Diverticular disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diverticular disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diverticular disease US Medical PG Question 1: A 72-year-old female presents to the emergency department complaining of severe abdominal pain and several days of bloody diarrhea. Her symptoms began with intermittent bloody diarrhea five days ago and have worsened steadily. For the last 24 hours, she has complained of fevers, chills, and abdominal pain. She has a history of ulcerative colitis, idiopathic hypertension, and hypothyroidism. Her medications include hydrochlorothiazide, levothyroxine, and sulfasalazine.
In the ED, her temperature is 39.1°C (102.4°F), pulse is 120/min, blood pressure is 90/60 mmHg, and respirations are 20/min. On exam, the patient is alert and oriented to person and place, but does not know the day. Her mucus membranes are dry. Heart and lung exam are not revealing. Her abdomen is distended with marked rebound tenderness. Bowel sounds are hyperactive.
Serum:
Na+: 142 mEq/L
Cl-: 107 mEq/L
K+: 3.3 mEq/L
HCO3-: 20 mEq/L
BUN: 15 mg/dL
Glucose: 92 mg/dL
Creatinine: 1.2 mg/dL
Calcium: 10.1 mg/dL
Hemoglobin: 11.2 g/dL
Hematocrit: 30%
Leukocyte count: 14,600/mm^3 with normal differential
Platelet count: 405,000/mm^3
What is the next best step in management?
- A. Emergent colonoscopy
- B. Contrast enema
- C. Colectomy
- D. Plain abdominal radiograph
- E. Abdominal CT with IV contrast (Correct Answer)
Diverticular disease Explanation: ***Abdominal CT with IV contrast***
- The patient presents with **severe abdominal pain, bloody diarrhea, fever, hypotension, tachycardia, abdominal distension, rebound tenderness, and leukocytosis**, all suggestive of **toxic megacolon** complicating her ulcerative colitis.
- An **abdominal CT with IV contrast** is the most appropriate next step to confirm the diagnosis, assess the extent of colonic dilation and inflammation, and rule out complications like perforation.
*Emergent colonoscopy*
- **Colonoscopy** is generally **contraindicated** in suspected toxic megacolon due to the high risk of **perforation** of the severely inflamed and dilated colon.
- While it can diagnose ulcerative colitis, the current acute, severe presentation makes it too risky.
*Contrast enema*
- A **contrast enema** is also **contraindicated** in setting of potential **toxic megacolon** or suspected colonic perforation.
- The pressure from the contrast agent could worsen dilation or cause perforation in an already compromised colon.
*Colectomy*
- **Colectomy** is a surgical intervention reserved for cases of **toxic megacolon** that **fail medical management** or when there is evidence of **perforation** or **ischemia**.
- It is not the *immediate* next step in management without further imaging and attempts at medical stabilization.
*Plain abdominal radiograph*
- A plain abdominal radiograph can show colonic dilation and air-fluid levels, which are indicative of toxic megacolon; however, it has **limited ability to assess the extent of inflammation**, detect complications like **perforation**, or rule out other intra-abdominal pathologies.
- It might be a useful initial screen but is not as comprehensive as a CT scan, especially when a definitive diagnosis and management plan is needed.
Diverticular disease US Medical PG Question 2: A 46-year-old woman comes to the emergency department because of intermittent abdominal pain and vomiting for 2 days. The abdominal pain is colicky and diffuse. The patient's last bowel movement was 3 days ago. She has had multiple episodes of upper abdominal pain that radiates to her scapulae and vomiting over the past 3 months; her symptoms subsided after taking ibuprofen. She has coronary artery disease, type 2 diabetes mellitus, gastroesophageal reflux disease, and osteoarthritis of both knees. Current medications include aspirin, atorvastatin, rabeprazole, insulin, and ibuprofen. She appears uncomfortable. Her temperature is 39°C (102.2°F), pulse is 111/min, and blood pressure is 108/68 mm Hg. Examination shows dry mucous membranes. The abdomen is distended and tympanitic with diffuse tenderness; bowel sounds are high-pitched. Rectal examination shows a collapsed rectum. Her hemoglobin concentration is 13.8 g/dL, leukocyte count is 14,400/mm3, and platelet count is 312,000/mm3. An x-ray of the abdomen is shown. Which of the following is the most likely cause of this patient's findings?
- A. Cecal torsion
- B. Viscus perforation
- C. Colonic diverticular inflammation
- D. Cholecystoenteric fistula (Correct Answer)
- E. Bowel infarction
Diverticular disease Explanation: ***Cholecystoenteric fistula***
- The patient's history of recurrent upper abdominal pain radiating to the scapula, responsive to NSAIDs, is highly suggestive of **biliary colic** due to **cholelithiasis**.
- The diffuse colicky pain, vomiting, distended abdomen with high-pitched bowel sounds, and particularly the **pneumobilia** (air in the biliary tree, visible as branching lucency in the hepatic area on X-ray, indicated by red arrows) along with signs of **small bowel obstruction** (dilated small bowel loops and air-fluid levels, indicated by green arrows), are classic features of **gallstone ileus** resulting from a cholecystoenteric fistula.
*Cecal torsion*
- While cecal torsion can cause a large bowel obstruction with colicky pain and distension, it typically presents with a **dilated cecum** and a characteristic "coffee-bean" appearance on X-ray, often without pneumobilia.
- The history of recurrent biliary pain and the presence of pneumobilia are not typical for cecal torsion.
*Viscus perforation*
- A viscus perforation would likely cause **sudden, severe onset abdominal pain**, signs of peritonitis, and usually **free air under the diaphragm** on an upright chest X-ray.
- While the patient has diffuse tenderness, the X-ray findings do not show free intraperitoneal air; instead, they show pneumobilia and small bowel obstruction.
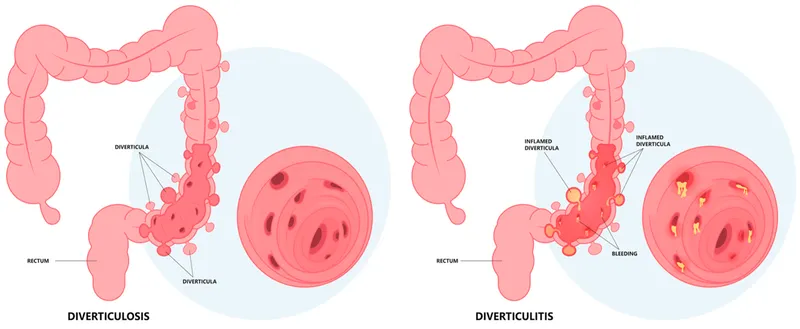
*Colonic diverticuli inflammation*
- **Diverticulitis** typically presents with **left lower quadrant pain**, fever, and changes in bowel habits, though diffuse pain can occur with complications.
- It does not explain the history of recurrent upper abdominal pain radiating to the scapula or the radiologic findings of pneumobilia and small bowel obstruction.
*Bowel infarction*
- Bowel infarction often presents with **severe, disproportionate abdominal pain** (pain out of proportion to exam findings), bloody diarrhea, and signs of sepsis.
- While the patient has some signs of systemic inflammation (fever, leukocytosis), the X-ray findings of pneumobilia and typical small bowel obstruction, without signs of portal venous gas or extensive bowel wall thickening, make infarction less likely as the primary cause.
Diverticular disease US Medical PG Question 3: A 68-year-old woman is brought to the emergency department with intense abdominal pain for the past 2 hours. She has had 1 episode of bloody diarrhea recently. She has an 18-year history of diabetes mellitus. She was diagnosed with hypertension and ischemic heart disease 6 years ago. She is fully alert and oriented. Her temperature is 37.5°C (99.5°F), blood pressure is 145/90 mm Hg, pulse is 78/min, and respirations are 14/min. Abdominal examination shows mild generalized abdominal tenderness without guarding or rebound tenderness. An abdominal plain X-ray shows no abnormalities. Abdominal CT reveals colonic wall thickening and pericolonic fat stranding in the splenic curvature. Bowel rest, intravenous hydration, and IV antibiotics are initiated. Which of the following is the most important diagnostic evaluation at this time?
- A. Angiography
- B. Gastrografin-enhanced X-ray
- C. Laparotomy
- D. Inpatient observation
- E. Sigmoidoscopy (Correct Answer)
Diverticular disease Explanation: ***Sigmoidoscopy***
- The patient's presentation with acute abdominal pain, bloody diarrhea, history of cardiovascular disease, and CT findings consistent with **colonic wall thickening** and **pericolonic fat stranding** strongly suggests **ischemic colitis**.
- **Flexible sigmoidoscopy** allows for direct visualization of the colonic mucosa to confirm the diagnosis, assess the extent and severity of ischemia, and rule out other causes of colitis, such as inflammatory bowel disease or infection.
*Angiography*
- While angiography can identify mesenteric arterial occlusion, it is generally reserved for cases of acute mesenteric ischemia involving the superior mesenteric artery, which typically presents with more severe pain out of proportion to physical exam findings and less clear CT findings of colitis.
- In cases of ischemic colitis, where the primary concern is mucosal ischemia rather than immediate large vessel occlusion, angiography is usually not the first-line diagnostic.
*Gastrografin-enhanced X-ray*
- This study (also known as a **Gastrografin swallow or enema**) is primarily used to evaluate for **perforations** or **obstructions**, or to assess lumen integrity.
- It does not provide the mucosal detail necessary to diagnose or assess the severity of **ischemic colitis**, and the contrast agent itself could potentially exacerbate an inflamed bowel.
*Laparotomy*
- **Laparotomy** (surgical exploration) is an invasive procedure reserved for cases with signs of peritonitis, bowel perforation, or severe, unresponsive ischemia requiring surgical intervention.
- Given the patient's stable vital signs, mild tenderness, and lack of guarding or rebound, immediate surgical exploration is not warranted without further diagnostic steps.
*Inpatient observation*
- While inpatient observation is part of the initial management (bowel rest, IV fluids, antibiotics), it is not a **diagnostic evaluation** itself.
- The question asks for the most important diagnostic evaluation to determine the underlying cause and guide further management.
Diverticular disease US Medical PG Question 4: A 75-year-old man presents to the emergency department for abdominal pain. The patient states the pain started this morning and has been worsening steadily. He decided to come to the emergency department when he began vomiting. The patient has a past medical history of obesity, diabetes, alcohol abuse, and hypertension. His current medications include captopril, insulin, metformin, sodium docusate, and ibuprofen. His temperature is 104.0°F (40°C), blood pressure is 160/97 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Abdominal exam reveals left lower quadrant tenderness. Cardiac exam reveals a crescendo systolic murmur heard best by the right upper sternal border. Lab values are ordered and return as below.
Hemoglobin: 15 g/dL
Hematocrit: 42%
Leukocyte count: 19,500 cells/mm^3 with normal differential
Platelet count: 226,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 101 mEq/L
K+: 4.4 mEq/L
HCO3-: 24 mEq/L
BUN: 22 mg/dL
Glucose: 144 mg/dL
Creatinine: 1.2 mg/dL
Ca2+: 9.8 mg/dL
Which of the following is the most accurate test for this patient's condition?
- A. Colonoscopy
- B. Sigmoidoscopy
- C. Amylase and lipase levels
- D. Barium enema
- E. CT scan (Correct Answer)
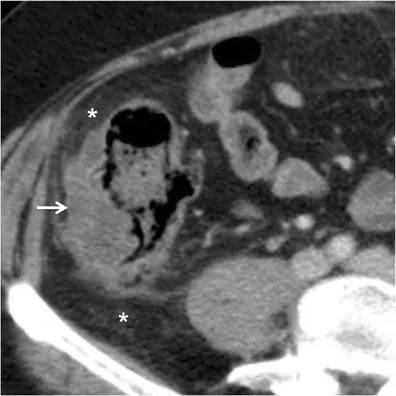
Diverticular disease Explanation: ***CT scan***
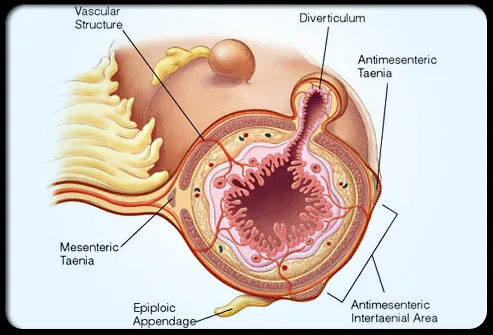
- The patient presents with classic symptoms of **diverticulitis**, including **left lower quadrant pain**, **fever**, and **leukocytosis**. A **CT scan with oral and IV contrast** is the most accurate diagnostic test to identify diverticular inflammation, abscess formation, or perforation.
- A CT scan can also help rule out other causes of abdominal pain and guide further management, such as the need for percutaneous drainage of an abscess.
*Colonoscopy*
- **Colonoscopy is contraindicated during an acute episode of diverticulitis** due to the risk of **perforation** of an inflamed colon.
- It may be considered **6-8 weeks after resolution of acute diverticulitis** to investigate for other pathologies such as malignancy.
*Sigmoidoscopy*
- Similar to colonoscopy, **sigmoidoscopy is generally avoided in acute diverticulitis** because of the risk of **perforation** of the inflamed bowel from instrumentation.
- Its diagnostic yield in acute settings is also limited compared to CT imaging.
*Amylase and lipase levels*
- These tests are primarily used to diagnose **pancreatitis**, which typically presents with **epigastric pain radiating to the back**, often associated with elevated enzyme levels.
- While vomiting is present, the **left lower quadrant tenderness and fever** point away from pancreatitis as the primary diagnosis.
*Barium enema*
- **Barium enema is generally contraindicated in acute diverticulitis** due to the risk of **perforation** and the introduction of barium into the peritoneum, which can cause severe peritonitis.
- It has largely been replaced by **CT scanning** for its superior safety profile and diagnostic accuracy in acute abdominal conditions.
Diverticular disease US Medical PG Question 5: An institutionalized 65-year-old man is brought to the emergency department because of abdominal pain and distension for 12 hours. The pain was acute in onset and is a cramping-type pain associated with nausea, vomiting, and constipation. He has a history of chronic constipation and has used laxatives for years. There is no history of inflammatory bowel disease in his family. He has not been hospitalized recently. There is no recent history of weight loss or change in bowel habits. On physical examination, the patient appears ill. The abdomen is distended with tenderness mainly in the left lower quadrant and is tympanic on percussion. The blood pressure is 110/79 mm Hg, heart rate is 100/min, the respiratory rate is 20/min, and the temperature is 37.2°C (99.0°F). The CBC shows an elevated white blood cell count. The plain abdominal X-ray is shown in the accompanying image. What is the most likely cause of his condition?
- A. Sigmoid volvulus (Correct Answer)
- B. Intussusception
- C. Acute diverticulitis
- D. Toxic megacolon
- E. Colon cancer
Diverticular disease Explanation: ***Sigmoid volvulus***
- The patient’s symptoms of acute **abdominal pain**, distension, and cramping strongly indicate **sigmoid volvulus**, often seen in chronic constipation and institutionalized patients.
- Physical examination revealing **tenderness in the left lower quadrant** and a tympanic abdomen supports the diagnosis of bowel obstruction typically caused by **volvulus**.
*Intussusception*
- Generally presents with **currant jelly stools** and is more common in children; the acute symptoms here are less typical.
- It often involves a **lead point** or associated conditions like **polyps** or tumors, which are not indicated in this case.
*Acute diverticulitis*
- Usually associated with **localized pain** in the left lower quadrant but would present with fever and changes in bowel habits, which the patient lacks.
- Typically shows **peritoneal signs** and may have complications like abscess or perforation, not indicated here.
*Toxic megacolon*
- Commonly associated with underlying **inflammatory bowel disease** or infections, not indicated in this patient with no recent history of **IBD**.
- Symptoms would include severe **diarrhea** and abdominal pain, which do not fit the current acute cramping and constipation pattern.
*Colon cancer*
- While it can cause abdominal symptoms, it presents more insidiously with **weight loss** or **change in bowel habits**, none of which are reported here.
- The acute presentation and findings do not align with a malignancy, which would often be chronic in nature.
Diverticular disease US Medical PG Question 6: A 70-year-old man with a history of chronic constipation presents to the emergency department with a two-day history of left lower quadrant abdominal pain. He is found to have a temperature of 100.8F, BP 140/90, HR 85, and RR 16. On physical examination, he is tender to light palpation in the left lower quadrant and exhibits voluntary guarding. Rectal examination reveals heme-positive stool. Laboratory values are unremarkable except for a WBC count of 12,500 with a left shift. Which of the following tests would be most useful in the diagnosis of this patient's disease?
- A. Abdominal x-ray
- B. Abdominal CT (Correct Answer)
- C. Emergent colonoscopy
- D. Left lower quadrant ultrasound
- E. Lipase
Diverticular disease Explanation: ***Abdominal CT***
- **CT scan** is the most accurate imaging modality for diagnosing **diverticulitis**, identifying bowel wall thickening, inflammation, and complications such as abscess formation.
- It effectively differentiates diverticulitis from other causes of **left lower quadrant pain** and can guide intervention if necessary.
*Abdominal x-ray*
- An **abdominal x-ray** is generally not useful for diagnosing **diverticulitis** as it provides limited soft tissue detail.
- It may identify free air in cases of perforation, but it is not sensitive or specific for diverticular inflammation.
*Emergent colonoscopy*
- **Colonoscopy** is generally contraindicated in acute **diverticulitis** due to the risk of **perforation** of the inflamed colon.
- It is typically performed after recovery from an acute episode (usually 4-6 weeks later) to rule out underlying malignancy or other inflammatory bowel conditions.
*Left lower quadrant ultrasound*
- While **ultrasound** can identify diverticulitis, its diagnostic accuracy is highly **operator-dependent** and can be limited by bowel gas.
- It is often less sensitive than CT, particularly for deeper structures or in obese patients, making **CT** the preferred initial imaging study.
*Lipase*
- **Lipase** is a marker for **pancreatitis** and is not relevant for the diagnosis of **diverticulitis**.
- The patient's symptoms are localized to the left lower quadrant and are not suggestive of pancreatic inflammation.
Diverticular disease US Medical PG Question 7: A 25-year-old male presents to his primary care physician for fatigue, abdominal pain, diarrhea, and weight loss. He states that this issue has occurred throughout his life but seems to “flare up” on occasion. He states that his GI pain is relieved with defecation, and his stools are frequent, large, and particularly foul-smelling. The patient has a past medical history of an ACL tear, as well as a car accident that resulted in the patient needing a transfusion and epinephrine to treat transfusion anaphylaxis. His current medications include vitamin D and ibuprofen. He recently returned from a camping trip in the eastern United States. He states that on the trip they cooked packed meats over an open fire and obtained water from local streams. His temperature is 99.5°F (37.5°C), blood pressure is 120/77 mmHg, pulse is 70/min, respirations are 11/min, and oxygen saturation is 98% on room air. Physical exam reveals poor motor control and an ataxic gait on neurologic exam. Cardiac and pulmonary exams are within normal limits. Laboratory studies are ordered and return as below:
Hemoglobin: 9.0 g/dL
Hematocrit: 25%
Haptoglobin: 12 mg/dL
Leukocyte count: 7,500 cells/mm^3 with normal differential
Platelet count: 255,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 102 mEq/L
K+: 5.0 mEq/L
HCO3-: 24 mEq/L
BUN: 24 mg/dL
Glucose: 82 mg/dL
Creatinine: 1.0 mg/dL
Ca2+: 9.0 mg/dL
LDH: 457 U/L
AST: 11 U/L
ALT: 11 U/L
Radiography is ordered which reveals a stress fracture in the patient’s left tibia. Which of the following is the best confirmatory test for this patient’s condition?
- A. Stool ELISA
- B. Vitamin B12 and folate level
- C. Vitamin E level (Correct Answer)
- D. Bowel wall biopsy
- E. Iron studies
Diverticular disease Explanation: ***Vitamin E level***
- The patient's presentation suggests **celiac disease** causing **malabsorption** with secondary **vitamin E deficiency**, which is causing the specific complications seen here.
- The **neurological findings** of **ataxic gait** and **poor motor control** combined with **hemolytic anemia** (low haptoglobin 12 mg/dL, elevated LDH 457 U/L, anemia) are **pathognomonic for vitamin E deficiency**.
- Vitamin E deficiency causes **spinocerebellar degeneration**, **peripheral neuropathy**, and **hemolytic anemia** due to oxidative damage to RBC membranes and neuronal lipids.
- The **stress fracture** suggests bone disease from calcium/vitamin D malabsorption, but the neuro-hematologic picture is most specific for vitamin E.
- **Serum vitamin E level** is the **confirmatory test** for this specific deficiency syndrome causing the patient's neurological and hematological complications.
- While the underlying condition is likely celiac disease, confirming vitamin E deficiency directly explains the constellation of findings and guides immediate treatment.
*Bowel wall biopsy*
- A **small intestine biopsy** would confirm the underlying diagnosis of **celiac disease** (villous atrophy, crypt hyperplasia) causing the malabsorption.
- However, the question asks for confirmation of "this patient's condition" - referring to the specific syndrome presenting with the characteristic triad of **ataxia + hemolysis + malabsorption**.
- This triad is pathognomonic for **vitamin E deficiency**, making direct measurement more confirmatory for the presenting complication than tissue diagnosis of the underlying cause.
*Vitamin B12 and folate level*
- **Vitamin B12 deficiency** can cause **subacute combined degeneration** with ataxia and neurological symptoms, but typically presents with **posterior column signs** (loss of proprioception, vibration) and **peripheral neuropathy**, not primarily cerebellar ataxia.
- **Folate deficiency** causes **megaloblastic anemia** but does **not** cause neurological deficits or the hemolytic pattern seen here (low haptoglobin, elevated LDH with normal liver enzymes).
- The **hemolytic anemia** is specific to vitamin E deficiency, not B12/folate deficiency.
*Stool ELISA*
- Could detect **Giardia lamblia** given the history of drinking stream water during camping, which can cause acute diarrhea and malabsorption.
- However, this does not explain the **lifelong, recurring symptoms**, **neurological deficits**, **hemolytic anemia**, or **stress fracture**.
- The chronic nature points to a primary malabsorption disorder, not acute infection.
*Iron studies*
- **Iron deficiency** commonly occurs with celiac disease due to duodenal malabsorption and could contribute to the **anemia**.
- However, iron deficiency causes **microcytic anemia**, not hemolytic anemia, and does **not** explain the **low haptoglobin**, **elevated LDH**, **ataxic gait**, or **motor control issues**.
- These findings are specific to vitamin E deficiency.
Diverticular disease US Medical PG Question 8: A 41-year-old male who takes NSAIDs regularly for his chronic back pain develops severe abdominal pain worse with eating. Upper endoscopy is performed and the medical student asks the supervising physician how the histological differentiation between a gastric ulcer and erosion is made. Which of the following layers of the gastric mucosa MUST be breached for a lesion to be considered an ulcer?
- A. Epithelium, lamina propria
- B. Epithelium
- C. Epithelium, lamina propria, muscularis mucosa (Correct Answer)
- D. Epithelium, lamina propria, muscularis mucosa, submucosa, and adventitia
- E. Epithelium, lamina propria, muscularis mucosa, and submucosa
Diverticular disease Explanation: ***Epithelium, lamina propria, muscularis mucosa***
- A **gastric ulcer** by definition involves a breach of the **entire mucosal thickness**, meaning the lesion extends through the muscularis mucosa.
- This deep penetration distinguishes an ulcer from an erosion, which is a more superficial lesion confined to the epithelium and lamina propria.
*Epithelium, lamina propria*
- This describes an **erosion**, a superficial lesion of the gastric mucosa that does not penetrate the **muscularis mucosa**.
- While erosions can cause symptoms, they are generally less severe and have a lower risk of complications like perforation compared to ulcers.
*Epithelium*
- A lesion confined solely to the **epithelium** would be considered a very superficial mucosal injury, often referred to as an **erosion** or sometimes a **superficial abrasion**.
- This degree of injury does not meet the criteria for either an erosion or an ulcer in a histological context.
*Epithelium, lamina propria, muscularis mucosa, submucosa, and adventitia*
- Penetration through the **submucosa** means the ulcer has become a **deep ulcer** or potentially a **perforating ulcer**, if it breaches the entire wall to the adventitia (serosa in the GI tract).
- While an ulcer *can* extend to these layers, only reaching the muscularis mucosa is the *minimum* requirement to be classified as an ulcer.
*Epithelium, lamina propria, muscularis mucosa, and submucosa*
- An ulcer that extends into the **submucosa** is indeed a true ulcer and a more severe one, but the defining histological feature separating an erosion from an ulcer is the breach of the **muscularis mucosa**.
- Therefore, reaching the submucosa is beyond the *minimum* requirement for an ulcer classification.
Diverticular disease US Medical PG Question 9: A 52-year-old man, with a history of alcoholism, presents with loss of appetite, abdominal pain, and fever for the past 24 hours. He says he consumed 12 beers and a bottle of vodka 2 days ago. He reports a 19-year history of alcoholism. His blood pressure is 100/70 mm Hg, pulse is 100/min, respirations are 20/min, and oxygen saturation is 99% on room air. Laboratory findings are significant for the following:
Sodium 137 mEq/L
Potassium 3.4 mEq/L
Alanine aminotransferase (ALT) 230 U/L
Aspartate aminotransferase (AST) 470 U/L
Which of the following histopathologic findings would most likely be found on a liver biopsy of this patient?
- A. Macronodular cirrhosis
- B. T-lymphocyte infiltration
- C. Periportal necrosis
- D. Cytoplasmic inclusion bodies with keratin (Correct Answer)
- E. Positive periodic acid-Schiff stain
Diverticular disease Explanation: ***Cytoplasmic inclusion bodies with keratin***
- The patient's history of **heavy alcohol consumption**, acute presentation with fever, abdominal pain, and elevated **AST and ALT (AST:ALT ratio >2:1)**, are highly suggestive of **alcoholic hepatitis**.
- **Mallory bodies**, which are **cytoplasmic inclusions consisting of intermediate filaments (keratin)**, are a characteristic histopathologic finding in alcoholic hepatitis.
*Macronodular cirrhosis*
- While **alcoholic liver disease** can progress to cirrhosis, the acute presentation with fever and significant transaminase elevation points more towards **alcoholic hepatitis** rather than established macronodular cirrhosis as the primary acute event.
- **Macronodular cirrhosis** typically involves larger nodules of regenerating hepatocytes, but the *acute inflammatory changes* of alcoholic hepatitis are paramount in this presentation.
*T-lymphocyte infiltration*
- While some inflammatory cells are present in alcoholic hepatitis, **T-lymphocyte infiltration** is more characteristic of **chronic viral hepatitis** or **autoimmune hepatitis**.
- The liver injury in alcoholic hepatitis is primarily mediated by neutrophils and direct hepatotoxic effects of alcohol metabolites.
*Periportal necrosis*
- **Periportal necrosis** is more commonly seen in **viral hepatitis** or other forms of **acute hepatitis** where the inflammatory process is concentrated around the portal tracts.
- In alcoholic hepatitis, the damage is typically *centrilobular (zone 3)*, around the terminal hepatic venule, due to its hypoxic vulnerability and high cytochrome P450 activity.
*Positive periodic acid-Schiff stain*
- A **positive periodic acid-Schiff (PAS) stain** that is *diastase-resistant* is a characteristic finding in **alpha-1 antitrypsin deficiency**, a genetic disorder affecting the liver and lungs.
- This patient's clinical presentation and lab findings are inconsistent with alpha-1 antitrypsin deficiency and strongly point towards **alcoholic liver disease**.
Diverticular disease US Medical PG Question 10: A 25-year-old woman presents to her primary care physician complaining of several months of diarrhea. She has also had crampy abdominal pain. She has tried modifying her diet without improvement. She has many watery, non-bloody bowel movements per day. She also reports feeling fatigued. The patient has not recently traveled outside of the country. She has lost 10 pounds since her visit last year, and her BMI is now 20. On exam, she has skin tags and an anal fissure. Which of the following would most likely be seen on endoscopy and biopsy?
- A. Diffuse, non-focal ulcerations with granuloma
- B. Diffuse, non-focal ulcerations without granuloma
- C. Focal ulcerations with granuloma (Correct Answer)
- D. Pseudopolyps and continuous mucosal involvement
- E. Friable mucosa with pinpoint hemorrhages
Diverticular disease Explanation: ***Focal ulcerations with granuloma***
- The patient's symptoms (diarrhea, crampy abdominal pain, fatigue, weight loss, skin tags, and anal fissure) are highly suggestive of **Crohn's disease**.
- **Crohn's disease** is characterized by **transmural inflammation** that often presents as **focal ulcerations** (skip lesions) and **non-caseating granulomas** on biopsy.
*Diffuse, non-focal ulcerations with granuloma*
- While granulomas are characteristic of Crohn's disease, the inflammation in Crohn's disease is typically **focal and discontinuous** (skip lesions), not diffuse.
- Diffuse inflammation with granulomas is less typical for inflammatory bowel disease and might prompt consideration for other granulomatous diseases not fitting this clinical picture.
*Diffuse, non-focal ulcerations without granuloma*
- **Diffuse ulcerations without granulomas** would be more suggestive of **ulcerative colitis**, but the presence of **skin tags** and **anal fissure** points away from this diagnosis and towards Crohn's disease.
- Ulcerative colitis is also characterized by **continuous inflammation** starting from the rectum, which is not described as focal.
*Pseudopolyps and continuous mucosal involvement*
- **Pseudopolyps** and **continuous mucosal involvement** are classic features of **ulcerative colitis**, not Crohn's disease.
- The patient's extraintestinal manifestations like **skin tags** and **anal fissure** are much more common in Crohn's disease.
*Friable mucosa with pinpoint hemorrhages*
- **Friable mucosa** and **pinpoint hemorrhages** are characteristic findings in **ulcerative colitis**, specifically indicating active inflammation and mucosal fragility.
- While these can be seen in inflammatory bowel disease, the full clinical picture with associated perianal disease is more specific for Crohn's disease.
More Diverticular disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.