Intestinal infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Intestinal infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Intestinal infections US Medical PG Question 1: A 16-year-old male with no significant past medical, surgical, or family history presents to his pediatrician with new symptoms following a recent camping trip. He notes that he went with a group of friends and 1 other group member is experiencing similar symptoms. Over the past 5 days, he endorses significant flatulence, nausea, and greasy, foul-smelling diarrhea. He denies tenesmus, urgency, and bloody diarrhea. The blood pressure is 118/74 mm Hg, heart rate is 88/min, respiratory rate is 14/min, and temperature is 37.0°C (98.6°F). Physical examination is notable for mild, diffuse abdominal tenderness. He has no blood in the rectal vault. What is the patient most likely to report about his camping activities?
- A. The patient camped as a side excursion from a cruise ship.
- B. The patient camped in Mexico.
- C. This has been going on for months.
- D. Recent antibiotic prescription
- E. Collecting water from a stream, without boiling or chemical treatment (Correct Answer)
Intestinal infections Explanation: ***Collecting water from a stream, without boiling or chemical treatment***
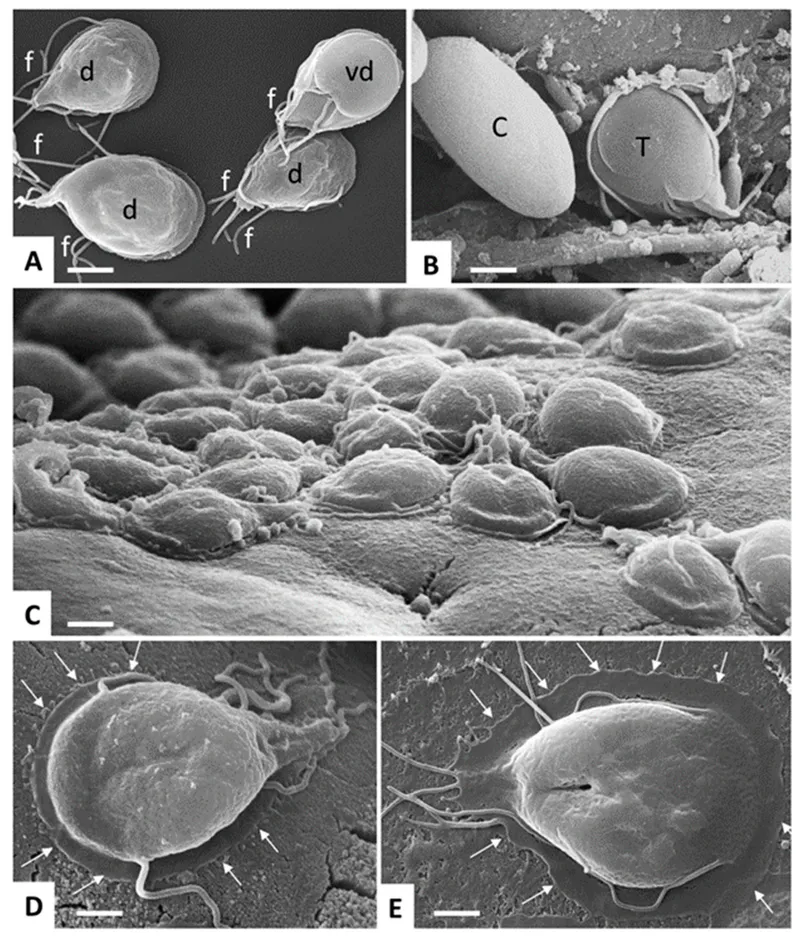
- The patient's symptoms of **greasy, foul-smelling diarrhea**, flatulence, and nausea following a camping trip are highly suggestive of **giardiasis**.
- **Giardiasis** is commonly acquired through the consumption of untreated **contaminated water**, often from streams or lakes in wilderness areas.
*The patient camped as a side excursion from a cruise ship.*
- While cruise ships can be sources of infectious outbreaks, the specific symptoms of **greasy, foul-smelling diarrhea** are less typical for common cruise-associated infections.
- Furthermore, cruise-related illnesses are usually associated with cruise ship facilities rather than **wilderness camping** directly.
*The patient camped in Mexico.*
- Traveling to Mexico is a risk factor for **traveler's diarrhea**, often caused by bacterial pathogens like ***E. coli***.
- However, typical traveler's diarrhea tends to be watery, occasionally bloody, and often presents with fever, which is not consistent with the patient's symptoms of **greasy, foul-smelling diarrhea** and absence of fever.
*This has been going on for months.*
- The symptoms are described as **new** and have developed over the past 5 days following a recent camping trip, indicating an **acute onset**, not a chronic condition.
- Chronic diarrhea lasting for months would point towards other persistent or long-term gastrointestinal issues, not an acute infection from a recent exposure.
*Recent antibiotic prescription*
- Recent antibiotic use can lead to **antibiotic-associated diarrhea**, most notably ***Clostridioides difficile*** infection.
- However, this patient has no history of recent antibiotic prescription, and the specific symptom of **greasy, foul-smelling diarrhea** is not characteristic of *C. difficile* infection.
Intestinal infections US Medical PG Question 2: A 32-year-old woman comes to the emergency department with a 2-day history of abdominal pain and diarrhea. She has had about 8 voluminous stools per day, some of which were bloody. She visited an international food festival three days ago. She takes no medications. Her temperature is 39.5°C (103.1°F), pulse is 90/min, and blood pressure is 110/65 mm Hg. Examination shows a tender abdomen, increased bowel sounds, and dry mucous membranes. Microscopic examination of the stool shows polymorphonuclear leukocytes. Stool culture results are pending. Which of the following most likely caused the patient's symptoms?
- A. Home-canned vegetables
- B. Yogurt dip
- C. Reheated rice
- D. Toxic mushrooms
- E. Omelette (Correct Answer)
Intestinal infections Explanation: **Omelette**
- The symptoms, including **bloody diarrhea**, fever, and exposure to an international food festival suggest a **bacterial infection**, likely from contaminated eggs (e.g., **Salmonella**).
- The presence of **polymorphonuclear leukocytes** in the stool indicates an **invasive bacterial infection**, consistent with salmonellosis.
*Home-canned vegetables*
- Poorly preserved home-canned vegetables are a classic cause of **botulism**, which presents with **neurological symptoms** (e.g., flaccid paralysis) and is not characterized by bloody diarrhea or fever.
- While it can cause gastrointestinal upset, bloody stools are not typical, and the primary concern is neurotoxicity due to **Clostridium botulinum toxin**.
*Yogurt dip*
- Yogurt is a dairy product, and contamination typically leads to **non-bloody diarrhea** and vomiting, often caused by bacteria like *Staphylococcus aureus* or *Bacillus cereus* producing enterotoxins.
- The symptoms would likely be less severe and lack the invasive features (bloody stools, fever, PMNs) seen in this patient.
*Reheated rice*
- Reheated rice is commonly associated with **Bacillus cereus** food poisoning, which typically causes either an emetic (vomiting) or diarrheal syndrome.
- The diarrhea caused by *Bacillus cereus* is usually **watery and non-bloody**, and it rarely presents with significant fever or invasive features like polymorphonuclear leukocytes in stool.
*Toxic mushrooms*
- Mushroom poisoning can present with a wide range of symptoms, including gastrointestinal distress (vomiting, diarrhea), but the presentation varies greatly depending on the mushroom species.
- **Bloody diarrhea** with fever and polymorphonuclear leukocytes in stool is not a typical hallmark of common toxic mushroom ingestions, which often involve hepatotoxicity or neurotoxicity.
Intestinal infections US Medical PG Question 3: A 31-year-old man comes to the physician because of a 2-day history of abdominal pain and diarrhea. He reports that his stools are streaked with blood and mucus. He returned from a vacation in the Philippines 3 weeks ago. His vital signs are within normal limits. Abdominal examination shows hyperactive bowel sounds. A photomicrograph of a trichrome-stained wet mount of a stool specimen is shown. Which of the following organisms is the most likely cause of this patient's symptoms?
- A. Campylobacter jejuni
- B. Giardia lamblia
- C. Cryptosporidium parvum
- D. Shigella dysenteriae
- E. Entamoeba histolytica (Correct Answer)
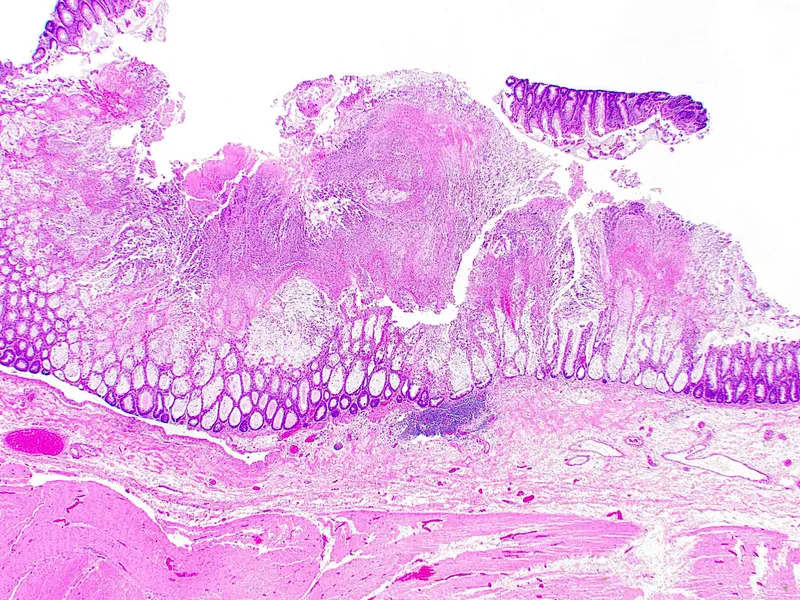
Intestinal infections Explanation: ***Entamoeba histolytica***
- The patient's symptoms of **bloody, mucoid diarrhea** (dysentery) after travel to the **Philippines** are highly suggestive of **amebic dysentery** caused by *Entamoeba histolytica*.
- A **trichrome-stained wet mount** of stool revealing trophozoites or cysts of *Entamoeba histolytica* in this clinical context would confirm the diagnosis.
*Campylobacter jejuni*
- While *Campylobacter jejuni* can cause **bloody diarrhea** and is a common cause of **traveler's diarrhea**, it is a **bacterial infection**, and the question implies a parasitic etiology with the mention of a trichrome-stained wet mount.
- Infection is typically associated with consumption of undercooked poultry or contaminated water.
*Giardia lamblia*
- *Giardia lamblia* causes **giardiasis**, which typically presents with **non-bloody, watery diarrhea**, **steatorrhea**, abdominal cramps, and bloating.
- It does not usually cause **dysentery** or bloody stools.
*Cryptosporidium parvum*
- *Cryptosporidium parvum* causes **cryptosporidiosis**, characterized by **profuse, watery diarrhea** and abdominal cramps.
- While it can be severe in immunocompromised individuals, it typically does not cause **bloody or mucoid stools** (dysentery).
*Shigella dysenteriae*
- *Shigella dysenteriae* causes **shigellosis**, a severe form of dysentery with **bloody, mucoid stools**, fever, and tenesmus.
- While it fits the clinical picture of dysentery, the diagnostic method mentioned (trichrome-stained wet mount) is primarily used for identifying **parasitic organisms**, not bacteria like *Shigella*.
Intestinal infections US Medical PG Question 4: A 2-year-old male presents to the emergency department with fatigue and lethargy. Upon presentation, the patient is found to be severely dehydrated. The patient's mother says that he has been having non-bloody diarrhea for a day. She also says that the patient has not received any vaccinations after 6 months and currently attends a daycare center. Which of the following organisms is most likely responsible for the symptoms seen in this child?
- A. Campylobacter jejuni
- B. Norovirus
- C. Shigella
- D. Salmonella
- E. Rotavirus (Correct Answer)
Intestinal infections Explanation: ***Rotavirus***
- The presentation of severe **dehydration** due to **non-bloody diarrhea** in an **unvaccinated** 2-year-old attending daycare is highly characteristic of **rotavirus gastro-enteritis**.
- Rotavirus is a common cause of severe infantile diarrhea and is notable for causing **epidemics in daycare settings** due to its easy transmission and high infectivity.
*Campylobacter jejuni*
- This typically causes **bloody diarrhea**, which is not seen in the patient's presentation.
- While it can occur in children, the sudden onset of severe dehydration with non-bloody diarrhea is less typical for *Campylobacter*.
*Norovirus*
- Norovirus is a common cause of **gastroenteritis** with vomiting and diarrhea in children and adults.
- However, rotavirus more commonly leads to **severe dehydration** requiring hospitalization in very young children, especially in unvaccinated populations.
*Shigella*
- *Shigella* infections commonly cause **dysentery**, characterized by **bloody stools**, fever, and cramps, which is not present in this case.
- While *Shigella* can cause severe illness, the history of non-bloody diarrhea makes it less likely.
*Salmonella*
- *Salmonella* gastroenteritis often presents with **fever**, **abdominal cramps**, and **bloody or non-bloody diarrhea**.
- However, it is less commonly associated with the rapid onset of severe dehydration in this age group compared to rotavirus, particularly with no mention of fever or other systemic symptoms.
Intestinal infections US Medical PG Question 5: A stool sample was taken from a 19-year-old male who presented with profuse watery diarrhea. He recently returned from a trip to Central America. A microbiologist identified the causative agent as a gram-negative, oxidase-positive, comma-shaped bacteria that is able to grow well in a pH > 8. Which of the following is a mechanism of action of the toxin produced by this bacteria?
- A. Overactivation of adenylate cyclase by inhibition of Gi subunit by ADP-ribosylation
- B. Inactivation of the 60S ribosomal subunit by cleaving an adenine from the 28S rRNA
- C. Overactivation of guanylate cyclase
- D. Overactivation of adenylate cyclase by activation of Gs subunit by ADP-ribosylation (Correct Answer)
- E. Degradation of cell membranes by hydrolysis of the phospholipids
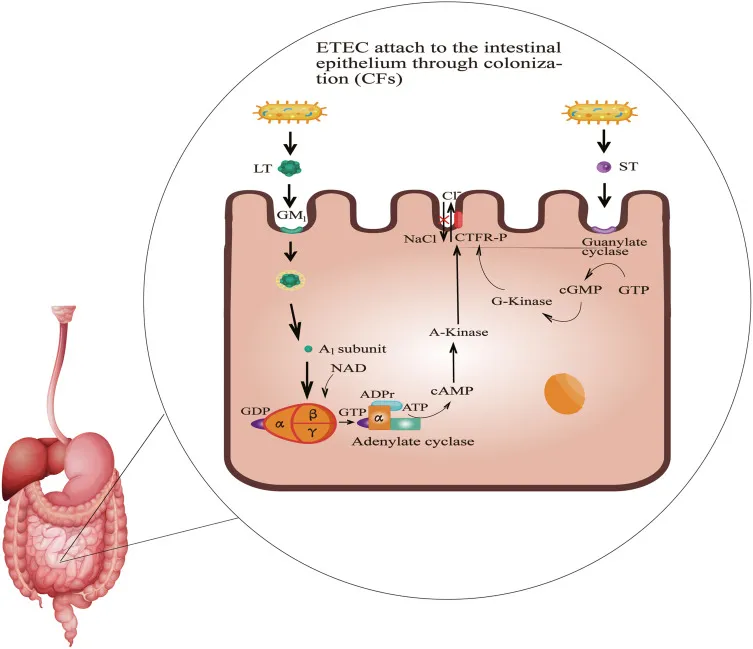
Intestinal infections Explanation: ***Overactivation of adenylate cyclase by activation of Gs subunit by ADP-ribosylation***
- The description of the bacterium as **gram-negative, oxidase-positive, comma-shaped, growing well in pH > 8**, and causing **profuse watery diarrhea** after travel to Central America points to *Vibrio cholerae*.
- **Cholera toxin** (CTX) produced by *V. cholerae* is an A-B toxin that **ADP-ribosylates the Gs α-subunit**, permanently activating **adenylate cyclase**. This leads to increased cAMP levels, causing secretion of water and electrolytes into the intestinal lumen.
*Overactivation of adenylate cyclase by inhibition of Gi subunit by ADP-ribosylation*
- This mechanism describes the action of **pertussis toxin** from *Bordetella pertussis*, which ADP-ribosylates and **inhibits the Gi subunit**, preventing adenylate cyclase inhibition.
- While both ultimately increase cAMP, the specific target and mechanism (inhibition of Gi vs. activation of Gs) differ from cholera toxin.
*Inactivation of the 60S ribosomal subunit by cleaving an adenine from the 28S rRNA*
- This mechanism is characteristic of **Shiga toxin** produced by *Shigella dysenteriae* and Shiga-like toxins (verotoxins) produced by **enterohemorrhagic *E. coli*** (EHEC).
- These toxins inhibit protein synthesis, leading to cell death and often bloody diarrhea and hemolytic uremic syndrome, which is not described here.
*Overactivation of guanylate cyclase*
- **Heat-stable enterotoxins (ST)** produced by **enterotoxigenic *E. coli*** (ETEC) activate **guanylate cyclase**, leading to increased cGMP and subsequent fluid secretion.
- While ETEC can cause watery diarrhea, the bacterial characteristics provided (oxidase-positive, comma-shaped) do not fit *E. coli*.
*Degradation of cell membranes by hydrolysis of the phospholipids*
- This mechanism is associated with toxins like **phospholipases** or **lecithinases** (e.g., alpha-toxin of *Clostridium perfringens*).
- These toxins cause direct cell lysis and tissue damage, which is not the primary mechanism of action for the watery diarrhea seen in cholera.
Intestinal infections US Medical PG Question 6: A 47-year-old man comes to the physician because of abdominal pain and foul-smelling, watery diarrhea for several days. He has not had nausea, vomiting, or blood in the stool. He has a history of alcohol use disorder and recently completed a 7-day course of clindamycin for pneumonia. He has not traveled out of the United States. Which of the following toxins is most likely to be involved in the pathogenesis of this patient's symptoms?
- A. Cereulide toxin
- B. Cholera toxin
- C. Clostridioides difficile cytotoxin (Correct Answer)
- D. Shiga toxin
- E. Alpha toxin
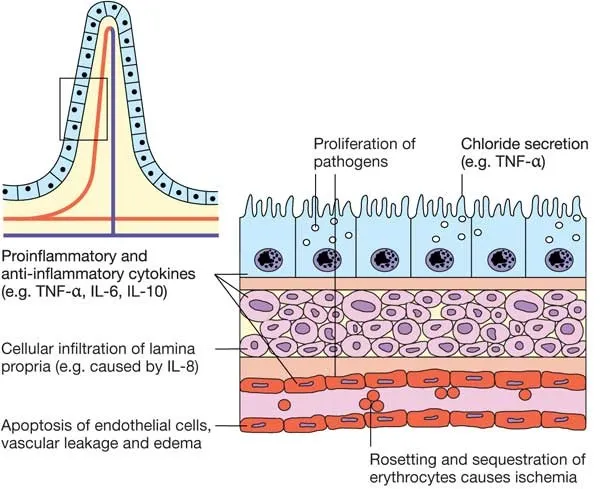
Intestinal infections Explanation: ***Clostridioides difficile cytotoxin***
- The patient's history of recent **clindamycin** use, followed by **abdominal pain** and **foul-smelling, watery diarrhea**, is highly suggestive of *Clostridioides difficile* infection.
- *C. difficile* produces **cytotoxin (TcdB)** and **enterotoxin (TcdA)**, which lead to colitis and diarrhea, often after antimicrobial therapy.
*Cereulide toxin*
- This preformed toxin is produced by *Bacillus cereus* and typically causes a **short-incubation** emetic type of food poisoning, characterized by **nausea and vomiting**.
- The patient's symptoms are primarily diarrhea, and nausea/vomiting are absent, making this less likely.
*Cholera toxin*
- Produced by *Vibrio cholerae*, this toxin causes profuse, **"rice-water" diarrhea** with rapid dehydration.
- The patient has not traveled to endemic areas, and there is no mention of the characteristic severe dehydration or "rice-water" stool.
*Shiga toxin*
- This toxin, produced by *Shigella dysenteriae* and enterohemorrhagic *E. coli* (EHEC), typically causes **bloody diarrhea** and can lead to **hemolytic uremic syndrome (HUS)**.
- The patient's diarrhea is watery and explicitly stated to be without blood, ruling out Shiga toxin as the cause.
*Alpha toxin*
- This toxin is produced by *Clostridium perfringens* and is primarily associated with **gas gangrene** (myonecrosis) and some forms of food poisoning.
- While *C. perfringens* can cause diarrhea, it's typically mild and self-limiting, and the clinical picture in this patient, especially with recent antibiotic use, points more strongly to *C. difficile*.
Intestinal infections US Medical PG Question 7: A mother brings her 4-year-old boy to the physician, as the boy has a 7-day history of foul-smelling diarrhea, abdominal cramps, and fever. The mother adds that he has been vomiting as well, and she is very much worried. The child is in daycare, and the mother endorses sick contacts with both family and friends. The boy has not been vaccinated as the parents do not think it is necessary. On physical exam, the child appears dehydrated. Stool examination is negative for blood cells, pus, and ova or parasites. What is the most likely diagnosis?
- A. Rotavirus infection (Correct Answer)
- B. Cryptosporidiosis
- C. Irritable bowel syndrome
- D. C. difficile colitis
- E. Norovirus infection
Intestinal infections Explanation: ***Rotavirus infection***
- The classic presentation of **foul-smelling diarrhea**, vomiting, abdominal cramps, and fever in an **unvaccinated child** attending daycare strongly suggests rotavirus. This virus is a common cause of **severe gastroenteritis** in young children.
- The absence of bacterial or parasitic indicators in the stool (blood cells, pus, ova/parasites) further narrows the diagnosis to a **viral cause**, with rotavirus being highly prevalent in this age group, especially without vaccination.
*Cryptosporidiosis*
- While it causes **watery diarrhea** and abdominal cramps, it is typically associated with **contaminated water sources** and often produces **oocysts** detectable in stool, which were not found in this case.
- The symptoms in the child are more classic for a common viral gastroenteritis rather than a parasitic infection, especially given the **absence of parasitic elements** on examination.
*Irritable bowel syndrome*
- **IBS** is a chronic functional gastrointestinal disorder and rarely presents acutely with fever and vomiting in a 4-year-old.
- Its diagnosis involves specific **Rome IV criteria** related to chronic abdominal pain and changes in bowel habits, which are not met by the acute presentation here.
*C. difficile colitis*
- **C. difficile colitis** typically follows **antibiotic use** or is acquired in healthcare settings and commonly causes **bloody diarrhea** and significant abdominal pain.
- The diarrhea is usually more profuse and the stool may contain **leukocytes** or be positive for C. difficile toxin, neither of which is indicated in the patient's presentation.
*Norovirus infection*
- Norovirus causes acute gastroenteritis with **vomiting** and **diarrhea**, but the diarrhea is often less foul-smelling and of shorter duration than described.
- While possible, the classic triad of **foul-smelling diarrhea, vomiting, and fever** in an unvaccinated child with sick contacts more strongly points to rotavirus, which tends to cause more severe and prolonged symptoms in young, unvaccinated children.
Intestinal infections US Medical PG Question 8: A 24-year-old woman presents with fever, abdominal pain, and bloody bowel movements. She says her symptoms onset 2 days ago and have not improved. She describes the abdominal pain as moderate, cramping in character, and poorly localized. 1 week ago, she says she was on a camping trip with her friends and had barbecued chicken which she thought tasted strange. The patient denies any chills, hemoptysis, hematochezia, or similar symptoms in the past. The vital signs include: pulse 87/min and temperature 37.8°C (100.0°F). Physical examination is significant for moderate tenderness to palpation in the periumbilical region with no rebound or guarding. Stool is guaiac positive. Which of the following is a complication associated with this patient’s most likely diagnosis?
- A. Reactive arthritis
- B. Hemolytic uremic syndrome
- C. Toxic megacolon
- D. Bacteremia
- E. Guillain-Barré syndrome (Correct Answer)
Intestinal infections Explanation: ***Guillain-Barré syndrome***
- **Guillain-Barré syndrome (GBS)** is a rare but serious post-infectious autoimmune neuropathy that can be triggered by *Campylobacter jejuni* infection.
- The patient's symptoms (fever, abdominal pain, bloody bowel movements after consuming undercooked chicken) are highly suggestive of **Campylobacter enteritis**, making GBS a potential complication.
*Reactive arthritis*
- While **reactive arthritis** can be a complication of *Campylobacter* infection, it typically involves sterile joint inflammation and is less severe than Guillain-Barré syndrome.
- Its clinical presentation often includes **asymmetric oligoarthritis**, dactylitis, and enthesitis, which are not described as the primary concern here.
*Hemolytic uremic syndrome*
- **Hemolytic uremic syndrome (HUS)** is primarily associated with **Shiga toxin-producing *E. coli* (STEC)** infections, particularly O157:H7.
- Although *Campylobacter* can rarely cause HUS, it's not the most common or direct complication compared to other options.
*Toxic megacolon*
- **Toxic megacolon** is a severe complication of inflammatory bowel disease or other severe colitis (e.g., *C. difficile* infection), characterized by acute dilation of the colon with systemic toxicity.
- While severe *Campylobacter* infection can cause colitis, toxic megacolon is a less common and specific complication in this context.
*Bacteremia*
- While **bacteremia** is possible with severe gastrointestinal infections, it is a direct extension of the infection itself rather than a post-infectious immune-mediated complication like Guillain-Barré syndrome.
- The question asks for a specific "complication," implying a distinct secondary condition.
Intestinal infections US Medical PG Question 9: A 19-year-old male college student presents to the clinic in the month of January with a 2-day history of watery diarrhea. The patient also complains of weakness, nausea, vomiting and abdominal cramps. He has no significant past medical history. He does not take any medication. He drinks socially on the weekends but does not smoke cigarettes. He recently returned from a cruise with his fraternity brothers. Blood pressure is 110/70 mm Hg, heart rate is 104/min, respiratory rate is 12/min and temperature is 37.7°C (99.9°F). On physical examination his buccal mucosa is dry. The physician suggests oral rehydration therapy. Which of the following is the most likely causative agent?
- A. Helicobacter pylori
- B. Norovirus (Correct Answer)
- C. Staphylococcus aureus
- D. Rotavirus
- E. Enterotoxigenic Escherichia coli
Intestinal infections Explanation: ***Norovirus***
- The constellation of **vomiting**, **watery diarrhea**, **abdominal cramps**, and a **recent cruise travel history** in a young adult is highly suggestive of norovirus. Norovirus outbreaks are common in semi-closed communities like cruise ships.
- Its high infectivity and rapid onset (1-2 days) align with the patient's symptoms and timeline.
*Helicobacter pylori*
- This bacterium is primarily associated with **peptic ulcers**, **gastritis**, and gastric cancer, not acute gastroenteritis with watery diarrhea and vomiting.
- Symptoms would typically be chronic abdominal pain, bloating, and possibly GI bleeding.
*Staphylococcus aureus*
- Causes **food poisoning** with a very rapid onset (1-6 hours) of severe nausea, vomiting, and abdominal cramps due to preformed toxins.
- While vomiting is present, the 2-day history is longer than typical for *S. aureus* toxin-mediated illness, and watery diarrhea is less prominent.
*Rotavirus*
- Primarily affects **infants and young children**, causing severe watery diarrhea, vomiting, and fever.
- While it can occur in adults, it's less common and the cruise ship setting points more towards norovirus in this age group.
*Enterotoxigenic Escherichia coli*
- This is a common cause of **traveler's diarrhea**, characterized by watery diarrhea and abdominal cramps, often acquired through contaminated food or water.
- While possible, the strong association with cruise ships and the prominent vomiting make norovirus a more characteristic diagnosis.
Intestinal infections US Medical PG Question 10: A 58-year-old female, being treated on the medical floor for community-acquired pneumonia with levofloxacin, develops watery diarrhea. She reports at least 9 episodes of diarrhea within the last two days, with lower abdominal discomfort and cramping. Her temperature is 98.6° F (37° C), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Her physical examination is unremarkable. Laboratory testing shows:
Hb% 13 gm/dL
Total count (WBC): 13,400/mm3
Differential count:
Neutrophils: 80%
Lymphocytes: 15%
Monocytes: 5%
ESR: 33 mm/hr
What is the most likely diagnosis?
- A. Ulcerative colitis
- B. C. difficile colitis (Correct Answer)
- C. Osmotic diarrhea
- D. Giardiasis
- E. Irritable bowel syndrome
Intestinal infections Explanation: ***C. difficile colitis***
- The patient's recent **antibiotic use (levofloxacin)**, followed by the development of **watery diarrhea** (9 episodes in 2 days) with abdominal cramping, is highly suggestive of *Clostridioides difficile* infection.
- The elevated **WBC count (13,400/mm3)** and **ESR (33 mm/hr)** indicate an inflammatory response, which is common in *C. difficile* colitis.
*Ulcerative colitis*
- Ulcerative colitis typically presents with **bloody diarrhea**, abdominal pain, and tenesmus, usually with a more chronic or relapsing course, which is not described.
- While it can manifest with flares, the direct temporal relationship with **antibiotic use** and the lack of bloody stools make it less likely.
*Osmotic diarrhea*
- Osmotic diarrhea is often related to the ingestion of **non-absorbable substances** (e.g., lactulose, sorbitol) or malabsorption and generally resolves with fasting.
- It is not typically associated with a significant **inflammatory response** (elevated WBC, ESR) or a clear link to recent antibiotic use.
*Giardiasis*
- Giardiasis is a parasitic infection that causes **protozoal diarrhea**, often characterized by foul-smelling, fatty stools, flatulence, and abdominal cramps.
- It is usually acquired from contaminated water and typically doesn't follow **antibiotic therapy** in this manner.
*Irritable bowel syndrome*
- IBS is a functional gastrointestinal disorder characterized by **chronic abdominal pain** and altered bowel habits (diarrhea, constipation, or both) in the absence of structural or biochemical abnormalities.
- It does not present as an acute, severe diarrheal illness linked to **antibiotic use** with systemic inflammatory markers.
More Intestinal infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.