Appendicitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Appendicitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Appendicitis US Medical PG Question 1: A 1-year-old boy is brought to the emergency room by his parents because of inconsolable crying and diarrhea for the past 6 hours. As the physician is concerned about acute appendicitis, she consults the literature base. She finds a paper with a table that summarizes data regarding the diagnostic accuracy of multiple clinical findings for appendicitis:
Clinical finding Sensitivity Specificity
Abdominal guarding (in children of all ages) 0.70 0.85
Anorexia (in children of all ages)
0.75 0.50
Abdominal rebound (in children ≥ 5 years of age) 0.85 0.65
Vomiting (in children of all ages) 0.40 0.63
Fever (in children from 1 month to 2 years of age) 0.80 0.80
Based on the table, the absence of which clinical finding would most accurately rule out appendicitis in this patient?
- A. Guarding
- B. Vomiting
- C. Anorexia
- D. Fever (Correct Answer)
- E. Rebound
Appendicitis Explanation: ***Fever***
- To **rule out** a diagnosis, a finding with **high sensitivity** is desired. A high sensitivity means that if the disease is present, the test result will almost always be positive. Therefore, a negative test result (absence of the finding) in a highly sensitive test makes the presence of the disease unlikely.
- Fever has a sensitivity of **0.80**, which means it is present in 80% of patients with appendicitis in the 1 month to 2 years age group. While 0.80 isn't extremely high, among the options applicable to this age group, it is the highest sensitivity for a "rule out" purpose. The absence of fever would therefore be the most useful finding to rule out appendicitis.
*Guarding*
- Guarding has a sensitivity of **0.70**, meaning it is present in 70% of appendicitis cases. While it's a useful sign, its sensitivity is lower than fever for ruling out the condition.
- Its higher specificity (0.85) means that its presence makes appendicitis more likely, but its absence is less helpful for ruling it out compared to a highly sensitive finding.
*Vomiting*
- Vomiting has a sensitivity of **0.40**, which is very low. This means that 60% of patients with appendicitis do not experience vomiting.
- Therefore, the absence of vomiting is not a reliable indicator to rule out appendicitis, as many appendicitis cases occur without it.
*Anorexia*
- Anorexia has a sensitivity of **0.75**. While higher than vomiting and guarding, it is still lower than fever (0.80) in the relevant age group for ruling out appendicitis.
- Its low specificity (0.50) indicates it's a common symptom even in children without appendicitis, making its presence less diagnostic and its absence less useful for ruling out.
*Rebound*
- The table states that abdominal rebound data is for children **≥ 5 years of age**. The patient is 1 year old.
- Therefore, this clinical finding's diagnostic accuracy is not applicable to the given patient's age and cannot be used for diagnosis or ruling out appendicitis.
Appendicitis US Medical PG Question 2: A 19-year-old man comes to the emergency department because of abdominal pain, nausea, and vomiting for 4 hours. Initially, the pain was dull and located diffusely around his umbilicus, but it has now become sharper and moved towards his lower right side. He has no history of serious illness and takes no medications. His temperature is 38.2°C (100.7°F) and blood pressure is 123/80 mm Hg. Physical examination shows severe right lower quadrant tenderness without rebound or guarding; bowel sounds are decreased. His hemoglobin concentration is 14.2 g/dL, leukocyte count is 12,000/mm3, and platelet count is 280,000/mm3. Abdominal ultrasonography shows a dilated noncompressible appendix with distinct wall layers and echogenic periappendiceal fat. Intravenous fluid resuscitation is begun. Which of the following is the most appropriate next step in management?
- A. Prescribe oral amoxicillin and clavulanic acid
- B. Perform laparoscopic appendectomy (Correct Answer)
- C. Perform percutaneous drainage
- D. Perform interval appendectomy
- E. Begin bowel rest and nasogastric aspiration
Appendicitis Explanation: ***Perform laparoscopic appendectomy***
- The patient presents with classic symptoms of **acute appendicitis**, including periumbilical pain migrating to the right lower quadrant, localized tenderness, fever, and leukocytosis.
- Abdominal ultrasonography showing a **dilated noncompressible appendix** with echogenic periappendiceal fat further confirms the diagnosis, making surgical removal the most appropriate and definitive treatment.
*Prescribe oral amoxicillin and clavulanic acid*
- While antibiotics are often given pre-operatively, they are not the definitive treatment for **acute appendicitis**, especially with clear imaging findings.
- Relying solely on antibiotics in this scenario would risk **perforation** and increased morbidity.
*Perform percutaneous drainage*
- Percutaneous drainage is typically reserved for **appendiceal abscesses** or phlegmons, especially if the patient is unstable or the inflammation is walled off.
- There is no mention of an abscess in this patient's presentation or imaging, making surgical removal of the inflamed appendix the primary treatment.
*Perform interval appendectomy*
- **Interval appendectomy** is considered for patients who initially respond to conservative antibiotic management for an appendiceal mass or phlegmon.
- Since this patient has acute symptoms with clear ultrasound findings of appendicitis without mention of an abscess that would necessitate conservative management, immediate surgical intervention is indicated.
*Begin bowel rest and nasogastric aspiration*
- Bowel rest and nasogastric aspiration are indicated for conditions like **bowel obstruction** or severe **pancreatitis** to decompress the gastrointestinal tract.
- These measures do not address the underlying inflammation and obstruction of acute appendicitis and would delay definitive treatment, increasing the risk of complications.
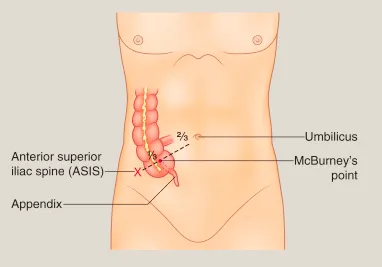
Appendicitis US Medical PG Question 3: A 24-year-old woman comes to the emergency department because of abdominal pain, fever, nausea, and vomiting for 12 hours. Her abdominal pain was initially dull and diffuse but has progressed to a sharp pain on the lower right side. Two years ago she had to undergo right salpingo-oophorectomy after an ectopic pregnancy. Her temperature is 38.7°C (101.7°F). Physical examination shows severe right lower quadrant tenderness with rebound tenderness; bowel sounds are decreased. Laboratory studies show leukocytosis with left shift. An abdominal CT scan shows a distended, edematous appendix. The patient is taken to the operating room for an appendectomy. During the surgery, the adhesions from the patient's previous surgery make it difficult for the resident physician to identify the appendix. Her attending mentions that she should use a certain structure for guidance to locate the appendix. The attending is most likely referring to which of the following structures?
- A. Epiploic appendages
- B. Right ureter
- C. Deep inguinal ring
- D. Ileocolic artery
- E. Teniae coli (Correct Answer)
Appendicitis Explanation: ***Teniae coli***
- The **teniae coli** are three distinct longitudinal bands of smooth muscle that run along the length of the cecum and colon, converging at the base of the **appendix**.
- Following these bands inferiorly from the ascending colon or cecum during surgery is a reliable method to locate the **vermiform appendix**, especially in the presence of adhesions.
*Epiploic appendages*
- These are small, fat-filled sacs that protrude from the surface of the **large intestine** but are not directly used as a reliable landmark for locating the appendix.
- While present in the vicinity, they do not consistently lead to the base of the appendix like the teniae coli.
*Right ureter*
- The **right ureter** is located retroperitoneally, deep to the cecum and appendix, and is not a direct anatomical landmark used for identifying the appendix during an appendectomy.
- Identifying the ureter is important to avoid injury, but not for localizing the appendix.
*Deep inguinal ring*
- The **deep inguinal ring** is an opening in the transversalis fascia, involved in the formation of the inguinal canal, and is located far anterior and inferior to the region of the appendix.
- It has no anatomical relationship that would guide a surgeon to locate the appendix.
*Ileocolic artery*
- The **ileocolic artery** branches from the superior mesenteric artery and supplies the terminal ileum, cecum, and appendix. While it provides blood supply to the appendix, it is not a direct or consistent surface landmark for locating the appendix itself, especially in complex cases with adhesions.
- Locating the artery would be more complex and less reliable for initial identification compared to the teniae coli.
Appendicitis US Medical PG Question 4: A 12-year-old boy is brought to the emergency room by his mother with complaints of abdominal pain and fever that started 24 hours ago. On further questioning, the mother says that her son vomited twice and has constipation that started approximately 1 and one-half days ago. The medical history is benign. The vital signs are as follows: heart rate 103/min, respiratory rate of 20/min, temperature 38.7°C (101.66°F), and blood pressure 109/69 mm Hg. On physical examination, there is severe right lower quadrant abdominal tenderness on palpation. Which of the following is the most likely cause for this patient’s symptoms?
- A. Luminal obstruction due to a fecalith (Correct Answer)
- B. Ascending infection of the urinary tract
- C. Telescoping of bowel segment causing intestinal obstruction
- D. Twisting of testes on its axis, hampering the blood supply
- E. Immune-mediated vasculitis associated with IgA deposition
Appendicitis Explanation: ***Luminal obstruction due to a fecalith***
- The classic presentation of **appendicitis** in a 12-year-old boy, including **abdominal pain**, fever, vomiting, constipation, and **right lower quadrant tenderness**, is most commonly caused by **luminal obstruction** due to a **fecalith**.
- This obstruction leads to inflammation, bacterial overgrowth, and edema of the appendix, resulting in the described symptoms.
- Other causes of appendiceal luminal obstruction include **lymphoid hyperplasia** and, less commonly, parasites or tumors.
*Ascending infection of the urinary tract*
- While urinary tract infections (UTIs) can cause fever and abdominal pain, the **severe, localized right lower quadrant tenderness** and specific progression of symptoms (vomiting, constipation) are less typical than for appendicitis.
- UTIs are usually associated with **dysuria, frequency, and urgency**, which are not mentioned here.
*Telescoping of bowel segment causing intestinal obstruction*
- This describes **intussusception**, which typically presents in **younger children (6 months to 3 years)** with **colicky abdominal pain**, vomiting, and **currant jelly stools**.
- While it can cause abdominal pain and vomiting, the **age of the patient**, **localized right lower quadrant tenderness**, and absence of classic signs make appendicitis more likely.
*Twisting of testes on its axis, hampering the blood supply*
- This describes **testicular torsion**, which presents with **sudden, severe scrotal pain**, swelling, and tenderness, sometimes with referred abdominal pain.
- The primary complaint of **abdominal pain** with associated vomiting, fever, and right lower quadrant tenderness makes appendicitis a more likely diagnosis.
*Immune-mediated vasculitis associated with IgA deposition*
- This refers to **Henoch-Schönlein purpura (HSP)**, which typically presents with a **palpable purpuric rash** on the lower extremities and buttocks, **arthralgia**, abdominal pain, and sometimes renal involvement.
- The absence of a rash and key features of HSP makes this diagnosis less likely than appendicitis.
Appendicitis US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Appendicitis Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Appendicitis US Medical PG Question 6: A 34-year-old man presents to the office for evaluation of a lesion on his upper arm that appeared a few months ago and has not healed. The patient appears healthful but has a history of cardiovascular disease. He states that his friend at the industrial ammunition factory where he works told him he should "get it looked at." The patient admits to some nausea, vomiting, and diarrhea over the past year, but he states that he "feels fine now." On physical examination, the lesion is an erythematous, scaly, ulcerated plaque on the flexor surface of his upper arm. The rest of the exam is within normal limits. What is the most likely diagnosis?
- A. Squamous cell carcinoma (SCC) (Correct Answer)
- B. Erythema multiforme
- C. Actinic keratosis
- D. Erysipelas
- E. Contact dermatitis
Appendicitis Explanation: ***Squamous cell carcinoma (SCC)***
- The patient's occupational exposure to chemicals at an **ammunition factory**, along with chronic non-healing, **ulcerated, scaly plaque**, raises suspicion for SCC, particularly **arsenic-induced SCC**.
- His history of vague **gastrointestinal symptoms** (nausea, vomiting, diarrhea) over the past year is also consistent with **chronic arsenic exposure**, which is a known carcinogen.
*Erythema multiforme*
- This is an **acute, self-limiting hypersensitivity reaction** to medications or infections, characterized by target lesions, not a chronic, non-healing ulcerated plaque.
- It would not typically present with a history of chronic GI symptoms related to occupational exposure.
*Actinic keratosis*
- This is a **precancerous lesion** caused by chronic sun exposure, typically presenting as a rough, scaly patch on sun-exposed areas.
- While it has malignant potential to transform into SCC, the description of an **ulcerated, non-healing lesion** with a history of probable chemical exposure makes SCC a more likely *current* diagnosis.
*Erysipelas*
- Erysipelas is a **superficial bacterial infection** of the skin characterized by a rapidly spreading, bright red, well-demarcated, and painful rash, often accompanied by fever and systemic symptoms.
- It would not manifest as a chronic, non-healing ulcerated plaque over several months.
*Contact dermatitis*
- This is an **inflammatory skin reaction** due to direct contact with an allergen or irritant, typically presenting as an itchy, erythematous rash with vesicles or papules.
- It would not typically result in a chronic, ulcerated, non-healing plaque and is not associated with the systemic symptoms or occupational exposure history presented.
Appendicitis US Medical PG Question 7: In which of the following pathological states would the oxygen content of the trachea resemble the oxygen content in the affected alveoli?
- A. Emphysema
- B. Exercise
- C. Pulmonary embolism (Correct Answer)
- D. Pulmonary fibrosis
- E. Foreign body obstruction distal to the trachea
Appendicitis Explanation: ***Pulmonary embolism***
- A pulmonary embolism blocks **blood flow** to a portion of the lung, creating **dead space ventilation** (high V/Q ratio).
- In the affected alveoli, **no blood perfusion** means no oxygen extraction occurs, so the alveolar oxygen content remains **high and similar to tracheal/inspired air**.
- This is the classic physiological state where ventilation continues but perfusion is absent, preventing gas exchange.
*Foreign body obstruction distal to the trachea*
- A complete obstruction **prevents fresh air** from reaching the affected alveoli.
- The trapped gas undergoes **resorption atelectasis**: oxygen is absorbed into capillary blood, CO2 diffuses in, and alveolar gas equilibrates with **venous blood** composition.
- Alveolar oxygen content becomes **very low**, not similar to tracheal air.
*Emphysema*
- Emphysema involves destruction of **alveolar walls** and enlargement of airspaces with impaired gas exchange.
- While V/Q mismatch occurs, oxygen is still extracted by perfusing blood.
- Alveolar oxygen content is **lower than tracheal air** due to ongoing (though inefficient) gas exchange.
*Exercise*
- During exercise, **oxygen consumption increases** dramatically with enhanced cardiac output and oxygen extraction.
- Alveolar oxygen content is **significantly lower** than tracheal air due to increased oxygen uptake by blood.
*Pulmonary fibrosis*
- Pulmonary fibrosis causes **thickening of the alveolar-capillary membrane**, impairing oxygen diffusion.
- Despite diffusion limitation, blood still perfuses the alveoli and extracts oxygen.
- Alveolar oxygen content is **lower than tracheal air**, though the A-a gradient is increased.
Appendicitis US Medical PG Question 8: A 52-year-old man, with a history of alcoholism, presents with loss of appetite, abdominal pain, and fever for the past 24 hours. He says he consumed 12 beers and a bottle of vodka 2 days ago. He reports a 19-year history of alcoholism. His blood pressure is 100/70 mm Hg, pulse is 100/min, respirations are 20/min, and oxygen saturation is 99% on room air. Laboratory findings are significant for the following:
Sodium 137 mEq/L
Potassium 3.4 mEq/L
Alanine aminotransferase (ALT) 230 U/L
Aspartate aminotransferase (AST) 470 U/L
Which of the following histopathologic findings would most likely be found on a liver biopsy of this patient?
- A. Macronodular cirrhosis
- B. T-lymphocyte infiltration
- C. Periportal necrosis
- D. Cytoplasmic inclusion bodies with keratin (Correct Answer)
- E. Positive periodic acid-Schiff stain
Appendicitis Explanation: ***Cytoplasmic inclusion bodies with keratin***
- The patient's history of **heavy alcohol consumption**, acute presentation with fever, abdominal pain, and elevated **AST and ALT (AST:ALT ratio >2:1)**, are highly suggestive of **alcoholic hepatitis**.
- **Mallory bodies**, which are **cytoplasmic inclusions consisting of intermediate filaments (keratin)**, are a characteristic histopathologic finding in alcoholic hepatitis.
*Macronodular cirrhosis*
- While **alcoholic liver disease** can progress to cirrhosis, the acute presentation with fever and significant transaminase elevation points more towards **alcoholic hepatitis** rather than established macronodular cirrhosis as the primary acute event.
- **Macronodular cirrhosis** typically involves larger nodules of regenerating hepatocytes, but the *acute inflammatory changes* of alcoholic hepatitis are paramount in this presentation.
*T-lymphocyte infiltration*
- While some inflammatory cells are present in alcoholic hepatitis, **T-lymphocyte infiltration** is more characteristic of **chronic viral hepatitis** or **autoimmune hepatitis**.
- The liver injury in alcoholic hepatitis is primarily mediated by neutrophils and direct hepatotoxic effects of alcohol metabolites.
*Periportal necrosis*
- **Periportal necrosis** is more commonly seen in **viral hepatitis** or other forms of **acute hepatitis** where the inflammatory process is concentrated around the portal tracts.
- In alcoholic hepatitis, the damage is typically *centrilobular (zone 3)*, around the terminal hepatic venule, due to its hypoxic vulnerability and high cytochrome P450 activity.
*Positive periodic acid-Schiff stain*
- A **positive periodic acid-Schiff (PAS) stain** that is *diastase-resistant* is a characteristic finding in **alpha-1 antitrypsin deficiency**, a genetic disorder affecting the liver and lungs.
- This patient's clinical presentation and lab findings are inconsistent with alpha-1 antitrypsin deficiency and strongly point towards **alcoholic liver disease**.
Appendicitis US Medical PG Question 9: A 25-year-old woman presents to her primary care physician complaining of several months of diarrhea. She has also had crampy abdominal pain. She has tried modifying her diet without improvement. She has many watery, non-bloody bowel movements per day. She also reports feeling fatigued. The patient has not recently traveled outside of the country. She has lost 10 pounds since her visit last year, and her BMI is now 20. On exam, she has skin tags and an anal fissure. Which of the following would most likely be seen on endoscopy and biopsy?
- A. Diffuse, non-focal ulcerations with granuloma
- B. Diffuse, non-focal ulcerations without granuloma
- C. Focal ulcerations with granuloma (Correct Answer)
- D. Pseudopolyps and continuous mucosal involvement
- E. Friable mucosa with pinpoint hemorrhages
Appendicitis Explanation: ***Focal ulcerations with granuloma***
- The patient's symptoms (diarrhea, crampy abdominal pain, fatigue, weight loss, skin tags, and anal fissure) are highly suggestive of **Crohn's disease**.
- **Crohn's disease** is characterized by **transmural inflammation** that often presents as **focal ulcerations** (skip lesions) and **non-caseating granulomas** on biopsy.
*Diffuse, non-focal ulcerations with granuloma*
- While granulomas are characteristic of Crohn's disease, the inflammation in Crohn's disease is typically **focal and discontinuous** (skip lesions), not diffuse.
- Diffuse inflammation with granulomas is less typical for inflammatory bowel disease and might prompt consideration for other granulomatous diseases not fitting this clinical picture.
*Diffuse, non-focal ulcerations without granuloma*
- **Diffuse ulcerations without granulomas** would be more suggestive of **ulcerative colitis**, but the presence of **skin tags** and **anal fissure** points away from this diagnosis and towards Crohn's disease.
- Ulcerative colitis is also characterized by **continuous inflammation** starting from the rectum, which is not described as focal.
*Pseudopolyps and continuous mucosal involvement*
- **Pseudopolyps** and **continuous mucosal involvement** are classic features of **ulcerative colitis**, not Crohn's disease.
- The patient's extraintestinal manifestations like **skin tags** and **anal fissure** are much more common in Crohn's disease.
*Friable mucosa with pinpoint hemorrhages*
- **Friable mucosa** and **pinpoint hemorrhages** are characteristic findings in **ulcerative colitis**, specifically indicating active inflammation and mucosal fragility.
- While these can be seen in inflammatory bowel disease, the full clinical picture with associated perianal disease is more specific for Crohn's disease.
Appendicitis US Medical PG Question 10: A 65-year-old man is brought to the emergency department because of a 1-day history of fever and disorientation. His wife reports that he had abdominal pain and diarrhea the previous day. He drinks 60 oz of alcohol weekly. His pulse is 110/min and blood pressure is 96/58 mm Hg. Examination shows jaundice, palmar erythema, spider nevi on his chest, dilated veins on the anterior abdominal wall, and 2+ edema of the lower extremities. The abdomen is soft and diffusely tender; there is shifting dullness to percussion. His albumin is 1.4 g/dL, bilirubin is 5 mg/dL, and prothrombin time is 31 seconds (INR = 3.3). Hepatitis serology is negative. A CT scan of the abdomen is shown. Which of the following processes is the most likely explanation for these findings?
- A. Accumulation of iron in hepatocytes
- B. Ground-glass hepatocytes with cytotoxic T cells
- C. Fibrous bands surrounding regenerating hepatocytes (Correct Answer)
- D. Misfolded protein aggregates in hepatocellular endoplasmic reticulum
- E. Hepatocyte swelling with Councilman bodies and monocyte infiltration
Appendicitis Explanation: ***Fibrous bands surrounding regenerating hepatocytes***
- The patient presents with classic signs of **cirrhosis** (jaundice, palmar erythema, spider nevi, dilated abdominal veins, edema, ascites), acute decompensation (fever, disorientation, hypotension), and severe **hepatic dysfunction** (low albumin, high bilirubin, prolonged PT/INR). The history of heavy alcohol use supports this.
- **Cirrhosis** is histologically characterized by diffuse **fibrosis** and the formation of **regenerative nodules**, which are hepatocytes surrounded by fibrous bands, leading to disruption of normal liver architecture and function.
*Accumulation of iron in hepatocytes*
- This is characteristic of **hereditary hemochromatosis**, which leads to **iron overload** and organ damage, including cirrhosis.
- While hemochromatosis can cause cirrhosis, the patient's acute symptoms and specific liver histology (macronodular cirrhosis often seen in alcoholic liver disease) make alcoholic cirrhosis a more direct fit, and there is no mention of increased iron in labs.
*Ground-glass hepatocytes with cytotoxic T cells*
- **Ground-glass hepatocytes** are typically seen in **chronic hepatitis B infection**, representing an accumulation of HBsAg in the endoplasmic reticulum.
- While chronic hepatitis B can lead to cirrhosis, the negative hepatitis serology and direct evidence of alcohol abuse do not support this as the primary cause.
*Misfolded protein aggregates in hepatocellular endoplasmic reticulum*
- This description is characteristic of **alpha-1 antitrypsin deficiency**, where defective alpha-1 antitrypsin accumulates in hepatocytes.
- Although it can cause cirrhosis, the patient's symptoms are more consistent with alcoholic liver disease, and there is no mention of respiratory symptoms often associated with alpha-1 antitrypsin deficiency.
*Hepatocyte swelling with Councilman bodies and monocyte infiltration*
- **Hepatocyte swelling** and **Councilman bodies** (apoptotic hepatocytes) are features of **acute viral hepatitis** or other forms of acute liver injury. Monocyte infiltration can also occur.
- While acute liver injury can occur, the chronic stigmata of liver disease (spider nevi, palmar erythema, ascites) and the history of alcohol abuse point to a chronic process like cirrhosis rather than just acute inflammation.
More Appendicitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.