Colon polyps and neoplasms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Colon polyps and neoplasms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Colon polyps and neoplasms US Medical PG Question 1: A 62-year-old man comes to the physician because of progressive fatigue and dyspnea on exertion for 3 months. During this time, he has also had increased straining during defecation and a 10-kg (22-lb) weight loss. He has no personal or family history of serious medical illness. Physical examination shows conjunctival pallor. Laboratory studies show microcytic anemia. Test of the stool for occult blood is positive. Colonoscopy shows an exophytic mass in the ascending colon. Pathologic examination of the mass shows a well-differentiated adenocarcinoma. A gain-of-function mutation in which of the following genes is most likely involved in the pathogenesis of this patient's condition?
- A. APC
- B. TP53
- C. MLH1
- D. KRAS (Correct Answer)
- E. DCC
Colon polyps and neoplasms Explanation: ***KRAS***
- A **gain-of-function mutation** in **KRAS** is a common early event in the development of colorectal adenocarcinoma, driving uncontrolled cell growth and proliferation.
- This mutation is frequently found in **sporadic colorectal cancers**, particularly in the advanced stages of adenoma to carcinoma progression.
*APC*
- **APC** is a **tumor suppressor gene**, and mutations in it are typically **loss-of-function**, not gain-of-function.
- While APC mutations are crucial early steps in the adenoma-carcinoma sequence, they lead to inactivation of the gene, not increased function.
*TP53*
- **TP53** is a **tumor suppressor gene** which, when mutated, usually involves **loss-of-function** or dominant-negative effects, impairing its ability to induce apoptosis or cell cycle arrest.
- Mutations in TP53 are typically associated with **later stages** of colorectal cancer progression and tend to be loss-of-function, not gain-of-function.
*MLH1*
- **MLH1** is involved in **DNA mismatch repair**, and mutations here lead to **microsatellite instability** and are characteristic of hereditary nonpolyposis colorectal cancer (Lynch syndrome).
- These are typically **loss-of-function mutations** that impair DNA repair, not gain-of-function mutations promoting oncogenesis directly through signaling pathways.
*DCC*
- **DCC** (**Deleted in Colorectal Carcinoma**) is a **tumor suppressor gene**, and its inactivation or loss is associated with colorectal cancer progression, particularly the transition from adenoma to carcinoma.
- Mutations or deletions in DCC result in a **loss-of-function**, not a gain-of-function, contributing to tumor growth by failing to regulate cell differentiation and apoptosis.
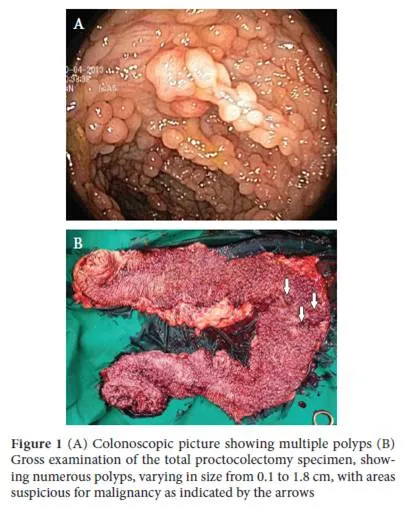
Colon polyps and neoplasms US Medical PG Question 2: A 19-year-old man comes to the physician because of a 2-day history of blood-speckled stools and a protruding rectal mass. He has no abdominal pain, altered bowel habits, or fever. His mother has inflammatory bowel disease. His vital signs are within normal limits. Examination shows multiple, small, hyperpigmented maculae on the lips, buccal mucosa, palms, and soles. The abdomen is soft with no organomegaly. Rectal examination shows a 4-cm pedunculated polyp with superficial excoriations on the mucosa. A colonoscopy shows 14 polyps. A biopsy shows hamartomatous mucosal polyps. This patient's diagnosis is most likely?
- A. Crohn's disease
- B. Juvenile polyposis syndrome
- C. Ulcerative colitis
- D. Familial adenomatous polyposis
- E. Peutz-Jeghers syndrome (Correct Answer)
Colon polyps and neoplasms Explanation: ***Peutz-Jeghers syndrome***
- The presence of **multiple hamartomatous polyps** in the gastrointestinal tract, coupled with **hyperpigmented macules** on the lips, buccal mucosa, palms, and soles, is pathognomonic for Peutz-Jeghers syndrome.
- This condition carries an increased risk of various cancers, including colorectal, breast, gastric, and pancreatic cancers.
*Crohn's disease*
- While Crohn's disease can cause bloody stools and rectal involvement, it is characterized by **chronic inflammation**, often with **skip lesions** and **granulomas**, and does not present with mucocutaneous hyperpigmented macules or hamartomatous polyps.
- Symptoms typically include abdominal pain, diarrhea, and weight loss, which are absent here.
*Juvenile polyposis syndrome*
- This syndrome is characterized by **multiple juvenile polyps**, primarily in the colon, but it does **not involve the characteristic mucocutaneous hyperpigmentation** seen in Peutz-Jeghers syndrome.
- The polyps are typically inflammatory rather than purely hamartomatous in the same way as Peutz-Jeghers.
*Familial adenomatous polyposis*
- This condition is characterized by hundreds to thousands of **adenomatous polyps** in the colon and rectum, with a very high risk of colorectal cancer.
- It does **not typically involve hamartomatous polyps** or the mucocutaneous pigmented lesions seen in this patient.
*Ulcerative colitis*
- Ulcerative colitis is characterized by **continuous inflammation** of the colon and rectum, typically causing bloody diarrhea, abdominal pain, and tenesmus.
- It is an inflammatory bowel disease and does **not involve the presence of hamartomatous polyps** or mucocutaneous hyperpigmentation.
Colon polyps and neoplasms US Medical PG Question 3: A 44-year-old man comes to the physician because of fatigue and increased straining during defecation for 3 months. During this time, he has lost 5 kg (12 lb) despite no change in appetite. He has a family history of colon cancer in his maternal uncle and maternal grandfather. His mother died of ovarian cancer at the age of 46. Physical examination shows conjunctival pallor. His hemoglobin concentration is 11.2 g/dL, hematocrit is 34%, and mean corpuscular volume is 76 μm3. Colonoscopy shows an exophytic mass in the ascending colon. Pathologic examination of the resected mass shows a poorly differentiated adenocarcinoma. Genetic analysis shows a mutation in the MSH2 gene. Which of the following is the most likely diagnosis?
- A. Familial adenomatous polyposis
- B. Peutz-Jeghers syndrome
- C. Turcot syndrome
- D. Lynch syndrome (Correct Answer)
- E. Gardner syndrome
Colon polyps and neoplasms Explanation: ***Lynch syndrome***
- The patient's **poorly differentiated adenocarcinoma** in the ascending colon, coupled with the **family history of colon and ovarian cancer** (early onset, diverse cancer types), and the **MSH2 gene mutation**, strongly indicates Lynch syndrome (hereditary nonpolyposis colorectal cancer).
- **Lynch syndrome** is caused by germline mutations in **DNA mismatch repair (MMR) genes** (e.g., MSH2, MLH1, MSH6, PMS2), leading to an increased risk of colorectal, ovarian, endometrial, and other cancers, often at a younger age and predominantly in the **right colon**.
*Familial adenomatous polyposis*
- This syndrome is characterized by the development of **hundreds to thousands of colorectal adenomatous polyps** during adolescence or early adulthood, a feature not mentioned in the patient's presentation.
- It is caused by a germline mutation in the **APC gene**, not MSH2, leading to an almost 100% lifetime risk of colorectal cancer if untreated.
*Peutz-Jeghers syndrome*
- This syndrome is characterized by **hamartomatous polyps** throughout the gastrointestinal tract and **mucocutaneous melanin pigmentation** (dark spots on lips, buccal mucosa, fingers/toes).
- It is associated with mutations in the **STK11 gene** and an increased risk of various cancers, but the clinical presentation and genetic mutation do not match.
*Turcot syndrome*
- Turcot syndrome is a rare condition characterized by the coexistence of **colorectal polyposis** (either FAP-like or Lynch-like) and **central nervous system tumors** (e.g., medulloblastoma, glioblastoma).
- While it can involve MMR gene mutations in some cases, the prominent feature of CNS tumors is absent in this patient's history.
*Gardner syndrome*
- This is a subtype of FAP, characterized by colorectal polyps along with **extra-intestinal manifestations** such as **osteomas** (especially in the mandible or skull), **epidermoid cysts**, and **desmoid tumors**.
- Like FAP, it is caused by mutations in the **APC gene**, and the characteristic extra-intestinal features are not described in the patient.
Colon polyps and neoplasms US Medical PG Question 4: A 50-year-old man presents to the emergency department complaining of blood in his stool. He reports that this morning he saw bright red blood in the toilet bowl. He denies fatigue, headache, weight loss, palpitations, constipation, or diarrhea. He has well-controlled hypertension and takes hydrochlorothiazide. His father has rheumatoid arthritis, and his mother has Graves disease. The patient’s temperature is 98°F (36.7°C), blood pressure is 128/78 mmHg, and pulse is 70/min. He appears well. No source for the bleeding is appreciated upon physical examination, including a digital rectal exam. A fecal occult blood test is positive. Which of the following is the most appropriate initial diagnostic test to rule out malignancy?
- A. Barium enema
- B. Colonoscopy (Correct Answer)
- C. Anoscopy
- D. Computed tomography
- E. Upper endoscopy
Colon polyps and neoplasms Explanation: ***Colonoscopy***
- **Colonoscopy** is the most appropriate initial diagnostic test for diagnosing the source of **lower gastrointestinal bleeding** and ruling out malignancy, especially in a 50-year-old with positive fecal occult blood. It offers direct visualization of the entire colon and permits **biopsy** of suspicious lesions.
- The patient's age and the presence of **bright red blood per rectum (hematochezia)**, even if intermittent, warrant a thorough evaluation for **colorectal cancer** or its precursors.
*Barium enema*
- A **barium enema** is an imaging study that can identify mass lesions but is less sensitive than colonoscopy for detecting small polyps or early cancers.
- It does not allow for **biopsy** of suspected lesions, which is crucial for confirming malignancy.
*Anoscopy*
- **Anoscopy** visualizes only the anal canal and the distal rectum, making it suitable for diagnosing conditions like **hemorrhoids** or **anal fissures**.
- It cannot evaluate for sources of bleeding higher up in the colon, which is necessary to rule out malignancy in this case.
*Computed tomography*
- **Computed tomography (CT) scans** can identify large masses or metastatic disease but are not the primary diagnostic tool for initial evaluation of **lower GI bleeding** or for ruling out primary colon cancer.
- CT does not offer direct visualization of the colonic mucosa or allow for **biopsy** of suspicious lesions.
*Upper endoscopy*
- **Upper endoscopy** evaluates the esophagus, stomach, and duodenum to identify sources of **upper gastrointestinal bleeding**.
- Given the symptom of **bright red blood per rectum**, the source of bleeding is most likely in the **lower GI tract**, making upper endoscopy an unlikely initial diagnostic choice.
Colon polyps and neoplasms US Medical PG Question 5: A 38-year-old man presents to his primary care practitioner for 2 months of rectal bleeding. He also reports occasional diarrhea and abdominal pain. His family history is relevant for his father and uncle, who died from complications of colorectal cancer. Colonoscopy shows more than 10 colorectal adenomas. Which of the following genes is most likely affected in this patient?
- A. RAS
- B. TP53
- C. hMLH1
- D. PPAR
- E. APC (Correct Answer)
Colon polyps and neoplasms Explanation: ***APC***
- This patient's presentation with **numerous colorectal adenomas** (over 10), early-onset symptoms (38 years old), and a strong **family history of colorectal cancer** (father and uncle) is highly characteristic of **Familial Adenomatous Polyposis (FAP)**.
- FAP is an **autosomal dominant** condition caused by a germline mutation in the **APC tumor suppressor gene**, leading to the development of hundreds to thousands of adenomatous polyps in the colon, which inevitably progress to colorectal cancer if untreated.
*RAS*
- **RAS mutations** are commonly found in sporadic colorectal cancers and play a role in tumor growth and progression, but they are not typically associated with the **hereditary syndrome of multiple adenomas** seen in this patient.
- RAS activation leads to an increase in **cell proliferation** and can contribute to the development of many cancers, but not as the primary genetic defect in a polyposis syndrome.
*TP53*
- **TP53** is a well-known tumor suppressor gene, and mutations are involved in various cancers, including colorectal cancer (often in its later stages). However, germline mutations in TP53 are associated with **Li-Fraumeni syndrome**, which involves a broad spectrum of early-onset cancers and is not primarily characterized by numerous colonic adenomas.
- TP53 mutations are generally hallmarks of **genomic instability** and are more often seen in the progression of sporadic cancers rather than initiating a polyposis syndrome.
*hMLH1*
- **hMLH1** is a gene involved in **DNA mismatch repair**. Germline mutations in this gene, along with other mismatch repair genes (e.g., MSH2, MSH6, PMS2), are responsible for **Lynch syndrome (hereditary non-polyposis colorectal cancer - HNPCC)**.
- While Lynch syndrome is an important cause of hereditary colorectal cancer, it is characterized by fewer polyps (typically <10) that progress rapidly to cancer, and an increased risk of other cancers (e.g., endometrial), which differs from the presentation of **hundreds of adenomas** seen in FAP.
*PPAR*
- **PPARs (Peroxisome Proliferator-Activated Receptors)** are a group of nuclear receptor proteins that play roles in metabolism, cell differentiation, and inflammation.
- While PPAR pathways have been investigated for their potential role in cancer development and as therapeutic targets, **mutations in PPAR genes are not directly linked** to a common hereditary colorectal cancer syndrome characterized by numerous adenomas like FAP.
Colon polyps and neoplasms US Medical PG Question 6: A 41-year-old woman is referred by her radiation oncologist to the medical genetics clinic. She was recently diagnosed with an infiltrating ductal carcinoma of the breast. She has a previous history of colonic polyps for which she undergoes bi-annual colonoscopy. The maternal and paternal family history is unremarkable for polyps and malignant or benign tumors. However, the patient reports that her 10-year-old son has dark brown pigmentation on his lips, and she also had similar pigmentation as a child. Histology of colonic polyps in this patient will most likely reveal which of the following?
- A. Adenomatous polyps
- B. Inflammatory polyps
- C. Retention polyps
- D. Hyperplastic polyps
- E. Hamartomatous polyps (Correct Answer)
Colon polyps and neoplasms Explanation: ***Hamartomatous polyps***
- The constellation of **breast carcinoma**, a history of **colonic polyps**, and **mucocutaneous pigmentation** (dark brown pigmentation on lips in the patient and her son) is highly suggestive of **Peutz-Jeghers Syndrome**.
- **Peutz-Jeghers Syndrome** is an autosomal dominant disorder characterized by the development of **hamartomatous polyps** in the gastrointestinal tract and an increased risk of various cancers, including breast and colorectal cancer.
*Adenomatous polyps*
- While adenomatous polyps are common and can be a precursor to colorectal cancer, the presence of associated **mucocutaneous pigmentation** points away from typical adenomatous familial or sporadic polyposis syndromes (e.g., FAP).
- These polyps are characteristic of **Familial Adenomatous Polyposis (FAP)** or sporadic colorectal cancer, but FAP usually presents with hundreds to thousands of polyps and does not typically involve mucocutaneous pigmentation.
*Inflammatory polyps*
- **Inflammatory polyps** are typically a reactive process secondary to chronic inflammation, such as in inflammatory bowel disease (Crohn's disease or ulcerative colitis), and are not associated with specific hereditary syndromes like Peutz-Jeghers or mucocutaneous pigmentation.
- They do not carry the same increased risk of malignancy as hamartomatous or adenomatous polyps in the context of a syndrome.
*Retention polyps*
- **Retention polyps**, also known as juvenile polyps, are usually found in children and are typically benign; however, they can occur sporadically in adults.
- They are generally solitary or few in number and are not associated with the distinct syndromic features of mucocutaneous pigmentation or the wide range of cancer risks seen in Peutz-Jeghers syndrome.
*Hyperplastic polyps*
- **Hyperplastic polyps** are generally considered benign and do not typically lead to cancer, although some serrated hyperplastic polyps can have malignant potential.
- They are not associated with hereditary syndromes presenting with cutaneous pigmentation and multiple extracolic malignancies.
Colon polyps and neoplasms US Medical PG Question 7: A previously healthy 35-year-old woman comes to the physician for a 3-week history of alternating constipation and diarrhea with blood in her stool. She has not had any fevers or weight loss. Her father died of gastric cancer at 50 years of age. Physical examination shows blue-gray macules on the lips and palms of both hands. Colonoscopy shows multiple polyps throughout the small bowel and colon with one ulcerated polyp at the level of the sigmoid colon. Multiple biopsy specimens are collected. These polyps are most likely to be characterized as which of the following histological subtypes?
- A. Hyperplastic
- B. Serrated
- C. Adenomatous
- D. Hamartomatous (Correct Answer)
- E. Inflammatory
Colon polyps and neoplasms Explanation: ***Hamartomatous***
- The combination of **mucocutaneous pigmentation** (blue-gray macules on lips and palms), a family history of **early-onset gastrointestinal cancer**, and widespread **gastrointestinal polyps** is highly suggestive of **Peutz-Jeghers syndrome**.
- Peutz-Jeghers polyps are histologically characterized as **hamartomas**, which are benign growths but carry a significant risk of malignant transformation over time.
*Hyperplastic*
- **Hyperplastic polyps** are generally small, sessile, and located in the rectosigmoid colon, with a very low malignant potential.
- They do not typically present with the extensive pancolonic distribution, mucocutaneous pigmentation, or genetic predisposition for cancer seen in this patient.
*Serrated*
- **Serrated polyps** include sessile serrated lesions and traditional serrated adenomas, which although having malignant potential, do not typically present with the distinct **mucocutaneous findings** characteristic of Peutz-Jeghers syndrome.
- They are also not associated with the same widespread distribution throughout the small bowel and colon as seen in this case.
*Adenomatous*
- **Adenomatous polyps** are the most common type of colorectal polyp and are well-known precursors to colorectal cancer.
- However, they do not typically present with **mucocutaneous pigmentation** on the lips and palms, nor do they often involve the small bowel as extensively as described, which points away from polyposis syndromes like Familial Adenomatous Polyposis (FAP) and towards Peutz-Jeghers syndrome in this specific clinical context.
*Inflammatory*
- **Inflammatory polyps** are usually associated with chronic inflammation, such as **inflammatory bowel disease (IBD)**, and are essentially pseudopolyps formed during cycles of ulceration and healing.
- While IBD can cause GI symptoms and blood in stool, the presence of **mucocutaneous pigmentation** and widespread polyps in the small bowel and colon makes inflammatory polyps an unlikely primary diagnosis in this patient.
Colon polyps and neoplasms US Medical PG Question 8: A 24-year-old man comes to the physician because of 2 episodes of bleeding from the rectum over the past month. The patient’s father died of colon cancer at the age of 42. The patient has no history of any serious illness and takes no medications. He does not smoke. His vital signs are within normal limits. Physical examination shows a small hard mass over the right mandible that is nontender and fixed to the underlying bone. A similarly hard and painless 5 × 5 mass is palpated over the rectus abdominis muscle. On examination of the rectum, a polypoid mass is palpated at fingertip. Proctosigmoidoscopy shows numerous polyps. Which of the following best explains these findings?
- A. Familial polyposis of the colon
- B. Peutz-Jeghers syndrome
- C. Turcot’s syndrome
- D. Gardner’s syndrome (Correct Answer)
- E. Lynch’s syndrome
Colon polyps and neoplasms Explanation: ***Gardner's syndrome***
- This syndrome is a variant of **familial adenomatous polyposis (FAP)**, characterized by numerous **colonic polyps** (leading to rectal bleeding) in conjunction with **extra-intestinal manifestations**.
- The extra-intestinal features described, such as **osteomas** (small hard mass over the mandible) and **desmoid tumors** (painless 5 × 5 mass over the rectus abdominis muscle), are classic findings of Gardner's syndrome. The family history of colon cancer further supports this diagnosis.
*Familial polyposis of the colon*
- Familial adenomatous polyposis (FAP) primarily involves the development of **hundreds to thousands of adenomatous colonic polyps**, leading to a high risk of colorectal cancer.
- While it explains the rectal polyps and family history, it does **not account for the extra-intestinal manifestations** like osteomas and desmoid tumors, which are key to Gardner's syndrome.
*Peutz-Jeghers syndrome*
- This syndrome is characterized by **hamartomatous polyps** throughout the gastrointestinal tract and **mucocutaneous hyperpigmentation** (dark spots) on the lips, buccal mucosa, and digits.
- The patient's presentation does not include hamartomatous polyps or mucocutaneous pigmentation.
*Turcot's syndrome*
- Turcot's syndrome is a rare condition involving the co-occurrence of **colorectal polyps** (often adenomatous) and **central nervous system (CNS) tumors**, such as medulloblastoma or glioblastoma.
- The patient presents with osteomas and desmoid tumors, which are not CNS manifestations central to Turcot's syndrome.
*Lynch's syndrome*
- Lynch syndrome (hereditary nonpolyposis colorectal cancer, HNPCC) is characterized by an increased risk of developing **colorectal cancer** and other cancers (e.g., endometrial, ovarian) due to defects in **DNA mismatch repair genes**.
- It typically involves fewer polyps than FAP and does not present with the specific extra-intestinal symptoms like osteomas or desmoid tumors seen in this patient.
Colon polyps and neoplasms US Medical PG Question 9: A 61-year-old man with a history of stage IIIa lung adenocarcinoma that has been treated with wedge resection and chemotherapy presents to the primary care clinic. He is largely asymptomatic, but he demonstrates a persistent microcytic anemia despite iron supplementation. Colonoscopy performed 3 years earlier was unremarkable. His past medical history is significant for diabetes mellitus type II, hypertension, acute lymphoblastic leukemia as a child, and hypercholesterolemia. He currently smokes 1 pack of cigarettes per day, drinks a glass of pinot grigio per day, and currently denies any illicit drug use. His vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 126/74 mm Hg; heart rate, 87/min; and respiratory rate, 17/min. On physical examination, his pulses are bounding, complexion is pale, but breath sounds remain clear. Oxygen saturation was initially 91% on room air, with a new oxygen requirement of 2 L by nasal cannula. Which of the following lab values would suggest anemia of chronic disease as the underlying etiology?
- A. Decreased serum iron and transferrin, decreased ferritin, normal serum transferrin receptor
- B. Increased serum iron and transferrin, increased ferritin, normal serum transferrin receptor
- C. Decreased serum iron, increased transferrin, decreased ferritin, increased serum transferrin receptor
- D. Decreased serum iron and transferrin, increased ferritin, normal serum transferrin receptor (Correct Answer)
- E. Decreased serum iron, decreased transferrin, increased ferritin, increased serum transferrin receptor
Colon polyps and neoplasms Explanation: ***Decreased serum iron and transferrin, increased ferritin, normal serum transferrin receptor***
- In **anemia of chronic disease (ACD)**, inflammation leads to increased **hepcidin** levels, which blocks iron release from stores and reduces iron absorption, resulting in **decreased serum iron and transferrin** (which reflects transferrin saturation).
- The inflammatory state also causes **ferritin** (an acute phase reactant and iron storage protein) to be **increased** or normal, as iron is sequestered. **Serum transferrin receptor** levels are typically normal, differentiating it from iron deficiency anemia.
*Decreased serum iron and transferrin, decreased ferritin, normal serum transferrin receptor*
- This pattern, particularly the **decreased ferritin**, is more indicative of **iron deficiency anemia**, where the body's iron stores are depleted.
- In iron deficiency, the body attempts to increase iron absorption and mobilization, thus ferritin would be low.
*Increased serum iron and transferrin, increased ferritin, normal serum transferrin receptor*
- This combination is not typical for any common anemia. **Increased serum iron and transferrin** might suggest iron overload conditions, but not iron-restricted erythropoiesis.
- While ferritin can be increased in chronic disease, the increased serum iron and transferrin are contradictory to ACD.
*Decreased serum iron, increased transferrin, decreased ferritin, increased serum transferrin receptor*
- This constellation, especially the **increased transferrin** and **decreased ferritin**, is characteristic of **iron deficiency anemia**.
- **Increased serum transferrin receptor** is a hallmark of iron deficiency, as cells upregulate receptors to capture more iron when deficient.
*Decreased serum iron, decreased transferrin, increased ferritin, increased serum transferrin receptor*
- While **decreased serum iron, decreased transferrin** (low transferrin saturation), and **increased ferritin** can be seen in ACD, the presence of an **increased serum transferrin receptor** is inconsistent.
- An increased serum transferrin receptor is usually a marker for increased erythropoietic activity or iron deficiency, which is not the primary mechanism of ACD.
Colon polyps and neoplasms US Medical PG Question 10: A 47-year-old woman presents for a routine wellness checkup. She complains of general fatigue and lethargy for the past 6 months. She does not have a significant past medical history and is currently not taking any medications. The patient reports that she drinks “socially” approx. 6 nights a week. She says she also enjoys a “nightcap,” which is 1–2 glasses of wine before bed every night. She denies any history of drug use or smoking. The patient is afebrile, and her vital signs are within normal limits. A physical examination reveals pallor of the mucous membranes. Her laboratory findings are significant for a mean corpuscular volume of 72 fL, leukocyte count of 5,300/mL, hemoglobin of 11.0 g/dL, and platelet count of 420,000/mL.
Which of the following is the most likely cause of this patient’s thrombocytosis?
- A. Iron deficiency anemia (Correct Answer)
- B. Essential thrombocytosis
- C. Aplastic anemia
- D. Chronic alcohol abuse
- E. Chronic myelogenous leukemia (CML)
Colon polyps and neoplasms Explanation: ***Iron deficiency anemia***
- The patient presents with **microcytic anemia** (MCV 72 fL, Hb 11.0 g/dL) and **pallor**, which are classic signs of iron deficiency.
- **Iron deficiency** is a common cause of **secondary thrombocytosis**, as iron plays a role in platelet production and maturation.
*Essential thrombocytosis*
- This is a **myeloproliferative neoplasm** characterized by significantly elevated platelet counts, usually much higher than 420,000/mL (often > 600,000/mL).
- While it causes thrombocytosis, it typically doesn't present with microcytic anemia unless there's a co-existing iron deficiency, which is the primary finding here.
*Aplastic anemia*
- **Aplastic anemia** would present with **pancytopenia** (low red blood cells, white blood cells, and platelets), which is not consistent with the patient's elevated platelet count and normal leukocyte count.
- The patient's presentation of fatigue and pallor would likely be more severe due to significant anemia, and thrombocytosis would not be present.
*Chronic alcohol abuse*
- **Chronic alcohol abuse** typically causes **macrocytic anemia** (elevated MCV) due to folate deficiency or direct bone marrow toxicity, not microcytic anemia.
- While it can sometimes lead to thrombocytopenia, it is not a direct cause of robust thrombocytosis, especially in the context of microcytic anemia.
*Chronic myelogenous leukemia (CML)*
- CML is a **myeloproliferative neoplasm** characterized by the **Philadelphia chromosome (BCR-ABL1 fusion gene)**, leading to a significant increase in **granulocytes** (leukocytosis) and often thrombocytosis.
- Although thrombocytosis can occur, the primary hallmark is significant leukocytosis, which is not seen here (leukocyte count is normal), and the anemia would typically be normocytic or even macrocytic if folate deficient.
More Colon polyps and neoplasms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.