medical PG Question 1: A 40-year-old man presents with acute abdominal pain. Past medical history is significant for hepatitis C, complicated by multiple recent visits with associated ascites. His temperature is 38.3°C (100.9°F), heart rate is 115/min, blood pressure is 88/48 mm Hg, and respiratory rate is 16/min. On physical examination, the patient is alert and in moderate discomfort. Cardiopulmonary examination is unremarkable. Abdominal examination reveals distant bowel sounds on auscultation. There is also mild diffuse abdominal tenderness to palpation with guarding present. The remainder of the physical examination is unremarkable. A paracentesis is performed. Laboratory results are significant for the following:
Leukocyte count 11,630/µL (with 94% neutrophils)
Platelets 24,000/µL
Hematocrit 29%
Ascitic fluid analysis:
Cell count 658 PMNs/µL
Total protein 1.2 g/dL
Glucose 24 mg/dL
Gram stain Gram-negative rods
Culture Culture yields growth of E. coli
Which of the following is the next, best step in the management of this patient?
- A. Serum lipase level
- B. Abdominal radiography and contrast CT of the abdomen
- C. Intravenous fluid resuscitation
- D. Intravenous cefotaxime (Correct Answer)
- E. Surgical consultation
Peritonitis Explanation: ***Intravenous cefotaxime***
- The patient's presentation with **fever**, **hypotension**, and **abdominal pain** in the context of **cirrhosis with ascites**, coupled with ascitic fluid analysis showing a **high PMN count (>250/µL)** and **positive E. coli culture**, is highly indicative of **spontaneous bacterial peritonitis (SBP)**.
- **Empiric intravenous antibiotics** like cefotaxime, a third-generation cephalosporin, are the cornerstone of SBP treatment due to its broad-spectrum coverage against common enteric bacteria.
- In septic patients with SBP, antibiotics represent the **definitive treatment** that addresses the source of infection.
*Serum lipase level*
- While **abdominal pain** is present, the overall clinical picture, particularly the **ascitic fluid analysis** and positive culture, points away from pancreatitis as the primary diagnosis.
- A serum lipase level would be more relevant in evaluating suspected **pancreatitis**, which is less likely given the specific findings of SBP.
*Abdominal radiography and contrast CT of the abdomen*
- Although imaging can be useful in evaluating abdominal pain, the **paracentesis results** already provide a definitive diagnosis of SBP, making immediate imaging unnecessary for initial management.
- Furthermore, **contrast CT** in a hypotensive patient with potentially compromised renal function from cirrhosis should be approached with caution.
*Intravenous fluid resuscitation*
- The patient is **hypotensive and tachycardic**, indicating **sepsis** associated with SBP, which does require **fluid resuscitation** as part of comprehensive sepsis management.
- However, when selecting the **"next best step"**, **antibiotics** take priority as they address the underlying infection that is the source of sepsis, while fluids are supportive care that would be administered concurrently.
- Without treating the infection, fluid resuscitation alone would not resolve the patient's condition.
*Surgical consultation*
- SBP is a **medical emergency** primarily managed with **antibiotics**, not surgery.
- Surgical intervention is typically reserved for cases of **secondary peritonitis** (e.g., perforated viscus), which would show different ascitic fluid characteristics (e.g., higher protein, glucose, multiple organisms).
Peritonitis US Medical PG Question 2: A 49-year-old woman with a history of hepatitis C cirrhosis complicated by esophageal varices, ascites, and hepatic encephalopathy presents with 1 week of increasing abdominal discomfort. Currently, she takes lactulose, rifaximin, furosemide, and spironolactone. On physical examination, she has mild asterixis, generalized jaundice, and a distended abdomen with positive fluid wave. Diagnostic paracentesis yields a WBC count of 1196/uL with 85% neutrophils. Which of the following is the most appropriate treatment?
- A. Cefotaxime (Correct Answer)
- B. Transjugular intrahepatic portosystemic shunt placement
- C. Large volume paracentesis with albumin
- D. Increased furosemide and spironolactone
- E. Metronidazole
Peritonitis Explanation: ***Cefotaxime***
- The patient presents with classic signs of **spontaneous bacterial peritonitis (SBP)**: increasing abdominal discomfort in a cirrhotic patient with ascites, and a diagnostic paracentesis showing **ascitic fluid neutrophil count >250 cells/mm³** (1196 × 0.85 = 1016 neutrophils/μL).
- **Third-generation cephalosporins** like cefotaxime or ceftriaxone are the **first-line treatment** for SBP due to their broad-spectrum coverage against common enteric gram-negative bacteria (especially E. coli and Klebsiella).
- Treatment should be initiated promptly once SBP is diagnosed to reduce mortality.
*Transjugular intrahepatic portosystemic shunt placement*
- TIPS is primarily used for **refractory ascites** or **recurrent variceal bleeding** that is not responsive to medical management.
- It is **not indicated** for the acute treatment of SBP and would be inappropriate in the setting of active infection.
*Large volume paracentesis with albumin*
- Large volume paracentesis is used to relieve symptoms of **tense ascites** causing respiratory compromise or severe discomfort, not as a primary treatment for SBP.
- While albumin is often given with large volume paracentesis (>5L removed) to prevent post-paracentesis circulatory dysfunction, it does not treat the underlying bacterial infection.
*Increased furosemide and spironolactone*
- Diuretics like furosemide and spironolactone are used to manage **chronic ascites** by promoting fluid excretion.
- Increasing their dose will not address the active bacterial infection causing SBP and may worsen renal function in an acutely ill patient.
*Metronidazole*
- Metronidazole is primarily effective against **anaerobic bacteria** and some protozoa.
- While it might be considered in specific polymicrobial intra-abdominal infections, it is **not sufficient as monotherapy** for SBP, which commonly involves gram-negative aerobic bacteria like E. coli and Klebsiella species.
Peritonitis US Medical PG Question 3: A 15-year-old boy presents with his father to the urgent care with 5 days of frequent diarrhea, occasionally with streaks of blood mixed in. Stool cultures are pending, but preliminary stool samples demonstrate fecal leukocytes and erythrocytes. His vital signs are as follows: blood pressure is 126/83 mm Hg, heart rate is 97/min, and respiratory rate is 15/min. He is started on outpatient therapy for presumed Shigella infection. Which of the following is the most appropriate therapy?
- A. Oral doxycycline
- B. Oral vancomycin
- C. Oral TMP-SMX
- D. Oral azithromycin (Correct Answer)
- E. Oral ciprofloxacin
Peritonitis Explanation: ***Oral azithromycin***
- **Azithromycin** is the **first-line empiric treatment** for suspected **Shigella infection** based on current CDC and WHO guidelines, particularly in pediatric and adolescent patients.
- The presence of **fecal leukocytes and erythrocytes** indicates an invasive bacterial infection, which warrants antibiotic therapy to shorten the course of illness and reduce transmission risks.
- Azithromycin has excellent efficacy against Shigella with relatively low resistance rates compared to older agents, and it is well-tolerated in adolescents.
*Oral TMP-SMX*
- **TMP-SMX (trimethoprim-sulfamethoxazole)** was historically first-line for Shigella, but **widespread resistance** (often >50% globally) has made it no longer recommended for empiric therapy.
- It may still be used if culture and susceptibility testing confirm sensitivity, but should not be chosen empirically.
*Oral ciprofloxacin*
- **Ciprofloxacin**, a fluoroquinolone, is highly effective against **Shigella** and is first-line in adults.
- However, its use in **pediatric patients under 18 years** is generally limited due to potential adverse effects on **cartilage development** and risk of tendinopathy.
- In a 15-year-old, while approaching adult age, azithromycin remains preferred unless there are specific contraindications.
*Oral doxycycline*
- **Doxycycline** has limited activity against **Shigella** and is not considered appropriate empiric therapy for this infection.
- It is more commonly used for atypical pathogens, certain sexually transmitted infections, or specific tick-borne diseases.
*Oral vancomycin*
- **Oral vancomycin** is primarily used to treat **Clostridioides difficile infection** (CDI) and is completely ineffective against **Shigella**.
- Vancomycin acts only on gram-positive bacteria and does not penetrate the systemic circulation when given orally, making it unsuitable for gram-negative enteric infections.
Peritonitis US Medical PG Question 4: A 58-year-old man with liver cirrhosis presents to his primary care physician complaining of increased abdominal girth and early satiety. He drinks 2–4 glasses of wine with dinner and recalls having had abnormal liver enzymes in the past. Vital signs include a temperature of 37.1°C (98.7°F), blood pressure of 110/70 mm Hg, and a pulse of 75/min. Physical examination reveals telangiectasias, mild splenomegaly, palpable firm liver, and shifting dullness. Liver function is shown:
Total bilirubin 3 mg/dL
Aspartate aminotransferase (AST) 150 U/L
Alanine aminotransferase (ALT) 70 U/L
Total albumin 2.5 g/dL
Abdominal ultrasonography confirms the presence of ascites. Diagnostic paracentesis is performed and its results are shown:
Polymorphonuclear cell count 10 cells/mm
Ascitic protein 1 g/dL
Which of the following best represents the mechanism of ascites in this patient?
- A. Peritoneal tuberculosis
- B. High sinusoidal pressure (Correct Answer)
- C. Pancreatic disease
- D. Serositis
- E. Peritoneal carcinomatosis
Peritonitis Explanation: ***High sinusoidal pressure***
- In **liver cirrhosis**, the fibrotic changes and regenerating nodules increase resistance to blood flow, leading to **portal hypertension** and increased pressure in the hepatic sinusoids.
- This elevated pressure drives fluid from the sinusoids into the abdominal cavity, forming **ascites**.
*Peritoneal tuberculosis*
- This condition typically presents with **ascitic fluid protein levels above 2.5 g/dL** and a significantly elevated **lymphocytic cell count** in the ascitic fluid.
- The patient's ascitic protein level is 1 g/dL, and the polymorphonuclear cell count is low, making this diagnosis less likely.
*Pancreatic disease*
- Pancreatic ascites results from a leaking **pancreatic duct or pseudocyst**, leading to ascitic fluid with very high **amylase levels** and often a high protein content.
- While the patient has alcohol use, the clinical presentation and paracentesis results point more strongly towards liver-related ascites rather than pancreatic.
*Serositis*
- **Serositis** involves inflammation of serous membranes, often seen in autoimmune diseases, and can cause ascites with a higher protein content and inflammatory cells.
- The patient's primary symptoms and signs are consistent with advanced liver disease, not systemic inflammatory serositis.
*Peritoneal carcinomatosis*
- **Peritoneal carcinomatosis** usually leads to ascites with a **high protein content** (>2.5 g/dL), sometimes with **malignant cells** present in the ascitic fluid cytology.
- The low ascitic fluid protein and absence of other signs of malignancy make this an unlikely cause.
Peritonitis US Medical PG Question 5: A 56-year-old male with a history of hepatitis C cirrhosis status post TIPS procedure is brought in by his wife to the emergency department because he has been acting disoriented, slurring his speech, and sleeping throughout the day. On arrival the patient is afebrile and his vital signs are pulse is 87/min, blood pressure is 137/93 mmHg, and respirations are 12/min with shallow breaths. Examination reveals a jaundiced male who appears older than stated age. Abdominal exam is positive for a fluid wave and shifting dullness to percussion. You note enlarged breasts, decreased facial hair, 3+ patellar reflexes bilaterally, and the following in the upper extremity (Image A). Paracentesis reveals ascitic fluid with neutrophil counts of < 100 cells/mcL. Serum creatinine is 1.0 and BUN is 15. Which of the following is the next best step in management?
- A. Administer neomycin and glucose
- B. IV albumin and antibiotic therapy with cefotaxime
- C. Administer rifaximin and glucose
- D. Administer lactulose (Correct Answer)
- E. Liver transplantation
Peritonitis Explanation: ***Administer lactulose***
- The patient exhibits classic symptoms of **hepatic encephalopathy** (disorientation, slurred speech, somnolence, asterixis as demonstrated by Image A), combined with findings consistent with **cirrhosis** (jaundice, ascites, gynecomastia, decreased facial hair, history of hepatitis C and TIPS).
- **Lactulose** is the first-line treatment for hepatic encephalopathy as it acidifies the colon, promoting the conversion of ammonia (a neurotoxin) to ammonium, which is then trapped and excreted in the feces.
*Administer neomycin and glucose*
- **Neomycin** is an antibiotic that can reduce ammonia-producing bacteria in the gut but is generally considered a second-line agent due to potential side effects like **ototoxicity** and **nephrotoxicity**.
- **Glucose** administration is not a primary treatment for hepatic encephalopathy; it would only be indicated if the patient were hypoglycemic, which is not suggested by the clinical picture.
*IV albumin and antibiotic therapy with cefotaxime*
- **IV albumin** is primarily used in **spontaneous bacterial peritonitis (SBP)** to prevent hepatorenal syndrome, and the paracentesis finding of < 100 cells/mcL neutrophils suggests SBP is unlikely.
- **Cefotaxime** is an appropriate antibiotic for **SBP**, but the patient's presentation is more consistent with hepatic encephalopathy, not an active infection.
*Administer rifaximin and glucose*
- **Rifaximin** is a non-absorbable antibiotic used to reduce ammonia-producing bacteria in the gut, often as an add-on or alternative to lactulose for maintenance therapy or in cases unresponsive to lactulose alone. It is not generally the initial monotherapy for an acute, severe encephalopathy episode.
- As mentioned, **glucose** is not a primary treatment for hepatic encephalopathy.
*Liver transplantation*
- **Liver transplantation** is a definitive treatment for end-stage liver disease, but it is not the **next best step** for acute management of hepatic encephalopathy.
- The immediate priority is to address the acute encephalopathy episode pharmacologically before considering long-term solutions like transplantation, which has a complex workup and waiting list.
Peritonitis US Medical PG Question 6: A 52-year-old man, with a history of alcoholism, presents with loss of appetite, abdominal pain, and fever for the past 24 hours. He says he consumed 12 beers and a bottle of vodka 2 days ago. He reports a 19-year history of alcoholism. His blood pressure is 100/70 mm Hg, pulse is 100/min, respirations are 20/min, and oxygen saturation is 99% on room air. Laboratory findings are significant for the following:
Sodium 137 mEq/L
Potassium 3.4 mEq/L
Alanine aminotransferase (ALT) 230 U/L
Aspartate aminotransferase (AST) 470 U/L
Which of the following histopathologic findings would most likely be found on a liver biopsy of this patient?
- A. Macronodular cirrhosis
- B. T-lymphocyte infiltration
- C. Periportal necrosis
- D. Cytoplasmic inclusion bodies with keratin (Correct Answer)
- E. Positive periodic acid-Schiff stain
Peritonitis Explanation: ***Cytoplasmic inclusion bodies with keratin***
- The patient's history of **heavy alcohol consumption**, acute presentation with fever, abdominal pain, and elevated **AST and ALT (AST:ALT ratio >2:1)**, are highly suggestive of **alcoholic hepatitis**.
- **Mallory bodies**, which are **cytoplasmic inclusions consisting of intermediate filaments (keratin)**, are a characteristic histopathologic finding in alcoholic hepatitis.
*Macronodular cirrhosis*
- While **alcoholic liver disease** can progress to cirrhosis, the acute presentation with fever and significant transaminase elevation points more towards **alcoholic hepatitis** rather than established macronodular cirrhosis as the primary acute event.
- **Macronodular cirrhosis** typically involves larger nodules of regenerating hepatocytes, but the *acute inflammatory changes* of alcoholic hepatitis are paramount in this presentation.
*T-lymphocyte infiltration*
- While some inflammatory cells are present in alcoholic hepatitis, **T-lymphocyte infiltration** is more characteristic of **chronic viral hepatitis** or **autoimmune hepatitis**.
- The liver injury in alcoholic hepatitis is primarily mediated by neutrophils and direct hepatotoxic effects of alcohol metabolites.
*Periportal necrosis*
- **Periportal necrosis** is more commonly seen in **viral hepatitis** or other forms of **acute hepatitis** where the inflammatory process is concentrated around the portal tracts.
- In alcoholic hepatitis, the damage is typically *centrilobular (zone 3)*, around the terminal hepatic venule, due to its hypoxic vulnerability and high cytochrome P450 activity.
*Positive periodic acid-Schiff stain*
- A **positive periodic acid-Schiff (PAS) stain** that is *diastase-resistant* is a characteristic finding in **alpha-1 antitrypsin deficiency**, a genetic disorder affecting the liver and lungs.
- This patient's clinical presentation and lab findings are inconsistent with alpha-1 antitrypsin deficiency and strongly point towards **alcoholic liver disease**.
Peritonitis US Medical PG Question 7: A 25-year-old woman presents to her primary care physician complaining of several months of diarrhea. She has also had crampy abdominal pain. She has tried modifying her diet without improvement. She has many watery, non-bloody bowel movements per day. She also reports feeling fatigued. The patient has not recently traveled outside of the country. She has lost 10 pounds since her visit last year, and her BMI is now 20. On exam, she has skin tags and an anal fissure. Which of the following would most likely be seen on endoscopy and biopsy?
- A. Diffuse, non-focal ulcerations with granuloma
- B. Diffuse, non-focal ulcerations without granuloma
- C. Focal ulcerations with granuloma (Correct Answer)
- D. Pseudopolyps and continuous mucosal involvement
- E. Friable mucosa with pinpoint hemorrhages
Peritonitis Explanation: ***Focal ulcerations with granuloma***
- The patient's symptoms (diarrhea, crampy abdominal pain, fatigue, weight loss, skin tags, and anal fissure) are highly suggestive of **Crohn's disease**.
- **Crohn's disease** is characterized by **transmural inflammation** that often presents as **focal ulcerations** (skip lesions) and **non-caseating granulomas** on biopsy.
*Diffuse, non-focal ulcerations with granuloma*
- While granulomas are characteristic of Crohn's disease, the inflammation in Crohn's disease is typically **focal and discontinuous** (skip lesions), not diffuse.
- Diffuse inflammation with granulomas is less typical for inflammatory bowel disease and might prompt consideration for other granulomatous diseases not fitting this clinical picture.
*Diffuse, non-focal ulcerations without granuloma*
- **Diffuse ulcerations without granulomas** would be more suggestive of **ulcerative colitis**, but the presence of **skin tags** and **anal fissure** points away from this diagnosis and towards Crohn's disease.
- Ulcerative colitis is also characterized by **continuous inflammation** starting from the rectum, which is not described as focal.
*Pseudopolyps and continuous mucosal involvement*
- **Pseudopolyps** and **continuous mucosal involvement** are classic features of **ulcerative colitis**, not Crohn's disease.
- The patient's extraintestinal manifestations like **skin tags** and **anal fissure** are much more common in Crohn's disease.
*Friable mucosa with pinpoint hemorrhages*
- **Friable mucosa** and **pinpoint hemorrhages** are characteristic findings in **ulcerative colitis**, specifically indicating active inflammation and mucosal fragility.
- While these can be seen in inflammatory bowel disease, the full clinical picture with associated perianal disease is more specific for Crohn's disease.
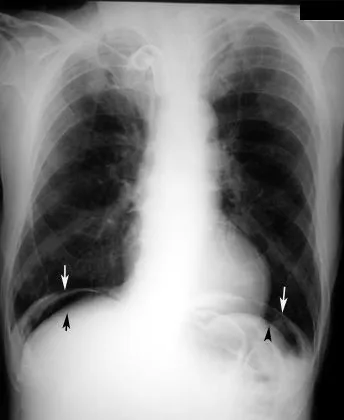
Peritonitis US Medical PG Question 8: A 65-year-old man is brought to the emergency department because of a 1-day history of fever and disorientation. His wife reports that he had abdominal pain and diarrhea the previous day. He drinks 60 oz of alcohol weekly. His pulse is 110/min and blood pressure is 96/58 mm Hg. Examination shows jaundice, palmar erythema, spider nevi on his chest, dilated veins on the anterior abdominal wall, and 2+ edema of the lower extremities. The abdomen is soft and diffusely tender; there is shifting dullness to percussion. His albumin is 1.4 g/dL, bilirubin is 5 mg/dL, and prothrombin time is 31 seconds (INR = 3.3). Hepatitis serology is negative. A CT scan of the abdomen is shown. Which of the following processes is the most likely explanation for these findings?
- A. Accumulation of iron in hepatocytes
- B. Ground-glass hepatocytes with cytotoxic T cells
- C. Fibrous bands surrounding regenerating hepatocytes (Correct Answer)
- D. Misfolded protein aggregates in hepatocellular endoplasmic reticulum
- E. Hepatocyte swelling with Councilman bodies and monocyte infiltration
Peritonitis Explanation: ***Fibrous bands surrounding regenerating hepatocytes***
- The patient presents with classic signs of **cirrhosis** (jaundice, palmar erythema, spider nevi, dilated abdominal veins, edema, ascites), acute decompensation (fever, disorientation, hypotension), and severe **hepatic dysfunction** (low albumin, high bilirubin, prolonged PT/INR). The history of heavy alcohol use supports this.
- **Cirrhosis** is histologically characterized by diffuse **fibrosis** and the formation of **regenerative nodules**, which are hepatocytes surrounded by fibrous bands, leading to disruption of normal liver architecture and function.
*Accumulation of iron in hepatocytes*
- This is characteristic of **hereditary hemochromatosis**, which leads to **iron overload** and organ damage, including cirrhosis.
- While hemochromatosis can cause cirrhosis, the patient's acute symptoms and specific liver histology (macronodular cirrhosis often seen in alcoholic liver disease) make alcoholic cirrhosis a more direct fit, and there is no mention of increased iron in labs.
*Ground-glass hepatocytes with cytotoxic T cells*
- **Ground-glass hepatocytes** are typically seen in **chronic hepatitis B infection**, representing an accumulation of HBsAg in the endoplasmic reticulum.
- While chronic hepatitis B can lead to cirrhosis, the negative hepatitis serology and direct evidence of alcohol abuse do not support this as the primary cause.
*Misfolded protein aggregates in hepatocellular endoplasmic reticulum*
- This description is characteristic of **alpha-1 antitrypsin deficiency**, where defective alpha-1 antitrypsin accumulates in hepatocytes.
- Although it can cause cirrhosis, the patient's symptoms are more consistent with alcoholic liver disease, and there is no mention of respiratory symptoms often associated with alpha-1 antitrypsin deficiency.
*Hepatocyte swelling with Councilman bodies and monocyte infiltration*
- **Hepatocyte swelling** and **Councilman bodies** (apoptotic hepatocytes) are features of **acute viral hepatitis** or other forms of acute liver injury. Monocyte infiltration can also occur.
- While acute liver injury can occur, the chronic stigmata of liver disease (spider nevi, palmar erythema, ascites) and the history of alcohol abuse point to a chronic process like cirrhosis rather than just acute inflammation.
Peritonitis US Medical PG Question 9: An esophageal biopsy sample from a 47-year-old male with chronic heartburn reveals intestinal metaplasia. Which of the following abnormal cell types is likely present in this patient's esophagus?
- A. Polymorphonuclear leukocytes
- B. Keratinized stratified squamous epithelium
- C. Pseudostratified ciliated columnar epithelium
- D. Goblet cells (Correct Answer)
- E. Simple cuboidal epithelium
Peritonitis Explanation: ***Goblet cells***
- The presence of **goblet cells** is the histological hallmark of **intestinal metaplasia** in the esophagus, specifically **Barrett's esophagus**.
- **Chronic acid reflux** causes the normal stratified squamous epithelium to be replaced by columnar epithelium containing goblet cells, similar to the intestinal lining.
*Polymorphonuclear leukocytes*
- These cells, primarily **neutrophils**, are typically associated with **acute inflammation** or **infection**.
- While they can be present in inflammatory conditions of the esophagus, they are not the specific abnormal cell type indicative of intestinal metaplasia.
*Keratinized stratified squamous epithelium*
- This type of epithelium is characteristic of the **skin** and oral cavity, providing protection against abrasion and desiccation.
- The normal esophagus is lined by **non-keratinized stratified squamous epithelium**, and its keratinization in the esophagus would be an abnormal finding but not indicative of intestinal metaplasia.
*Pseudostratified ciliated columnar epithelium*
- This type of epithelium is typically found in the **trachea** and bronchi, specialized for mucus secretion and particulate removal.
- Its presence in the esophagus would be an abnormal finding, but it is not the specific cell type associated with intestinal metaplasia (Barrett's esophagus).
*Simple cuboidal epithelium*
- This type of epithelium is commonly found in glands, kidney tubules, and ducts, specialized for secretion and absorption.
- It is not typically found as a lining epithelium in the esophagus under normal or metaplastic conditions.
Peritonitis US Medical PG Question 10: A 21-year-old man comes to the physician because of a 6-month history of severe abdominal pain, bloating, and episodic diarrhea. He has also had a 5-kg (11-lb) weight loss during this time. Physical examination shows a mildly distended abdomen, hyperactive bowel sounds, and diffuse abdominal tenderness. A biopsy specimen of the colonic mucosa shows scattered areas of inflammation with fibrosis and noncaseating granulomas. Which of the following is most likely involved in the pathogenesis of this patient's condition?
- A. Increased activity of type 1 T helper cells (Correct Answer)
- B. Viral infection with intranuclear inclusions
- C. Intestinal overgrowth of toxigenic bacteria
- D. Accumulation of intracellular bacteria in macrophages
- E. Ectopic secretion of serotonin
Peritonitis Explanation: ***Increased activity of type 1 T helper cells***
- The described clinical picture (abdominal pain, bloating, diarrhea, weight loss, and **noncaseating granulomas**) is classic for **Crohn's disease**.
- Crohn's disease is characterized by a **Th1-mediated immune response**, involving immune cells like **type 1 T helper cells** that produce pro-inflammatory cytokines such as **TNF-α** and **interferon-γ**.
*Viral infection with intranuclear inclusions*
- **Intranuclear inclusions** are characteristic features of certain viral infections, such as those caused by **cytomegalovirus (CMV)**, which can present with colitis.
- However, CMV colitis typically lacks **noncaseating granulomas** and the chronic, progressive nature associated with this patient's symptoms.
*Intestinal overgrowth of toxigenic bacteria*
- While **toxigenic bacteria** (e.g., *Clostridium difficile*) can cause severe colitis and diarrhea, their primary mechanism involves toxin production, leading to mucosal damage.
- This scenario would not typically present with **noncaseating granulomas** and chronic, diffuse inflammation characteristic of Crohn's disease.
*Accumulation of intracellular bacteria in macrophages*
- This mechanism is associated with conditions like **Mycobacterium avium complex (MAC) infection** or **Whipple's disease**, which involve foamy macrophages containing bacteria.
- However, these conditions do not typically present with the prominent **noncaseating granulomas** seen in Crohn's disease.
*Ectopic secretion of serotonin*
- **Ectopic serotonin secretion** is characteristic of **carcinoid syndrome**, often associated with neuroendocrine tumors.
- Symptoms typically include flushing, diarrhea, and bronchospasm, which are distinct from the abdominal pain, weight loss, and granulomatous inflammation described in this patient.
More Peritonitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.