Inflammatory bowel diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Inflammatory bowel diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Inflammatory bowel diseases US Medical PG Question 1: A 22-year-old woman comes to the physician because of abdominal pain and diarrhea for 2 months. The pain is intermittent, colicky and localized to her right lower quadrant. She has anorexia and fears eating due to the pain. She has lost 4 kg (8.8 lb) during this time. She has no history of a serious illness and takes no medications. Her temperature is 37.8°C (100.0°F), blood pressure 125/65 mm Hg, pulse 75/min, and respirations 14/min. An abdominal examination shows mild tenderness of the right lower quadrant on deep palpation without guarding. Colonoscopy shows small aphthous-like ulcers in the right colon and terminal ileum. Biopsy from the terminal ileum shows noncaseating granulomas in all layers of the bowel wall. Which of the following is the most appropriate pharmacotherapy at this time?
- A. Budesonide (Correct Answer)
- B. Azathioprine
- C. Ciprofloxacin
- D. Metronidazole
- E. Rectal mesalamine
Inflammatory bowel diseases Explanation: ***Budesonide***
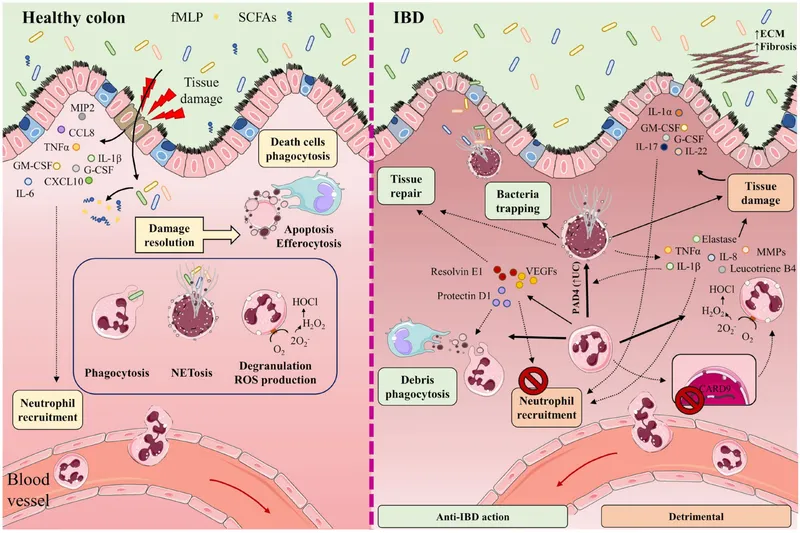
- This patient presents with symptoms and findings (RLQ pain, aphthous ulcers, noncaseating granulomas in the terminal ileum) consistent with **Crohn's disease** isolated to the **ileum and right colon**.
- **Budesonide** is a glucocorticoid with high first-pass metabolism, making it effective for localized ileal and right colonic Crohn's disease with fewer systemic side effects than prednisone.
*Azathioprine*
- **Azathioprine** is an immunomodulator used for maintaining remission in moderate to severe Crohn's disease, not typically for acute exacerbations as first-line monotherapy.
- Its onset of action is slow (several weeks to months), making it unsuitable for immediate symptom control.
*Ciprofloxacin*
- **Ciprofloxacin** is an antibiotic mainly used when there is concern for bacterial overgrowth, abscess, or perianal disease in Crohn's, none of which are explicitly indicated here.
- There is no evidence suggesting a primary bacterial infection as the cause of her current symptoms.
*Metronidazole*
- **Metronidazole** is an antibiotic often used for Crohn's disease with perianal involvement or fistulas, and sometimes for active colonic disease, but less effective for ileal involvement.
- Like ciprofloxacin, it's not the primary treatment for uncomplicated flare of ileocolonic Crohn's.
*Rectal mesalamine*
- **Rectal mesalamine** is an aminosalicylate primarily used for mild to moderate **ulcerative colitis**, particularly proctitis or left-sided colitis due to its topical action.
- It is ineffective for Crohn's disease involving the terminal ileum and right colon, as it would not reach this location in sufficient concentration.
Inflammatory bowel diseases US Medical PG Question 2: A 35-year-old man presents with yellow discoloration of his eyes and skin for the past week. He also says he has pain in the right upper quadrant for the past few days. He is fatigued constantly and has recently developed acute onset itching all over his body. The patient denies any allergies. Past medical history is significant for ulcerative colitis diagnosed 2 years ago, managed medically. He is vaccinated against hepatitis A and B and denies any recent travel abroad. There is scleral icterus present, and mild hepatosplenomegaly is noted. The remainder of the physical examination is unremarkable. Laboratory findings are significant for:
Total bilirubin 3.4 mg/dL
Prothrombin time 12 s
Aspartate transaminase (AST) 158 IU/L
Alanine transaminase (ALT) 1161 IU/L
Alkaline phosphatase 502 IU/L
Serum albumin 3.1 g/dL
Perinuclear antineutrophil cytoplasmic antibodies (p-ANCA) positive
Which of the following is the most likely diagnosis in this patient?
- A. Primary sclerosing cholangitis (Correct Answer)
- B. Hepatitis A
- C. Hepatitis B
- D. Hepatitis E
- E. Primary biliary cholangitis
Inflammatory bowel diseases Explanation: ***Primary sclerosing cholangitis***
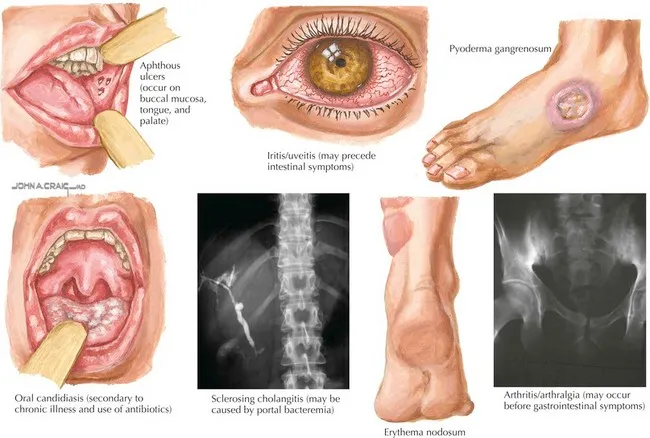
- The patient's history of **ulcerative colitis**, elevated **alkaline phosphatase**, and positive **p-ANCA** are highly suggestive of **primary sclerosing cholangitis (PSC)**.
- PSC often presents with **jaundice**, **pruritus**, and **right upper quadrant pain**, which are all present in this case.
*Hepatitis A*
- This is unlikely given the patient's **vaccination status** and the absence of recent travel to endemic areas.
- While it can cause jaundice and elevated liver enzymes, it does not explain the association with **ulcerative colitis** or **p-ANCAs**.
*Hepatitis B*
- The patient is **vaccinated against hepatitis B**, making this diagnosis very unlikely.
- Chronic hepatitis B can cause liver damage, but symptoms would typically be more gradual, and it is not directly associated with **ulcerative colitis** or **p-ANCA**.
*Hepatitis E*
- Although hepatitis E can cause acute hepatitis with jaundice, the patient denies recent travel abroad to **endemic areas**, and there's no clear exposure route.
- Furthermore, it does not explain the chronic association with **ulcerative colitis** or the presence of **p-ANCA**.
*Primary biliary cholangitis*
- While it shares features like **pruritus** and elevated **alkaline phosphatase**, it is more commonly associated with **anti-mitochondrial antibodies (AMAs)**, which were not mentioned, and often affects middle-aged women.
- It is also not typically associated with **ulcerative colitis** or positive **p-ANCA** to the same extent as PSC.
Inflammatory bowel diseases US Medical PG Question 3: An 18-year-old man presents with bloody diarrhea and weight loss. He undergoes endoscopic biopsy which shows pseudopolyps. Biopsies taken during the endoscopy show inflammation only involving the mucosa and submucosa. He is diagnosed with an inflammatory bowel disease. Which of the following characteristics was most likely present?
- A. Cobblestone mucosa
- B. Skip lesions
- C. Fistulas and strictures
- D. Noncaseating granuloma
- E. Rectal involvement (Correct Answer)
Inflammatory bowel diseases Explanation: **_Rectal involvement_**
- The description of **bloody diarrhea** and **pseudopolyps** on endoscopy, along with inflammation limited to the **mucosa and submucosa**, is highly characteristic of **ulcerative colitis (UC)**. UC invariably involves the rectum and extends proximally in a continuous fashion.
- The presence of **pseudopolyps** is common in UC due to cycles of mucosal ulceration and regeneration.
*Cobblestone mucosa*
- **Cobblestone mucosa** is a classic endoscopic finding in **Crohn's disease**, resulting from deep ulcerations interspersed with islands of edematous, non-ulcerated mucosa.
- This feature points to a transmural pattern of inflammation, which is inconsistent with the superficial inflammation confined to the **mucosa and submucosa** described.
*Skip lesions*
- **Skip lesions** refer to discontinuous areas of inflammation separated by healthy tissue, a hallmark feature of **Crohn's disease**.
- **Ulcerative colitis** (implied by the superficial inflammation) is characterized by continuous inflammation extending proximally from the rectum without skipped areas.
*Fistulas and strictures*
- **Fistulas** (abnormal connections between organs or to the skin) and **strictures** (narrowing of the intestinal lumen) are complications typically associated with **Crohn's disease**, due to its **transmural inflammation**.
- These are rare in **ulcerative colitis**, which primarily affects the superficial layers of the colon.
*Noncaseating granuloma*
- The presence of **noncaseating granulomas** on biopsy is a key histological feature distinguishing **Crohn's disease** from ulcerative colitis.
- The inflammation described as restricted to the **mucosa and submucosa** makes granulomas less likely, as they often imply a transmural process.
Inflammatory bowel diseases US Medical PG Question 4: A 38-year-old man presents to his primary care provider for abdominal pain. He reports that he has had a dull, burning pain for several months that has progressively gotten worse. He also notes a weight loss of about five pounds over that time frame. The patient endorses nausea and feels that the pain is worse after meals, but he denies any vomiting or diarrhea. He has a past medical history of hypertension, and he reports that he has been under an unusual amount of stress since losing his job as a construction worker. His home medications include enalapril and daily ibuprofen, which he takes for lower back pain he developed at his job. The patient drinks 1-2 beers with dinner and has a 25-pack-year smoking history. His family history is significant for colorectal cancer in his father and leukemia in his grandmother. On physical exam, the patient is moderately tender to palpation in the epigastrium. A fecal occult test is positive for blood in the stool.
Which of the following in the patient’s history is most likely causing this condition?
- A. Family history of cancer
- B. Physiologic stress
- C. Medication use (Correct Answer)
- D. Smoking history
- E. Alcohol use
Inflammatory bowel diseases Explanation: ***Medication use***
- The patient's daily use of **ibuprofen**, an **NSAID**, is a significant risk factor for **peptic ulcer disease**, which can cause abdominal pain, weight loss, and GI bleeding.
- NSAIDs **inhibit prostaglandin synthesis**, disrupting the protective **gastric mucosal barrier**.
*Family history of cancer*
- While a family history of colorectal cancer can increase an individual's risk, the patient's symptoms (epigastric pain, pain worse after meals, positive fecal occult) are more characteristic of an **upper GI source**, not typically colorectal cancer.
- The type of cancers in his family (colorectal, leukemia) are not directly linked to the patient's current presentation of **epigastric pain** and likely **gastric ulceration**.
*Physiologic stress*
- While stress can exacerbate gastrointestinal symptoms and is a risk factor for various GI issues, the combination of specific symptoms (burning pain, post-prandial worsening, and GI bleeding) points more strongly to an **organic cause** like an ulcer, particularly given the other risk factors.
- Stress alone is less likely to be the primary cause of a **positive fecal occult test** and the described persistent, worsening pain over several months without other clear organic pathology.
*Smoking history*
- **Smoking** is a known risk factor for **peptic ulcer disease** and an independent risk factor for many GI cancers.
- However, the direct, immediate causal link to the patient's acute presentation of symptoms and positive fecal occult test is less direct than NSAID use.
*Alcohol use*
- Moderate alcohol intake (1-2 beers daily) is generally not considered a direct or primary cause of peptic ulcer disease in the same way that NSAID use is.
- While excessive alcohol can irritate the gastric mucosa, this patient's reported intake is **not typically sufficient** to be the most likely sole cause of the described symptoms and bleeding.
Inflammatory bowel diseases US Medical PG Question 5: A 22-year-old woman presents to the emergency department with a 3-day history of fever and abdominal pain. She says that the pain is located in the left lower quadrant of the abdomen and feels crampy in nature. The pain has been associated with bloody diarrhea and joint tenderness. She has no past medical history but says that she returned 2 weeks ago from vacation in Asia where she tried many new foods. Her family history is significant for multiple cancers in close relatives. Physical exam reveals swollen ulcers on her legs, and colonoscopy reveals contiguous ulcerations from the rectum through the descending colon. Which of the following is associated with the most likely cause of this patient's symptoms?
- A. Noncaseating granulomas
- B. Severe aortic stenosis
- C. Gram-negative rod
- D. HLA-DQ2 positivity
- E. Perinuclear anti-neutrophil cytoplasmic antibodies (Correct Answer)
Inflammatory bowel diseases Explanation: ***Perinuclear anti-neutrophil cytoplasmic antibodies***
- The patient's presentation with **bloody diarrhea**, low-grade fever, **crampy abdominal pain**, joint tenderness, and contiguous ulcerations in the colon is highly suggestive of **ulcerative colitis**.
- **Perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA)** are found in 50-70% of patients with ulcerative colitis and are associated with a more extensive disease.
*Noncaseating granulomas*
- **Noncaseating granulomas** are a characteristic histological finding in **Crohn's disease**, not ulcerative colitis.
- Crohn's disease typically presents with **skip lesions**, **transmural inflammation**, and affects any part of the GI tract, often with perianal disease.
*Severe aortic stenosis*
- **Severe aortic stenosis** is a condition of the heart valves that can lead to symptoms like chest pain, syncope, and heart failure, and is not directly associated with the patient's gastrointestinal and systemic symptoms.
- While inflammatory conditions can rarely have cardiac manifestations, there's no direct link between aortic stenosis and inflammatory bowel disease in this context.
*Gram-negative rod*
- While infections, especially from **Gram-negative rods** like *Shigella* or *Salmonella*, can cause acute bloody diarrhea, the 3-day history with joint tenderness and contiguous ulcers on colonoscopy points more towards an inflammatory bowel disease.
- The chronicity and systemic involvement are less typical for an acute bacterial enteritis, although such infections might trigger IBD.
*HLA-DQ2 positivity*
- **HLA-DQ2 positivity** is strongly associated with **celiac disease**, an immune-mediated enteropathy triggered by gluten.
- Celiac disease typically presents with malabsorption symptoms like fatty stools, weight loss, and iron deficiency, rather than bloody diarrhea and contiguous colonic ulcerations.
Inflammatory bowel diseases US Medical PG Question 6: A 25-year-old man presents with abdominal pain and bloody diarrhea. His symptoms have been recurrent for the past few months, and, currently, he says he is having on average four bowel movements daily, often bloody. He describes the pain as cramping and localized to the left side of his abdomen. He also says that he has lost around 4.5 kg (10 lb) over the past 3 months. There is no other significant past medical history and the patient is not on current medications. His temperature is 37.7° C (100.0° F), pulse rate is 100/min, respiratory rate is 18/min, and blood pressure is 123/85 mm Hg. On physical examination, there is mild tenderness to palpation in the lower left quadrant of the abdomen with no rebound or guarding. Laboratory studies show anemia and thrombocytosis. Colonoscopy is performed, which confirms the diagnosis of ulcerative colitis (UC). What is the mechanism of action of the recommended first-line medication for the treatment of this patient’s condition?
- A. Suppression of cellular and humoral immunity
- B. TNF-⍺ antagonism
- C. Inhibition of enzyme phospholipase A2
- D. Cross-linking of bacterial DNA
- E. Inhibition of leukotriene synthesis and lipoxygenase (Correct Answer)
Inflammatory bowel diseases Explanation: ***Inhibition of leukotriene synthesis and lipoxygenase***
- The first-line medications for mild to moderate ulcerative colitis (UC) are **aminosalicylates** like **mesalamine** (5-ASA).
- Mesalamine is thought to exert its anti-inflammatory effects by inhibiting **leukotriene synthesis** and the **lipoxygenase pathway**, thereby reducing inflammation in the colon.
*Suppression of cellular and humoral immunity*
- This mechanism of action describes **immunosuppressants** such as azathioprine or methotrexate, which are typically used for more severe or refractory cases of UC, not as first-line therapy.
- These drugs broadly suppress the immune system, leading to a higher risk of infections and other side effects.
*TNF-⍺ antagonism*
- This is the mechanism of action of **biologic agents** like infliximab or adalimumab, which are reserved for moderate to severe UC that has not responded to conventional therapy.
- **TNF-α inhibitors** block the inflammatory cytokine TNF-α, reducing inflammation but are not the initial treatment choice.
*Inhibition of enzyme phospholipase A2*
- This mechanism describes **corticosteroids** such as prednisone or budesonide, which are used to induce remission in moderate to severe UC flares, but not as first-line maintenance therapy due to significant side effects.
- Corticosteroids inhibit **phospholipase A2**, thereby blocking the entire arachidonic acid cascade and the production of all inflammatory mediators.
*Cross-linking of bacterial DNA*
- This mechanism describes **antibiotics** like metronidazole or ciprofloxacin, which work by cross-linking DNA in bacteria.
- While antibiotics may be used in specific UC scenarios (such as pouchitis or suspected superimposed infection), UC itself is an idiopathic inflammatory disease, not a bacterial infection, and antibiotics are not first-line treatment for the underlying condition.
Inflammatory bowel diseases US Medical PG Question 7: A 31-year-old woman visits the clinic with chronic diarrhea on most days for the past four months. She also complains of lower abdominal discomfort and cramping, which is relieved by episodes of diarrhea. She denies any recent change in her weight. Bowel movements are preceded by a sensation of urgency, associated with mucus discharge, and followed by a feeling of incomplete evacuation. The patient went camping several months earlier, and another member of her camping party fell ill recently. Her temperature is 37° C (98.6° F), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Her physical examination is unremarkable. A routine stool examination is within normal limits and blood test results show:
Hb% 13 gm/dL
Total count (WBC): 11,000/mm3
Differential count:
Neutrophils: 70%
Lymphocytes: 25%
Monocytes: 5%
ESR: 10 mm/hr
What is the most likely diagnosis?
- A. Giardiasis
- B. Ulcerative colitis
- C. Crohn’s disease
- D. Irritable bowel syndrome (Correct Answer)
- E. Laxative abuse
Inflammatory bowel diseases Explanation: ***Irritable bowel syndrome (IBS)***
- The patient's symptoms of chronic diarrhea, abdominal discomfort relieved by defecation, urgency, and incomplete evacuation, without significant weight loss or alarming signs, are highly characteristic of **Irritable Bowel Syndrome** meeting **Rome IV criteria**.
- The camping history suggests possible infectious gastroenteritis, but the **chronic duration (4 months)**, **normal stool examination**, and **absence of systemic illness** make infectious causes unlikely.
- The mild WBC elevation and normal ESR are non-specific findings; IBS is a **functional disorder** without inflammatory markers.
*Giardiasis*
- While giardiasis can cause chronic diarrhea, it often presents with **malabsorption symptoms** such as fatty stools, weight loss, and nutrient deficiencies.
- The routine stool examination being within normal limits makes giardiasis less likely, as **Giardia cysts or trophozoites** would typically be detected on microscopy.
*Ulcerative colitis*
- Ulcerative colitis is an **inflammatory bowel disease** typically characterized by bloody diarrhea, abdominal pain, and systemic symptoms like fever and weight loss.
- The patient's symptoms include the absence of blood in stools and no weight loss, with **normal ESR**, which makes ulcerative colitis unlikely.
*Crohn's disease*
- Crohn's disease is another **inflammatory bowel disease** that can affect any part of the GI tract and presents with chronic diarrhea, abdominal pain, and often systemic symptoms like weight loss, fever, or perianal disease.
- The lack of weight loss, systemic inflammation markers (normal ESR), and absence of blood or inflammatory markers in the stool make Crohn's disease less probable.
*Laxative abuse*
- Laxative abuse can cause chronic diarrhea, but it's typically associated with a history of **eating disorders** (anorexia nervosa, bulimia nervosa) or other psychological conditions, which are not mentioned in this case.
- The patient's description of abdominal discomfort relieved by defecation, urgency, and incomplete evacuation is more consistent with **IBS** (a functional bowel disorder) rather than solely laxative-induced diarrhea.
Inflammatory bowel diseases US Medical PG Question 8: A 52-year-old woman complains of intermittent diffuse abdominal pain that becomes worse after eating meals and several episodes of diarrhea, the last of which was bloody. These symptoms have been present for the previous 6 months but have worsened recently. She has had significant weight loss since the onset of symptoms. Her past medical history includes systemic lupus erythematosus (SLE), which has been difficult to manage medically. Vital signs include a blood pressure of 100/70 mm Hg, temperature of 37.1°C (98.8 °F), and pulse of 95/min. On physical examination, the patient appears to be in severe pain, and there is mild diffuse abdominal tenderness. Which of the following is the most likely diagnosis?
- A. Ischemic bowel disease (Correct Answer)
- B. Small bowel obstruction
- C. Acute pancreatitis
- D. Gastroenteritis
- E. Ulcerative colitis
Inflammatory bowel diseases Explanation: ***Ischemic bowel disease***
- The patient's history of **diffuse abdominal pain worsening after meals** (postprandial pain or "abdominal angina"), **bloody diarrhea**, and **significant weight loss** is highly suggestive of **chronic mesenteric ischemia**.
- Her history of **systemic lupus erythematosus (SLE)**, which can cause **vasculitis** and **hypercoagulability**, increases the risk of mesenteric artery thrombosis or emboli, leading to bowel ischemia.
*Small bowel obstruction*
- This typically presents with **colicky abdominal pain**, **vomiting**, and **abdominal distension**, often with obstipation.
- While it can cause pain, it does not typically lead to **bloody diarrhea** or chronic postprandial worsening of symptoms.
*Acute pancreatitis*
- Characterized by **severe epigastric pain** radiating to the back, often associated with nausea and vomiting, and elevated lipase/amylase.
- It does not typically present with **bloody diarrhea** or a chronic history of symptoms worsening after eating.
*Gastroenteritis*
- Usually presents with **acute onset** of nausea, vomiting, diarrhea, and fever, often resolving within a few days to a week.
- The **chronic nature** (6 months) of symptoms, significant weight loss, and the specific pattern of postprandial pain make gastroenteritis unlikely.
*Ulcerative colitis*
- While it causes **bloody diarrhea** and abdominal pain, it typically involves the colon and rectum, and pain is less commonly described as diffuse and worsening specifically after meals due to ischemia.
- The primary symptoms are usually **tenesmus**, frequent bowel movements, and rectal bleeding, and it does not typically present with the specific "abdominal angina" associated with mesenteric ischemia.
Inflammatory bowel diseases US Medical PG Question 9: A 24-year-old woman comes to the physician because of progressively worsening episodes of severe, crampy abdominal pain and nonbloody diarrhea for the past 3 years. Examination of the abdomen shows mild distension and generalized tenderness. There is a fistula draining stool in the perianal region. Immunohistochemistry shows dysfunction of the nucleotide oligomerization binding domain 2 (NOD2) protein. This dysfunction most likely causes overactivity of which of the following immunological proteins in this patient?
- A. Interferon-γ
- B. β-catenin
- C. IL-1β
- D. IL-10
- E. NF-κB (Correct Answer)
Inflammatory bowel diseases Explanation: ***NF-κB***
- **NOD2** is a pattern recognition receptor that normally detects bacterial products and regulates inflammatory responses. In **Crohn's disease**, loss-of-function **NOD2 mutations** lead to impaired bacterial sensing and clearance.
- This defective NOD2 function results in **compensatory overactivation of NF-κB** through alternative inflammatory pathways (particularly TLR signaling), causing excessive **pro-inflammatory cytokine** production.
- This **NF-κB hyperactivation** is a key driver of chronic inflammation in **Crohn's disease**, contributing to symptoms like fistulas, strictures, and transmural inflammation.
*Interferon-γ*
- **Interferon-γ** is an important pro-inflammatory cytokine in Crohn's disease and is part of the Th1-mediated immune response.
- However, its production is downstream of **NF-κB** activation and other inflammatory cascades. **NOD2 dysfunction** does not directly cause **IFN-γ** overactivity through the primary molecular pathway.
*β-catenin*
- **β-catenin** is a key component of the **Wnt signaling pathway** involved in cell adhesion, proliferation, and differentiation.
- It is not directly affected by **NOD2 dysfunction**. Dysregulation of **β-catenin** is more commonly associated with colorectal adenomas and cancer, not the inflammatory mechanisms of Crohn's disease.
*IL-1β*
- **IL-1β** is a potent pro-inflammatory cytokine that is indeed elevated in **Crohn's disease**.
- However, **IL-1β** is produced **downstream** of **NF-κB** activation. The primary molecular consequence of **NOD2 dysfunction** is the overactivity of **NF-κB**, which then drives production of various cytokines including **IL-1β**.
*IL-10*
- **IL-10** is an **anti-inflammatory cytokine** essential for maintaining intestinal immune homeostasis and suppressing excessive inflammatory responses.
- In Crohn's disease, **IL-10** signaling is often **impaired or deficient** rather than overactive. The question asks about overactivity, making this the opposite of what occurs in the disease.
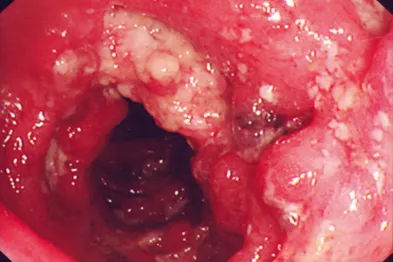
Inflammatory bowel diseases US Medical PG Question 10: A 27-year-old woman presents to her primary care physician for evaluation of involuntary weight loss and recurrent abdominal pain. She noticed blood in her stool several times. The medical history is significant for the polycystic ovarian syndrome. The vital signs are as follows: temperature, 38.0°C (100.4°F); heart rate, 78/min; respiratory rate, 14/min; and blood pressure, 110/80 mm Hg. The family history is notable for paternal colon cancer. A colonoscopy is performed and is presented in the picture. What findings are expected?
- A. Crypt abscess (Correct Answer)
- B. Dermatitis herpetiformis
- C. Blunting of villi and crypt hyperplasia
- D. Non-caseating granulomas
- E. Aphthous stomatitis
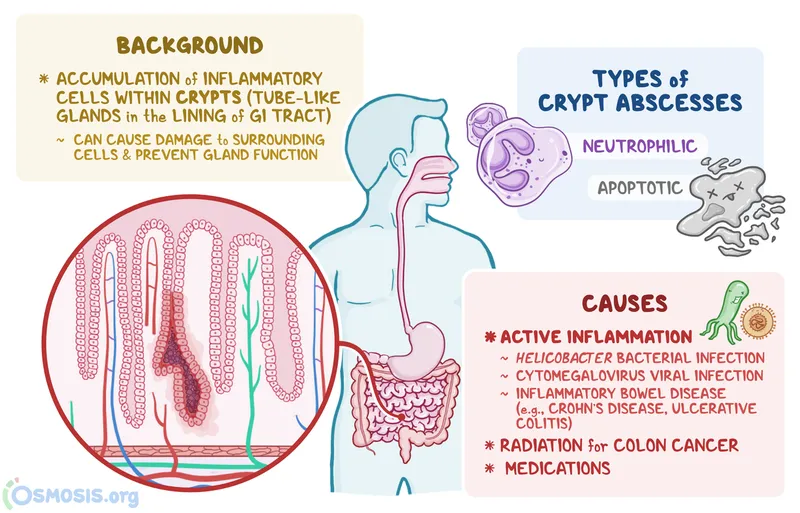
Inflammatory bowel diseases Explanation: ***Crypt abscess***
- The image provided shows **neutrophils infiltrating and filling the crypt lumina**, which are characteristic findings of crypt abscesses seen in **ulcerative colitis**.
- This pathology, combined with the patient's symptoms of **bloody diarrhea**, involuntary weight loss, and recurrent abdominal pain, points towards an inflammatory bowel disease, most consistent with ulcerative colitis.
*Dermatitis herpetiformis*
- This is a **skin manifestation of celiac disease**, presenting as intensely pruritic papules and vesicles, typically on extensor surfaces.
- It is not directly associated with inflammatory bowel disease, especially ulcerative colitis, and is not a histological finding in the colon.
*Blunting of villi and crypt hyperplasia*
- These are characteristic histological findings of **celiac disease** in the **small intestine**.
- The patient's symptoms and the histological image are from the colon, ruling out celiac disease as the primary diagnosis.
*Aphthous stomatitis*
- While **aphthous ulcers** are common extraintestinal manifestations in both Crohn's disease and ulcerative colitis, it is a clinical finding in the oral cavity, not a histological finding in the colon.
- The question asks for *other findings expected* in the context of the provided colonic histology.
*Non-caseating granulomas*
- **Non-caseating granulomas** are a hallmark histological feature of **Crohn's disease**, not ulcerative colitis.
- The image shown, with widespread crypt abscesses and diffuse inflammatory infiltrate, is more typical of ulcerative colitis rather than Crohn's disease.
More Inflammatory bowel diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.