Nutritional diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nutritional diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nutritional diseases US Medical PG Question 1: A 21-year-old woman presents to the clinic complaining of fatigue for the past 2 weeks. She reports that it is difficult for her to do strenuous tasks such as lifting heavy boxes at the bar she works at. She denies any precipitating factors, weight changes, nail changes, dry skin, chest pain, abdominal pain, or urinary changes. She is currently trying out a vegetarian diet for weight loss and overall wellness. Besides heavier than usual periods, the patient is otherwise healthy with no significant medical history. A physical examination demonstrates conjunctival pallor. Where in the gastrointestinal system is the most likely mineral that is deficient in the patient absorbed?
- A. Large intestine
- B. Ileum
- C. Jejunum
- D. Stomach
- E. Duodenum (Correct Answer)
Nutritional diseases Explanation: ***Duodenum***
- The patient's symptoms (fatigue, conjunctival pallor, heavy periods, vegetarian diet) are highly suggestive of **iron deficiency anemia**. The **duodenum** is the primary site for the absorption of dietary iron.
- Iron absorption is tightly regulated here to maintain iron homeostasis, and conditions like a vegetarian diet can reduce bioavailable iron, leading to deficiency.
*Large intestine*
- The large intestine is primarily involved in **water and electrolyte absorption** and the formation of stool.
- It does not play a significant role in the absorption of essential minerals like iron.
*Ileum*
- The ileum is the main site for the absorption of **bile salts** and **vitamin B12**.
- While it absorbs some nutrients, it is not the primary site for iron absorption.
*Jejunum*
- The jejunum is the main site for the absorption of most **nutrients**, including carbohydrates, proteins, and fats.
- While some iron absorption can occur here, the **duodenum** is the specialized and most significant site for this process.
*Stomach*
- The stomach's main roles include **digestion** of proteins and production of **intrinsic factor** for vitamin B12 absorption.
- While **acidic pH** in the stomach aids in converting ferric iron (Fe3+) to ferrous iron (Fe2+), which is more readily absorbed, direct iron absorption in the stomach lining is minimal.
Nutritional diseases US Medical PG Question 2: A 27-year-old female presents to general medical clinic for a routine checkup. She has a genetic disease marked by a mutation in a chloride transporter. She has a history of chronic bronchitis. She has a brother with a similar history of infections as well as infertility. Which of the following is most likely true regarding a potential vitamin deficiency complication secondary to this patient's chronic illness?
- A. It may result in connective tissue defects
- B. It may result in corneal vascularization
- C. It may result in the triad of confusion, ophthalmoplegia, and ataxia
- D. It may manifest itself as a prolonged PT (Correct Answer)
- E. It may be exacerbated by excessive ingestion of raw eggs
Nutritional diseases Explanation: ***It may manifest itself as a prolonged PT***
- The patient's presentation with a **chloride transporter mutation**, chronic bronchitis, and a brother with similar infections and infertility is highly suggestive of **cystic fibrosis (CF)**.
- CF leads to **pancreatic insufficiency** and **malabsorption of fat-soluble vitamins (A, D, E, K)**. A deficiency in **vitamin K** can result in impaired synthesis of **clotting factors**, leading to a **prolonged prothrombin time (PT)**.
*It may result in connective tissue defects*
- This symptom is characteristic of **vitamin C deficiency (scurvy)**, which manifests as impaired **collagen synthesis** and fragile connective tissues.
- While CF patients can have various deficiencies, connective tissue defects are not a primary consequence of the fat-soluble vitamin deficiencies associated with CF.
*It may result in corneal vascularization*
- **Corneal vascularization** is typically associated with **riboflavin (vitamin B2) deficiency** or chronic ocular inflammation.
- This is not a common complication of the fat-soluble vitamin malabsorption seen in cystic fibrosis.
*It may result in the triad of confusion, ophthalmoplegia, and ataxia*
- This triad describes **Wernicke-Korsakoff syndrome**, which is caused by a **thiamine (vitamin B1) deficiency**.
- This deficiency is common in alcoholism or severe malnutrition but is not a direct complication of the fat-soluble vitamin malabsorption in cystic fibrosis.
*It may be exacerbated by excessive ingestion of raw eggs*
- Excessive ingestion of raw eggs can lead to **biotin (vitamin B7) deficiency** due to **avidin** binding to biotin, preventing its absorption.
- While CF patients can have various nutritional issues, this specific interaction is unrelated to the fat-soluble vitamin deficiencies caused by their pancreatic insufficiency.
Nutritional diseases US Medical PG Question 3: A 35-year-old alcoholic patient presents with high-output cardiac failure, tachycardia, a bounding pulse, and warm extremities. Blood work reveals vitamin deficiency. Which of the following vitamin deficiencies is most likely associated with such a clinical presentation?
- A. Thiamine (Correct Answer)
- B. Riboflavin
- C. Vitamin B12
- D. Vitamin D
- E. Niacin
Nutritional diseases Explanation: ***Thiamine***
- **Thiamine deficiency**, particularly in alcoholics, can lead to **wet beriberi**, characterized by **high-output cardiac failure** due to peripheral vasodilation, resulting in symptoms like tachycardia, bounding pulse, and warm extremities.
- Thiamine (vitamin B1) is a crucial cofactor in carbohydrate metabolism, and its deficiency impairs myocardial energy production and causes systemic vasodilation.
*Riboflavin*
- **Riboflavin deficiency** (ariboflavinosis) typically presents with **cheilosis**, glossitis, angular stomatitis, and seborrheic dermatitis, and is not directly associated with high-output cardiac failure.
- While it can occur in alcoholics, cardiac failure is not a prominent feature.
*Vitamin B12*
- **Vitamin B12 deficiency** primarily causes **megaloblastic anemia** and neurological symptoms such as **peripheral neuropathy**, ataxia, and cognitive impairment, rather than high-output cardiac failure.
- Cardiac manifestations are usually due to severe anemia leading to compensatory high output, but not the primary cause as seen in thiamine deficiency.
*Vitamin D*
- **Vitamin D deficiency** is associated with **osteomalacia** in adults and rickets in children, leading to bone pain, muscle weakness, and increased fracture risk.
- It does not cause high-output cardiac failure or related cardiovascular symptoms.
*Niacin*
- **Niacin deficiency** (pellagra) is characterized by the "3 Ds": **dermatitis**, **diarrhea**, and **dementia**, along with glossitis and stomatitis.
- While cardiovascular symptoms can occur in severe cases, high-output cardiac failure with a bounding pulse is not a typical hallmark of pellagra.
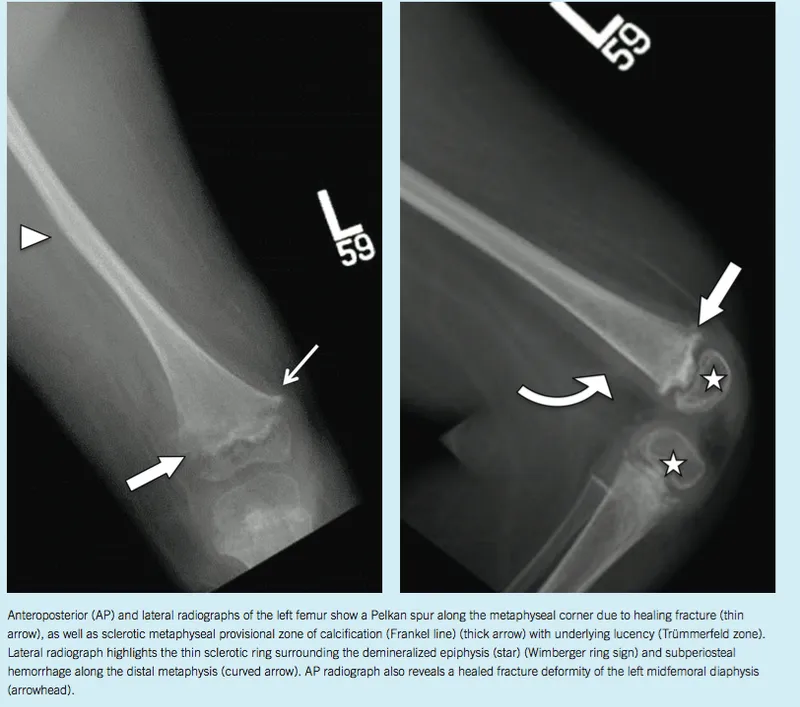
Nutritional diseases US Medical PG Question 4: A 7-year-old girl presents to her primary care physician for a routine check-up. The physician allows the medical student to perform a physical examination. The medical student notes hearing impairment as well as the findings show in Figures A and B. Radiographs show indications of multiple old fractures of the humerus that have healed. After questioning the girl’s parents, the medical student learns that in addition, the patient is extremely picky with her food and eats a diet consisting mainly of cereal and pasta. What is the most likely etiology of the patient’s disease?
- A. Dietary deficiency of ascorbic acid
- B. Defect in type I collagen (Correct Answer)
- C. Defective mineralization of cartilage
- D. Decreased bone mineral density
- E. Non-accidental trauma
Nutritional diseases Explanation: ***Defect in type I collagen***
- The constellation of **frequent fractures**, **hearing impairment**, and **blue sclerae** (as indicated by Figure A, which shows a bluish tint to the white part of the eye) is characteristic of **osteogenesis imperfecta (OI)**, a genetic disorder caused by mutations in COL1A1 or COL1A2 genes leading to **defective type I collagen synthesis**.
- Type I collagen is the primary structural protein in bone, and defects result in brittle bones, blue sclerae (due to thin sclera allowing choroid visibility), and conductive hearing loss (from ossicle abnormalities).
- While the patient's diet is described as "picky," the primary features point towards a genetic collagen defect rather than a nutritional deficiency as the underlying cause for the bone and connective tissue abnormalities.
*Dietary deficiency of ascorbic acid*
- A deficiency in **ascorbic acid (vitamin C)** leads to **scurvy**, characterized by **gingivitis**, **poor wound healing**, **petechiae**, and easy bruising due to impaired collagen synthesis.
- While collagen synthesis is affected, the specific presentation of blue sclerae, hearing impairment, and multiple fractures as primary symptoms is not typical for scurvy.
*Defective mineralization of cartilage*
- **Defective mineralization of cartilage** often points to **rickets in children** or **osteomalacia in adults**, usually due to **vitamin D deficiency** or disorders of phosphate metabolism.
- While these conditions can cause bone fragility, they do not typically present with blue sclerae or hearing impairment as defining features. The "old fractures" suggest a chronic bone fragility predating any acute nutritional issues.
*Decreased bone mineral density*
- **Decreased bone mineral density (BMD)** is a general term seen in many conditions, including **osteoporosis** and **osteogenesis imperfecta**.
- While the patient likely has decreased BMD due to their frequent fractures, this option describes a symptom rather than the **underlying etiology** of the disorder.
*Non-accidental trauma*
- **Non-accidental trauma (child abuse)** should always be considered in a child with multiple fractures.
- However, the presence of other systemic findings like **blue sclerae** and **hearing impairment** strongly suggests an underlying genetic disorder like osteogenesis imperfecta, making non-accidental trauma less likely as the primary cause for all observed symptoms.
Nutritional diseases US Medical PG Question 5: A 21-year-old woman is admitted to the hospital for severe malnutrition with a BMI of 15 kg/m2. Past medical history is significant for chronic anorexia nervosa. During the course of her stay, she is treated with parenteral fluids and nutrition management. On the 4th day, her status changes. Her blood pressure is 110/75 mm Hg, heart rate is 120/min, respiratory rate is 25/min, and temperature is 37.0°C (98.6°F). On physical exam, her heart is tachycardic with a regular rhythm and her lungs are clear to auscultation bilaterally. She appears confused, disoriented, and agitated. Strength in her lower extremities is 4/5. What is the next step in management?
- A. MRI of the brain
- B. Administer insulin
- C. Measure electrolytes (Correct Answer)
- D. Arrange for outpatient counseling
- E. Doppler ultrasound on lower extremities
Nutritional diseases Explanation: ***Measure electrolytes***
- The patient's presentation with **confusion, disorientation, agitation**, and **lower extremity weakness** after refeeding for severe **malnutrition** is highly suggestive of **refeeding syndrome**. This syndrome is characterized by severe electrolyte shifts, particularly **hypophosphatemia**, **hypokalemia**, and **hypomagnesemia**.
- Measuring electrolytes immediately is crucial to diagnose and then correct these imbalances, which can lead to life-threatening complications like **cardiac arrhythmias**, **respiratory failure**, and **seizures**.
*MRI of the brain*
- While neurological symptoms are present, a brain MRI is not the immediate first step given the context of refeeding in a severely malnourished patient.
- The symptoms are more consistent with **metabolic derangements** associated with **refeeding syndrome** than an acute primary neurological event.
*Administer insulin*
- Administering insulin without knowing the patient's glucose or electrolyte status could be dangerous, especially given the increased risk of **hypokalemia** and **hypophosphatemia** in refeeding syndrome, which insulin can exacerbate.
- Refeeding syndrome typically involves glucose shifts, but **hypoglycemia** is not the primary immediate concern, and hyperinsulinemia in this context can cause cellular uptake of electrolytes leading to further depletion.
*Arrange for outpatient counseling*
- The patient is acutely ill and experiencing a potentially life-threatening complication requiring immediate medical intervention.
- **Outpatient counseling** is not appropriate for an acute hospital admission with severe, rapidly changing symptoms.
*Doppler ultrasound on lower extremities*
- While immobility can increase the risk of deep vein thrombosis (DVT), the patient's symptoms of **confusion, agitation, tachycardia, tachypnea**, and **weakness** are not primary indicators of DVT.
- The clinical picture points strongly towards **metabolic complications** of refeeding.
Nutritional diseases US Medical PG Question 6: A 60-year-old male presents with fatigue, dyspnea on exertion, and lower extremity edema. Physical examination reveals an elevated jugular venous pressure and an S3 heart sound. Which of the following medications is most likely to improve this patient's symptoms?
- A. Metoprolol
- B. Furosemide (Correct Answer)
- C. Losartan
- D. Lisinopril
- E. Spironolactone
Nutritional diseases Explanation: ***Correct: Furosemide***
- The patient presents with classic signs of **heart failure with fluid overload**: dyspnea on exertion, lower extremity edema, elevated jugular venous pressure, and an S3 heart sound (indicating volume overload).
- **Furosemide**, a **loop diuretic**, is the most effective medication for **rapid symptomatic relief** in heart failure with congestion. It works by blocking sodium and water reabsorption in the loop of Henle, promoting diuresis and reducing **pulmonary congestion** and **peripheral edema**.
- While other medications like ACE inhibitors, beta-blockers, and aldosterone antagonists are crucial for **long-term mortality reduction** and disease modification, loop diuretics provide the **fastest and most direct symptomatic improvement** for fluid overload.
*Incorrect: Metoprolol*
- **Metoprolol** is a **beta-blocker** that is essential for chronic HFrEF management, providing **mortality reduction** and **reverse cardiac remodeling**.
- However, beta-blockers take **weeks to months** to show symptomatic benefit and can initially **worsen symptoms** due to negative inotropic effects, especially in acute decompensation.
- While important for long-term management, metoprolol does not provide immediate symptomatic relief from fluid overload.
*Incorrect: Losartan*
- **Losartan** is an **angiotensin receptor blocker (ARB)** used as an alternative to ACE inhibitors in HFrEF, particularly in patients who develop cough with ACE inhibitors.
- ARBs reduce **afterload** and prevent **cardiac remodeling**, contributing to improved long-term outcomes and mortality reduction.
- However, they do not directly address fluid overload and do not provide rapid symptomatic relief compared to diuretics.
*Incorrect: Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that improves mortality in HFrEF by preventing myocardial fibrosis, reducing cardiac remodeling, and preventing potassium loss.
- While beneficial for long-term management, spironolactone has **weak diuretic effects** and takes weeks to provide symptomatic benefit.
- It is not the first-line choice for **acute symptomatic relief** of volume overload, though it is an important component of chronic HFrEF therapy.
*Incorrect: Lisinopril*
- **Lisinopril** is an **ACE inhibitor** and a cornerstone of HFrEF therapy, reducing **mortality**, **hospitalizations**, and preventing **cardiac remodeling** by reducing afterload and preload.
- While ACE inhibitors improve symptoms over time, they do not provide the **rapid diuretic effect** needed for immediate relief of dyspnea and edema.
- Lisinopril is essential for long-term management but is not the most effective option for acute symptomatic improvement of fluid overload.
Nutritional diseases US Medical PG Question 7: A 17-year-old girl is brought in by her mother due to rapid weight loss over the past month. The patient says she has been having episodes of diarrhea, which she attributes to laxatives she takes regularly to keep her weight down. She also says she has not had her period yet. The patient’s mother adds that the patient has been underperforming at school and acting very strangely at home. Her current BMI is 16.8 kg/m2. On physical examination, the skin on her limbs and around her neck is inflamed and erythematous. Her tongue is bright red and smooth. She states that over the last 2 weeks, she has been eating nothing but small portions of fruit. She is diagnosed with a vitamin deficiency. Which of the following statements is true about the vitamin most likely deficient in this patient?
- A. It increases the GI absorption of iron
- B. It is derived from tyrosine
- C. Synthesis requires vitamin B2 and B6 (Correct Answer)
- D. Synthesis requires vitamin B1 and B6
- E. It is used to treat hypertension
Nutritional diseases Explanation: ***Synthesis requires vitamin B2 and B6***
- The patient's symptoms (diarrhea, dermatitis, dementia-like behavior, glossitis, and weight loss) are classic for **pellagra**, which is caused by a deficiency in **niacin (vitamin B3)**.
- The synthesis of **niacin** from **tryptophan** requires **pyridoxine (vitamin B6)** and **riboflavin (vitamin B2)** as cofactors.
*It increases the GI absorption of iron*
- **Vitamin C** (ascorbic acid) enhances the **gastrointestinal absorption of non-heme iron** by reducing ferric iron to its ferrous form.
- Niacin does not play a direct role in the absorption of iron.
*It is derived from tyrosine*
- **Tyrosine** is a precursor to several important compounds, including **catecholamines** (dopamine, norepinephrine, epinephrine) and **thyroid hormones**.
- **Niacin** is predominantly synthesized from the essential amino acid **tryptophan**.
*Synthesis requires vitamin B1 and B6*
- While **vitamin B6** is essential for niacin synthesis from tryptophan, **vitamin B1 (thiamine)** is not directly involved in this pathway.
- Thiamine's primary role is in carbohydrate metabolism.
*It is used to treat hypertension*
- While **niacin** can affect lipid profiles, it is **not commonly used as a primary treatment for hypertension**.
- **Niacin** is used, primarily in pharmacologic doses, to **lower LDL cholesterol** and **triglycerides** and **raise HDL cholesterol**, often in conjunction with other lipid-lowering agents.
Nutritional diseases US Medical PG Question 8: A 9-month-old girl is brought to the physician because of a 1-month history of poor feeding and irritability. She is at the 15th percentile for height and 5th percentile for weight. Examination shows hypotonia and wasting of skeletal muscles. Cardiopulmonary examination shows no abnormalities. There is hepatomegaly. Her serum glucose is 61 mg/dL, creatinine kinase is 100 U/L, and lactic acid is within the reference range. Urine ketone bodies are elevated. Which of the following enzymes is most likely deficient in this patient?
- A. Glucose-6-phosphatase
- B. Muscle phosphorylase
- C. Acid alpha-glucosidase
- D. Glycogen debrancher (Correct Answer)
- E. Glucocerebrosidase
Nutritional diseases Explanation: ***Glycogen debrancher***
- The patient's symptoms of **hepatomegaly**, **hypoglycemia**, **poor feeding**, **growth failure**, and **elevated urine ketones** in the presence of normal lactic acid suggest Type III glycogen storage disease (Cori disease), caused by a deficiency in **glycogen debrancher enzyme**.
- **Muscle wasting** and **hypotonia** are also consistent with Type III GSD, as the debranching enzyme is present in both liver and muscle.
*Glucose-6-phosphatase*
- Deficiency in **glucose-6-phosphatase** (Type I GSD, Von Gierke disease) also presents with **hepatomegaly** and **hypoglycemia**.
- However, Type I GSD is characterized by **lactic acidosis**, which is explicitly stated as normal in this patient, and **hyperlipidemia**, which is not mentioned.
*Muscle phosphorylase*
- Deficiency in **muscle phosphorylase** (Type V GSD, McArdle disease) primarily affects skeletal muscle, causing **exercise intolerance** and **muscle pain**.
- It does not typically present with **hypoglycemia**, **hepatomegaly**, or **growth failure** in infancy.
*Acid alpha-glucosidase*
- Deficiency in **acid alpha-glucosidase** (Type II GSD, Pompe disease) causes accumulation of glycogen in lysosomes, leading to severe **cardiomyopathy**, **hypotonia**, and **muscle weakness**.
- While hypotonia is present, the absence of **cardiomegaly** and significant **liver involvement** makes this diagnosis less likely.
*Glucocerebrosidase*
- Deficiency in **glucocerebrosidase** causes Gaucher disease, a lysosomal storage disorder, not a glycogen storage disorder.
- Symptoms include **hepatosplenomegaly**, **bone crises**, and neurological symptoms, but not **hypoglycemia** or isolated muscle wasting directly related to glycogen metabolism.
Nutritional diseases US Medical PG Question 9: An 80-year-old woman is brought to the physician by her 2 daughters for worsening memory loss. They report that their mother is increasingly forgetful about recent conversations and events. She is unable to remember her appointments and commitments she has made. 3 years ago, the patient was moved into an elder care facility because she was often getting lost on her way home and forgetting to take her medications. The patient reports that she is very socially active at her new home and has long conversations with the other residents about her adventures as an air hostess during her youth. Which of the following cerebral pathologies is most likely present in this patient?
- A. Lewy bodies
- B. Lacunar infarcts
- C. Intracytoplasmic vacuoles
- D. Neurofibrillary tangles (Correct Answer)
- E. Demyelination
Nutritional diseases Explanation: ***Neurofibrillary tangles***
- The patient's presentation with **progressive memory loss** affecting recent events, getting lost, and forgetting medications, while largely preserving long-term memory (recalling youth as an air hostess and engaging in conversations), is highly characteristic of **Alzheimer's disease**.
- **Neurofibrillary tangles**, composed of hyperphosphorylated tau protein, along with **amyloid plaques**, are the hallmark pathological findings in Alzheimer's disease.
*Lewy bodies*
- **Lewy bodies** are characteristic of **Lewy body dementia** or Parkinson's disease with dementia, which typically present with prominent **fluctuations in cognition**, recurrent **visual hallucinations**, and parkinsonism.
- While memory loss can occur, the dominant features in this case point away from Lewy body pathology.
*Lacunar infarcts*
- **Lacunar infarcts** are associated with **vascular dementia**, which often presents with a more **step-wise decline** in cognitive function, focal neurological deficits, and evidence of cerebrovascular disease on imaging.
- The patient's gradual and progressive memory loss is less typical of lacunar infarcts as the primary cause.
*Intracytoplasmic vacuoles*
- **Intracytoplasmic vacuoles** are characteristic of **Creutzfeldt-Jakob disease** (spongiform encephalopathy), which is a rapidly progressive and fatal neurodegenerative disorder with distinct neurological symptoms such as myoclonus and ataxia, not fitting this patient's profile.
- The disease course is typically much faster than the 3-year progression described.
*Demyelination*
- **Demyelination** is the hallmark of conditions like **multiple sclerosis**, which primarily affects younger individuals and typically presents with a range of neurological deficits, including motor, sensory, and visual disturbances, that often relapse and remit.
- It does not typically present as a primary, progressive memory disorder in an 80-year-old in this manner.
Nutritional diseases US Medical PG Question 10: A 45-year-old African American man presents with nausea and severe abdominal pain. He denies vomiting. He says that, 2 days ago, his divorce was finalized, so he went to a bar and had multiple shots of tequila and vodka. This morning, upon waking, he noticed his urine was red, which lasted throughout the day. The patient denies any history of similar symptoms. Past medical history is significant for low blood counts diagnosed on routine laboratory work 6 months ago, which was not followed up due to the stress of the divorce. A review of systems is significant for erectile dysfunction and chronic fatigue. His temperature is 37.2°C (99.0°F), the heart rate is 90/min, the blood pressure is 136/88 mm Hg, and the respiratory rate is 20/min. Physical examination shows scleral icterus. Mucous membranes are pale. Cardiac auscultation reveals a systolic flow murmur loudest along the left sternal border. There is moderate right upper quadrant abdominal tenderness with no rebound or guarding. The remainder of the exam is unremarkable. Laboratory findings are significant for the following:
Hematocrit 27%
Mean corpuscular volume 81 µm3
Leukocytes 6,000/mm3
Platelets 130,000/µL
Haptoglobin 30 mg/dL (50–150 mg/dL)
Reticulocyte count 3%
Total bilirubin 7.1 mg/dL
LDH 766 U/L
AST 150 U/L
ALT 195 U/L
HbA1 96%
HbA2 2%
HbF 2%
CD55 50% of expected
The peripheral smear is unremarkable. Which of the following would be the most likely cause of mortality given this patient’s likely diagnosis?
- A. Hemorrhage
- B. High-output cardiac failure
- C. Cerebral vein thrombosis
- D. Infection
- E. Budd-Chiari syndrome (Correct Answer)
Nutritional diseases Explanation: ***Budd-Chiari syndrome***
- The patient's symptoms, including **abdominal pain**, **fatigue**, **erectile dysfunction**, and **dark urine** after alcohol consumption, along with lab findings like **low haptoglobin**, **elevated LDH and bilirubin**, and **reduced CD55 expression**, are highly suggestive of **paroxysmal nocturnal hemoglobinuria (PNH)**. **Budd-Chiari syndrome**, caused by **hepatic vein thrombosis**, is a life-threatening complication and a common cause of mortality in PNH due to the prothrombotic state.
- **PNH** is characterized by complement-mediated hemolysis due to deficient GPI-anchored proteins (CD55, CD59). The diagnosis is confirmed by **flow cytometry showing decreased CD55 and CD59** on red blood cells, which is indicated by the 50% CD55 of expected finding.
*Hemorrhage*
- While **thrombocytopenia** is present (platelets 130,000/µL), severe hemorrhage is not typically the leading cause of mortality in PNH.
- The clinical picture points more towards thrombotic complications rather than bleeding.
*High-output cardiac failure*
- Chronic anemia can lead to **high-output cardiac failure** over time, but it is less common as an acute cause of mortality compared to thrombotic events in PNH patients.
- The patient's current vital signs and symptoms do not strongly suggest immediate cardiac failure.
*Cerebral vein thrombosis*
- **Cerebral vein thrombosis** is indeed a serious thrombotic complication of PNH, but **Budd-Chiari syndrome** (hepatic vein thrombosis) is more frequently cited as a major and often fatal cause of mortality in PNH.
- Although possible, the abdominal symptoms point more directly to hepatic involvement.
*Infection*
- PNH patients are not typically considered severely immunocompromised. While chronic disease can increase susceptibility, infection is not the primary cause of mortality associated with the pathophysiological mechanisms of PNH.
- The clinical presentation does not strongly suggest an active, life-threatening infection as the most likely cause of mortality.
More Nutritional diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.