Gastric tumors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gastric tumors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gastric tumors US Medical PG Question 1: A 63-year-old man comes to the physician because of a 2-month history of progressive fatigue. He also has shortness of breath and palpitations, which worsen on physical exertion and improve with rest. He has had intermittent constipation, low-grade fever, and generalized myalgia for the past 3 months. He has had a 10.4-kg (23-lb) weight loss over the past 4 months despite no change in appetite. His temperature is 37°C (98.6°F), pulse is 108/min, respirations are 16/min, and blood pressure is 130/78 mm Hg. Examination shows pale conjunctivae. His hemoglobin concentration is 9.1 g/dL, mean corpuscular volume is 70 μm3, and serum ferritin is 12 ng/mL. Test of the stool for occult blood is positive. Colonoscopy shows a 1.7-cm wide exophytic ulcer with irregular, bleeding edges in the ascending colon. Which of the following biopsy findings would have been the greatest predisposing factor for developing this patient's current condition?
- A. A pedunculated inflammatory polyp
- B. A villous adenomatous polyp (Correct Answer)
- C. A serrated hyperplastic polyp
- D. A submucosal lipomatous polyp
- E. A tubular adenomatous polyp
Gastric tumors Explanation: ***A villous adenomatous polyp***
- Villous adenomas are **predisposed to malignant transformation** due to their large size, increased cellular atypia, and high-grade dysplasia.
- The patient's presentation with **iron-deficiency anemia**, weight loss, and a bleeding colonic ulcer is highly suggestive of **colorectal adenocarcinoma**, which often arises from adenomatous polyps.
*A pedunculated inflammatory polyp*
- Inflammatory polyps are typically **non-neoplastic** and develop in response to chronic inflammation, such as in inflammatory bowel disease.
- They have **minimal to no malignant potential** and are not a significant risk factor for colorectal cancer.
*A serrated hyperplastic polyp*
- Hyperplastic polyps are generally **benign** and have a very low risk of malignant transformation, especially if small and located in the rectosigmoid colon.
- While serrated polyps (including sessile serrated adenomas) can progress to cancer via the **serrated pathway**, hyperplastic polyps specifically are largely considered harmless.
*A submucosal lipomatous polyp*
- Lipomas are **benign tumors** composed of mature adipose tissue that arise in the submucosa.
- They are **non-neoplastic** and have no malignant potential, thus not contributing to cancer development.
*A tubular adenomatous polyp*
- Tubular adenomas are adenomatous polyps with malignant potential, but **villous adenomas have a higher risk** of progression to adenocarcinoma.
- The presence of symptoms such as anemia and weight loss, along with the description of a bleeding ulcer, points to a more advanced lesion, which is more characteristic of a villous component or an already transformed malignancy.
Gastric tumors US Medical PG Question 2: A 62-year-old man presents to his primary care physician because of abdominal pain that started after he went camping several months ago and drank from a mountain stream. This past year, he also went on a trip around the world, eating local foods at each stop. Furthermore, he has had a history of cholelithiasis and had his gallbladder removed 3 years ago. Otherwise, his medical history is significant for well-controlled hypertension and diabetes. Based on clinical suspicion, an endoscopy and biopsy was performed showing a mix of mononuclear cells and a motile, urease-positive, oxidase-positive, spiral shaped organism. The changes seen on biopsy in this patient most likely predispose him to which of the following pathologies?
- A. Gallbladder adenocarcinoma
- B. Esophageal adenocarcinoma
- C. Colon adenocarcinoma
- D. MALT lymphoma (Correct Answer)
- E. Pancreatic adenocarcinoma
Gastric tumors Explanation: ***MALT lymphoma***
- The description of a **motile, urease-positive, oxidase-positive, spiral-shaped organism** from an endoscopic biopsy points to **Helicobacter pylori** infection.
- **H. pylori** infection chronic gastritis is a significant risk factor for the development of **MALT (Mucosa-Associated Lymphoid Tissue) lymphoma** of the stomach.
*Gallbladder adenocarcinoma*
- This is primarily associated with chronic inflammation of the gallbladder, often due to **cholelithiasis**, but the patient's gallbladder was removed.
- There is no direct link between **H. pylori infection** of the stomach and gallbladder adenocarcinoma.
*Esophageal adenocarcinoma*
- This is predominantly linked to **Barrett's esophagus**, which is caused by chronic **gastroesophageal reflux disease (GERD)**.
- While H. pylori can sometimes be associated with GERD, it's not a primary direct cause of esophageal adenocarcinoma.
*Colon adenocarcinoma*
- This is primarily associated with genetic predispositions like **familial adenomatous polyposis** or **Lynch syndrome**, as well as environmental factors like diet and inflammatory bowel disease.
- There is no direct causal link between **H. pylori** infection and colon adenocarcinoma.
*Pancreatic adenocarcinoma*
- Risk factors for pancreatic cancer include **smoking, obesity, chronic pancreatitis, and certain genetic syndromes**.
- There is no established direct link between **H. pylori infection** and pancreatic adenocarcinoma.
Gastric tumors US Medical PG Question 3: A 41-year-old male who takes NSAIDs regularly for his chronic back pain develops severe abdominal pain worse with eating. Upper endoscopy is performed and the medical student asks the supervising physician how the histological differentiation between a gastric ulcer and erosion is made. Which of the following layers of the gastric mucosa MUST be breached for a lesion to be considered an ulcer?
- A. Epithelium, lamina propria
- B. Epithelium
- C. Epithelium, lamina propria, muscularis mucosa (Correct Answer)
- D. Epithelium, lamina propria, muscularis mucosa, submucosa, and adventitia
- E. Epithelium, lamina propria, muscularis mucosa, and submucosa
Gastric tumors Explanation: ***Epithelium, lamina propria, muscularis mucosa***
- A **gastric ulcer** by definition involves a breach of the **entire mucosal thickness**, meaning the lesion extends through the muscularis mucosa.
- This deep penetration distinguishes an ulcer from an erosion, which is a more superficial lesion confined to the epithelium and lamina propria.
*Epithelium, lamina propria*
- This describes an **erosion**, a superficial lesion of the gastric mucosa that does not penetrate the **muscularis mucosa**.
- While erosions can cause symptoms, they are generally less severe and have a lower risk of complications like perforation compared to ulcers.
*Epithelium*
- A lesion confined solely to the **epithelium** would be considered a very superficial mucosal injury, often referred to as an **erosion** or sometimes a **superficial abrasion**.
- This degree of injury does not meet the criteria for either an erosion or an ulcer in a histological context.
*Epithelium, lamina propria, muscularis mucosa, submucosa, and adventitia*
- Penetration through the **submucosa** means the ulcer has become a **deep ulcer** or potentially a **perforating ulcer**, if it breaches the entire wall to the adventitia (serosa in the GI tract).
- While an ulcer *can* extend to these layers, only reaching the muscularis mucosa is the *minimum* requirement to be classified as an ulcer.
*Epithelium, lamina propria, muscularis mucosa, and submucosa*
- An ulcer that extends into the **submucosa** is indeed a true ulcer and a more severe one, but the defining histological feature separating an erosion from an ulcer is the breach of the **muscularis mucosa**.
- Therefore, reaching the submucosa is beyond the *minimum* requirement for an ulcer classification.
Gastric tumors US Medical PG Question 4: A 53-year-old man comes to the physician because of fatigue, recurrent diarrhea, and an 8-kg (17.6-lb) weight loss over the past 6 months. He has a 4-month history of recurrent blistering rashes on different parts of his body that grow and develop into pruritic, crusty lesions before resolving spontaneously. Physical examination shows scaly lesions in different phases of healing with central, bronze-colored induration around the mouth, perineum, and lower extremities. Laboratory studies show:
Hemoglobin 10.1 mg/dL
Mean corpuscular volume 85 μm3
Mean corpuscular hemoglobin 30.0 pg/cell
Serum
Glucose 236 mg/dL
Abdominal ultrasonography shows a 3-cm, solid mass located in the upper abdomen. This patient's mass is most likely derived from which of the following types of cells?
- A. Gastrointestinal enterochromaffin cells
- B. Pancreatic β-cells
- C. Pancreatic δ-cells
- D. Pancreatic α-cells (Correct Answer)
- E. Gastric G-cells
Gastric tumors Explanation: ***Pancreatic α-cells***
- The patient's symptoms of **fatigue, recurrent diarrhea, weight loss, blistering rash (necrolytic migratory erythema)**, and **hyperglycemia** are classic features of a **glucagonoma**.
- A **glucagonoma** is a tumor of the pancreatic α-cells that **secretes excessive glucagon**, leading to these characteristic signs and symptoms, supported by the presence of an **upper abdominal mass**.
*Gastrointestinal enterochromaffin cells*
- Tumors of gastrointestinal enterochromaffin cells (carcinoid tumors) typically produce **serotonin** and present with flushing, diarrhea, bronchospasm, and valvular heart disease, not the skin rash or hyperglycemia seen here.
- While carcinoid tumors can cause diarrhea, the additional symptoms of **necrolytic migratory erythema** and **diabetes** are not characteristic.
*Pancreatic β-cells*
- Tumors of pancreatic β-cells (**insulinomas**) produce excessive insulin, leading to **hypoglycemia**, not the hyperglycemia observed in this patient.
- Insulinomas cause symptoms like sweating, tremors, confusion, and palpitations, which are inconsistent with the patient's presentation.
*Pancreatic δ-cells*
- Pancreatic δ-cell tumors (**somatostatinomas**) secrete **somatostatin**, which can cause **diabetes mellitus**, steatorrhea, and gallstones.
- While diabetes is present, the characteristic **necrolytic migratory erythema** and severe diarrhea are less common with somatostatinomas.
*Gastric G-cells*
- Tumors of gastric G-cells (**gastrinomas**) secrete **gastrin**, leading to **Zollinger-Ellison syndrome**, characterized by severe peptic ulcers, abdominal pain, and chronic diarrhea.
- Gastrinomas do not typically cause **necrolytic migratory erythema** or significant hyperglycemia.
Gastric tumors US Medical PG Question 5: A 40-year-old female comes in with several months of unintentional weight loss, epigastric pain, and a sensation of abdominal pressure. She has diabetes well-controlled on metformin but no other prior medical history. She has not previously had any surgeries. On physical exam, her doctor notices brown velvety areas of pigmentation on her neck. Her doctor also notices an enlarged, left supraclavicular node. Endoscopic findings show a stomach wall that appears to be grossly thickened. Which of the following findings would most likely be seen on biopsy?
- A. Keratin pearls
- B. Noncaseating granulomas
- C. Peyer's patches
- D. Psammoma bodies
- E. Cells with central mucin pool (Correct Answer)
Gastric tumors Explanation: ***Cells with central mucin pool***
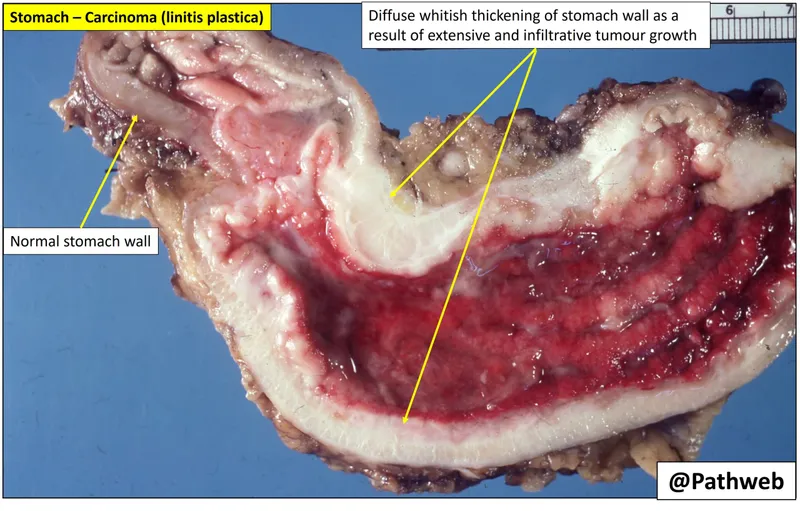
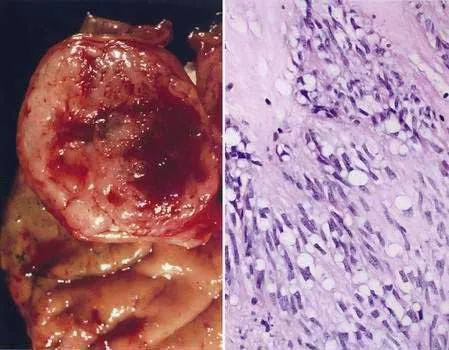
- The patient's symptoms (unintentional weight loss, epigastric pain, abdominal pressure, **acanthosis nigricans**, and a **Virchow node**) are highly suggestive of **gastric adenocarcinoma**, particularly the **diffuse type**.
- **Signet ring cells**, characterized by a **large central mucin vacuole** that displaces the nucleus to the periphery, are pathognomonic for **diffuse gastric adenocarcinoma**.
*Keratin pearls*
- **Keratin pearls** are a hallmark feature of **squamous cell carcinoma**, which is a type of cancer arising from squamous epithelial cells.
- While squamous cell carcinoma can occur in the esophagus, it is an extremely rare finding in the stomach, which is lined by glandular epithelium.
*Noncaseating granulomas*
- **Noncaseating granulomas** are characteristic of conditions like **Crohn's disease** or **sarcoidosis**.
- These conditions do not typically present with the described aggressive features of gastric malignancy or the presence of acanthosis nigricans and a Virchow node.
*Peyer's patches*
- **Peyer's patches** are normal lymphoid structures found in the **ileum** of the small intestine, playing a role in immune surveillance.
- Their presence in a biopsy would indicate normal small intestinal tissue, not a malignant gastric lesion.
*Psammoma bodies*
- **Psammoma bodies** are concentric, laminated calcified structures typically seen in certain types of **cancers with serous or papillary differentiation**, such as **papillary thyroid carcinoma**, **meningioma**, and **serous ovarian carcinoma**.
- They are not a characteristic finding in gastric adenocarcinoma.
Gastric tumors US Medical PG Question 6: A 61-year-old man comes to the physician because of a 6-month history of epigastric pain and a 9-kg (20-lb) weight loss. He feels full and bloated even after eating small portions of food. His hemoglobin concentration is 9.5 g/dL with a mean corpuscular volume of 78 μm3. Test of the stool for occult blood is positive. Esophagogastroduodenoscopy shows a 2-cm raised lesion with central ulceration on the lesser curvature of the stomach. Histologic examination of a gastric biopsy specimen from the lesion is most likely to show which of the following?
- A. Mucin-filled round cells
- B. Gland-forming cuboidal cells (Correct Answer)
- C. Neutrophilic infiltration with pit abscesses
- D. Lymphocytic aggregates with noncaseating granulomas
- E. Foveolar and smooth muscle hyperplasia
Gastric tumors Explanation: ***Gland-forming cuboidal cells***
- The patient's symptoms (epigastric pain, weight loss, early satiety, anemia, and positive occult blood in stool) along with the endoscopic finding of a raised, ulcerated lesion on the lesser curvature are highly suggestive of **gastric adenocarcinoma**.
- Gastric adenocarcinoma is characterized histologically by **malignant glandular proliferation** with cuboidal or columnar cells forming irregular glands, often with varying degrees of differentiation.
*Mucin-filled round cells*
- This description is characteristic of **signet-ring cell carcinoma**, a specific poorly differentiated subtype of gastric adenocarcinoma.
- While signet-ring cells are a type of gastric cancer, the more general and common histological pattern for gastric adenocarcinoma involves **glandular formation** by cuboidal or columnar cells, making the gland-forming option a broader and typically more direct answer for gastric adenocarcinoma unless specified as diffuse type.
*Neutrophilic infiltration with pit abscesses*
- This histological pattern is indicative of **acute gastritis** or **H. pylori infection**.
- While *H. pylori* is a risk factor for gastric cancer, these findings are not consistent with a malignant tumor presenting with significant weight loss and a mass.
*Lymphocytic aggregates with noncaseating granulomas*
- This finding is characteristic of **Crohn's disease** or other **granulomatous conditions**, not gastric cancer.
- Noncaseating granulomas are not typically seen in gastric adenocarcinoma.
*Foveolar and smooth muscle hyperplasia*
- This describes a **hyperplastic gastric polyp** or a **Menetrier's disease**-like pattern (giant rugal hypertrophy).
- While these conditions can be associated with gastric symptoms, they are not typically malignant lesions causing significant weight loss and a distinct ulcerated mass, as seen in this patient.
Gastric tumors US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Gastric tumors Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Gastric tumors US Medical PG Question 8: A 51-year-old woman comes to the physician because of a persistent cough and a 5-kg (11-lb) weight loss over the past 2 months. Yesterday, she coughed up bloody sputum. She does not smoke. Pulmonary examination shows decreased breath sounds over the right upper lobe. A CT scan of the chest shows a mass in the periphery of the right upper lobe. Histopathologic examination of a specimen obtained on CT-guided biopsy shows glandular cells with papillary components and signet ring cells that stain positive for mucin. An alteration in which of the following genes is most likely to have occurred in this patient?
- A. TP53
- B. SMAD4 (DPC4)
- C. APC
- D. MYCL1
- E. ALK (Correct Answer)
Gastric tumors Explanation: ***ALK***
- The patient's presentation with **adenocarcinoma** (glandular cells, mucin, peripheral location) in a **non-smoker** suggests a higher likelihood of specific driver mutations, such as **ALK rearrangements**.
- **ALK gene rearrangements** are characteristic oncogenic drivers in a subset of lung adenocarcinomas, particularly in younger patients and non-smokers.
*TP53*
- **TP53** is a tumor suppressor gene frequently mutated in many cancers, including lung cancer, but its mutation is not as specific to the clinical and histopathological findings of this patient's adenocarcinoma presenting in a non-smoker.
- While common in lung cancer overall, **TP53 mutations** are more strongly associated with squamous cell carcinoma or small cell lung cancer, or with smoking-related adenocarcinoma.
*SMAD4 (DPC4)*
- **SMAD4** is a tumor suppressor gene primarily associated with **pancreatic cancer** and **colorectal cancer**, playing a key role in the TGF-β signaling pathway.
- Its mutation is not a common or characteristic driver in lung adenocarcinoma, especially with the features described.
*APC*
- The **APC gene** is a tumor suppressor gene centrally involved in the **Wnt signaling pathway** and is primarily associated with **colorectal cancer**, particularly **familial adenomatous polyposis**.
- APC mutations are not typically found as primary drivers in lung adenocarcinoma.
*MYCL1*
- **MYCL1 (L-MYC)** is an oncogene belonging to the MYC family, implicated in cell proliferation and apoptosis.
- While MYC family genes can be amplified in various cancers, **MYCL1 amplification** is more characteristic of **small cell lung cancer**, not adenocarcinoma, and does not align with the glandular and papillary features described.
Gastric tumors US Medical PG Question 9: A 75-year-old man comes to his primary care physician because he has been having diarrhea and difficulty breathing. The diarrhea has been intermittent with frequent watery stools that occur along with abdominal cramps. Furthermore, the skin on his face and upper chest feels hot and changes color in episodes lasting from a few minutes to hours. Finally, the patient complains of loss of appetite and says that he has unexpectedly lost 20 pounds over the last two months. Based on clinical suspicion, magnetic resonance imaging is obtained showing a small mass in this patient's lungs. Which of the following is associated with the most likely cause of this patient's symptoms?
- A. It also arises in the GI tract (Correct Answer)
- B. Stains positive for vimentin
- C. Has keratin pearls and intercellular bridges
- D. Most common lung cancer in non-smokers and females
- E. Contains psammoma bodies
Gastric tumors Explanation: ***Correct: It also arises in the GI tract***
- The patient's symptoms (diarrhea, flushing, difficulty breathing, weight loss) are highly suggestive of **carcinoid syndrome**, often caused by a **neuroendocrine tumor (NET)** in the lung or gastrointestinal tract that metastasizes to the liver.
- While a lung mass is identified here, **carcinoid tumors** (a type of NET) most commonly originate in the **gastrointestinal tract** (especially the appendix, small intestine, and rectum), making this option strongly associated with the likely cause.
- Carcinoid syndrome typically occurs when liver metastases allow serotonin and other vasoactive substances to bypass hepatic metabolism and enter systemic circulation.
*Incorrect: Stains positive for vimentin*
- **Vimentin** is an intermediate filament typically found in **mesenchymal cells** and is often positive in sarcomas, lymphomas, and melanomas.
- Neuroendocrine tumors, including carcinoid, typically stain positive for **chromogranin** and **synaptophysin**, not vimentin.
*Incorrect: Has keratin pearls and intercellular bridges*
- **Keratin pearls** and **intercellular bridges** are characteristic histological features of **squamous cell carcinoma**, which is a type of non-small cell lung cancer.
- While the patient has a lung mass, his symptoms of carcinoid syndrome point away from squamous cell carcinoma and towards a neuroendocrine tumor.
*Incorrect: Most common lung cancer in non-smokers and females*
- **Adenocarcinoma** is the most common type of lung cancer, particularly prevalent in non-smokers and females.
- However, adenocarcinoma does not typically cause carcinoid syndrome, which is a key clinical presentation in this case.
*Incorrect: Contains psammoma bodies*
- **Psammoma bodies** are concentric, laminated calcified structures seen in certain tumors, such as papillary thyroid carcinoma, meningioma, and serous papillary ovarian cancer.
- They are not characteristic features of neuroendocrine tumors or carcinoid tumors.
Gastric tumors US Medical PG Question 10: A 54-year-old woman comes to the physician because of a painful skin lesion on her right leg for 1 month. It initially started out as a small red spot but has rapidly increased in size during this period. She remembers an ant bite on her leg prior to the lesion occurring. She was treated for anterior uveitis 8 months ago with corticosteroids. She has Crohn's disease, type 2 diabetes mellitus, and hypertension. Current medications include insulin, mesalamine, enalapril, and aspirin. She returned from Wisconsin after visiting her son 2 months ago. Her temperature is 37.6°C (98°F), pulse is 98/min, and blood pressure is 126/88 mm Hg. Examination shows pitting pedal edema of the lower extremities. There is a 4-cm tender ulcerative lesion on the anterior right leg with a central necrotic base and purplish irregular borders. There are dilated tortuous veins in both lower legs. Femoral and pedal pulses are palpated bilaterally. Which of the following is the most likely diagnosis?
- A. Pyoderma gangrenosum (Correct Answer)
- B. Basal cell carcinoma
- C. Squamous cell carcinoma
- D. Ecthyma gangrenosum
- E. Blastomycosis
Gastric tumors Explanation: ***Pyoderma gangrenosum***
- The patient's history of **Crohn's disease**, **anterior uveitis**, and a rapidly progressing, **tender ulcerative lesion** with a **necrotic base** and **purplish irregular borders** are highly characteristic of pyoderma gangrenosum.
- The phenomenon of **pathergy** (exacerbation of lesions after minor trauma like a bug bite) further supports this diagnosis.
*Basal cell carcinoma*
- Typically presents as a **slow-growing lesion** with **pearly borders** and **telangiectasias**, not a rapidly enlarging, tender ulcer with a necrotic base.
- It is often associated with sun exposure and rarely presents with the systemic associations seen in this case.
*Squamous cell carcinoma*
- Usually appears as a **scaly, erythematous patch** or an **indurated nodule** that may ulcerate, but it is generally a chronic lesion and less acutely painful or rapidly progressing.
- While it can be aggressive, the clinical presentation and rapid progression with a necrotic center and systemic associations point away from this diagnosis.
*Ecthyma gangrenosum*
- This condition is caused by **Pseudomonas aeruginosa bacteremia** and is characterized by a central necrotic area surrounded by an erythematous halo, typically in immunocompromised patients.
- While there is some overlap in appearance, ecthyma gangrenosum is usually associated with **sepsis** and systemic signs of infection, which are not prominent here.
*Blastomycosis*
- A **fungal infection** endemic to the Great Lakes region (including Wisconsin), which can cause skin lesions that may be verrucous, ulcerative, or plaque-like.
- However, the description of a rapidly progressing, deeply ulcerative lesion with purplish, undermined borders and strong association with inflammatory bowel disease is more consistent with pyoderma gangrenosum.
More Gastric tumors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.