Thromboembolic disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thromboembolic disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thromboembolic disease US Medical PG Question 1: A 21-year-old woman comes to the physician because of a 1-day history of right leg pain. The pain is worse while walking and improves when resting. Eight months ago, she was diagnosed with a pulmonary embolism and was started on warfarin. Anticoagulant therapy was discontinued two months ago. Her mother had systemic lupus erythematosus. On examination, her right calf is diffusely erythematous, swollen, and tender. Cardiopulmonary examination shows no abnormalities. On duplex ultrasonography, the right popliteal vein is not compressible. Laboratory studies show an elevated serum level of D-dimer and insensitivity to activated protein C. Further evaluation of this patient is most likely to show which of the following?
- A. Deficiency of protein C
- B. Protein S deficiency
- C. Elevated coagulation factor VIII levels
- D. Mutation of coagulation factor V (Correct Answer)
- E. Mutation of prothrombin
Thromboembolic disease Explanation: ***Mutation of coagulation factor V***
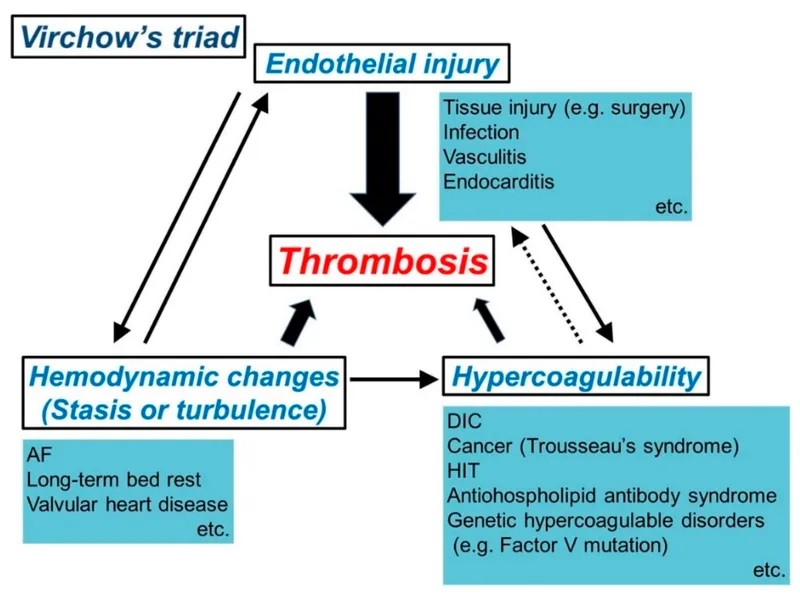
- The patient's history of **recurrent DVT/PE** at a young age, family history of autoimmune disease (mother's SLE), and laboratory finding of **insensitivity to activated protein C** strongly point towards **Factor V Leiden mutation**.
- This mutation makes **Factor V resistant to inactivation** by activated protein C, leading to a hypercoagulable state and increased risk of venous thromboembolism.
*Deficiency of protein C*
- While it also causes **insensitivity to activated protein C** and a hypercoagulable state, a true deficiency of protein C would lead to quantitative reduction, not primarily functional insensitivity.
- Protein C deficiency can cause **severe thrombotic events**, but the given lab finding of "insensitivity to activated protein C" points more directly to a defect in Factor V.
*Protein S deficiency*
- **Protein S** acts as a cofactor for activated protein C, so its deficiency would also impair the anticoagulant pathway and could lead to thrombosis.
- However, **Protein S deficiency** does not directly cause "insensitivity to activated protein C" as the primary defect; rather, it reduces the effectiveness of activated protein C.
*Elevated coagulation factor VIII levels*
- **High levels of Factor VIII** are a risk factor for VTE, but this condition would not lead to **insensitivity to activated protein C**.
- While it contributes to a hypercoagulable state, it's a distinct mechanism not indicated by the specific lab finding mentioned.
*Mutation of prothrombin*
- **Prothrombin G20210A mutation** (mutation of prothrombin) leads to increased prothrombin levels and increased thrombin generation, predisposing to thrombosis.
- However, this mutation would not result in **insensitivity to activated protein C**, which is the key laboratory finding in this patient.
Thromboembolic disease US Medical PG Question 2: A 48-year-old man comes to the emergency department because of sudden right flank pain that began 3 hours ago. He also noticed blood in his urine. Over the past two weeks, he has developed progressive lower extremity swelling and a 4-kg (9-lb) weight gain. Examination shows bilateral 2+ pitting edema of the lower extremities. Urinalysis with dipstick shows 4+ protein, positive glucose, and multiple red cell and fatty casts. Abdominal CT shows a large right kidney with abundant collateral vessels and a filling defect in the right renal vein. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Factor V Leiden
- B. Malignant erythropoietin production
- C. Antiphospholipid antibodies
- D. Increased lipoprotein synthesis
- E. Loss of antithrombin III (Correct Answer)
Thromboembolic disease Explanation: ***Loss of antithrombin III***
- The patient presents with **nephrotic syndrome** (lower extremity edema, weight gain, 4+ proteinuria, fatty casts), which causes massive urinary loss of proteins, including **antithrombin III**, a critical inhibitor of coagulation.
- Loss of **antithrombin III** creates a **hypercoagulable state**, predisposing to **renal vein thrombosis** (RVT), which explains the acute flank pain, hematuria, enlarged kidney, and filling defect on CT.
- This is the underlying mechanism linking the nephrotic syndrome to the thrombotic complication.
*Factor V Leiden*
- This is a **genetic mutation** causing Factor V resistance to activated protein C, leading to hypercoagulability.
- While it can cause venous thrombosis, it does **not cause nephrotic syndrome** with massive proteinuria and fatty casts as seen in this patient.
- This would be a predisposing factor, not the underlying cause of the nephrotic syndrome itself.
*Antiphospholipid antibodies*
- These antibodies cause a **hypercoagulable state** and can lead to both arterial and venous thromboses, including RVT.
- However, they do **not directly cause nephrotic syndrome** with the massive proteinuria and fatty casts seen here.
- Like Factor V Leiden, this would predispose to thrombosis but doesn't explain the primary renal pathology.
*Increased lipoprotein synthesis*
- This is a **consequence** of nephrotic syndrome, where hepatic compensation for albumin loss leads to increased synthesis of all proteins, including lipoproteins, causing hyperlipidemia.
- It is a **secondary effect**, not the mechanism causing the hypercoagulable state and renal vein thrombosis.
*Malignant erythropoietin production*
- This would cause **polycythemia** (increased RBC count) and potentially thrombotic events due to hyperviscosity.
- It does **not explain** the profound nephrotic syndrome with massive proteinuria, edema, and fatty casts.
- There is no evidence of polycythemia in this clinical presentation.
Thromboembolic disease US Medical PG Question 3: A 23-year-old woman with no significant past medical history currently on oral contraceptive pills presents to the emergency department with pleuritic chest pain. She states that it started today. Yesterday she had a trip and returned via plane. Her temperature is 98°F (36.7°C), blood pressure is 117/66 mmHg, pulse is 105/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam reveals tachycardia, a normal S1 and S2, and clear breath sounds. The patient’s lower extremities are non-tender and symmetric. Chest pain is not reproducible with position changes or palpation but is worsened with deep breaths. Which of the following is the most appropriate next test for this patient?
- A. D-dimer
- B. Ultrasound of the lower extremities
- C. Ventilation-perfusion scan
- D. CT angiogram (Correct Answer)
- E. Chest radiograph
Thromboembolic disease Explanation: ***CT angiogram***
- This patient has **HIGH probability for pulmonary embolism (PE)** based on **Wells criteria**: oral contraceptive use (hypercoagulable state), recent long-haul flight (immobilization), pleuritic chest pain, and tachycardia (pulse 105/min).
- With a **Wells score ≥4**, the appropriate next step is **definitive imaging with CT pulmonary angiography (CTPA)**, which is the **gold standard** for diagnosing PE.
- **D-dimer should be bypassed** in high-probability cases, as a negative result would not adequately rule out PE, and a positive result (expected in high-probability patients) would require CTPA anyway.
- CTPA provides direct visualization of pulmonary arterial thrombi and can also identify alternative diagnoses.
*D-dimer*
- D-dimer is appropriate for **low to moderate probability PE** (Wells score <4) where a negative result can safely rule out PE and avoid unnecessary imaging.
- In this **high-probability case**, D-dimer is likely to be positive regardless, making it an unnecessary intermediate step that delays definitive diagnosis.
- Using D-dimer in high-probability patients can lead to false reassurance if negative or simply confirms the need for CTPA if positive.
*Ultrasound of the lower extremities*
- Lower extremity ultrasound diagnoses **deep vein thrombosis (DVT)**, not PE directly.
- While finding DVT in a patient with suspected PE would support anticoagulation, **absence of DVT does not rule out PE**, as thrombi may have already embolized.
- This would delay appropriate diagnosis and is not the most direct test for suspected PE.
*Ventilation-perfusion scan*
- V/Q scan is reserved for patients with **contraindications to CT contrast** (severe renal insufficiency, contrast allergy) or pregnant patients where radiation exposure should be minimized.
- This young patient has no mentioned contraindications to contrast-enhanced CT.
- V/Q scanning is less specific than CTPA and often yields indeterminate results.
*Chest radiograph*
- Chest X-ray is often **normal in PE** or shows non-specific findings (Westermark sign, Hampton's hump are rare).
- While it may help exclude alternative diagnoses like pneumothorax or pneumonia, it cannot definitively diagnose or rule out PE.
- In a patient with high clinical suspicion for PE, delaying CTPA to obtain a chest X-ray is not optimal management.
Thromboembolic disease US Medical PG Question 4: A 62-year-old man comes to the physician because of a 5-day history of swelling in his left arm. Two months ago, he was diagnosed with a deep venous thrombosis in the left calf. He has had a 7-kg (15-lb) weight loss in the last 3 months. He has smoked 1 pack of cigarettes daily for the past 25 years. His only medication is warfarin. Physical examination shows warm edema of the left forearm with overlying erythema and a tender, palpable cord-like structure along the medial arm. His lungs are clear to auscultation bilaterally. Duplex sonography shows thrombosis of the left basilic and external jugular veins. Which of the following is the most appropriate next step to confirm the underlying diagnosis?
- A. CT scan of the chest
- B. X-ray of the chest (Correct Answer)
- C. Transesophageal echocardiography
- D. Serum antiphospholipid antibody level
- E. Serum D-dimer level
Thromboembolic disease Explanation: **X-ray of the chest**
- The patient presents with **recurrent deep venous thrombosis (DVT)**, specifically in an unusual location (upper extremity), combined with **unexplained weight loss** and a **significant smoking history**. These are strong indicators of an underlying malignancy.
- A **chest x-ray** is a readily available and cost-effective initial screening tool to evaluate for **lung cancer**, which is common in smokers and can present with paraneoplastic phenomena like hypercoagulability (Trousseau phenomenon) leading to DVT.
*CT scan of the chest*
- While a **CT scan of the chest** is more sensitive than an X-ray for detecting lung masses, an **X-ray is the more appropriate initial step** for screening given the clinical context.
- A **CT scan** would typically be performed after an abnormal chest X-ray or if clinical suspicion remains high despite a normal X-ray.
*Transesophageal echocardiography*
- **Transesophageal echocardiography (TEE)** is primarily used to evaluate **cardiac structures**, valve function, and to detect intracardiac thrombi or vegetations.
- It is not indicated as a primary screening tool for an underlying malignancy or in the workup of a **venous thrombosis** not directly related to cardiac pathology.
*Serum antiphospholipid antibody level*
- **Antiphospholipid antibody syndrome** is a cause of recurrent thrombosis, but the patient's other symptoms (weight loss, smoking history, unusual DVT location) point more strongly towards an underlying malignancy.
- While it might be considered in a broader workup for hypercoagulability, it is not the most immediate next step given the constellation of findings strongly suggestive of cancer.
*Serum D-dimer level*
- A **serum D-dimer level** is a marker of fibrin degradation and is useful for **excluding DVT/PE** in low-probability patients.
- In this patient, a DVT has already been diagnosed by duplex sonography, so a D-dimer level would not provide additional diagnostic information regarding the presence of thrombosis, nor would it help in identifying the underlying cause of the recurrent thrombosis.
Thromboembolic disease US Medical PG Question 5: A 67-year-old woman presents with right leg pain and swelling of 5 days’ duration. She has a history of hypertension for 15 years and had a recent hospitalization for pneumonia. She had been recuperating at home but on beginning to mobilize and walk, the right leg became painful and swollen. Her temperature is 37.1°C (98.7°F), the blood pressure is 130/80 mm Hg, and the pulse is 75/min. On physical examination, the right calf is 4 cm greater in circumference than the left when measured 10 cm below the tibial tuberosity. Dilated superficial veins are present on the right foot and the right leg is slightly redder than the left. There is some tenderness on palpation in the popliteal fossa behind the knee. Which of the following is the best initial step in the management of this patient’s condition?
- A. International normalized ratio (INR)
- B. Thrombophilia screen
- C. Wells’ clinical probability tool (Correct Answer)
- D. Computerized tomography (CT) with contrast
- E. Activated partial thromboplastin time (aPTT)
Thromboembolic disease Explanation: ***Wells' clinical probability tool***
- The patient presents with classic signs and symptoms of **deep vein thrombosis (DVT)**, including unilateral leg pain and swelling, dilated superficial veins, and tenderness. The Wells' clinical probability tool helps stratify the risk of DVT, guiding further diagnostic testing.
- Using this validated clinical decision rule for risk assessment is the **best initial step** to determine the likelihood of DVT before proceeding with imaging studies (compression ultrasound) or D-dimer testing.
- Based on the Wells' score, patients are categorized as low, moderate, or high probability, which then directs appropriate diagnostic testing and potential empiric anticoagulation.
*International normalized ratio (INR)*
- **INR** is used to monitor the effectiveness of **warfarin** therapy, an anticoagulant, and to assess liver function.
- It is not an initial diagnostic tool for DVT; rather, it is used **after a DVT diagnosis** has been made and anticoagulation with warfarin has been initiated.
*Thrombophilia screen*
- A **thrombophilia screen** investigates underlying genetic or acquired clotting disorders.
- This is typically performed **after a DVT diagnosis** in younger patients, those with recurrent DVT, or those with a family history of thrombosis, not as an initial diagnostic step unless there is strong suspicion for an underlying clotting disorder.
*Computerized tomography (CT) with contrast*
- A **CT with contrast** (specifically **CT venography**) can diagnose DVT, but it is not the **first-line imaging modality** for suspected DVT because of radiation exposure and contrast risks.
- **Compression ultrasonography** is generally the preferred initial imaging study for DVT, especially after a risk assessment using the Wells' score.
*Activated partial thromboplastin time (aPTT)*
- The **aPTT** is a measure of the intrinsic and common pathways of coagulation and is used to monitor **unfractionated heparin** therapy.
- It is not an initial diagnostic test for DVT; like INR, it is used **after diagnosis** for monitoring anticoagulant treatment.
Thromboembolic disease US Medical PG Question 6: A 12-year-old boy is brought to the emergency department with a hot, swollen, and painful knee. He was playing with his friends and accidentally bumped into one of them with his knee prior to presentation. His medical history is significant for an immunodeficiency syndrome, and he has been treated with long courses of antibiotics for multiple infections. His mother is concerned because he has also had significant bleeding that was hard to control following previous episodes of trauma. Laboratory tests are obtained with the following results:
Prothrombin time: Prolonged
Partial thromboplastin time: Prolonged
Bleeding time: Normal
The activity of which of the following circulating factors would most likely be affected by this patient's disorder?
- A. von Willebrand factor
- B. Factor VIII
- C. Factor X (Correct Answer)
- D. Protein C
- E. Factor XI
Thromboembolic disease Explanation: ***Factor X***
- This patient presents with **vitamin K deficiency** secondary to long-term antibiotic use, which disrupts gut flora responsible for vitamin K synthesis.
- **Factor X** is a vitamin K-dependent procoagulant factor essential for both the intrinsic and extrinsic coagulation pathways (common pathway).
- Vitamin K deficiency leads to reduced activity of **all vitamin K-dependent factors** (II, VII, IX, X, Protein C, Protein S), but the **bleeding presentation** is caused by deficiency of the **procoagulant factors** (II, VII, IX, X).
- Factor X deficiency results in **prolonged PT and PTT** (affects both pathways) with **normal bleeding time** (platelet function intact), exactly matching this patient's lab findings.
- The clinical presentation of **hemarthrosis and significant bleeding** following trauma is consistent with a coagulation factor deficiency, specifically Factor X in the context of vitamin K deficiency.
*Factor XI*
- Factor XI deficiency (Hemophilia C) would cause a **prolonged PTT only**, not prolonged PT.
- This patient has **both prolonged PT and PTT**, ruling out isolated Factor XI deficiency.
*von Willebrand factor*
- von Willebrand factor deficiency primarily causes **prolonged bleeding time** due to impaired platelet adhesion.
- This patient has **normal bleeding time**, making von Willebrand disease unlikely.
*Factor VIII*
- Factor VIII deficiency (Hemophilia A) causes **prolonged PTT only** with normal PT.
- The patient's **prolonged PT and PTT** excludes isolated Factor VIII deficiency.
*Protein C*
- Protein C is a vitamin K-dependent **anticoagulant** factor, so its activity would indeed be reduced in vitamin K deficiency.
- However, Protein C deficiency causes **thrombosis** (increased clotting), not bleeding.
- This patient presents with **bleeding** and prolonged coagulation times, which are caused by deficiency of **procoagulant factors** like Factor X, not anticoagulant factors like Protein C.
- While Protein C activity is affected by vitamin K deficiency, it does not explain the patient's bleeding presentation.
Thromboembolic disease US Medical PG Question 7: A 24-year-old male was in a motor vehicle accident that caused him to fracture his femur and pelvis. After 2 days in the hospital, the patient became delirious, tachypneic, and a petechial rash was found in his upper extremities. Which of the following is most likely responsible for this patient’s symptoms?
- A. Thrombotic clot in the pulmonary artery
- B. Aspiration of oropharyngeal contents
- C. Alveolar foamy exudates with disc shaped cysts seen with methenamine silver stain
- D. Fat microglobules in the microvasculature (Correct Answer)
- E. Type I and type II pneumocyte damage due to neutrophils
Thromboembolic disease Explanation: ***Fat microglobules in the microvasculature***
- This scenario describes **fat embolism syndrome (FES)**, often triggered by trauma to long bones (like the femur) or the pelvis.
- The classic triad of FES includes **respiratory distress (tachypnea)**, **neurological symptoms (delirium)**, and a **petechial rash**, which perfectly matches the patient's presentation.
*Thrombotic clot in the pulmonary artery*
- A **pulmonary embolism (PE)** can cause tachypnea and delirium, but it typically does not present with a **petechial rash**.
- PE is usually due to a **venous thromboembolism** from deep leg veins, though trauma can increase risk, the rash points away from a simple thrombotic PE.
*Aspiration of oropharyngeal contents*
- **Aspiration pneumonia** can cause respiratory distress, but it doesn't typically lead to **delirium or a petechial rash** in this timeframe.
- The symptoms would likely include fever, cough, and infiltrates on chest X-ray.
*Alveolar foamy exudates with disc-shaped cysts seen with methenamine silver stain*
- This description is characteristic of **Pneumocystis pneumonia** (*Pneumocystis jirovecii*), an opportunistic infection typically seen in immunocompromised individuals.
- It would not manifest acutely after trauma with a petechial rash.
*Type I and type II pneumocyte damage due to neutrophils*
- This describes **acute respiratory distress syndrome (ARDS)**, which can be a complication of severe trauma.
- While ARDS could cause respiratory distress and potentially delirium, it generally doesn't present with a **petechial rash** as a hallmark symptom in this context.
Thromboembolic disease US Medical PG Question 8: An 80-year-old woman is brought to the physician by her 2 daughters for worsening memory loss. They report that their mother is increasingly forgetful about recent conversations and events. She is unable to remember her appointments and commitments she has made. 3 years ago, the patient was moved into an elder care facility because she was often getting lost on her way home and forgetting to take her medications. The patient reports that she is very socially active at her new home and has long conversations with the other residents about her adventures as an air hostess during her youth. Which of the following cerebral pathologies is most likely present in this patient?
- A. Lewy bodies
- B. Lacunar infarcts
- C. Intracytoplasmic vacuoles
- D. Neurofibrillary tangles (Correct Answer)
- E. Demyelination
Thromboembolic disease Explanation: ***Neurofibrillary tangles***
- The patient's presentation with **progressive memory loss** affecting recent events, getting lost, and forgetting medications, while largely preserving long-term memory (recalling youth as an air hostess and engaging in conversations), is highly characteristic of **Alzheimer's disease**.
- **Neurofibrillary tangles**, composed of hyperphosphorylated tau protein, along with **amyloid plaques**, are the hallmark pathological findings in Alzheimer's disease.
*Lewy bodies*
- **Lewy bodies** are characteristic of **Lewy body dementia** or Parkinson's disease with dementia, which typically present with prominent **fluctuations in cognition**, recurrent **visual hallucinations**, and parkinsonism.
- While memory loss can occur, the dominant features in this case point away from Lewy body pathology.
*Lacunar infarcts*
- **Lacunar infarcts** are associated with **vascular dementia**, which often presents with a more **step-wise decline** in cognitive function, focal neurological deficits, and evidence of cerebrovascular disease on imaging.
- The patient's gradual and progressive memory loss is less typical of lacunar infarcts as the primary cause.
*Intracytoplasmic vacuoles*
- **Intracytoplasmic vacuoles** are characteristic of **Creutzfeldt-Jakob disease** (spongiform encephalopathy), which is a rapidly progressive and fatal neurodegenerative disorder with distinct neurological symptoms such as myoclonus and ataxia, not fitting this patient's profile.
- The disease course is typically much faster than the 3-year progression described.
*Demyelination*
- **Demyelination** is the hallmark of conditions like **multiple sclerosis**, which primarily affects younger individuals and typically presents with a range of neurological deficits, including motor, sensory, and visual disturbances, that often relapse and remit.
- It does not typically present as a primary, progressive memory disorder in an 80-year-old in this manner.
Thromboembolic disease US Medical PG Question 9: A 25-year-old woman comes to the physician because of recurrent episodes of reddish discoloration of her urine. She also has a 3-month history of intermittent abdominal pain, yellowish discoloration of the skin and eyes, and fatigue. Physical examination shows pallor and scleral icterus. The spleen is not palpable. Her hemoglobin concentration is 7.8 g/dL, leukocyte count is 2,000/mm3, and platelet count is 80,000/mm3. Serum LDH and unconjugated bilirubin concentrations are elevated. Addition of a serum containing anti-human globulins to a blood sample shows no agglutination. A urine dipstick shows blood; urinalysis shows no RBCs. A CT scan of the abdomen shows a thrombus in a distal branch of the superior mesenteric vein. Which of the following is the most likely cause of this patient's condition?
- A. Activation and consumption of platelets and coagulation factors
- B. Absence of protective factors against destruction by complement (Correct Answer)
- C. Replacement of a single amino acid in a β-globin chain
- D. Formation of IgG antibodies against glycoprotein IIb/IIIa
- E. Endothelial cell dysfunction from bacterial toxin production
Thromboembolic disease Explanation: ***Absence of protective factors against destruction by complement***
- The patient's presentation is **classic for Paroxysmal Nocturnal Hemoglobinuria (PNH)**: hemoglobinuria (positive urine dipstick with no RBCs), intravascular hemolysis (elevated LDH/unconjugated bilirubin), pancytopenia, negative Coombs test, and venous thrombosis.
- PNH is caused by an acquired **PIGA gene mutation** leading to deficiency of **GPI-anchored proteins CD55 and CD59** on hematopoietic cells.
- Without these complement regulatory proteins, red blood cells undergo uncontrolled **complement-mediated hemolysis**, and platelet activation leads to thrombotic complications.
*Activation and consumption of platelets and coagulation factors*
- This describes **Disseminated Intravascular Coagulation (DIC)**, which presents with both bleeding and thrombosis, prolonged PT/aPTT, decreased fibrinogen, and elevated D-dimer.
- While PNH can cause thrombosis, the primary pathophysiology is complement dysregulation, not consumption coagulopathy. The negative Coombs test, hemoglobinuria pattern, and pancytopenia point to PNH rather than DIC.
*Replacement of a single amino acid in a β-globin chain*
- This describes **sickle cell disease** (glutamic acid → valine substitution in β-globin), causing RBC sickling under hypoxic conditions.
- Sickle cell typically presents with painful vaso-occlusive crises, acute chest syndrome, and splenic sequestration. The hemoglobinuria without RBCs, pancytopenia, and mesenteric vein thrombosis are characteristic of PNH, not sickle cell disease.
*Formation of IgG antibodies against glycoprotein IIb/IIIa*
- This describes **Immune Thrombocytopenic Purpura (ITP)**, characterized by isolated thrombocytopenia with mucocutaneous bleeding.
- ITP does not cause hemolytic anemia, leukopenia, hemoglobinuria, or thrombosis—features central to this patient's presentation.
*Endothelial cell dysfunction from bacterial toxin production*
- This describes **Hemolytic Uremic Syndrome (HUS)**, typically caused by Shiga toxin-producing E. coli, presenting with the classic triad: microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury.
- HUS features schistocytes on blood smear and renal failure, not pancytopenia or the typical venous thrombosis pattern seen in PNH.
Thromboembolic disease US Medical PG Question 10: A 27-year-old woman presents to the emergency department complaining of a left-sided headache and right-sided blurry vision. She states that 2 weeks ago she developed dark urine and abdominal pain. She thought it was a urinary tract infection so she took trimethoprim-sulfamethoxazole that she had left over. She planned on going to her primary care physician today but then she developed headache and blurry vision so she came to the emergency department. The patient states she is otherwise healthy. Her family history is significant for a brother with sickle cell trait. On physical examination, there is mild abdominal tenderness, and the liver edge is felt 4 cm below the right costal margin. Labs are drawn as below:
Hemoglobin: 7.0 g/dL
Platelets: 149,000/mm^3
Reticulocyte count: 5.4%
Lactate dehydrogenase: 3128 U/L
Total bilirubin: 2.1 mg/dL
Indirect bilirubin: 1.4 mg/dL
Aspartate aminotransferase: 78 U/L
Alanine aminotransferase: 64 U/L
A peripheral smear shows polychromasia. A Doppler ultrasound of the liver shows decreased flow in the right hepatic vein. Magnetic resonance imaging of the brain is pending. Which of the following tests, if performed, would most likely identify the patient’s diagnosis?
- A. Flow cytometry (Correct Answer)
- B. Glucose-6-phosphate-dehydrogenase levels
- C. Anti-histone antibodies
- D. Bone marrow biopsy
- E. Hemoglobin electrophoresis
Thromboembolic disease Explanation: ***Flow cytometry***
- The patient's symptoms (headache, blurry vision, dark urine, abdominal pain, hepatomegaly) along with laboratory findings of **hemolytic anemia** (low hemoglobin, elevated reticulocyte count, high LDH, elevated indirect bilirubin) and signs of **thrombosis** (decreased hepatic vein flow, neurological symptoms) are highly suggestive of **paroxysmal nocturnal hemoglobinuria (PNH)**.
- **Flow cytometry** is the gold standard for diagnosing PNH by detecting the absence of **CD55** and **CD59** on red blood cells, granulocytes, and monocytes, indicating a deficiency in the **GPI anchor protein**.
*Glucose-6-phosphate-dehydrogenase levels*
- **G6PD deficiency** typically presents with hemolytic anemia triggered by **oxidant stressors** (like trimethoprim-sulfamethoxazole) but does not typically cause **thrombosis** or widespread organ involvement (e.g., hepatic vein thrombosis, neurological symptoms) as seen in this patient.
- Measuring G6PD levels would be appropriate if G6PD deficiency was suspected, but the clinical picture points more strongly to PNH due to the thrombotic events.
*Anti-histone antibodies*
- **Anti-histone antibodies** are primarily associated with drug-induced **lupus erythematosus**, which can manifest with various systemic symptoms, but not typically with severe hemolytic anemia and thrombotic microangiopathy in this specific pattern.
- While drug exposure is present (trimethoprim-sulfamethoxazole), the overall clinical and lab findings (especially the severe hemolytic picture and thrombosis) are not characteristic of drug-induced lupus in this context.
*Bone marrow biopsy*
- A **bone marrow biopsy** might show findings consistent with increased erythropoiesis due to hemolysis but is not a primary diagnostic test for PNH or its associated thrombotic complications.
- While it could be part of an evaluation for underlying bone marrow disorders, it would not directly confirm a diagnosis of PNH, which requires specific surface marker detection.
*Hemoglobin electrophoresis*
- **Hemoglobin electrophoresis** is used to diagnose **hemoglobinopathies** such as **sickle cell disease** or **thalassemia**. The patient's brother has sickle cell trait, but the patient's symptoms, particularly the prominent hemolytic anemia and thrombotic events, are not typical of a hemoglobinopathy in this acute presentation.
- While it could rule out a hemoglobinopathy, it wouldn't explain the full spectrum of symptoms, especially the thrombosis and the specific pattern of hemolysis (e.g., elevated LDH, indirect bilirubin).
More Thromboembolic disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.