Pediatric pathology principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pediatric pathology principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pediatric pathology principles US Medical PG Question 1: A 4-year-old boy is brought to his pediatrician by his mother for a physical exam before summer camp. They have no complaints or concerns at this time. He was born at 37 weeks gestation by cesarean delivery. The delivery was complicated by an omphalocele and macrosomia. During infancy and into early childhood, he struggled to breathe and eat due to an enlarged tongue. Growth and development were mostly normal with mild uneven growth of his body. He has one uncle that had similar symptoms and is alive and well. The child is up to date on all vaccines and is meeting developmental goals. He enjoys school and playing with his friends. His heart rate of 90/min, respiratory rate of 22/min, blood pressure of 110/65 mm Hg, and temperature of 36.9°C (98.4°F). Overall the child appears healthy. Physical exam findings include known hemihypertrophy of the right side along with a mildly enlarged tongue. This patient is at increased risk of developing which of the following?
- A. Sudden infant death syndrome
- B. Scoliosis
- C. Alzheimer's disease
- D. Diabetes mellitus
- E. Wilms tumor (Correct Answer)
Pediatric pathology principles Explanation: ***Wilms tumor***
- The constellation of **macrosomia**, **omphalocele**, **macroglossia**, and **hemihypertrophy** in a child points to **Beckwith-Wiedemann syndrome (BWS)**.
- Children with BWS have a significantly increased risk of developing childhood cancers, most notably **Wilms tumor** (nephroblastoma) and **hepatoblastoma**.
*Sudden infant death syndrome*
- While macrosomia can be associated with some complications, **SIDS** is not a primary or significantly increased risk for children with BWS past infancy.
- SIDS is typically defined as the sudden, unexplained death of an infant younger than one year of age.
*Scoliosis*
- **Scoliosis** is a curvature of the spine that can occur in some genetic syndromes, but it is not a hallmark or particularly increased risk feature of BWS.
- **Hemihypertrophy** in BWS can cause limb length discrepancies, which might indirectly lead to scoliosis, but it's not a direct cancer risk associated with the syndrome.
*Alzheimer's disease*
- **Alzheimer's disease** is a neurodegenerative disorder that primarily affects older adults and is not associated with childhood syndromes like BWS.
- There is no known genetic link between BWS and an increased risk of early-onset or childhood Alzheimer's.
*Diabetes mellitus*
- While individuals with BWS can have issues with **hypoglycemia** in infancy due to **pancreatic islet cell hyperplasia**, they are not typically at an increased risk of developing **type 1 or type 2 diabetes mellitus** later in childhood.
- The initial hypoglycemia usually resolves over time.
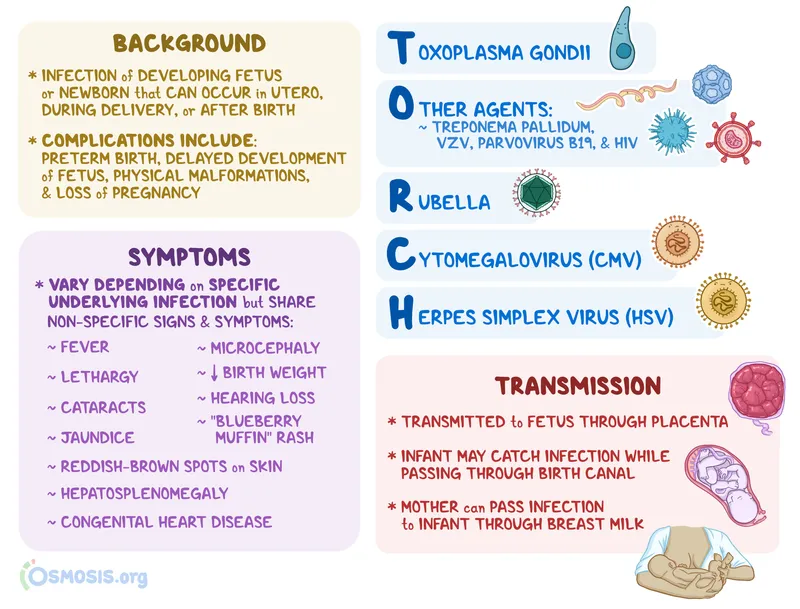
Pediatric pathology principles US Medical PG Question 2: A 28-year-old female in the 2nd trimester of pregnancy is diagnosed with primary Toxoplasma gondii infection. Her physician fears that the fetus may be infected in utero. Which of the following are associated with T. gondii infection in neonates?
- A. Hutchinson’s teeth, saddle nose, short maxilla
- B. Deafness, seizures, petechial rash
- C. Hydrocephalus, chorioretinitis, intracranial calcifications (Correct Answer)
- D. Patent ductus arteriosus, cataracts, deafness
- E. Temporal encephalitis, vesicular lesions
Pediatric pathology principles Explanation: ***Hydrocephalus, chorioretinitis, intracranial calcifications***
- These are the classic triad of symptoms (known as the **Sabin triad**) often associated with **congenital toxoplasmosis**.
- **Hydrocephalus** results from obstruction of cerebrospinal fluid flow, **chorioretinitis** can lead to vision loss, and **intracranial calcifications** are a hallmark of the infection's impact on the brain.
*Hutchinson’s teeth, saddle nose, short maxilla*
- These are characteristic features of **congenital syphilis**, not *Toxoplasma gondii* infection.
- **Hutchinson's triad** includes Hutchinson's teeth, interstitial keratitis, and sensorineural hearing loss in congenital syphilis.
*Deafness, seizures, petechial rash*
- While seizures can occur with severe congenital infections, this combination is more suggestive of **cytomegalovirus (CMV)** infection or **rubella**, which can cause petechial rash (blueberry muffin baby) and profound sensorineural deafness.
- *Toxoplasma gondii* does not typically cause a petechial rash as a primary symptom.
*Patent ductus arteriosus, cataracts, deafness*
- This constellation of symptoms is highly characteristic of **congenital rubella syndrome**.
- **Cardiac defects** (like patent ductus arteriosus), **ocular abnormalities** (cataracts), and **sensorineural deafness** are classical signs of rubella.
*Temporal encephalitis, vesicular lesions*
- **Temporal encephalitis** with vesicular lesions, particularly in a neonatal context, is a classic presentation of **congenital herpes simplex virus (HSV) infection**.
- *Toxoplasma gondii* can cause encephalitis, but not typically with vesicular lesions or a primary predilection for the temporal lobe in this specific clinical presentation.
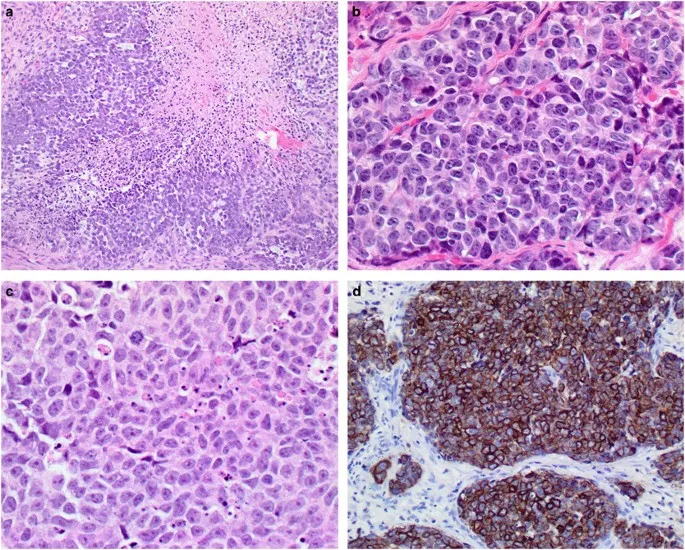
Pediatric pathology principles US Medical PG Question 3: A 4-year-old boy presents with involuntary jerks seen in his upper extremities. The patient’s mother says that “his eyes move in different directions every now and then”. Last winter, the patient had chickenpox but otherwise has always been healthy. His vital signs are a blood pressure of 100/90 mm Hg, temperature of 36.8°C (98.2°F), and respiratory rate of 17/min. On physical examination, the patient’s eyes move chaotically in all directions. Laboratory tests are unremarkable, except for a random urinary vanillylmandelic acid (VMA) level of 18 mg/g creatinine (reference range for children aged 2–4 years: < 13 mg/g creatinine). An abdominal ultrasound shows a 2 cm x 3 cm x 5 cm mass in the left adrenal gland. A biopsy of the mass reveals neuroblasts arranged in a rosette pattern. Which of the following oncogenes is most commonly associated with this condition?
- A. MYCN (Correct Answer)
- B. JAK2
- C. RET
- D. ALK
- E. KRAS
Pediatric pathology principles Explanation: ***MYCN***
- The clinical presentation with **opsoclonus-myoclonus syndrome**, elevated **urinary VMA**, an adrenal mass with a biopsy showing **neuroblasts arranged in a rosette pattern**, is classic for neuroblastoma.
- **MYCN amplification** is the most commonly associated oncogene with neuroblastoma, found in ~20-25% of cases, and is the single most important prognostic indicator of aggressive disease.
*JAK2*
- **JAK2 mutations** are primarily associated with **myeloproliferative neoplasms** (e.g., polycythemia vera, essential thrombocythemia, primary myelofibrosis), which are hematologic malignancies and do not present as an adrenal mass.
- There is no clinical or pathological evidence to suggest a myeloproliferative disorder in this patient.
*RET*
- **RET proto-oncogene mutations** are linked to **Multiple Endocrine Neoplasia type 2 (MEN2)** syndromes and **medullary thyroid carcinoma**.
- These conditions typically involve endocrine tumors and do not present with opsoclonus-myoclonus syndrome or neuroblastoma histology.
*ALK*
- **ALK gene alterations** occur in ~10-15% of neuroblastomas and can be a therapeutic target, but are **less frequently amplified than MYCN** (20-25%).
- While clinically important (especially for targeted therapy with ALK inhibitors), **MYCN amplification** remains the most common oncogenic driver and primary prognostic marker in neuroblastoma.
*KRAS*
- **KRAS mutations** are common in many adult solid tumors, such as **pancreatic adenocarcinoma**, **colorectal cancer**, and **non-small cell lung cancer**.
- They are not typically associated with neuroblastoma.
Pediatric pathology principles US Medical PG Question 4: A 5-year-old boy presents for a regularly scheduled check-up. The child is wheelchair bound due to lower extremity paralysis and suffers from urinary incontinence. At birth, it was noted that the child had lower limbs of disproportionately small size in relation to the rest of his body. Radiograph imaging at birth also revealed several abnormalities in the spine, pelvis, and lower limbs. Complete history and physical performed on the child's birth mother during her pregnancy would likely have revealed which of the following?
- A. Maternal use of nicotine
- B. Maternal use of tetracyclines
- C. Maternal hyperthyroidism
- D. Maternal use of lithium
- E. Uncontrolled maternal diabetes mellitus (Correct Answer)
Pediatric pathology principles Explanation: ***Uncontrolled maternal diabetes mellitus***
- **Maternal diabetes** is a significant risk factor for **caudal regression syndrome**, which presents with **lower limb paralysis**, **urinary incontinence**, and **spinal/pelvic abnormalities**.
- The combination of disproportionately small lower limbs and the associated neurological and skeletal issues strongly points to a congenital anomaly linked to **poor glycemic control** during pregnancy.
*Maternal use of nicotine*
- Maternal nicotine use is associated with a range of adverse pregnancy outcomes, including **low birth weight**, **premature birth**, and **respiratory problems**, but not typically caudal regression syndrome.
- While concerning, it does not directly explain the specific constellation of skeletal, neurological, and urological abnormalities described.
*Maternal use of tetracyclines*
- **Tetracycline exposure** during pregnancy can lead to **tooth discoloration** and **bone growth inhibition**, particularly in the developing fetus.
- It is not known to cause the severe spinal and lower limb malformations, paralysis, or urinary incontinence seen in this case.
*Maternal hyperthyroidism*
- Uncontrolled maternal hyperthyroidism can lead to complications such as **fetal tachycardia**, **goiter**, and **preterm birth**.
- It is not directly associated with congenital malformations like caudal regression syndrome that affect the lower spine and limbs.
*Maternal use of lithium*
- Maternal lithium use is most notably associated with an increased risk of **Ebstein's anomaly**, a congenital **heart defect**.
- It does not explain the specific musculoskeletal, neurological, and urological abnormalities presented in the case.
Pediatric pathology principles US Medical PG Question 5: A 3-day-old female newborn delivered vaginally at 36 weeks to a 27-year-old woman has generalized convulsions lasting 3 minutes. Prior to the event, she was lethargic and had difficulty feeding. The infant has two healthy older siblings and the mother's immunizations are up-to-date. The infant appears icteric. The infant's weight and length are at the 5th percentile, and her head circumference is at the 99th percentile for gestational age. There are several purpura of the skin. Ocular examination shows posterior uveitis. Cranial ultrasonography shows ventricular dilatation, as well as hyperechoic foci within the cortex, basal ganglia, and periventricular region. Which of the following is the most likely diagnosis?
- A. Congenital parvovirus infection
- B. Congenital Toxoplasma gondii infection (Correct Answer)
- C. Congenital Treponema pallidum infection
- D. Congenital cytomegalovirus infection
- E. Congenital rubella infection
Pediatric pathology principles Explanation: ***Congenital Toxoplasma gondii infection***
- **Ventricular dilatation** with widespread **hyperechoic foci** (calcifications) in the brain, along with **posterior uveitis**, highly suggests congenital toxoplasmosis.
- Other features like **generalized convulsions**, **icterus**, **purpura**, and **microcephaly** (indicated by 5th percentile weight/length vs 99th percentile head circumference discrepancy suggesting hydrocephalus with macrocephaly) are also consistent with this diagnosis.
*Congenital parvovirus infection*
- Primarily causes severe **anemia**, **hydrops fetalis**, and **myocarditis**; it does not typically present with extensive cerebral calcifications or uveitis.
- While it can lead to neurological issues, the specific brain imaging findings and ocular involvement described are not characteristic.
*Congenital Treponema pallidum infection*
- Characterized by rhinitis (**snuffles**), **hepatosplenomegaly**, **bone abnormalities** (e.g., osteochondritis), and **rash**.
- While it can cause CNS involvement and developmental delays, the distinct pattern of brain calcifications and uveitis is not typical.
*Congenital cytomegalovirus infection*
- Can cause **periventricular calcifications**, but the widespread, diffuse calcifications (cortex, basal ganglia, periventricular) are less typical than with toxoplasmosis, which often shows more diffuse parenchymal calcifications.
- While it shares features like small for gestational age, icterus, and purpura, **posterior uveitis** is more strongly associated with toxoplasmosis.
*Congenital rubella infection*
- Classic triad includes **cataracts** (or glaucoma), **sensorineural hearing loss**, and **congenital heart defects** (e.g., PDA, pulmonary artery stenosis).
- While CNS involvement (e.g., intellectual disability, microcephaly) can occur, the widespread cerebral calcifications and posterior uveitis are not characteristic.
Pediatric pathology principles US Medical PG Question 6: A 3000-g (6.6-lb) female newborn is delivered at term to a 23-year-old primigravid woman. The mother has had no prenatal care. Immunization records are not available. Cardiac examination shows a continuous heart murmur. There are several bluish macules on the skin that do not blanch with pressure. Slit lamp examination shows cloudy lenses in both eyes. The newborn does not pass his auditory screening tests. Which of the following is the most likely diagnosis?
- A. Congenital parvovirus infection
- B. Congenital cytomegalovirus infection
- C. Congenital rubella infection (Correct Answer)
- D. Congenital syphilis
- E. Congenital toxoplasmosis
Pediatric pathology principles Explanation: ***Congenital rubella infection***
- The classic triad of congenital rubella includes **sensorineural hearing loss**, **ocular abnormalities** (e.g., cataracts, glaucoma), and **cardiac defects** (e.g., patent ductus arteriosus, pulmonary artery stenosis), all of which are present in this case.
- The **blueberry muffin rash** (bluish macules) is also a characteristic, although non-specific, finding due to **extramedullary hematopoiesis**.
*Congenital parvovirus infection*
- Primarily causes **hydrops fetalis**, severe **anemia**, and fetal demise, often without the specific cardiac, ocular, and auditory defects described.
- While it can cause skin lesions, the constellation of findings strongly points away from parvovirus.
*Congenital cytomegalovirus infection*
- Can cause **sensorineural hearing loss** and central nervous system abnormalities (e.g., **periventricular calcifications**, microcephaly), but **cardiac defects** and **cataracts** are less common than with rubella.
- The typical skin lesions are often petechiae or purpura, not the distinct bluish macules seen here.
*Congenital syphilis*
- Presents with a wide range of manifestations, including **hepatosplenomegaly**, **rash** (often maculopapular or desquamating), **saddle nose deformity**, and bone abnormalities.
- While it can cause some ocular (e.g., interstitial keratitis) and auditory issues, the specific combination of **cataracts**, **patent ductus arteriosus**, and **sensorineural deafness** is not its hallmark.
*Congenital toxoplasmosis*
- Characterized by the classic triad of **chorioretinitis**, **hydrocephalus**, and **intracranial calcifications**.
- While it can cause hearing loss and some skin manifestations, the cardiac defect and cataracts described are not typical features.
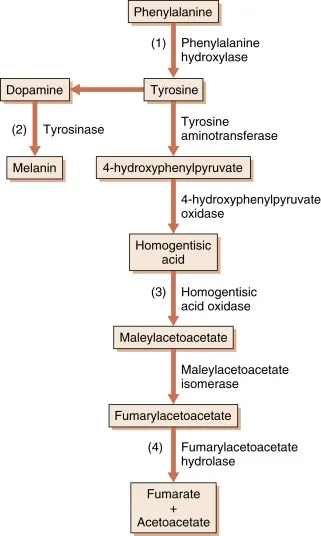
Pediatric pathology principles US Medical PG Question 7: A 2-day-old newborn boy is brought to the emergency department because of apnea, cyanosis, and seizures. He is severely hypoglycemic and does not improve with glucagon administration. His blood pressure is 100/62 mm Hg and heart rate is 75/min. Blood tests show high lactate levels. Physical examination is notable for hepatomegaly. Which of the following enzymes is most likely to be deficient in this baby?
- A. α-ketoacid dehydrogenase
- B. Phenylalanine hydroxylase
- C. Glucose-6-phosphatase (Correct Answer)
- D. Glucocerebrosidase
- E. Sphingomyelinase
Pediatric pathology principles Explanation: ***Correct: Glucose-6-phosphatase***
- The presentation of severe **hypoglycemia** not responsive to glucagon, coupled with **hepatomegaly** and **lactic acidosis** in a neonate, is highly suggestive of **Type I glycogen storage disease (von Gierke disease)**.
- Deficiency of **glucose-6-phosphatase** prevents the liver from releasing glucose into the bloodstream (the final step of both gluconeogenesis and glycogenolysis), leading to profound hypoglycemia.
- **Key diagnostic clue**: Lack of response to glucagon occurs because glucagon stimulates glycogenolysis, but without functional glucose-6-phosphatase, glucose-6-phosphate cannot be converted to free glucose for release.
- Accumulated glucose-6-phosphate shunts to glycolysis, producing **lactate** (lactic acidosis), and to glycogen synthesis, causing **hepatomegaly**.
*Incorrect: α-ketoacid dehydrogenase*
- Deficiency of **branched-chain α-ketoacid dehydrogenase** causes **maple syrup urine disease (MSUD)**, which presents with poor feeding, vomiting, lethargy, and a characteristic maple syrup odor in urine.
- While MSUD can cause neurological symptoms and seizures, **severe hypoglycemia unresponsive to glucagon** and **hepatomegaly** as primary features are not typical.
*Incorrect: Phenylalanine hydroxylase*
- Deficiency in **phenylalanine hydroxylase** causes **phenylketonuria (PKU)**, which is primarily characterized by intellectual disability, seizures (if untreated), and a musty odor, usually manifesting later in infancy.
- PKU does not present with acute neonatal hypoglycemia, lactic acidosis, or hepatomegaly.
*Incorrect: Glucocerebrosidase*
- Deficiency in **glucocerebrosidase** leads to **Gaucher disease**, a lysosomal storage disorder characterized by hepatosplenomegaly, bone crises, and neurological symptoms in severe infantile forms.
- While hepatomegaly may be present, Gaucher disease does not cause acute, severe neonatal hypoglycemia, lactic acidosis, or lack of response to glucagon.
*Incorrect: Sphingomyelinase*
- Deficiency in **sphingomyelinase** causes **Niemann-Pick disease**, another lysosomal storage disorder, which typically presents with hepatosplenomegaly, neurological deterioration, and "cherry-red spots" in the retina.
- This condition does not cause acute neonatal hypoglycemia, lactic acidosis, or glucagon unresponsiveness.
Pediatric pathology principles US Medical PG Question 8: A 7-month-old boy is brought to the pediatrician for a change in his behavior. The patient has been exclusively breastfeeding up until this point and has been meeting his developmental milestones. He is in the 90th percentile for weight and 89th percentile for height. Two weeks ago, his parents began introducing weaning foods including fruit purees and baby formula. This past week, the patient has been increasingly lethargic, vomiting, and has been refusing to eat. The patient's parents state that he had an episode this morning where he was not responsive and was moving his extremities abnormally followed by a period of somnolence. The patient's past medical history is notable for shoulder dystocia and poorly managed maternal diabetes during the pregnancy. His temperature is 99.5°F (37.5°C), blood pressure is 60/30 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you note a lethargic infant with a distinctive sweet, fruity smell to his breath. Which of the following is most likely deficient in this patient?
- A. Branched chain alpha-ketoacid dehydrogenase (Correct Answer)
- B. Galactose-1-phosphate uridyltransferase
- C. Aldolase B
- D. Glucose-6-phosphatase
- E. Ornithine transcarbamolase
Pediatric pathology principles Explanation: ***Branched chain alpha-ketoacid dehydrogenase***
- This patient's presentation is classic for **maple syrup urine disease (MSUD)**, caused by deficiency of branched chain alpha-ketoacid dehydrogenase complex.
- The **distinctive sweet, fruity smell to the breath** (and urine) is pathognomonic for MSUD, resulting from accumulation of branched chain amino acids (leucine, isoleucine, valine) and their ketoacid metabolites.
- Symptoms typically manifest upon introduction of **increased protein load** (baby formula), presenting with **lethargy, vomiting, poor feeding, seizures, and encephalopathy** due to neurotoxicity from elevated leucine and other metabolites.
- The timing (introduced weaning foods including formula) and clinical picture of acute metabolic crisis with characteristic odor make this the most likely diagnosis.
*Ornithine transcarbamylase*
- OTC deficiency causes **hyperammonemic crisis** with similar neurological symptoms (lethargy, vomiting, seizures) triggered by protein intake.
- However, hyperammonemia typically produces a **musty or ammonia-like odor**, NOT the sweet, fruity smell described in this case.
- While the clinical timing fits, the **characteristic breath odor is inconsistent** with urea cycle disorders.
*Galactose-1-phosphate uridyltransferase*
- Deficiency causes **classic galactosemia**, presenting with **vomiting, lethargy, jaundice, hepatomegaly, and cataracts** after lactose exposure (milk/formula).
- The **sweet, fruity breath odor is NOT characteristic** of galactosemia.
- While formula introduction could trigger symptoms, the specific odor and predominant neurological presentation point away from this diagnosis.
*Aldolase B*
- **Hereditary fructose intolerance** manifests upon fructose exposure (fruit purees) with **vomiting, hypoglycemia, jaundice, hepatomegaly, and renal dysfunction**.
- The patient did consume fruit purees, but the **sweet, fruity breath odor is NOT a feature** of fructose intolerance.
- The severe acute encephalopathy and characteristic odor make MSUD more likely.
*Glucose-6-phosphatase*
- **Von Gierke disease (Type I GSD)** presents with **severe fasting hypoglycemia, lactic acidosis, hepatomegaly, and hyperlipidemia**.
- The **sweet, fruity odor is NOT characteristic**, and symptoms are primarily related to fasting/glucose homeostasis rather than acute protein-induced metabolic crisis.
- The clinical picture does not fit a glycogen storage disorder.
Pediatric pathology principles US Medical PG Question 9: A 12-year-old boy is brought to the emergency department after he vomited and said he was having double vision in school. He also says that he has been experiencing morning headaches, nausea, and dizziness over the last month. He has no past medical history and is not taking any medications. Physical exam reveals a broad-based gait, dysmetria on finger-to-nose testing, and nystagmus. Both serum and urine toxicology are negative, and radiography reveals a solid mass in the midline cerebellum that enhances after contrast administration. Biopsy of this lesion reveals cells of primitive neuroectodermal origin. Which of the following would most likely be seen on histology of this lesion?
- A. Rosettes with small blue cells (Correct Answer)
- B. Rosenthal fibers
- C. Tooth enamel-like calcification
- D. Foamy cells and high vascularity
- E. Perivascular pseudorosettes
Pediatric pathology principles Explanation: ***Rosettes with small blue cells***
- The description of a **midline cerebellar mass** in a child, presenting with signs of **increased intracranial pressure (headaches, vomiting, double vision)** and **cerebellar dysfunction (broad-based gait, dysmetria, nystagmus)**, is classic for **medulloblastoma**.
- **Medulloblastomas** are primitive neuroectodermal tumors (PNETs) known for their distinctive histology of **small, round, blue cells** forming **Homer-Wright rosettes**.
*Rosenthal fibers*
- **Rosenthal fibers** are eosinophilic, corkscrew-shaped structures that are characteristic histological features of **pilocytic astrocytomas**.
- While pilocytic astrocytomas can be cerebellar and common in children, the question describes a "solid mass of primitive neuroectodermal origin" rather than the typical cystic lesion with mural nodule associated with pilocytic astrocytomas, and the aggressive presentation points away from pilocytic astrocytoma.
*Tooth enamel-like calcification*
- **Tooth enamel-like calcification** is a pathognomonic feature of **craniopharyngiomas**, which are typically supratentorial (in the sellar region) and cause symptoms related to pituitary dysfunction and optic chiasm compression, not cerebellar dysfunction.
- The location and symptoms provided in the vignette do not match the typical presentation of a craniopharyngioma.
*Foamy cells and high vascularity*
- **Foamy cells and high vascularity** are characteristic features of **hemangioblastomas**, which are typically seen in adults, often associated with **von Hippel-Lindau disease**, and are more commonly located in the cerebellum.
- However, the patient's age (12-year-old) and the description of cells of "primitive neuroectodermal origin" do not align with the typical presentation or origin of hemangioblastomas.
*Perivascular pseudorosettes*
- **Perivascular pseudorosettes** are the classic histological finding in **ependymomas**, another common pediatric brain tumor.
- While ependymomas can occur in the posterior fossa, they typically arise from the floor of the fourth ventricle and are not described as having primitive neuroectodermal origin in the same way medulloblastomas are, and the specific rosettes formed by medulloblastomas are Homer-Wright rosettes.
Pediatric pathology principles US Medical PG Question 10: A 32-year-old woman presents to her primary care physician for an annual checkup. She reports that she has been feeling well and has no medical concerns. Her past medical history is significant for childhood asthma but she has not experienced any symptoms since she was a teenager. Physical exam reveals a 1-centimeter hard mobile mass in the left upper outer quadrant of her breast. A mammogram was performed and demonstrated calcifications within the mass so a biopsy was obtained. The biopsy shows acinar proliferation with intralobular fibrosis. Which of the following conditions is most likely affecting this patient?
- A. Sclerosing adenosis (Correct Answer)
- B. Fibroadenoma
- C. Cystic hyperplasia
- D. Invasive lobular carcinoma
- E. Infiltrating ductal carcinoma
Pediatric pathology principles Explanation: ***Sclerosing adenosis***
- This condition is characterized by **acinar proliferation with intralobular fibrosis**, which exactly matches the biopsy findings mentioned in the vignette.
- Sclerosing adenosis can present as a palpable mass with **calcifications on mammography**, mimicking carcinoma, necessitating biopsy for definitive diagnosis.
*Fibroadenoma*
- Characterized by proliferation of both **stromal and epithelial elements**, often forming well-circumscribed, mobile masses.
- While it can present as a mobile mass, the specific histological finding of "acinar proliferation with intralobular fibrosis" is not the primary descriptive characteristic of a fibroadenoma.
*Cystic hyperplasia*
- This term, often used interchangeably with **fibrocystic changes**, involves the formation of cysts and an increase in fibrous tissue.
- While it can involve hyperplasia, it doesn't typically describe the distinct pattern of "acinar proliferation with intralobular fibrosis" as seen in sclerosing adenosis.
*Invasive lobular carcinoma*
- This carcinoma is characterized by its **infiltrative growth pattern** often in single file lines, and typically does not form a well-defined mass.
- While it can present with calcifications, the absence of overt malignant features and the specific benign histological description rule out this diagnosis.
*Infiltrating ductal carcinoma*
- The most common type of breast cancer, characterized by **malignant epithelial cells infiltrating the stroma**.
- The biopsy findings described ("acinar proliferation with intralobular fibrosis") are features of a benign process, not a malignant one.
More Pediatric pathology principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.