Shock pathophysiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Shock pathophysiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Shock pathophysiology US Medical PG Question 1: A 51-year-old woman is brought into the emergency department following a motor vehicle accident. She is unconscious and was intubated in the field. Past medical history is unknown. Upon arrival, she is hypotensive and tachycardic. Her temperature is 37.2°C (99.1°F), the pulse is 110/min, the respiratory rate is 22/min, and the blood pressure is 85/60 mm Hg. There is no evidence of head trauma, she withdraws to pain and her pupils are 2mm and reactive to light. Her heart has a regular rhythm without any murmurs or rubs and her lungs are clear to auscultation. Her abdomen is firm and distended with decreased bowel sounds. Her extremities are cool and clammy with weak, thready pulses. There is no peripheral edema. Of the following, what is the likely cause of her presentation?
- A. Septic shock
- B. Neurogenic shock
- C. Obstructive shock
- D. Hypovolemic shock (Correct Answer)
- E. Cardiogenic shock
Shock pathophysiology Explanation: ***Hypovolemic shock***
- The patient's presentation with ***hypotension*** (BP 85/60 mm Hg), ***tachycardia*** (pulse 110/min), ***cool and clammy extremities***, ***weak peripheral pulses***, and a ***firm, distended abdomen*** after a motor vehicle accident strongly suggests internal hemorrhage leading to hypovolemic shock.
- The ***firm and distended abdomen*** is a key indicator of potential intra-abdominal bleeding, significantly contributing to the loss of intravascular volume.
*Septic shock*
- Septic shock is characterized by signs of infection along with organ dysfunction and circulatory compromise, often presenting with **fever** or **hypothermia**, and sometimes **warm extremities** initially due to vasodilation. This patient's temperature is normal, and extremities are cool.
- While hypotension and tachycardia are present, the absence of clear signs of infection and the presence of a firm, distended abdomen make hypovolemia a more immediate concern following trauma.
*Neurogenic shock*
- Neurogenic shock typically follows severe spinal cord injury above T6, leading to a loss of sympathetic tone. This results in **hypotension with bradycardia** and **warm, dry skin** due to widespread vasodilation.
- This patient is tachycardic and has cool, clammy extremities, which contradicts the classic presentation of neurogenic shock.
*Obstructive shock*
- Obstructive shock occurs due to a physical obstruction to central circulation, such as **tension pneumothorax**, **cardiac tamponade**, or **pulmonary embolism**.
- There is no mention of absent breath sounds, jugular venous distention, muffled heart sounds, or other specific signs pointing to an obstructive cause. Lungs are clear to auscultation and heart rhythm is regular.
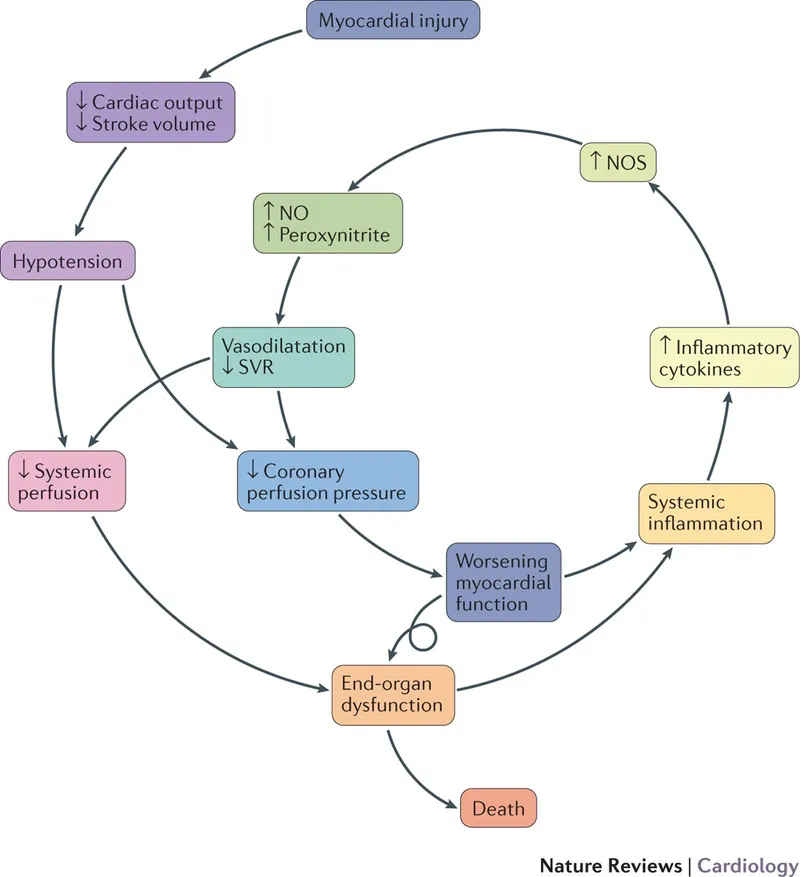
*Cardiogenic shock*
- Cardiogenic shock results from primary cardiac dysfunction, often presenting with signs of **heart failure**, such as **pulmonary edema** (rales), **jugular venous distention**, gallop rhythms, or new murmurs.
- The patient has clear lungs, a regular heart rhythm, and no murmurs, which makes primary cardiac dysfunction less likely as the immediate cause of shock in this trauma setting.
Shock pathophysiology US Medical PG Question 2: A 56-year-old man is brought to the Emergency Department with intense chest pain that radiates to his left arm and jaw. He also complains of feeling lightheaded. Upon arrival, his blood pressure is 104/60 mm Hg, pulse is 102/min, respiratory rate is 25/min, body temperature is 36.5°C (97.7°F), and oxygen saturation is 94% on room air. An electrocardiogram shows an ST-segment elevation in I, aVL, and V5-6. The patient is transferred to the cardiac interventional suite for a percutaneous coronary intervention. The patient is admitted to the hospital after successful revascularization. During his first night on the ICU floor his urinary output is 0.15 mL/kg/h. Urinalysis shows muddy brown casts. Which of the following outcomes specific to the patient’s condition would you expect to find?
- A. Blood urea nitrogen (BUN):Serum creatinine ratio (Cr) < 15:1 (Correct Answer)
- B. Urinary osmolality 900 mOsmol/kg (normal: 500–800 mOsmol/kg)
- C. Urinary osmolality 550 mOsmol/kg (normal: 500–800 mOsmol/kg)
- D. FENa+ < 1%
- E. Blood urea nitrogen (BUN):Serum creatinine ratio (Cr) > 20:1
Shock pathophysiology Explanation: ***Blood urea nitrogen (BUN):Serum creatinine ratio (Cr) < 15:1***
- The patient's presentation with **ST-segment elevation myocardial infarction (STEMI)** followed by low urinary output and **muddy brown casts** strongly indicates **acute tubular necrosis (ATN)**, a form of intrinsic renal failure.
- In ATN, **tubular damage** impairs reabsorption of urea more than creatinine, leading to a **BUN:Cr ratio typically less than 15:1**.
*Urinary osmolality 900 mOsmol/kg (normal: 500–800 mOsmol/kg)*
- A urinary osmolality of 900 mOsmol/kg indicates appropriately concentrated urine, which is characteristic of **prerenal azotemia**, not ATN.
- In ATN, the damaged tubules lose their ability to concentrate urine, resulting in **isosthenuric** urine with osmolality typically **< 350 mOsmol/kg** (approaching plasma osmolality).
*Urinary osmolality 550 mOsmol/kg (normal: 500–800 mOsmol/kg)*
- While 550 mOsmol/kg is within the normal range, it is still **too concentrated for ATN**.
- In ATN, damaged tubules cannot effectively concentrate urine, resulting in **urine osmolality < 350 mOsmol/kg** (isosthenuric, similar to plasma osmolality of ~290 mOsmol/kg).
- This value of 550 mOsmol/kg suggests preserved concentrating ability, which would be more consistent with prerenal azotemia or normal renal function.
*FENa+ < 1%*
- A **fractional excretion of sodium (FENa+) less than 1%** indicates good tubular reabsorption of sodium and is characteristic of **prerenal azotemia**, where the kidneys are attempting to conserve volume.
- In ATN, the damaged tubules cannot effectively reabsorb sodium, so the **FENa+ is typically greater than 2%**.
*Blood urea nitrogen (BUN):Serum creatinine ratio (Cr) > 20:1*
- A **BUN:Cr ratio greater than 20:1** is characteristic of **prerenal azotemia**, reflecting decreased renal perfusion causing increased urea reabsorption relative to creatinine.
- In ATN, the **tubular damage** leads to inefficient urea reabsorption, keeping the ratio **below 15:1**.
Shock pathophysiology US Medical PG Question 3: A 40-year-old Caucasian male presents to the emergency room after being shot in the arm in a hunting accident. His shirt is soaked through with blood. He has a blood pressure of 65/40, a heart rate of 122, and his skin is pale, cool to the touch, and moist. This patient is most likely experiencing all of the following EXCEPT:
- A. Decreased sarcomere length in the myocardium
- B. Increased stroke volume (Correct Answer)
- C. Confusion and irritability
- D. Decreased preload
- E. Increased thromboxane A2
Shock pathophysiology Explanation: ***Increased stroke volume***
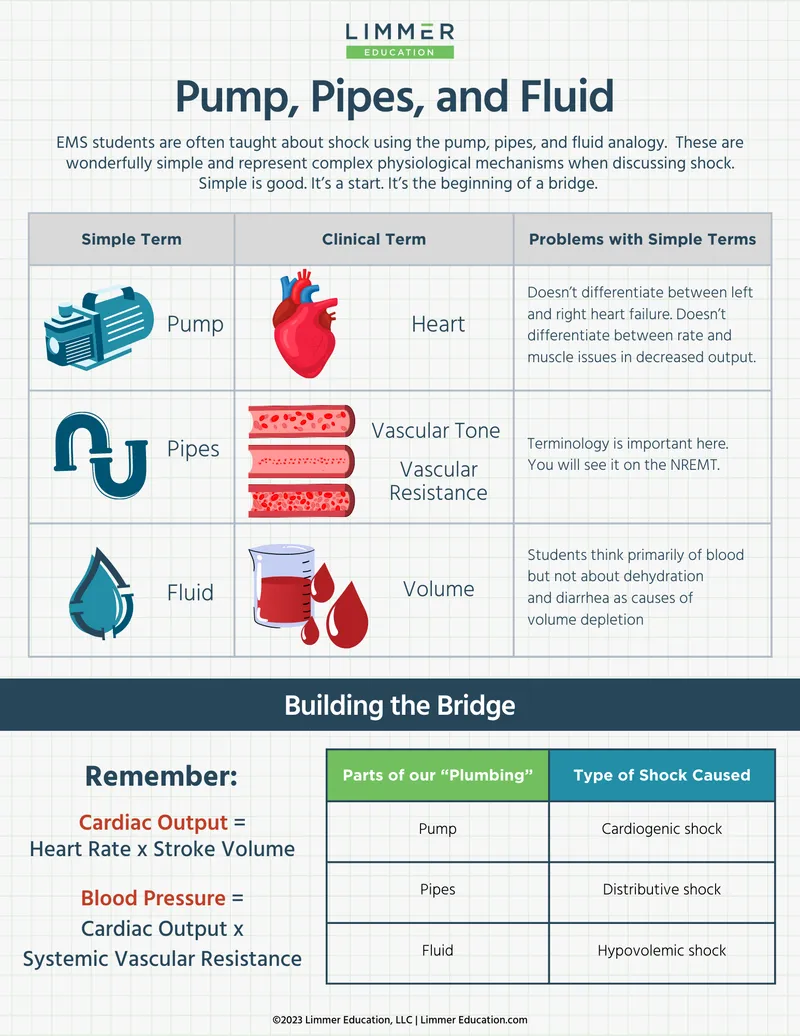
- The patient is experiencing **hypovolemic shock** due to significant blood loss, meaning their **cardiac output** is severely compromised.
- In shock, the heart attempts to compensate by increasing **heart rate**, but **stroke volume** is typically decreased due to reduced **preload**.
*Decreased sarcomere length in the myocardium*
- In situations of significant blood loss and **decreased preload**, there is less venous return to the heart, leading to reduced end-diastolic volume.
- According to the **Frank-Starling law**, reduced end-diastolic volume results in shorter initial sarcomere length, which reduces the force of contraction and thus, **stroke volume**.
*Confusion and irritability*
- **Hypovolemic shock** leads to widespread **tissue hypoperfusion**, especially to vital organs like the brain.
- Reduced cerebral blood flow results in impaired brain function, manifesting as **confusion, irritability**, and altered mental status.
*Decreased preload*
- Significant blood loss leads to a reduction in the **total circulating blood volume**.
- This reduction directly decreases the venous return to the heart, thus lowering the **end-diastolic volume** and subsequently, the **preload**.
*Increased thromboxane A2*
- In response to **vascular injury and bleeding**, the body initiates hemostasis, a critical component of which is platelet aggregation.
- **Thromboxane A2** is a potent vasoconstrictor and platelet aggregator released by activated platelets to form a **platelet plug** and help stop bleeding.
Shock pathophysiology US Medical PG Question 4: A 70-year-old woman is on hospital day 2 in the medical intensive care unit. She was admitted from the emergency department for a 2-day history of shortness of breath and fever. In the emergency department, her temperature is 39.4°C (103.0°F), the pulse is 120/min, the blood pressure is 94/54 mm Hg, the respiratory rate is 36/min, and oxygen saturation was 82% while on 4L of oxygen via a non-rebreather mask. Chest X-ray shows a right lower lobe consolidation. She was intubated, sedated, and started on broad-spectrum antibiotics for sepsis of pulmonary origin and intravenous norepinephrine for blood pressure support. Since then, her clinical condition has been stable, though her vasopressor and oxygen requirements have not improved. Today, her physician is called to the bedside because her nurse noted some slow bleeding from her intravenous line sites and around her urinary catheter. Which of the following most likely represents the results of coagulation studies for this patient?
- A. D-dimer: negative, fibrinogen level: low, platelet count: low
- B. D-dimer: elevated, fibrinogen level: normal, platelet count: normal
- C. D-dimer: elevated, fibrinogen level: low, platelet count: low (Correct Answer)
- D. D-dimer: negative, fibrinogen level: elevated, platelet count: elevated
- E. D-dimer: negative, fibrinogen level: normal, platelet count: normal
Shock pathophysiology Explanation: ***D-dimer: elevated, fibrinogen level: low, platelet count: low***
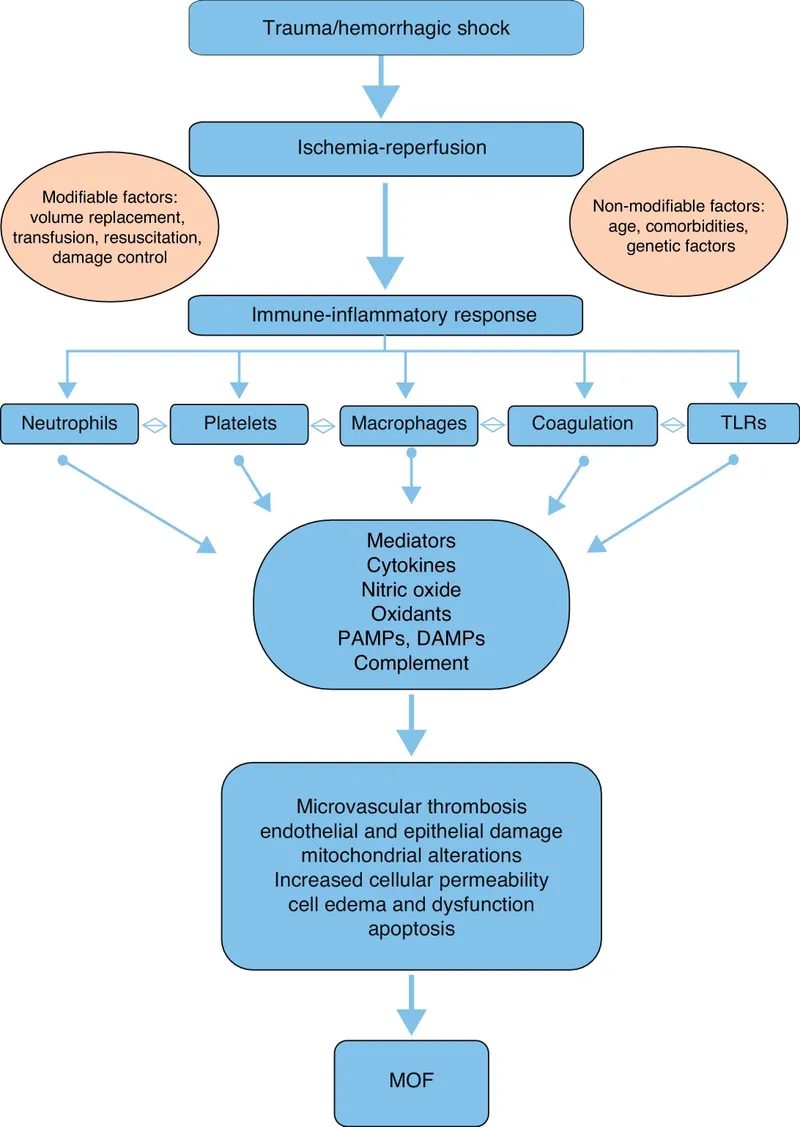
- The patient's presentation with **sepsis** requiring intubation and vasopressors, along with diffuse **bleeding from IV sites and urinary catheter**, strongly suggests **disseminated intravascular coagulation (DIC)**.
- In DIC, widespread activation of the coagulation cascade leads to consumption of **platelets** and **clotting factors (including fibrinogen)**, resulting in thrombocytopenia and hypofibrinogenemia. The breakdown of clots produces **elevated D-dimer** levels.
*D-dimer: negative, fibrinogen level: low, platelet count: low*
- A **negative D-dimer** would contradict the diagnosis of DIC, as D-dimer is a product of fibrin degradation and is almost always elevated in DIC due to extensive clot formation and subsequent fibrinolysis.
- While low fibrinogen and platelet count are characteristic of DIC, the negative D-dimer makes this option unlikely in the context of active bleeding from multiple sites.
*D-dimer: elevated, fibrinogen level: normal, platelet count: normal*
- While an **elevated D-dimer** is consistent with fibrinolysis occurring in DIC, normal **fibrinogen** and **platelet counts** would argue against the consumptive coagulopathy that defines DIC.
- The presence of diffuse bleeding in a patient with sepsis usually indicates significant depletion of clotting factors and platelets.
*D-dimer: negative, fibrinogen level: elevated, platelet count: elevated*
- This profile suggests an **inflammatory state** or a hypercoagulable state without significant fibrinolysis or consumption of clotting factors.
- A **negative D-dimer** and **elevated fibrinogen/platelets** contradict the signs and symptoms of DIC with active bleeding.
*D-dimer: negative, fibrinogen level: normal, platelet count: normal*
- This result would be inconsistent with **DIC** and the patient's clinical picture of widespread bleeding.
- In DIC, there is active coagulation and fibrinolysis, leading to consumption of platelets and fibrinogen and production of D-dimers.
Shock pathophysiology US Medical PG Question 5: A 32-year-old man is brought to the emergency department after a car accident; he was extricated after 4 hours. He did not lose consciousness and does not have headache or nausea. He is in severe pain. He sustained severe injuries to both arms and the trauma team determines that surgical intervention is needed. Urinary catheterization shows dark colored urine. His temperature is 38°C (100.4°F), pulse is 110/min, and blood pressure is 90/60 mm Hg. The patient is alert and oriented. Examination shows multiple injuries to the upper extremities, contusions on the trunk, and abdominal tenderness. Laboratory studies show:
Hemoglobin 9.2 g/dL
Leukocyte count 10,900/mm3
Platelet count 310,000/mm3
Serum
Na+ 137 mEq/L
K+ 6.8 mEq/L
Cl- 97 mEq/L
Glucose 168 mg/dL
Creatinine 1.7 mg/dL
Calcium 7.7 mg/dL
Arterial blood gas analysis on room air shows a pH of 7.30 and a serum bicarbonate of 14 mEq/L. An ECG shows peaked T waves. A FAST scan of the abdomen is negative. Two large bore cannulas are inserted and intravenous fluids are administered. Which of the following is the most appropriate next step in management?
- A. Intravenous mannitol
- B. Intravenous sodium bicarbonate
- C. Packed red blood cell transfusion
- D. Intravenous calcium gluconate (Correct Answer)
- E. Intravenous insulin
Shock pathophysiology Explanation: ***Intravenous calcium gluconate***
- The patient presents with severe **hyperkalemia** (K+ 6.8 mEq/L) and ECG changes (peaked T waves), indicating immediate cardiotoxicity risk. **Calcium gluconate** stabilizes the cardiac cell membranes, protecting the heart from the effects of high potassium.
- While other options address other issues, stabilizing the heart takes precedence in cases of extreme hyperkalemia with ECG changes.
*Intravenous mannitol*
- **Mannitol** is an osmotic diuretic used to reduce intracranial pressure or acute cerebral edema. The patient does not show signs or symptoms requiring this intervention (no consciousness loss, headache, or nausea).
- Its use here would not address the life-threatening hyperkalemia or cardiologic findings.
*Intravenous sodium bicarbonate*
- **Sodium bicarbonate** can help shift potassium intracellularly and correct metabolic acidosis, but its effect is slower and less reliable than calcium for immediate cardiac stabilization in severe hyperkalemia.
- The primary concern here is the acute cardiac risk, which calcium directly addresses.
*Packed red blood cell transfusion*
- The patient has a hemoglobin of 9.2 g/dL, indicating **anemia**, likely due to trauma. However, his blood pressure is 90/60 mm Hg despite intravenous fluids, suggesting ongoing hypovolemia or other shock.
- While addressing blood loss is important, the immediate life threat is the **cardiac instability due to hyperkalemia**, which must be managed first.
*Intravenous insulin*
- Insulin, often given with dextrose, helps shift potassium into cells. This is an effective treatment for hyperkalemia but does not provide immediate **cardiac membrane stabilization** like calcium gluconate.
- Given the peaked T waves, protecting the heart from arrhythmias is the most critical first step.
Shock pathophysiology US Medical PG Question 6: A 34-year-old male is brought to the emergency department by fire and rescue following a motor vehicle accident in which the patient was an unrestrained driver. The paramedics report that the patient was struck from behind by a drunk driver. He was mentating well at the scene but complained of pain in his abdomen. The patient has no known past medical history. In the trauma bay, his temperature is 98.9°F (37.2°C), blood pressure is 86/51 mmHg, pulse is 138/min, and respirations are 18/min. The patient is somnolent but arousable to voice and pain. His lungs are clear to auscultation bilaterally. He is diffusely tender to palpation on abdominal exam with bruising over the left upper abdomen. His distal pulses are thready, and capillary refill is delayed bilaterally. Two large-bore peripheral intravenous lines are placed to bolus him with intravenous 0.9% saline. Chest radiograph shows multiple left lower rib fractures.
Which of the following parameters is most likely to be seen in this patient?
- A. Increased cardiac output
- B. Increased mixed venous oxygen saturation
- C. Decreased pulmonary capillary wedge pressure (Correct Answer)
- D. Decreased systemic vascular resistance
- E. Increased right atrial pressure
Shock pathophysiology Explanation: ***Decreased pulmonary capillary wedge pressure***
- The patient presents with classic signs of **hemorrhagic shock** (hypotension, tachycardia, somnolence, abdominal bruising, thready pulses) due to trauma, likely involving the spleen or kidney given the left upper abdominal bruising and rib fractures.
- **Decreased pulmonary capillary wedge pressure (PCWP)** is expected in hypovolemic shock because it reflects left atrial and left ventricular end-diastolic pressure, which will be low due to reduced venous return and intravascular volume.
*Increased cardiac output*
- In **hemorrhagic shock**, the body attempts to compensate by increasing heart rate, but overall **cardiac output is typically decreased** due to profound reduction in preload (venous return) from blood loss.
- While heart rate is elevated, the stroke volume is severely diminished, leading to a net decrease in cardiac output despite compensatory efforts.
*Increased mixed venous oxygen saturation*
- **Mixed venous oxygen saturation (SvO2)** is generally **decreased in hemorrhagic shock** due to increased oxygen extraction by tissues.
- Inadequate oxygen delivery to the tissues forces them to extract more oxygen from the blood, leading to a lower SvO2.
*Decreased systemic vascular resistance*
- In **hemorrhagic shock**, the body activates compensatory mechanisms, including generalized **vasoconstriction**, to maintain blood pressure and prioritize blood flow to vital organs.
- This leads to an **increased systemic vascular resistance (SVR)**, not decreased, as reflected by the thready distal pulses and delayed capillary refill.
*Increased right atrial pressure*
- **Right atrial pressure (RAP)**, representing CVP, is typically **decreased in hemorrhagic shock** due to reduced circulating blood volume.
- A lower RAP indicates decreased venous return to the heart, a hallmark of hypovolemia.
Shock pathophysiology US Medical PG Question 7: A 27-year-old man is brought to the emergency department by emergency medical services. The patient was an unrestrained passenger in a head-on collision that occurred 15 minutes ago and is currently unresponsive. His temperature is 99.5°F (37.5°C), blood pressure is 60/33 mmHg, pulse is 180/min, respirations are 17/min, and oxygen saturation is 95% on room air. A FAST exam demonstrates fluid in Morrison’s pouch. Laboratory values are drawn upon presentation to the ED and sent off. The patient is started on IV fluids and an initial trauma survey is started. Twenty minutes later, his blood pressure is 95/65 mmHg, and his pulse is 110/min. The patient is further stabilized and is scheduled for emergency surgery. Which of the following best represents this patient’s most likely initial laboratory values?
- A. Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3
- B. Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3
- C. Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3
- D. Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3 (Correct Answer)
- E. Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3
Shock pathophysiology Explanation: ***Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3***
- The patient experienced significant trauma and is experiencing **hemorrhagic shock**, as evidenced by his initial **hypotension** (BP 60/33 mmHg), **tachycardia** (pulse 180/min), and positive **FAST exam** for fluid in Morrison's pouch, indicating intra-abdominal bleeding.
- The initial hemoglobin and hematocrit could be mildly decreased due to acute blood loss, but significant drops are often *not immediately apparent* as plasma volume has not yet moved into the intravascular compartment to dilute the remaining red blood cells. A hemoglobin of 11 g/dL and hematocrit of 33% are consistent with **acute blood loss** before significant hemodilution occurs. MCV of 88 µm^3 is within the normal range for **normocytic anemia** seen in acute hemorrhage.
*Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3*
- While a hemoglobin of 10 g/dL and hematocrit of 30% are consistent with anemia due to blood loss, an **MCV of 110 µm^3** (macrocytic) is not typically seen in acute hemorrhage.
- Macrocytic anemia usually results from conditions like **B12 or folate deficiency**, alcoholism, or liver disease, which are not suggested by the acute traumatic scenario.
*Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3*
- This indicates **polycythemia** (abnormally high red blood cell count), which is the opposite of what would be expected in a patient experiencing acute hemorrhagic shock.
- These values would suggest conditions like **polycythemia vera** or severe dehydration, which are not relevant in this acute trauma setting.
*Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3*
- While a hemoglobin of 7 g/dL and hematocrit of 21% represent significant anemia consistent with major blood loss, these values are typically seen *later* as **hemodilution** occurs, or in cases of chronic blood loss.
- An **MCV of 75 µm^3** (microcytic) is generally indicative of **iron deficiency anemia** or thalassemia, which develops over time and is not characteristic of acute traumatic blood loss.
*Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3*
- These values are within the **normal range** for hemoglobin and hematocrit, which would not be expected in a patient presenting with signs of **hemorrhagic shock** and a positive FAST exam indicating significant internal bleeding.
- This would suggest either very minor blood loss or that the values were taken before any bleeding had occurred or before hemodilution had a chance to manifest.
Shock pathophysiology US Medical PG Question 8: A 12-year-old boy admitted to the intensive care unit 1 day ago for severe pneumonia suddenly develops hypotension. He was started on empiric antibiotics and his blood culture reports are pending. According to the nurse, the patient was doing fine until his blood pressure suddenly dropped. Vital signs include: blood pressure is 88/58 mm Hg, temperature is 39.4°C (103.0°F), pulse is 120/min, and respiratory rate is 24/min. His limbs feel warm. The resident physician decides to start him on intravenous vasopressors, as the blood pressure is not responding to intravenous fluids. The on-call intensivist suspects shock due to a bacterial toxin. What is the primary mechanism responsible for the pathogenesis of this patient's condition?
- A. Inactivation of elongation factor (EF) 2
- B. Inhibition of GABA and glycine
- C. Inhibition of acetylcholine release
- D. Release of tumor necrosis factor (TNF) (Correct Answer)
- E. Degradation of lecithin in cell membranes
Shock pathophysiology Explanation: ***Release of tumor necrosis factor (TNF)***
- The patient's presentation with **warm limbs** and **hypotension** despite fluid resuscitation in the setting of severe pneumonia is highly suggestive of **septic shock**.
- **Bacterial toxins**, particularly **endotoxins** from gram-negative bacteria or **exotoxins** like superantigens, trigger a massive **inflammatory response** by stimulating immune cells to release pro-inflammatory cytokines such as **TNF-α**, IL-1, and IL-6, leading to systemic vasodilation and capillary leak.
*Inactivation of elongation factor (EF) 2*
- This is the mechanism of action of **diphtheria toxin** and **exotoxin A** from *Pseudomonas aeruginosa*.
- While these toxins can cause severe systemic illness, their primary role is not typically the induction of septic shock characterized by widespread vasodilation and warm extremities.
*Inhibition of GABA and glycine*
- This mechanism is characteristic of **tetanus toxin**, which prevents the release of inhibitory neurotransmitters and leads to spastic paralysis.
- This is not consistent with the patient's presentation of septic shock.
*Inhibition of acetylcholine release*
- This is the mechanism of action of **botulinum toxin**, which causes flaccid paralysis by blocking acetylcholine release at the neuromuscular junction.
- This effect is not associated with the pathogenesis of septic shock.
*Degradation of lecithin in cell membranes*
- This mechanism is associated with **alpha toxin** of *Clostridium perfringens* (lecithinase), which causes gas gangrene and hemolysis.
- While this toxin contributes to tissue damage in certain infections, it is not the primary mechanism behind the systemic inflammatory response and vasodilation seen in septic shock.
Shock pathophysiology US Medical PG Question 9: A 14-year-old boy presents to an urgent care clinic complaining of a runny nose that has lasted for a few weeks. He also reports sneezing attacks that last up to an hour, nasal obstruction, and generalized itching. He has similar episodes each year during the springtime that prevent him from going out with his friends or trying out for sports. His younger brother has a history of asthma. Which of the following diseases has a similar pathophysiology?
- A. Irritant contact dermatitis
- B. Dermatitis herpetiformis
- C. Allergic contact dermatitis
- D. Atopic dermatitis (Correct Answer)
- E. Systemic lupus erythematosus
Shock pathophysiology Explanation: ***Atopic dermatitis***
- This patient's symptoms are highly suggestive of **allergic rhinitis**, a **type I hypersensitivity reaction** mediated by IgE antibodies, which also underlies atopic dermatitis.
- The family history of asthma (part of the **atopic triad** – allergic rhinitis, asthma, atopic dermatitis) further supports a common underlying allergic predisposition.
*Irritant contact dermatitis*
- This is a **non-allergic inflammatory reaction** caused by direct skin irritation from chemical or physical agents, not an immunological hypersensitivity.
- It does not involve IgE-mediated mechanisms or a systemic allergic predisposition like the patient's condition.
*Dermatitis herpetiformis*
- This is a **chronic blistering skin condition** strongly associated with **celiac disease** and characterized by IgA deposition in the skin.
- It involves an autoimmune response to gluten and is not related to the IgE-mediated allergic response seen in allergic rhinitis.
*Allergic contact dermatitis*
- This is a **type IV delayed-type hypersensitivity reaction** mediated by T cells, often occurring days after exposure to an allergen (e.g., poison ivy, nickel).
- It is distinct from the immediate IgE-mediated (type I) hypersensitivity responsible for allergic rhinitis.
*Systemic lupus erythematosus*
- This is a **chronic autoimmune disease** characterized by systemic inflammation and autoantibody production against various self-antigens, leading to diverse organ involvement.
- It is a complex autoimmune disorder with different immunological mechanisms (e.g., type III hypersensitivity) rather than the IgE-mediated allergy seen in this case.
Shock pathophysiology US Medical PG Question 10: A 53-year-old woman presents to her physician for evaluation of sudden onset respiratory distress for the past few hours. The past medical history includes a myocardial infarction 2 years ago. The vital signs include a blood pressure 70/40 mm Hg, pulse 92/min, respiratory rate 28/min, and SpO2 92% on room air. The physical examination reveals bilateral basal crepitations on auscultation. The echocardiogram reveals an ejection fraction of 34%. She is admitted to the medical floor and started on furosemide. The urine output in 24 hours is 400 mL. The blood urea nitrogen is 45 mg/dL and the serum creatinine is 1.85 mg/dL. The fractional excretion of sodium is 2.4%. Urinalysis revealed muddy brown granular casts. Which of the following is the most likely cause of the abnormal urinalysis?
- A. Acute interstitial nephritis
- B. Acute tubular necrosis (Correct Answer)
- C. Acute pyelonephritis
- D. Chronic kidney disease
- E. Acute glomerulonephritis
Shock pathophysiology Explanation: ***Acute tubular necrosis***
- The presence of **muddy brown granular casts** on urinalysis is pathognomonic for **acute tubular necrosis (ATN)**, indicating damage to the renal tubules.
- The patient's history of **cardiogenic shock** (low BP 70/40 mm Hg, respiratory distress, low SpO2, low ejection fraction of 34%) led to **renal hypoperfusion** and ischemic tubular injury.
- The **fractional excretion of sodium (FENa) of 2.4%** (>2%) is characteristic of **intrinsic renal injury** (ATN), as damaged tubules cannot effectively reabsorb sodium.
- **Oliguria** (400 mL/24 hours), elevated **BUN (45 mg/dL)** and **creatinine (1.85 mg/dL)** further support acute kidney injury from ATN.
*Acute interstitial nephritis*
- This condition is typically associated with **drug hypersensitivity** (e.g., NSAIDs, antibiotics, PPIs) or **infections** and is characterized by inflammatory infiltrate in the renal interstitium.
- Urinalysis typically shows **white blood cell casts** and **eosinophiluria**, not muddy brown granular casts.
*Acute pyelonephritis*
- This is an **infection of the kidney** parenchyma, usually caused by bacterial ascension from the urinary tract.
- Symptoms often include **fever, flank pain, dysuria**, and urinalysis reveals **leukocyturia** (white blood cells) and **bacterial casts**, not muddy brown granular casts.
*Chronic kidney disease*
- While the patient has elevated creatinine and BUN, **chronic kidney disease (CKD)** develops over months to years and is characterized by persistent kidney damage or decreased function.
- Urinalysis in CKD often shows **broad waxy casts** and typically does not present with such **acute, sudden onset** of severe renal dysfunction with muddy brown granular casts.
*Acute glomerulonephritis*
- This condition involves inflammation of the glomeruli and typically presents with **hematuria, proteinuria, and red blood cell casts** (dysmorphic RBCs).
- The patient's clinical picture, including the absence of significant hematuria and the presence of **muddy brown granular casts**, does not fit acute glomerulonephritis.
More Shock pathophysiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.