Malabsorption syndromes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Malabsorption syndromes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Malabsorption syndromes US Medical PG Question 1: A 35-year-old Caucasian female presents with anemia, malaise, bloating, and diarrhea. Past genetic testing revealed that this patient carries the HLA-DQ2 allele. The physician suspects that the patient's presentation is dietary in cause. Which of the following findings would definitively confirm this diagnosis?
- A. CT scan showing inflammation of the small bowel wall
- B. Biopsy of the duodenum showing atrophy and blunting of villi (Correct Answer)
- C. Biopsy of the colon showing epithelial cell apoptosis
- D. Esophageal endoscopy showing lower esophageal metaplasia
- E. Liver biopsy showing apoptosis of hepatocytes
Malabsorption syndromes Explanation: ***Biopsy of the duodenum showing atrophy and blunting of villi***
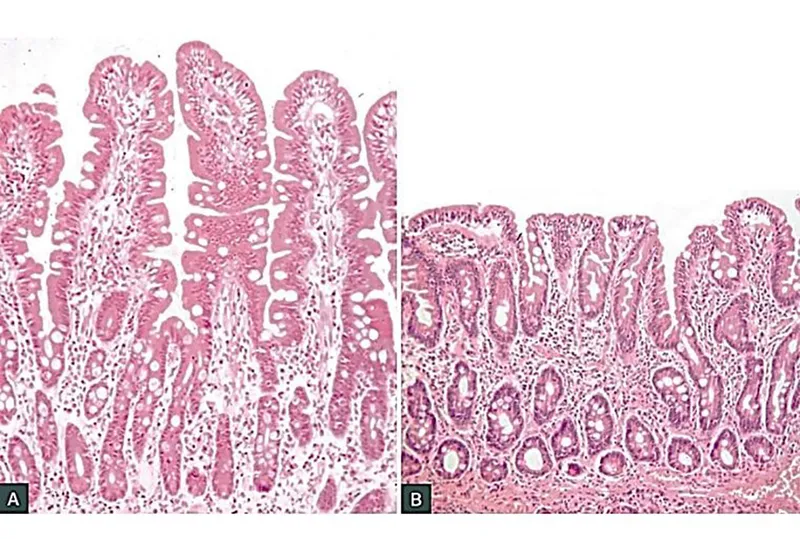
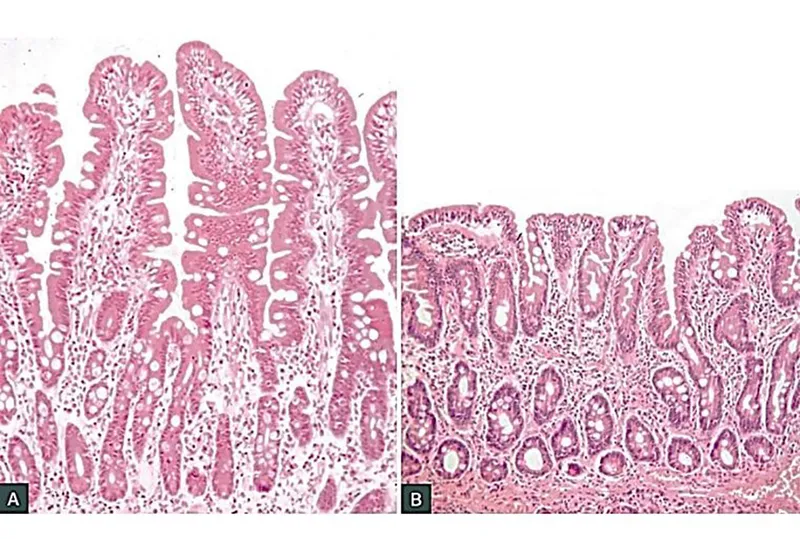
- This finding is the **gold standard** for diagnosing **celiac disease**, which aligns with the patient's symptoms (anemia, malaise, bloating, diarrhea), genetic predisposition (HLA-DQ2 allele), and suspected dietary cause.
- The characteristic **villous atrophy** and **crypt hyperplasia** seen in duodenal biopsies are hallmark pathological changes in celiac disease due to gluten exposure.
*CT scan showing inflammation of the small bowel wall*
- While a CT scan can show **inflammation**, it is not specific enough to definitively diagnose celiac disease, as many other conditions can cause small bowel inflammation.
- It does not provide the **histopathological detail** necessary to confirm villous atrophy, which is key for celiac diagnosis.
*Biopsy of the colon showing epithelial cell apoptosis*
- **Epithelial cell apoptosis** in the colon is not a primary diagnostic feature of celiac disease, which primarily affects the **small intestine**.
- This finding might be associated with other inflammatory bowel conditions or infections, not gluten-induced enteropathy.
*Esophageal endoscopy showing lower esophageal metaplasia*
- **Lower esophageal metaplasia**, or **Barrett's esophagus**, is a pre-cancerous condition of the esophagus, often caused by chronic acid reflux.
- This finding is unrelated to celiac disease and does not explain the patient's gastrointestinal symptoms or genetic predisposition.
*Liver biopsy showing apoptosis of hepatocytes*
- **Apoptosis of hepatocytes** (liver cell death) would indicate liver damage or disease, such as hepatitis or drug-induced injury.
- While celiac disease can sometimes have **hepatic manifestations**, liver apoptosis is not a primary or definitive diagnostic criterion for celiac disease itself.
Malabsorption syndromes US Medical PG Question 2: A 23-year-old man presents to the office complaining of weight loss and fatigue for the past 2 months. He states that he has been experiencing foul-smelling, light-colored stools but thinks it is because he hasn’t been eating well, recently. He has a past medical history significant for cystic fibrosis, which is well-controlled medically. He denies any shortness of breath, chest or abdominal pain, nausea, vomiting, or melena. On physical examination, his skin is pale and dry. Which of the following would be the most likely etiology of a malabsorption syndrome giving rise to this patient’s current condition?
- A. Decreased recycling of bile acids
- B. Pancreatic insufficiency (Correct Answer)
- C. Autoimmune damage to parietal cells
- D. Chronic damage to intestinal mucosa
- E. Damage to intestinal brush border
Malabsorption syndromes Explanation: ***Pancreatic insufficiency***
- Cystic fibrosis typically causes **exocrine pancreatic insufficiency** due to thick secretions blocking the pancreatic ducts, leading to malabsorption of fats and fat-soluble vitamins.
- **Foul-smelling, light-colored stools** (steatorrhea) are a classic symptom of fat malabsorption resulting from inadequate lipase production.
*Decreased recycling of bile acids*
- This typically results in **fat malabsorption**, but it is commonly associated with diseases affecting the **terminal ileum** (e.g., Crohn's disease, resection).
- While it can cause steatorrhea, it is not the primary or most common cause of malabsorption in cystic fibrosis.
*Autoimmune damage to parietal cells*
- This condition leads to **pernicious anemia** due to a lack of intrinsic factor and subsequent **vitamin B12 malabsorption**.
- It does not typically cause **steatorrhea** or generalized fat malabsorption, and it is not directly associated with cystic fibrosis.
*Chronic damage to intestinal mucosa*
- This points towards conditions like **celiac disease** or severe inflammatory bowel disease, which impair nutrient absorption through mucosal injury.
- While cystic fibrosis can have gastrointestinal manifestations, primary mucosal damage is not the leading cause of malabsorption, and the patient's symptoms are more consistent with fat malabsorption.
*Damage to intestinal brush border*
- This is characteristic of conditions like **lactase deficiency** or **celiac disease**, which affect the absorption of specific nutrients (e.g., carbohydrates).
- While it causes malabsorption, the patient's presentation with **steatorrhea** points more specifically to fat malabsorption, which is primarily due to pancreatic enzyme deficiency in cystic fibrosis.
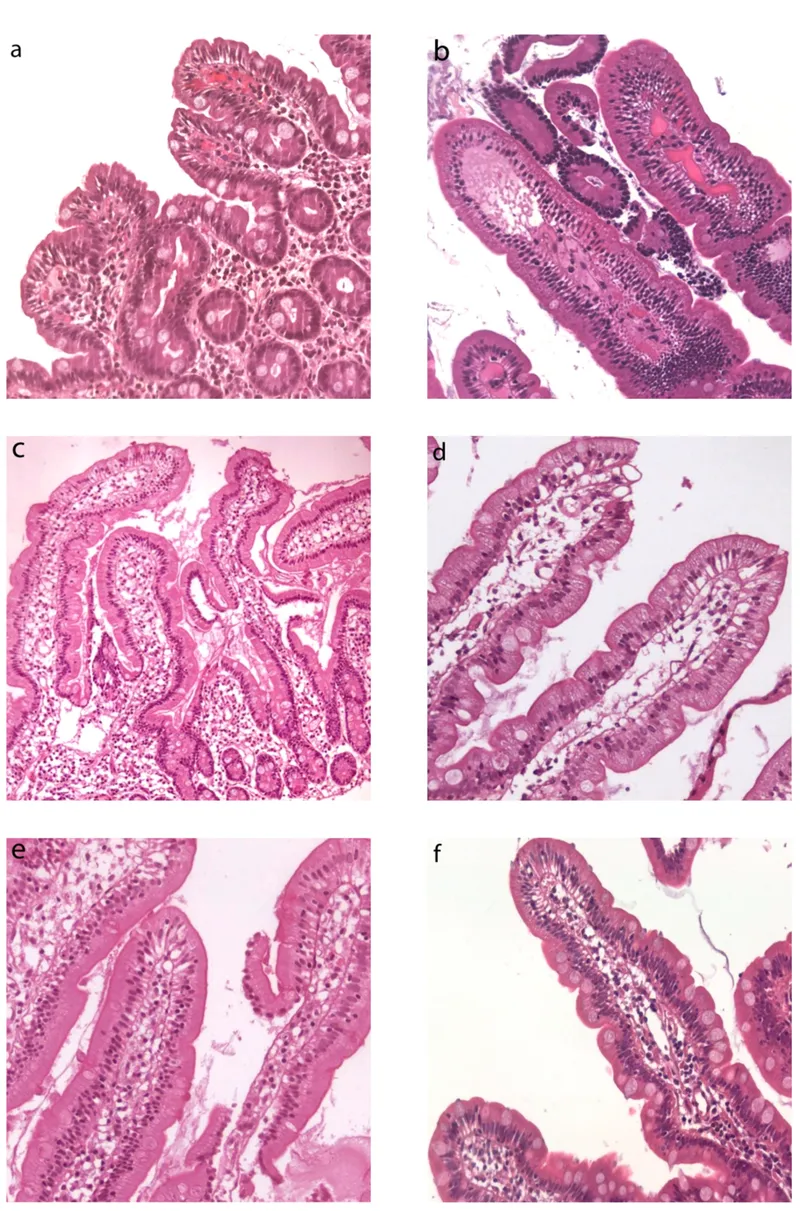
Malabsorption syndromes US Medical PG Question 3: A 63-year-old man comes to the physician with a 4-week history of fatigue, crampy abdominal pain, watery diarrhea, and pain in his mouth and gums. He returned from a 2-week trip to the Dominican Republic 2 months ago. He has smoked one pack of cigarettes daily for 45 years. Examination shows three 1.5-cm, painful ulcers in the mouth. Abdominal examination shows mild tenderness to palpation in the right lower quadrant without guarding or rebound. His hemoglobin concentration is 11.2 g/dL, mean corpuscular volume is 75 fL, and leukocyte count is 11,900/mm³. Colonoscopy shows a cobblestone mucosa. A photomicrograph of a biopsy specimen is shown. Which of the following is the most likely diagnosis?
- A. Behcet disease
- B. Tropical sprue
- C. Ulcerative colitis
- D. Crohn disease (Correct Answer)
- E. Whipple disease
Malabsorption syndromes Explanation: ***Crohn disease***
- The combination of **crampy abdominal pain**, **watery diarrhea**, **oral ulcers**, and **cobblestone mucosa** seen on colonoscopy strongly suggests Crohn disease. Crohn disease can affect any part of the gastrointestinal tract from mouth to anus, and oral manifestations like aphthous ulcers are common.
- The **microcytic anemia** (hemoglobin 11.2 g/dL, MCV 75 fL) is consistent with **chronic blood loss** and **iron malabsorption** often seen in Crohn disease. The elevated leukocyte count (11,900/mm³) indicates inflammation.
*Behcet disease*
- Behcet disease is characterized by recurrent **oral aphthous ulcers**, genital ulcers, and uveitis. While oral ulcers are present, the significant **gastrointestinal symptoms** (crampy abdominal pain, watery diarrhea, cobblestone mucosa) are not typical primary features of Behcet disease.
- Although it can rarely involve the GI tract, it typically doesn't present with extensive bowel involvement resembling inflammatory bowel disease to this degree, nor does it typically cause microcytic anemia from chronic GI blood loss.
*Tropical sprue*
- Tropical sprue typically presents with chronic **malabsorption**, foul-smelling diarrhea, and weight loss, occurring after travel to tropical regions. While the patient visited the Dominican Republic, the key findings of **oral ulcers** and **cobblestone mucosa** are not characteristic of tropical sprue.
- Tropical sprue is primarily a disease of the small intestine characterized by villous atrophy, not typically presenting with the "cobblestone" appearance associated with transmural inflammation seen in Crohn’s.
*Ulcerative colitis*
- Ulcerative colitis is characterized by continuous inflammation of the **colon and rectum**, typically presenting with bloody diarrhea and abdominal pain. While GI symptoms are present, the patient's **oral ulcers** and the finding of **cobblestone mucosa** strongly argue against ulcerative colitis.
- Ulcerative colitis affects only the colon and does not cause oral ulcers or skip lesions or transmural inflammation; the "cobblestone" appearance is indicative of deep fissures and ulcers separated by edematous mucosa, characteristic of Crohn disease.
*Whipple disease*
- Whipple disease is a rare systemic infection caused by *Tropheryma whipplei*, presenting with malabsorption, arthralgia, neurological symptoms, and lymphadenopathy. While GI symptoms like diarrhea and abdominal pain may occur, **oral ulcers** are not a typical feature, and the **colonoscopy findings** (cobblestone mucosa) are not characteristic of Whipple disease.
- Biopsy in Whipple disease would show **foamy macrophages** in the lamina propria that stain positive with periodic acid-Schiff (PAS), which is not indicated by the provided information.
Malabsorption syndromes US Medical PG Question 4: A 15-year-old girl is brought to the physician because of an 8-month history of fatigue, intermittent postprandial abdominal bloating and discomfort, foul-smelling, watery diarrhea, and a 7-kg (15-lb) weight loss. She developed a pruritic rash on her knees 3 days ago. Physical examination shows several tense, excoriated vesicles on the knees bilaterally. The abdomen is soft and nontender. Her hemoglobin concentration is 8.2 g/dL and mean corpuscular volume is 76 μm3. Further evaluation of this patient is most likely to show which of the following findings?
- A. IgA tissue transglutaminase antibodies (Correct Answer)
- B. Elevated serum amylase concentration
- C. Intraluminal esophageal membrane
- D. Periodic acid-Schiff-positive macrophages
- E. Positive hydrogen breath test
Malabsorption syndromes Explanation: ***IgA tissue transglutaminase antibodies***
- The patient's symptoms of **fatigue, abdominal bloating and discomfort, watery diarrhea, weight loss, iron deficiency anemia**, and a **pruritic rash (dermatitis herpetiformis)** are highly suggestive of **celiac disease**.
- **IgA tissue transglutaminase (tTG) antibodies** are the most sensitive and specific serological test for celiac disease.
*Elevated serum amylase concentration*
- **Elevated serum amylase** is typically indicative of **pancreatitis**, which is not supported by the patient's symptoms (e.g., severe epigastric pain radiating to the back).
- While malabsorption can lead to some pancreatic dysfunction, it would not be the primary diagnostic finding for this presentation.
*Intraluminal esophageal membrane*
- **Intraluminal esophageal membranes** or **webs** are typically associated with conditions like **Plummer-Vinson syndrome** or **eosinophilic esophagitis**, presenting with dysphagia.
- These findings do not explain the patient's prominent gastrointestinal symptoms, weight loss, rash, or anemia.
*Periodic acid-Schiff-positive macrophages*
- **Periodic acid-Schiff (PAS)-positive macrophages** in the lamina propria are characteristic of **Whipple disease**.
- Whipple disease typically presents with polyarthralgia, lymphadenopathy, and neurological symptoms in addition to malabsorption, which are not described here.
*Positive hydrogen breath test*
- A **positive hydrogen breath test** suggests **small intestinal bacterial overgrowth (SIBO)** or **lactose intolerance**.
- While SIBO can cause bloating and diarrhea, it does not explain the pruritic rash (dermatitis herpetiformis) or the severity of the anemia and weight loss as the primary diagnosis.
Malabsorption syndromes US Medical PG Question 5: A previously healthy 20-year-old woman comes to the physician because of recurrent abdominal cramps, bloating, and diarrhea for 4 months. She describes her stools as greasy, foul-smelling, and difficult to flush. During this time she has had a 6-kg (13.2-lb) weight loss. She has no personal or family history of serious illness. Physical examination shows pallor and cheilitis. Laboratory studies show a hemoglobin concentration of 11 g/dL. Serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference range. Test of the stool for occult blood is negative and stool microscopy reveals no pathogens and no leukocytes. Analysis of a 24-hour stool sample shows 12 g of fat. The patient is asked to consume 25 g of d-xylose. Five hours later, its concentration is measured in urine at 2 g (N = > 4 g/5 h). The test is repeated after a two-week course of rifaximin, but the urinary concentration of d-xylose remains the same. Which of the following is the most likely diagnosis?
- A. Exocrine pancreatic insufficiency
- B. Bacterial overgrowth in the small intestine
- C. Tropheryma whipplei infection
- D. Hypersensitivity to gliadin (Correct Answer)
- E. Lactose intolerance
Malabsorption syndromes Explanation: ***Hypersensitivity to gliadin***
* The patient's symptoms (greasy, foul-smelling stools, weight loss, abdominal cramps, bloating, diarrhea, pallor, cheilitis, iron-deficiency anemia) are highly suggestive of **malabsorption**.
* The **impaired d-xylose absorption** that does not improve after antibiotics points to an intrinsic small bowel mucosal defect rather than bacterial overgrowth, making celiac disease (hypersensitivity to gliadin) the most likely diagnosis.
*Exocrine pancreatic insufficiency*
* While it causes **steatorrhea** and malabsorption, it typically presents with normal d-xylose absorption because **d-xylose is a monosaccharide that is absorbed directly by the intestinal mucosa without requiring pancreatic enzymes**.
* The normal function of the small intestinal mucosa would allow for adequate d-xylose absorption.
*Bacterial overgrowth in the small intestine*
* Symptoms can mimic malabsorption, and d-xylose absorption may be impaired due to bacterial consumption.
* However, the patient's d-xylose test did not improve after a course of **rifaximin**, which is an antibiotic effective against bacterial overgrowth.
*Tropheryma whipplei infection*
* Whipple's disease can cause malabsorption, **steatorrhea**, and abdominal symptoms similar to those described.
* However, it also commonly presents with **arthralgia, lymphadenopathy, and neurological symptoms**, which are absent in this patient.
*Lactose intolerance*
* This condition primarily causes bloating, cramps, and diarrhea, but typically does not lead to **significant weight loss** or **steatorrhea (greasy stools)**.
* D-xylose absorption would also be expected to be normal because it is a **monosaccharide** that is absorbed directly, unlike lactose which requires lactase.
Malabsorption syndromes US Medical PG Question 6: An 82-year-old woman presents with 2 months of foul-smelling, greasy diarrhea. She says that she also has felt very tired recently and has had some associated bloating and flatus. She denies any recent abdominal pain, nausea, melena, hematochezia, or vomiting. She also denies any history of recent travel and states that her home has city water. Which of the following tests would be most appropriate to initially work up the most likely diagnosis in this patient?
- A. Fecal fat test (Correct Answer)
- B. Tissue transglutaminase antibody test
- C. Stool O&P
- D. Stool guaiac test
- E. CT of the abdomen with oral contrast
Malabsorption syndromes Explanation: ***Fecal fat test***
- The patient's symptoms of **foul-smelling, greasy diarrhea**, along with **fatigue, bloating, and flatus**, strongly suggest **malabsorption**, specifically **steatorrhea** (excess fat in stool).
- A **fecal fat test** (e.g., Sudan stain or 72-hour quantitative stool fat collection) directly assesses fat malabsorption and would be the most appropriate initial diagnostic test.
*Tissue transglutaminase antibody test*
- This test is used to screen for **celiac disease**, which can cause malabsorption symptoms.
- While celiac disease is a possibility, a fecal fat test is a more general and appropriate initial step to confirm fat malabsorption before looking for specific causes.
*Stool O&P*
- Stands for **Stool Ova and Parasites**, used to detect parasitic infections like **Giardia** or **Cryptosporidium**, which can cause diarrhea.
- However, the absence of recent travel, city water, and the prominent greasy nature of the stool make this less likely as the primary initial investigation compared to confirming malabsorption.
*Stool guaiac test*
- This test detects **occult blood in stool**.
- The patient denies **melena or hematochezia**, and there are no signs pointing to gastrointestinal bleeding, making this test irrelevant for her presenting symptoms.
*CT of the abdomen with oral contrast*
- A CT scan with contrast might be used to investigate structural abnormalities or inflammation if other tests confirm malabsorption or point to a specific organ pathology (e.g., pancreatitis, Crohn's disease).
- It's an imaging study and generally not the most appropriate *initial* test for evaluating the described symptoms of malabsorption.
Malabsorption syndromes US Medical PG Question 7: A 32-year-old woman presents with multiple pruritic papules and vesicles on her elbows and knees. She reports a history of gluten sensitivity. Skin biopsy shows granular IgA deposits in dermal papillae. Which of the following is most likely to be elevated in this patient's serum?
- A. Anti-DNA antibodies
- B. Anti-type VII collagen antibodies
- C. Anti-BP180 antibodies
- D. Anti-tissue transglutaminase antibodies (Correct Answer)
Malabsorption syndromes Explanation: ***Anti-tissue transglutaminase antibodies***
- The patient's presentation with **pruritic papules and vesicles on elbows and knees**, history of **gluten sensitivity**, and **IgA deposits in dermal papillae** points to **dermatitis herpetiformis**.
- **Dermatitis herpetiformis** is strongly associated with **celiac disease**, which involves an immune response to **gluten**, leading to elevated **anti-tissue transglutaminase (tTG) antibodies**.
*Anti-DNA antibodies*
- **Anti-DNA antibodies**, particularly **anti-dsDNA**, are characteristic markers for **systemic lupus erythematosus (SLE)**, a systemic autoimmune disease not suggested by the clinical picture or biopsy findings.
- SLE presents with a wide range of symptoms including joint pain, malar rash, renal involvement, and serositis, which are not described here.
*Anti-type VII collagen antibodies*
- **Anti-type VII collagen antibodies** are associated with **epidermolysis bullosa acquisita (EBA)**, a subepidermal blistering disease.
- EBA lesions are typically more **tense bullae** and often associated with trauma, and the immunofluorescence pattern is different from the granular IgA deposits seen in dermatitis herpetiformis.
*Anti-BP180 antibodies*
- **Anti-BP180 antibodies** (also known as anti-BPAg2) are the primary autoantibodies found in **bullous pemphigoid**, another subepidermal blistering disease.
- **Bullous pemphigoid** typically presents with large, tense blisters in elderly patients, and direct immunofluorescence shows **linear IgA/IgG deposition along the basement membrane zone**, not granular IgA in dermal papillae.
Malabsorption syndromes US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Malabsorption syndromes Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Malabsorption syndromes US Medical PG Question 9: A 52-year-old man presents with 2 months of diarrhea, abdominal pain, and fatigue. He reports a weight loss of 4 kg (8 lb). He also says his joints have been hurting recently, as well. Past medical history is unremarkable. Review of systems is significant for problems with concentration and memory. Physical examination is unremarkable. A GI endoscopy is performed with a biopsy of the small bowel. Which of the following histologic finding would most likely be seen in this patient?
- A. PAS positive macrophages (Correct Answer)
- B. Non-caseating granulomas in the small intestine
- C. Absence of nerves in the myenteric plexus
- D. Blunting of the villi
- E. Crypt hyperplasia with increased intraepithelial lymphocytes
Malabsorption syndromes Explanation: **PAS positive macrophages**
- The clinical presentation with **diarrhea**, abdominal pain, weight loss, joint pain, and **neurological symptoms** (problems with concentration and memory) is classic for **Whipple's disease**.
- **Whipple's disease** is caused by the bacterium **Tropheryma whipplei**, which is characterized histologically by **foamy macrophages** in the lamina propria that stain **positive with Periodic Acid-Schiff (PAS)** due to undigested bacterial cell wall material.
*Non-caseating granulomas in the small intestine*
- **Non-caseating granulomas** are characteristic of **Crohn's disease**, which typically presents with abdominal pain, diarrhea, and weight loss, but **neurological symptoms** are not a primary feature.
- While Crohn's disease can cause joint pain (arthritis), the combination of GI and neurological symptoms points away from it.
*Absence of nerves in the myenteric plexus*
- An **absence of nerves in the myenteric plexus** is the hallmark of **Hirschsprung's disease**, which is a congenital disorder primarily affecting neonates and infants, causing intestinal obstruction and chronic constipation.
- This finding is inconsistent with the patient's age and presenting symptoms of diarrhea and neurological issues.
*Blunting of the villi*
- **Villi blunting** is characteristic of **celiac disease** (gluten-sensitive enteropathy), which presents with malabsorption symptoms like diarrhea, weight loss, and abdominal pain.
- However, **celiac disease** typically does not involve **neurological symptoms** like concentration and memory problems as a prominent feature, and the PAS-positive macrophages are specific to Whipple's.
*Crypt hyperplasia with increased intraepithelial lymphocytes*
- **Crypt hyperplasia** and **increased intraepithelial lymphocytes (IELs)** are seen in various small bowel pathologies, including **celiac disease** and **microscopic colitis**.
- While these findings suggest intestinal inflammation, they are not specific to **Whipple's disease** and do not account for the characteristic neurological involvement.
Malabsorption syndromes US Medical PG Question 10: A 25-year-old male presents to his primary care physician for fatigue, abdominal pain, diarrhea, and weight loss. He states that this issue has occurred throughout his life but seems to “flare up” on occasion. He states that his GI pain is relieved with defecation, and his stools are frequent, large, and particularly foul-smelling. The patient has a past medical history of an ACL tear, as well as a car accident that resulted in the patient needing a transfusion and epinephrine to treat transfusion anaphylaxis. His current medications include vitamin D and ibuprofen. He recently returned from a camping trip in the eastern United States. He states that on the trip they cooked packed meats over an open fire and obtained water from local streams. His temperature is 99.5°F (37.5°C), blood pressure is 120/77 mmHg, pulse is 70/min, respirations are 11/min, and oxygen saturation is 98% on room air. Physical exam reveals poor motor control and an ataxic gait on neurologic exam. Cardiac and pulmonary exams are within normal limits. Laboratory studies are ordered and return as below:
Hemoglobin: 9.0 g/dL
Hematocrit: 25%
Haptoglobin: 12 mg/dL
Leukocyte count: 7,500 cells/mm^3 with normal differential
Platelet count: 255,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 102 mEq/L
K+: 5.0 mEq/L
HCO3-: 24 mEq/L
BUN: 24 mg/dL
Glucose: 82 mg/dL
Creatinine: 1.0 mg/dL
Ca2+: 9.0 mg/dL
LDH: 457 U/L
AST: 11 U/L
ALT: 11 U/L
Radiography is ordered which reveals a stress fracture in the patient’s left tibia. Which of the following is the best confirmatory test for this patient’s condition?
- A. Stool ELISA
- B. Vitamin B12 and folate level
- C. Vitamin E level (Correct Answer)
- D. Bowel wall biopsy
- E. Iron studies
Malabsorption syndromes Explanation: ***Vitamin E level***
- The patient's presentation suggests **celiac disease** causing **malabsorption** with secondary **vitamin E deficiency**, which is causing the specific complications seen here.
- The **neurological findings** of **ataxic gait** and **poor motor control** combined with **hemolytic anemia** (low haptoglobin 12 mg/dL, elevated LDH 457 U/L, anemia) are **pathognomonic for vitamin E deficiency**.
- Vitamin E deficiency causes **spinocerebellar degeneration**, **peripheral neuropathy**, and **hemolytic anemia** due to oxidative damage to RBC membranes and neuronal lipids.
- The **stress fracture** suggests bone disease from calcium/vitamin D malabsorption, but the neuro-hematologic picture is most specific for vitamin E.
- **Serum vitamin E level** is the **confirmatory test** for this specific deficiency syndrome causing the patient's neurological and hematological complications.
- While the underlying condition is likely celiac disease, confirming vitamin E deficiency directly explains the constellation of findings and guides immediate treatment.
*Bowel wall biopsy*
- A **small intestine biopsy** would confirm the underlying diagnosis of **celiac disease** (villous atrophy, crypt hyperplasia) causing the malabsorption.
- However, the question asks for confirmation of "this patient's condition" - referring to the specific syndrome presenting with the characteristic triad of **ataxia + hemolysis + malabsorption**.
- This triad is pathognomonic for **vitamin E deficiency**, making direct measurement more confirmatory for the presenting complication than tissue diagnosis of the underlying cause.
*Vitamin B12 and folate level*
- **Vitamin B12 deficiency** can cause **subacute combined degeneration** with ataxia and neurological symptoms, but typically presents with **posterior column signs** (loss of proprioception, vibration) and **peripheral neuropathy**, not primarily cerebellar ataxia.
- **Folate deficiency** causes **megaloblastic anemia** but does **not** cause neurological deficits or the hemolytic pattern seen here (low haptoglobin, elevated LDH with normal liver enzymes).
- The **hemolytic anemia** is specific to vitamin E deficiency, not B12/folate deficiency.
*Stool ELISA*
- Could detect **Giardia lamblia** given the history of drinking stream water during camping, which can cause acute diarrhea and malabsorption.
- However, this does not explain the **lifelong, recurring symptoms**, **neurological deficits**, **hemolytic anemia**, or **stress fracture**.
- The chronic nature points to a primary malabsorption disorder, not acute infection.
*Iron studies*
- **Iron deficiency** commonly occurs with celiac disease due to duodenal malabsorption and could contribute to the **anemia**.
- However, iron deficiency causes **microcytic anemia**, not hemolytic anemia, and does **not** explain the **low haptoglobin**, **elevated LDH**, **ataxic gait**, or **motor control issues**.
- These findings are specific to vitamin E deficiency.
More Malabsorption syndromes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.