Esophageal pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Esophageal pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Esophageal pathology US Medical PG Question 1: A 23-year-old college senior visits the university health clinic after vomiting large amounts of blood. He has been vomiting for the past 36 hours after celebrating his team’s win at the national hockey championship with his varsity friends while consuming copious amounts of alcohol. His personal medical history is unremarkable. His blood pressure is 129/89 mm Hg while supine and 100/70 mm Hg while standing. His pulse is 98/min, strong and regular, with an oxygen saturation of 98%. His body temperature is 36.5°C (97.7°F), while the rest of the physical exam is normal. Which of the following is associated with this patient’s condition?
- A. Esophageal tear (Correct Answer)
- B. Portal hypertension
- C. Esophageal metaplasia
- D. Esophageal varices
- E. Esophageal perforation
Esophageal pathology Explanation: ***Esophageal tear***
- This patient's presentation of **hematemesis** after prolonged, forceful vomiting, especially following substantial alcohol consumption, is highly characteristic of a **Mallory-Weiss tear**.
- A Mallory-Weiss tear is a **longitudinal mucosal laceration** at the gastroesophageal junction, caused by the sudden increase in **intra-abdominal and intra-gastric pressure** during retching or vomiting.
*Portal hypertension*
- While portal hypertension can lead to upper GI bleeding from **esophageal varices**, there is no clinical evidence of **chronic liver disease** (e.g., jaundice, ascites, spider angiomata) in this otherwise healthy young man.
- The patient's unremarkable medical history and acute onset of symptoms after an episode of severe vomiting are not typical for a new presentation of chronic **portal hypertension**.
*Esophageal metaplasia*
- **Esophageal metaplasia (Barrett's esophagus)** is a change in the lining of the esophagus from squamous to columnar epithelium, usually due to chronic gastroesophageal reflux disease (GERD).
- It is an asymptomatic precursor to adenocarcinoma and does not cause acute, massive hematemesis without associated ulceration or malignancy.
*Esophageal varices*
- **Esophageal varices** are dilated veins in the lower esophagus that can rupture and cause life-threatening bleeding, typically due to **portal hypertension** from cirrhosis or other liver diseases.
- The patient's lack of a history of liver disease and the context of excessive vomiting make variceal bleeding less likely than a Mallory-Weiss tear.
*Esophageal perforation*
- **Esophageal perforation (Boerhaave syndrome)** is a transmural tear of the esophagus, also associated with severe vomiting, but it presents with more severe symptoms.
- Key differentiating features include **severe retrosternal chest pain**, **dyspnea**, **subcutaneous emphysema**, and potentially **septic shock** due to mediastinitis, none of which are described in this patient.
Esophageal pathology US Medical PG Question 2: A 62-year-old man is referred to a gastroenterologist because of difficulty swallowing for the past 5 months. He has difficulty swallowing both solid and liquid foods, but there is no associated pain. He denies any shortness of breath or swelling in his legs. He immigrated from South America 10 years ago. He is a non-smoker and does not drink alcohol. His physical examination is unremarkable. A barium swallow study was ordered and the result is given below. Esophageal manometry confirms the diagnosis. What is the most likely underlying cause of this patient’s condition?
- A. Pharyngoesophageal diverticulum
- B. Chagas disease (Correct Answer)
- C. Esophageal rupture
- D. Gastroesophageal reflux disease
- E. Squamous cell carcinoma of the esophagus
Esophageal pathology Explanation: ***Chagas disease***
- The patient's history of living in **South America** and presenting with **dysphagia for both solids and liquids** (suggesting a motility disorder), along with the **barium swallow image showing esophageal dilation and a 'bird's beak' appearance** at the gastroesophageal junction, are highly characteristic of achalasia caused by Chagas disease.
- Chagas disease, caused by *Trypanosoma cruzi*, leads to the destruction of **myenteric plexus neurons** in the esophagus, resulting in achalasia (failure of the lower esophageal sphincter to relax) and megaesophagus.
*Pharyngoesophageal diverticulum*
- This typically presents as **Zenker's diverticulum**, causing **difficulty initiating a swallow**, regurgitation of undigested food, and sometimes halitosis, which is different from the described dysphagia for both solids and liquids.
- A Zenker's diverticulum would appear as a **pouch-like protrusion** in the posterior pharynx, not the diffuse esophageal dilation seen in the image.
*Esophageal rupture*
- Esophageal rupture (Boerhaave syndrome) is an acute, life-threatening condition associated with **severe chest pain, vomiting, and crepitus**, not a chronic, progressive dysphagia without pain.
- Imaging would reveal **extravasation of contrast** into the mediastinum or pleural space, not the smooth dilation and distal narrowing observed.
*Gastroesophageal reflux disease*
- While chronic GERD can lead to **strictures** and dysphagia, it typically causes **heartburn**, regurgitation, and sometimes odynophagia, and the dysphagia is usually progressive for solids first.
- The barium swallow would show reflux or a stricture, not the **classic achalasia findings** of a dilated esophagus tapering to a narrow distal segment.
*Squamous cell carcinoma of the esophagus*
- Squamous cell carcinoma usually presents with **progressive dysphagia, initially for solids**, and is often associated with weight loss, smoking, and alcohol use, none of which are present in this patient.
- A tumor would typically appear as an **irregular, focal narrowing or mass** on barium swallow, not the smooth, diffuse dilation seen in this image.
Esophageal pathology US Medical PG Question 3: A 25-year-old man presents to the emergency department after numerous episodes of vomiting. The patient states that he thinks he ‘ate something weird’ and has been vomiting for the past 48 hours. He says that he came to the hospital because the last few times he "threw up blood". He is hypotensive with a blood pressure of 90/55 mm Hg and a pulse of 120/min. After opening an intravenous line, a physical examination is performed which is normal except for mild epigastric tenderness. An immediate endoscopy is performed and a tear involving the mucosa and submucosa of the gastroesophageal junction is visualized. Which of the following is the most likely diagnosis?
- A. Mallory-Weiss tear (Correct Answer)
- B. Hiatal hernia
- C. Esophageal varices
- D. Boerhaave syndrome
- E. Gastric ulcer
Esophageal pathology Explanation: ***Mallory-Weiss tear***
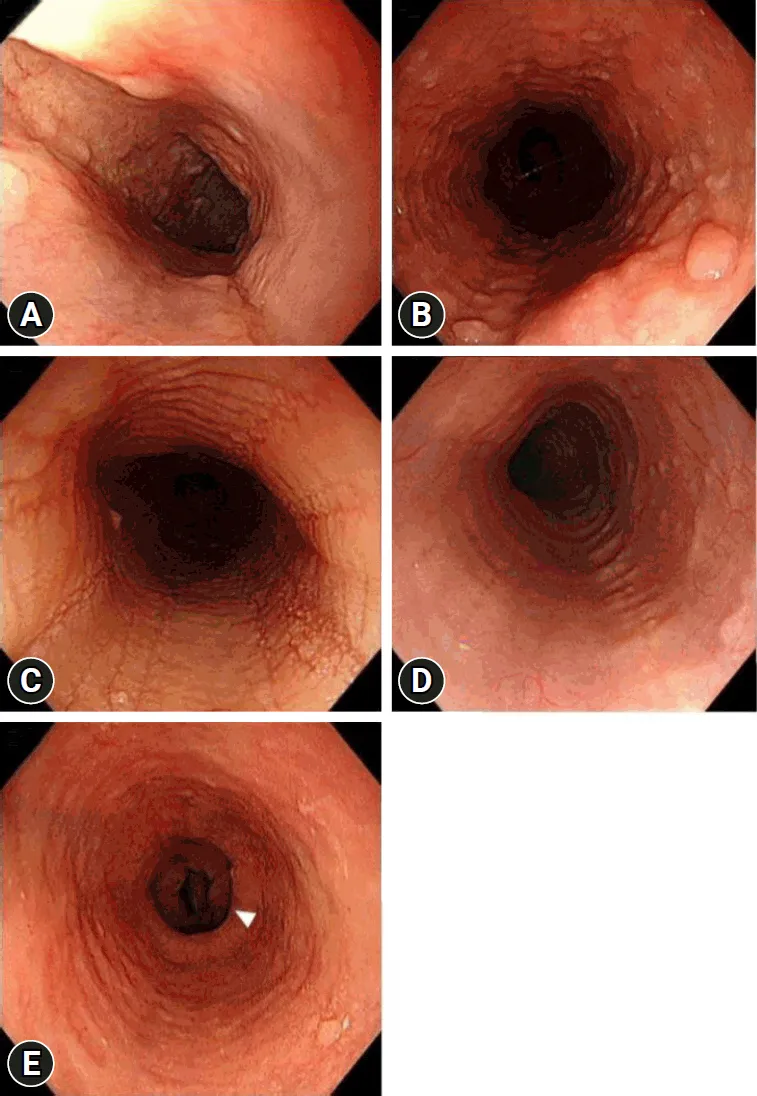
- The patient's history of **repeated vomiting** followed by **hematemesis** is hallmark for a Mallory-Weiss tear. The endoscopic finding of a **mucosal and submucosal tear at the gastroesophageal junction** confirms this diagnosis.
- This condition is often precipitated by events that cause a sudden increase in intra-abdominal pressure, such as forceful retching or vomiting, leading to a linear tear.
*Hiatal hernia*
- A hiatal hernia involves the **protrusion of the stomach through the esophageal hiatus of the diaphragm** and would not typically cause acute hematemesis from a tear.
- While it can be associated with gastroesophageal reflux, it does not directly explain sudden-onset bleeding after vomiting.
*Esophageal varices*
- Esophageal varices are **dilated veins in the lower esophagus** usually due to **portal hypertension**, often seen in patients with liver cirrhosis.
- While varices can cause significant upper gastrointestinal bleeding, the endoscopy here reveals a tear, not ruptured varices, and there is no mention of underlying liver disease.
*Boerhaave syndrome*
- Boerhaave syndrome is a **transmural rupture of the esophagus** following forceful vomiting, which is a much more severe condition than a Mallory-Weiss tear.
- It would typically present with **severe chest pain**, **crepitus**, and signs of **mediastinitis** or **pleural effusion** due to esophageal contents leaking into the mediastinum, none of which are described here.
*Gastric ulcer*
- A gastric ulcer is an **erosion in the stomach lining** that can cause bleeding.
- While it can cause hematemesis, the endoscopic finding of a tear specifically at the **gastroesophageal junction** points away from a sole gastric ulcer as the cause.
Esophageal pathology US Medical PG Question 4: A 45-year-old man comes to the physician for the evaluation of painful swallowing and retrosternal pain over the past 2 days. He was recently diagnosed with HIV infection, for which he now takes tenofovir, emtricitabine, and raltegravir. There is no family history of serious illness. He has smoked one pack of cigarettes daily for the past 20 years. He drinks 2–3 beers per day. He does not use illicit drugs. Vital signs are within normal limits. Physical examination of the oral cavity shows no abnormalities. The patient's CD4+ T-lymphocyte count is 80/mm3 (normal ≥ 500). Empiric treatment is started. Two weeks later, he reports no improvement in his symptoms. Esophagogastroduodenoscopy is performed and shows multiple well-circumscribed, round, superficial ulcers in the upper esophagus. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Degeneration of inhibitory neurons within the myenteric plexuses
- B. Infection with cytomegalovirus
- C. Infection with herpes simplex virus (Correct Answer)
- D. Transient lower esophageal sphincter relaxation
- E. Allergic inflammation of the esophagus
Esophageal pathology Explanation: ***Infection with herpes simplex virus***
- The patient's **HIV infection** and **low CD4+ T-lymphocyte count (80/mm3)** indicate severe immunosuppression, making him highly susceptible to opportunistic infections like HSV esophagitis.
- The EGD findings of **multiple well-circumscribed, round, superficial ulcers** predominantly in the **upper esophagus** are classic endoscopic features of HSV esophagitis.
*Degeneration of inhibitory neurons within the myenteric plexuses*
- This condition, known as **achalasia**, typically presents with **dysphagia for both liquids and solids**, regurgitation, and chest pain, which can be confused with retrosternal pain.
- However, achalasia does not typically cause **ulcers in the esophagus** and is not primarily linked to HIV or immunosuppression.
*Infection with cytomegalovirus*
- While CMV esophagitis can occur in immunosuppressed patients and cause odynophagia and retrosternal pain, the ulcers are typically **linear**, **serpiginous**, or **giant** and located more commonly in the **distal esophagus**, unlike the round, superficial ulcers seen here.
- CMV infection often presents with other systemic symptoms like fever, fatigue, and leukopenia, which are not mentioned in this case.
*Transient lower esophageal sphincter relaxation*
- This is a common mechanism contributing to **gastroesophageal reflux disease (GERD)**, which can cause retrosternal pain and dysphagia due to esophageal strictures or erosions.
- However, GERD typically causes **diffuse inflammation** and **erosions** rather than discrete, well-circumscribed ulcers, and it's not directly linked to the patient's immunosuppressed state.
*Allergic inflammation of the esophagus*
- This describes **eosinophilic esophagitis (EoE)**, which presents with dysphagia and food impaction, especially in younger individuals or those with other atopic conditions.
- Endoscopy in EoE often shows **trachealization** (concentric rings), **linear furrows**, or **white exudates**, not well-circumscribed ulcers, and it's not associated with HIV infection or severe immunosuppression.
Esophageal pathology US Medical PG Question 5: An 85-year-old man who recently immigrated to the US from Spain presents to your office complaining of hoarseness and dysphagia for the past 2 months. He says his symptoms have been getting progressively worse, and he expresses concerns about the difficulty swallowing as he cannot eat well and has even lost 9 kg (20 lb) since his last visit 3 months ago. He denies any shortness of breath, coughing of blood, and chest pain. His bowel and bladder habit are normal. Past medical history is unremarkable. He has a 60-pack-year history of smoking tobacco and drinks alcohol occasionally. Which of the following is the most likely cause of his symptoms?
- A. Malignant proliferation of squamous cells (Correct Answer)
- B. Transformation leading to metaplasia in the lower esophagus
- C. Chronic autoimmune gastritis
- D. Malignant proliferation of glandular tissue in the esophagus
- E. Reduced lower esophageal pressure
Esophageal pathology Explanation: ***Malignant proliferation of squamous cells***
- The patient's presentation with **progressive hoarseness, dysphagia, and significant weight loss** in an 85-year-old male with a significant **60-pack-year smoking history** strongly suggests **squamous cell carcinoma of the esophagus or larynx/pharynx**.
- **Tobacco and alcohol use** are major risk factors for squamous cell carcinoma of the upper aerodigestive tract, and his symptoms align with advanced disease.
*Transformation leading to metaplasia in the lower esophagus*
- This describes **Barrett's esophagus**, a metaplastic change from squamous to columnar epithelium in the lower esophagus, usually due to **chronic gastroesophageal reflux disease (GERD)**.
- While Barrett's esophagus can progress to **adenocarcinoma** (with smoking as an additional risk factor), the primary presentation here with **hoarseness** strongly suggests squamous cell carcinoma of the upper aerodigestive tract rather than adenocarcinoma of the distal esophagus.
*Chronic autoimmune gastritis*
- This condition primarily affects the **stomach**, leading to **vitamin B12 deficiency** and megaloblastic anemia, and generally does not cause hoarseness or dysphagia as primary symptoms.
- The patient's symptoms are localized to the throat and esophagus, with systemic signs of disease progression (weight loss), rather than gastric issues.
*Malignant proliferation of glandular tissue in the esophagus*
- This refers to **esophageal adenocarcinoma**, which typically arises from **Barrett's esophagus** in the **distal esophagus**.
- While dysphagia and weight loss can occur, the prominent **hoarseness** points more towards a lesion affecting the pharynx or larynx, which are more commonly sites of **squamous cell carcinoma** due to smoking, rather than glandular tissue (adenocarcinoma).
*Reduced lower esophageal pressure*
- This is a characteristic feature of **achalasia**, a motility disorder where the lower esophageal sphincter fails to relax, leading to **dysphagia** and regurgitation.
- However, achalasia does not typically cause **hoarseness**, nor does it inherently explain the rapid and significant **weight loss** in the context of extensive smoking history, which strongly points to malignancy.
Esophageal pathology US Medical PG Question 6: A 65-year-old African-American man presents to your office with dysphagia. He reports that he has found it progressively more difficult to swallow food over the past year. At the time of presentation, he is able to eat only soup. Social history is significant for asbestos exposure, multiple daily drinks of hard alcohol, and a 70 pack-year smoking history. What would you most expect to see on an esophageal biopsy of this patient?
- A. Esophageal varices
- B. Ferruginous bodies
- C. Keratin nests and pearls (Correct Answer)
- D. Glandular metaplasia
- E. Mucosal abrasions
Esophageal pathology Explanation: ***Keratin nests and pearls***
- This patient's significant **smoking history** and **alcohol consumption** are major risk factors for **esophageal squamous cell carcinoma**, which is characterized microscopically by **keratin nests and pearls** on biopsy.
- The progressive **dysphagia** (difficulty swallowing) over a year, especially progressing to difficulty with solids, is a classic symptom of **esophageal cancer**.
*Esophageal varices*
- Esophageal varices are typically caused by **portal hypertension**, most commonly due to cirrhosis from chronic alcohol abuse.
- While alcohol abuse is present, varices would present with **hematemesis** or melena due to rupture, not progressive dysphagia as the primary symptom.
*Ferruginous bodies*
- These are indicative of **asbestos exposure** in the lungs, typically seen in conditions like asbestosis or mesothelioma.
- They are found in the **lungs**, not in the esophagus, although asbestos exposure is noted in the history.
*Glandular metaplasia*
- **Glandular metaplasia** of the esophagus, also known as **Barrett's esophagus**, is a precursor to **esophageal adenocarcinoma**.
- This typically results from chronic **gastroesophageal reflux disease (GERD)** symptoms, which are not mentioned in this patient.
*Mucosal abrasions*
- Mucosal abrasions would suggest trauma or inflammation but would not explain the **progressive, obstructive dysphagia** over a year.
- Abrasions are generally acute findings and not consistent with the underlying pathology suggested by this patient's long history and risk factors.
Esophageal pathology US Medical PG Question 7: A 56-year-old man comes to the physician because of intermittent retrosternal chest pain. Physical examination shows no abnormalities. Endoscopy shows salmon pink mucosa extending 5 cm proximal to the gastroesophageal junction. Biopsy specimens from the distal esophagus show nonciliated columnar epithelium with numerous goblet cells. Which of the following is the most likely cause of this patient's condition?
- A. Hypermotile esophageal contractions
- B. Atopic inflammation of the esophagus
- C. Fungal infection of the lower esophagus
- D. Esophageal exposure to gastric acid (Correct Answer)
- E. Neoplastic proliferation of esophageal epithelium
Esophageal pathology Explanation: ***Esophageal exposure to gastric acid***
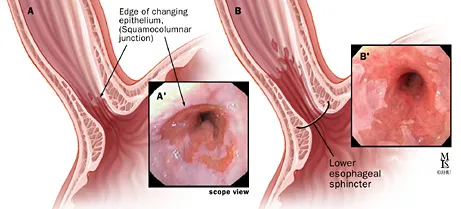
- The presence of **salmon pink mucosa** extending 5 cm proximally from the gastroesophageal junction, along with **nonciliated columnar epithelium** and **goblet cells** in biopsy specimens, is characteristic of **Barrett's esophagus**.
- Barrett's esophagus is a metaplastic change in the esophageal lining, typically caused by chronic **gastroesophageal reflux disease (GERD)**, where recurrent exposure to **gastric acid** leads to the replacement of normal stratified squamous epithelium with intestinal-type columnar epithelium.
*Hypermotile esophageal contractions*
- **Hypermotile esophageal contractions**, such as in spastic disorders, can cause chest pain but do not typically lead to the **mucosal changes** of Barrett's esophagus.
- While they can contribute to reflux, they are not the direct cause of the intestinal metaplasia seen in this patient.
*Atopic inflammation of the esophagus*
- **Atopic inflammation of the esophagus** refers to **eosinophilic esophagitis**, characterized by dysphagia and food impaction, and histologically by significant eosinophil infiltration.
- This condition does not typically present with the **salmon pink mucosa** or **goblet cells** that are indicative of Barrett's esophagus.
*Fungal infection of the lower esophagus*
- **Fungal infections**, such as **Candida esophagitis**, usually present with **odynophagia** and endoscopy showing **white plaques**, not salmon pink mucosa or columnar metaplasia.
- Biopsy would reveal fungal elements, not goblet cells or columnar epithelium.
*Neoplastic proliferation of esophageal epithelium*
- **Neoplastic proliferation** would involve dysplastic changes or carcinoma, which would show severe architectural distortion and cytologic atypia, distinct from the **metaplastic changes** (nonciliated columnar epithelium with goblet cells) observed here.
- While Barrett's esophagus is a **precursor to adenocarcinoma**, the biopsy description indicates metaplasia, not active neoplasia.
Esophageal pathology US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Esophageal pathology Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Esophageal pathology US Medical PG Question 9: A 47-year-old woman presents for a routine wellness checkup. She complains of general fatigue and lethargy for the past 6 months. She does not have a significant past medical history and is currently not taking any medications. The patient reports that she drinks “socially” approx. 6 nights a week. She says she also enjoys a “nightcap,” which is 1–2 glasses of wine before bed every night. She denies any history of drug use or smoking. The patient is afebrile, and her vital signs are within normal limits. A physical examination reveals pallor of the mucous membranes. Her laboratory findings are significant for a mean corpuscular volume of 72 fL, leukocyte count of 5,300/mL, hemoglobin of 11.0 g/dL, and platelet count of 420,000/mL.
Which of the following is the most likely cause of this patient’s thrombocytosis?
- A. Iron deficiency anemia (Correct Answer)
- B. Essential thrombocytosis
- C. Aplastic anemia
- D. Chronic alcohol abuse
- E. Chronic myelogenous leukemia (CML)
Esophageal pathology Explanation: ***Iron deficiency anemia***
- The patient presents with **microcytic anemia** (MCV 72 fL, Hb 11.0 g/dL) and **pallor**, which are classic signs of iron deficiency.
- **Iron deficiency** is a common cause of **secondary thrombocytosis**, as iron plays a role in platelet production and maturation.
*Essential thrombocytosis*
- This is a **myeloproliferative neoplasm** characterized by significantly elevated platelet counts, usually much higher than 420,000/mL (often > 600,000/mL).
- While it causes thrombocytosis, it typically doesn't present with microcytic anemia unless there's a co-existing iron deficiency, which is the primary finding here.
*Aplastic anemia*
- **Aplastic anemia** would present with **pancytopenia** (low red blood cells, white blood cells, and platelets), which is not consistent with the patient's elevated platelet count and normal leukocyte count.
- The patient's presentation of fatigue and pallor would likely be more severe due to significant anemia, and thrombocytosis would not be present.
*Chronic alcohol abuse*
- **Chronic alcohol abuse** typically causes **macrocytic anemia** (elevated MCV) due to folate deficiency or direct bone marrow toxicity, not microcytic anemia.
- While it can sometimes lead to thrombocytopenia, it is not a direct cause of robust thrombocytosis, especially in the context of microcytic anemia.
*Chronic myelogenous leukemia (CML)*
- CML is a **myeloproliferative neoplasm** characterized by the **Philadelphia chromosome (BCR-ABL1 fusion gene)**, leading to a significant increase in **granulocytes** (leukocytosis) and often thrombocytosis.
- Although thrombocytosis can occur, the primary hallmark is significant leukocytosis, which is not seen here (leukocyte count is normal), and the anemia would typically be normocytic or even macrocytic if folate deficient.
Esophageal pathology US Medical PG Question 10: A 61-year-old man with a history of stage IIIa lung adenocarcinoma that has been treated with wedge resection and chemotherapy presents to the primary care clinic. He is largely asymptomatic, but he demonstrates a persistent microcytic anemia despite iron supplementation. Colonoscopy performed 3 years earlier was unremarkable. His past medical history is significant for diabetes mellitus type II, hypertension, acute lymphoblastic leukemia as a child, and hypercholesterolemia. He currently smokes 1 pack of cigarettes per day, drinks a glass of pinot grigio per day, and currently denies any illicit drug use. His vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 126/74 mm Hg; heart rate, 87/min; and respiratory rate, 17/min. On physical examination, his pulses are bounding, complexion is pale, but breath sounds remain clear. Oxygen saturation was initially 91% on room air, with a new oxygen requirement of 2 L by nasal cannula. Which of the following lab values would suggest anemia of chronic disease as the underlying etiology?
- A. Decreased serum iron and transferrin, decreased ferritin, normal serum transferrin receptor
- B. Increased serum iron and transferrin, increased ferritin, normal serum transferrin receptor
- C. Decreased serum iron, increased transferrin, decreased ferritin, increased serum transferrin receptor
- D. Decreased serum iron and transferrin, increased ferritin, normal serum transferrin receptor (Correct Answer)
- E. Decreased serum iron, decreased transferrin, increased ferritin, increased serum transferrin receptor
Esophageal pathology Explanation: ***Decreased serum iron and transferrin, increased ferritin, normal serum transferrin receptor***
- In **anemia of chronic disease (ACD)**, inflammation leads to increased **hepcidin** levels, which blocks iron release from stores and reduces iron absorption, resulting in **decreased serum iron and transferrin** (which reflects transferrin saturation).
- The inflammatory state also causes **ferritin** (an acute phase reactant and iron storage protein) to be **increased** or normal, as iron is sequestered. **Serum transferrin receptor** levels are typically normal, differentiating it from iron deficiency anemia.
*Decreased serum iron and transferrin, decreased ferritin, normal serum transferrin receptor*
- This pattern, particularly the **decreased ferritin**, is more indicative of **iron deficiency anemia**, where the body's iron stores are depleted.
- In iron deficiency, the body attempts to increase iron absorption and mobilization, thus ferritin would be low.
*Increased serum iron and transferrin, increased ferritin, normal serum transferrin receptor*
- This combination is not typical for any common anemia. **Increased serum iron and transferrin** might suggest iron overload conditions, but not iron-restricted erythropoiesis.
- While ferritin can be increased in chronic disease, the increased serum iron and transferrin are contradictory to ACD.
*Decreased serum iron, increased transferrin, decreased ferritin, increased serum transferrin receptor*
- This constellation, especially the **increased transferrin** and **decreased ferritin**, is characteristic of **iron deficiency anemia**.
- **Increased serum transferrin receptor** is a hallmark of iron deficiency, as cells upregulate receptors to capture more iron when deficient.
*Decreased serum iron, decreased transferrin, increased ferritin, increased serum transferrin receptor*
- While **decreased serum iron, decreased transferrin** (low transferrin saturation), and **increased ferritin** can be seen in ACD, the presence of an **increased serum transferrin receptor** is inconsistent.
- An increased serum transferrin receptor is usually a marker for increased erythropoietic activity or iron deficiency, which is not the primary mechanism of ACD.
More Esophageal pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.