Hernia complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hernia complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hernia complications US Medical PG Question 1: A 36-year-old woman is brought to the emergency department 20 minutes after being involved in a high-speed motor vehicle collision. On arrival, she is unconscious. Her pulse is 140/min, respirations are 12/min and shallow, and blood pressure is 76/55 mm Hg. 0.9% saline infusion is begun. A focused assessment with sonography shows blood in the left upper quadrant of the abdomen. Her hemoglobin concentration is 7.6 g/dL and hematocrit is 22%. The surgeon decided to move the patient to the operating room for an emergent explorative laparotomy. Packed red blood cell transfusion is ordered prior to surgery. However, a friend of the patient asks for the transfusion to be held as the patient is a Jehovah's Witness. The patient has no advance directive and there is no documentation showing her refusal of blood transfusions. The patient's husband and children cannot be contacted. Which of the following is the most appropriate next best step in management?
- A. Administer hydroxyethyl starch
- B. Transfusion of packed red blood cells (Correct Answer)
- C. Consult hospital ethics committee
- D. Administer high-dose iron dextran
Hernia complications Explanation: ***Transfusion of packed red blood cells***
- This patient is in **hemorrhagic shock** (tachycardia, hypotension, low hemoglobin, and hematocrit with evidence of active bleeding), requiring emergent blood transfusion to prevent irreversible organ damage and death.
- In an **emergency setting** with an **unconscious patient** and **no documented refusal** of blood products, the principle of **presumed consent** for life-saving treatment takes precedence, especially when next of kin cannot be reached.
*Administer hydroxyethyl starch*
- **Colloids** like hydroxyethyl starch can temporarily increase intravascular volume but do not provide oxygen-carrying capacity, which is critically needed for a patient with severe anemia and hemorrhagic shock.
- While useful for volume expansion, it is **not a substitute for blood products** in severe bleeding and can have adverse effects such as kidney injury.
*Consult hospital ethics committee*
- Consulting an ethics committee is appropriate for **complex ethical dilemmas** when there is time for deliberation and the patient's life is not in immediate danger.
- In this acute, life-threatening emergency, **delaying treatment** to consult an ethics committee would jeopardize the patient's life and is not appropriate.
*Administer high-dose iron dextran*
- **Iron dextran** is used to treat iron-deficiency anemia and works by supporting red blood cell production over several days to weeks.
- It is **ineffective in acute hemorrhagic shock** where immediate restoration of oxygen-carrying capacity is required.
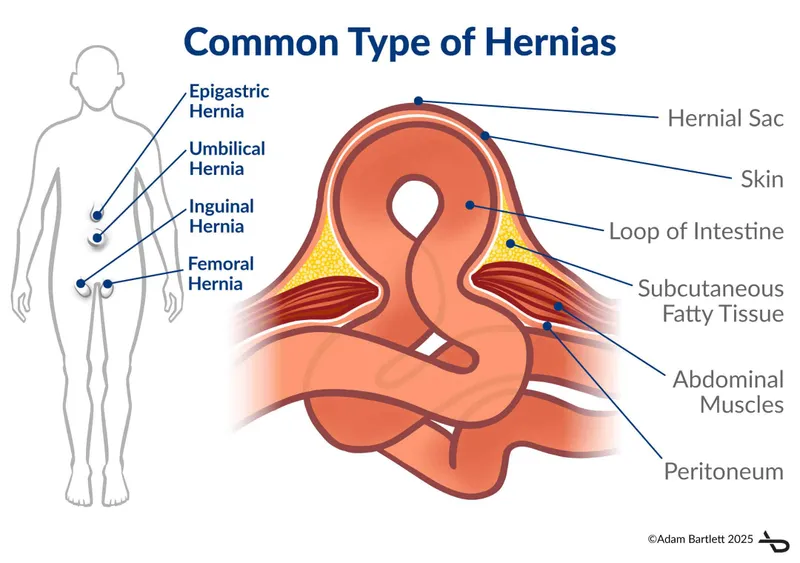
Hernia complications US Medical PG Question 2: A 67-year-old woman is brought to the emergency department by her husband because of a 1-hour history of severe groin pain, nausea, and vomiting. She has had a groin swelling that worsens with standing, coughing, and straining for the past 3 months. Her pulse is 120/min. Examination shows pallor; there is swelling, erythema, and tenderness to palpation of the right groin that is centered below the inguinal ligament. The most likely cause of this patient's condition is entrapment of an organ between which of the following structures?
- A. Inferior epigastric artery and rectus sheath
- B. Lacunar ligament and femoral vein (Correct Answer)
- C. Medial and median umbilical ligaments
- D. Conjoint tendon and inguinal ligament
- E. Linea alba and conjoint tendon
Hernia complications Explanation: ***Lacunar ligament and femoral vein***
- The patient presents with symptoms highly suggestive of a **strangulated femoral hernia**, characterized by acute severe groin pain, nausea, vomiting, and a tender, erythematous groin swelling located below the inguinal ligament.
- A femoral hernia involves the protrusion of abdominal contents through the femoral canal, which is bounded medially by the **lacunar (Gimbernat's) ligament** and laterally by the **femoral vein**, making this the most likely site of entrapment.
*Inferior epigastric artery and rectus sheath*
- This configuration describes the likely location of an **epigastric hernia** or the boundaries relevant to a **direct inguinal hernia**, but not a femoral hernia.
- An epigastric hernia is located in the midline above the umbilicus, and an indirect inguinal hernia is lateral to the inferior epigastric artery, which is not consistent with the patient's symptoms.
*Medial and median umbilical ligaments*
- These ligaments are remnants of fetal structures (umbilical arteries and urachus, respectively) and are primarily associated with the anterior abdominal wall, specifically in the umbilical region.
- They are not directly involved in the formation or boundaries of a **femoral hernia**.
*Conjoint tendon and inguinal ligament*
- The **conjoint tendon** (formed by the internal oblique and transversus abdominis muscles) and the **inguinal ligament** are key structures defining the posterior and inferior boundaries of the **inguinal canal**.
- This anatomical relationship is pertinent to **inguinal hernias** (both direct and indirect), which are located above the inguinal ligament, unlike the patient's swelling which is below it.
*Linea alba and conjoint tendon*
- The **linea alba** is a fibrous structure in the midline of the anterior abdominal wall that can be the site of epigastric or umbilical hernias.
- The **conjoint tendon** is involved in inguinal hernias. Neither of these structures, in combination, defines the boundary of a femoral hernia.
Hernia complications US Medical PG Question 3: A 22-year-old man is brought to the emergency department by his friends 30 minutes after falling down a flight of stairs. His friends report that they were at a college party, where he drank large amounts of alcohol. He is aggressive and restless. Examination shows tenderness to palpation and swelling of his right lower leg. An x-ray of the right leg shows a lower tibial shaft fracture. The physician recommends overnight observation and surgery the following morning. The patient refuses the suggested treatment and requests immediate discharge. Otherwise, he says, he will call his lawyer and sue the entire medical staff involved in his care. Which of the following is the most appropriate response by the physician?
- A. You can leave the hospital after signing a self-discharge against medical advice form.
- B. If you don't consent to treatment, I'll be forced to obtain consent from your parents.
- C. I understand that you want to go home, but I'll have to keep you here as long as you are intoxicated. (Correct Answer)
- D. Have you ever felt you should cut down on your drinking?
- E. I can't force you to stay here, but I'll have to inform your dean of this incident.
Hernia complications Explanation: ***I understand that you want to go home, but I'll have to keep you here as long as you are intoxicated.***
- An **intoxicated patient may lack decision-making capacity** to refuse medically necessary treatment for a serious injury.
- Before accepting a refusal of treatment or allowing AMA discharge, physicians must **assess the patient's capacity** to make informed decisions.
- Signs of impaired capacity include **acute intoxication, aggressive behavior, and restlessness**, all present in this patient.
- Temporarily holding a patient who lacks capacity and has a serious medical condition requiring urgent care is **legally and ethically justified** to prevent harm—this is NOT false imprisonment.
- Once the patient regains capacity (i.e., sobers up), his decision-making ability can be reassessed, and if he still refuses, AMA discharge can be offered.
*You can leave the hospital after signing a self-discharge against medical advice form.*
- While competent adults have the right to refuse treatment and leave AMA, this option is **premature** because it fails to address the patient's **impaired decision-making capacity** due to acute intoxication.
- A valid refusal requires **capacity to understand the risks and consequences** of leaving—offering AMA discharge without capacity assessment is inappropriate and potentially negligent.
*I can't force you to stay here, but I'll have to inform your dean of this incident.*
- Threatening to inform the patient's dean is a **breach of confidentiality** and an unprofessional response.
- Healthcare providers are bound by **patient confidentiality (HIPAA)**, and sharing this information without consent is unethical and illegal.
*If you don't consent to treatment, I'll be forced to obtain consent from your parents.*
- Since the patient is a **competent adult (age 22)**, his parents cannot give or withhold consent for his medical treatment.
- Parental consent is only required for **minors** or adults who have been legally declared **incompetent** through a court process.
*Have you ever felt you should cut down on your drinking?*
- While addressing alcohol use disorder is important, asking a **CAGE screening question** in this acute, high-stress situation is **inappropriate timing** and poor prioritization.
- The immediate priority is addressing the patient's **acute medical needs and impaired capacity**, not initiating a substance abuse screening.
Hernia complications US Medical PG Question 4: A 63-year-old man comes to the emergency department because of pain in his left groin for the past hour. The pain began soon after he returned from a walk. He describes it as 8 out of 10 in intensity and vomited once on the way to the hospital. He has had a swelling of the left groin for the past 2 months. He has chronic obstructive pulmonary disease and hypertension. Current medications include amlodipine, albuterol inhaler, and a salmeterol-fluticasone inhaler. He appears uncomfortable. His temperature is 37.4°C (99.3°F), pulse is 101/min, and blood pressure is 126/84 mm Hg. Examination shows a tender bulge on the left side above the inguinal ligament that extends into the left scrotum; lying down or applying external force does not reduce the swelling. Coughing does not make the swelling bulge further. There is no erythema. The abdomen is distended. Bowel sounds are hyperactive. Scattered rhonchi are heard throughout both lung fields. Which of the following is the most appropriate next step in management?
- A. Laparoscopic surgical repair
- B. Surgical drainage
- C. Antibiotic therapy
- D. Open surgical repair (Correct Answer)
- E. Surgical exploration of the testicle
Hernia complications Explanation: ***Open surgical repair***
- The patient presents with a **painful, non-reducible inguinal hernia** that has likely **incarcerated** or **strangulated**, given the acute onset of severe pain, vomiting, and abdominal distension with hyperactive bowel sounds.
- In cases of suspected incarceration or strangulation, **urgent open surgical repair** is indicated to prevent **bowel ischemia** and its serious complications (e.g., perforation, sepsis).
*Laparoscopic surgical repair*
- While laparoscopic repair is an option for elective hernia repair, it is generally **contraindicated** in cases of **incarcerated or strangulated hernias** due to the higher risk of bowel injury, inadequate assessment of bowel viability, and longer operative times in an emergency setting.
- Also, the patient's **COPD** might make him a less ideal candidate for laparoscopy due to the risks associated with pneumoperitoneum.
*Surgical drainage*
- Surgical drainage is typically performed for abscesses or fluid collections, which are **not the primary issue** in this presentation.
- A hernia involves displacement of organs, not an accumulation of fluid or pus requiring drainage.
*Antibiotic therapy*
- Although antibiotics might be considered as an adjunctive therapy if infection is suspected or confirmed (e.g., with bowel necrosis), they are **not the definitive primary treatment** for an incarcerated or strangulated hernia.
- The mechanical obstruction and potential ischemia require surgical intervention for resolution.
*Surgical exploration of the testicle*
- While the bulge extends into the scrotum, the primary concern is the **incarcerated hernia** itself.
- Surgical exploration of the testicle would be indicated for conditions like testicular torsion, epididymitis, or testicular masses, which are not suggested by the presented symptoms.
Hernia complications US Medical PG Question 5: A 5-year-old girl is brought to a medical office for evaluation of persistent abdominal pain that has worsened over the past 24 hours. The mother states that the girl often has constipation which has worsened over the last 3 days. The mother denies that the girl has had bloody stools. The girl has not had a bowel movement or passed flatulence in 72 hours. She has vomited 3 times since last night and refuses to eat. She has no significant medical history, including no history of surgeries. On exam, there are no abdominal masses; however, the upper abdomen is distended and tympanic. What is the most likely underlying cause of the girl’s symptoms?
- A. Duodenal atresia
- B. Malrotation of the gut (Correct Answer)
- C. Pyloric stenosis
- D. Meckel’s diverticulum
- E. Volvulus
Hernia complications Explanation: ***Malrotation of the gut***
- The question asks for the **underlying cause** of symptoms in a 5-year-old presenting with her **first episode** of acute bowel obstruction and **no prior surgical history**. **Malrotation** is the congenital anatomical abnormality that predisposes to **midgut volvulus**.
- **Malrotation** occurs when the bowel fails to rotate properly during fetal development, leaving the mesentery on a narrow pedicle. This anatomical defect is the underlying cause that makes volvulus possible.
- While volvulus (twisting) is the acute mechanical event causing obstruction, **malrotation is the underlying anatomical defect** being asked for in the question.
- The presentation of **abdominal pain**, **vomiting**, **abdominal distension**, inability to pass **flatus or stool** for 72 hours, and **tympanic upper abdomen** indicates acute bowel obstruction from midgut volvulus occurring on the background of malrotation.
*Volvulus*
- **Volvulus** (twisting of the bowel) is the **acute complication** that occurs, not the underlying cause.
- Volvulus is the mechanism of obstruction, but it occurs because of the underlying anatomical defect (malrotation).
- The question specifically asks for "underlying cause" - volvulus is the acute event, while malrotation is the predisposing anatomical abnormality.
*Duodenal atresia*
- **Duodenal atresia** is a congenital complete obstruction that presents in the **neonatal period** with vomiting (bilious), the classic "double bubble" sign, and feeding intolerance.
- This would have been diagnosed much earlier than 5 years of age and is not compatible with this presentation.
*Pyloric stenosis*
- **Pyloric stenosis** presents with **non-bilious projectile vomiting** in infants between **2 to 6 weeks of age**, not in a 5-year-old child.
- Physical exam classically reveals an **olive-shaped mass** in the epigastrium and visible gastric peristaltic waves.
*Meckel's diverticulum*
- **Meckel's diverticulum** most commonly presents with **painless rectal bleeding** (from ectopic gastric mucosa causing ulceration) following the "rule of 2s."
- While it can cause obstruction via intussusception or serve as a lead point, it is not the most likely underlying cause of this presentation in a 5-year-old with acute complete bowel obstruction and no prior symptoms.
Hernia complications US Medical PG Question 6: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Hernia complications Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
Hernia complications US Medical PG Question 7: A 72-year-old man presents to his primary care physician complaining of pain and bulging in his groin. He is otherwise healthy and has never had surgery. He is referred to a general surgeon, and is scheduled for an elective hernia repair the following week. On closer inspection in the operating room, the surgeon notes a hernia sac that protrudes medial to the inferior epigastric vessels through a weakness in the posterior wall of the inguinal canal. Which of the following accurately describes this patient's condition?
- A. Direct inguinal hernia (Correct Answer)
- B. Isolated rectus diastasis
- C. Direct incisional hernia
- D. Hiatal hernia
- E. Femoral hernia
Hernia complications Explanation: ***Direct inguinal hernia***
- This hernia protrudes directly through the **posterior wall of the inguinal canal** via Hesselbach's triangle (medial to the inferior epigastric vessels), rather than entering through the deep inguinal ring like an indirect hernia.
- They are more common in older men due to weakening of the abdominal wall and are acquired (not congenital).
*Isolated rectus diastasis*
- This is a **separation of the rectus abdominis muscles** at the linea alba, often presenting as a bulge in the midline of the abdomen.
- It is not a true hernia as it involves no fascial defect or protrusion through the abdominal wall, and the patient presents with a true hernia.
*Direct incisional hernia*
- An incisional hernia occurs at the site of a **previous surgical incision**, where the abdominal wall has been weakened.
- This patient has no history of prior surgery, ruling out an incisional hernia.
*Hiatal hernia*
- A hiatal hernia involves the **protrusion of the stomach through the esophageal hiatus** of the diaphragm into the chest cavity.
- Symptoms are typically gastrointestinal (e.g., GERD), and the bulge would be in the chest/abdomen, not the groin.
*Femoral hernia*
- A femoral hernia protrudes through the **femoral ring**, below the inguinal ligament, and is more common in women.
- The description of the hernia sac protruding medial to the inferior epigastric vessels through the posterior wall is characteristic of a direct inguinal hernia, not a femoral one.
Hernia complications US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Hernia complications Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Hernia complications US Medical PG Question 9: A 34-year-old man presents to the office for evaluation of a lesion on his upper arm that appeared a few months ago and has not healed. The patient appears healthful but has a history of cardiovascular disease. He states that his friend at the industrial ammunition factory where he works told him he should "get it looked at." The patient admits to some nausea, vomiting, and diarrhea over the past year, but he states that he "feels fine now." On physical examination, the lesion is an erythematous, scaly, ulcerated plaque on the flexor surface of his upper arm. The rest of the exam is within normal limits. What is the most likely diagnosis?
- A. Squamous cell carcinoma (SCC) (Correct Answer)
- B. Erythema multiforme
- C. Actinic keratosis
- D. Erysipelas
- E. Contact dermatitis
Hernia complications Explanation: ***Squamous cell carcinoma (SCC)***
- The patient's occupational exposure to chemicals at an **ammunition factory**, along with chronic non-healing, **ulcerated, scaly plaque**, raises suspicion for SCC, particularly **arsenic-induced SCC**.
- His history of vague **gastrointestinal symptoms** (nausea, vomiting, diarrhea) over the past year is also consistent with **chronic arsenic exposure**, which is a known carcinogen.
*Erythema multiforme*
- This is an **acute, self-limiting hypersensitivity reaction** to medications or infections, characterized by target lesions, not a chronic, non-healing ulcerated plaque.
- It would not typically present with a history of chronic GI symptoms related to occupational exposure.
*Actinic keratosis*
- This is a **precancerous lesion** caused by chronic sun exposure, typically presenting as a rough, scaly patch on sun-exposed areas.
- While it has malignant potential to transform into SCC, the description of an **ulcerated, non-healing lesion** with a history of probable chemical exposure makes SCC a more likely *current* diagnosis.
*Erysipelas*
- Erysipelas is a **superficial bacterial infection** of the skin characterized by a rapidly spreading, bright red, well-demarcated, and painful rash, often accompanied by fever and systemic symptoms.
- It would not manifest as a chronic, non-healing ulcerated plaque over several months.
*Contact dermatitis*
- This is an **inflammatory skin reaction** due to direct contact with an allergen or irritant, typically presenting as an itchy, erythematous rash with vesicles or papules.
- It would not typically result in a chronic, ulcerated, non-healing plaque and is not associated with the systemic symptoms or occupational exposure history presented.
Hernia complications US Medical PG Question 10: A 52-year-old man, with a history of alcoholism, presents with loss of appetite, abdominal pain, and fever for the past 24 hours. He says he consumed 12 beers and a bottle of vodka 2 days ago. He reports a 19-year history of alcoholism. His blood pressure is 100/70 mm Hg, pulse is 100/min, respirations are 20/min, and oxygen saturation is 99% on room air. Laboratory findings are significant for the following:
Sodium 137 mEq/L
Potassium 3.4 mEq/L
Alanine aminotransferase (ALT) 230 U/L
Aspartate aminotransferase (AST) 470 U/L
Which of the following histopathologic findings would most likely be found on a liver biopsy of this patient?
- A. Macronodular cirrhosis
- B. T-lymphocyte infiltration
- C. Periportal necrosis
- D. Cytoplasmic inclusion bodies with keratin (Correct Answer)
- E. Positive periodic acid-Schiff stain
Hernia complications Explanation: ***Cytoplasmic inclusion bodies with keratin***
- The patient's history of **heavy alcohol consumption**, acute presentation with fever, abdominal pain, and elevated **AST and ALT (AST:ALT ratio >2:1)**, are highly suggestive of **alcoholic hepatitis**.
- **Mallory bodies**, which are **cytoplasmic inclusions consisting of intermediate filaments (keratin)**, are a characteristic histopathologic finding in alcoholic hepatitis.
*Macronodular cirrhosis*
- While **alcoholic liver disease** can progress to cirrhosis, the acute presentation with fever and significant transaminase elevation points more towards **alcoholic hepatitis** rather than established macronodular cirrhosis as the primary acute event.
- **Macronodular cirrhosis** typically involves larger nodules of regenerating hepatocytes, but the *acute inflammatory changes* of alcoholic hepatitis are paramount in this presentation.
*T-lymphocyte infiltration*
- While some inflammatory cells are present in alcoholic hepatitis, **T-lymphocyte infiltration** is more characteristic of **chronic viral hepatitis** or **autoimmune hepatitis**.
- The liver injury in alcoholic hepatitis is primarily mediated by neutrophils and direct hepatotoxic effects of alcohol metabolites.
*Periportal necrosis*
- **Periportal necrosis** is more commonly seen in **viral hepatitis** or other forms of **acute hepatitis** where the inflammatory process is concentrated around the portal tracts.
- In alcoholic hepatitis, the damage is typically *centrilobular (zone 3)*, around the terminal hepatic venule, due to its hypoxic vulnerability and high cytochrome P450 activity.
*Positive periodic acid-Schiff stain*
- A **positive periodic acid-Schiff (PAS) stain** that is *diastase-resistant* is a characteristic finding in **alpha-1 antitrypsin deficiency**, a genetic disorder affecting the liver and lungs.
- This patient's clinical presentation and lab findings are inconsistent with alpha-1 antitrypsin deficiency and strongly point towards **alcoholic liver disease**.
More Hernia complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.