Molecular diagnostic methods US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Molecular diagnostic methods. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Molecular diagnostic methods US Medical PG Question 1: A genetic counselor sees a family for the first time for genetic assessment. The 24-year-old businessman and his 19-year-old sister are concerned about having a mutant allele and have decided to get tested. Their grandfather and great aunt both have Huntington’s disease which became apparent when they turned 52. Their father who is 47 years old appears healthy. The geneticist discusses both the benefits and risks of getting tested and orders some tests. Which of the following tests would best provide evidence for whether the siblings are carriers or not?
- A. Gel electrophoresis
- B. Restriction enzyme digestion products
- C. Polymerase chain reaction (Correct Answer)
- D. Pyrosequencing
- E. DNA isolation and purification
Molecular diagnostic methods Explanation: ***Polymerase chain reaction***
- **PCR is the essential first step** for detecting Huntington's disease carrier status by **amplifying the CAG trinucleotide repeat region** in the *HTT* gene.
- After PCR amplification, **fragment analysis** (capillary electrophoresis or gel electrophoresis) is used to determine the exact number of CAG repeats, which distinguishes carriers (≥36 repeats) from non-carriers (<27 repeats).
- Among the options listed, **PCR is the critical enabling technology** without which carrier testing cannot proceed.
- The complete diagnostic test is called "CAG repeat analysis" or "trinucleotide repeat analysis," which uses PCR as its foundation.
*Gel electrophoresis*
- **Gel electrophoresis** can be used to visualize the size of PCR-amplified DNA fragments and may help distinguish expanded repeats from normal-sized alleles.
- However, modern laboratories typically use **capillary electrophoresis** (automated fragment analysis) for more precise repeat counting.
- Gel electrophoresis alone, without prior PCR amplification, cannot detect the CAG repeat expansion.
*Restriction enzyme digestion products*
- Huntington's disease is caused by a **CAG trinucleotide repeat expansion**, not a point mutation that creates or abolishes restriction enzyme sites.
- **Restriction fragment length polymorphism (RFLP)** analysis is not the primary method for detecting dynamic repeat expansions.
- This approach was historically used for linkage analysis before direct repeat testing became available.
*Pyrosequencing*
- **Pyrosequencing** is designed for **sequencing short DNA stretches** and detecting single nucleotide polymorphisms (SNPs).
- It is **not suitable for quantifying long trinucleotide repeat expansions** like those in Huntington's disease, where repeat numbers can range from 10 to over 100.
- **Fragment analysis** is the standard method for measuring repeat length, not sequencing.
*DNA isolation and purification*
- **DNA isolation** is a necessary preliminary step for any genetic testing but provides no diagnostic information by itself.
- It simply extracts genomic DNA from blood or tissue samples, which must then be analyzed using specific molecular techniques like PCR and fragment analysis.
Molecular diagnostic methods US Medical PG Question 2: A 24-year-old woman presents to the ED with symptoms of pelvic inflammatory disease despite being previously treated with azithromycin for chlamydial infection. Based on your clinical understanding about the epidemiology of PID, you decide to obtain a gram stain which shows a gram-negative diplococci. What is the next step in order to confirm the identity of the organism described?
- A. Perform an RT-PCR
- B. Culture in TCBS agar
- C. Culture in Thayer-Martin media (Correct Answer)
- D. Obtain an acid fast stain
- E. Culture in Bordet-Gengou agar
Molecular diagnostic methods Explanation: ***Culture in Thayer-Martin media***
- The presence of **gram-negative diplococci** in a patient with PID symptoms strongly suggests *Neisseria gonorrhoeae*.
- **Thayer-Martin media** is a selective **agar** specifically designed for the isolation and identification of *Neisseria* species, including *N. gonorrhoeae*, by inhibiting the growth of most commensal bacteria and fungi.
*Perform an RT-PCR*
- While **RT-PCR** can detect *Neisseria gonorrhoeae* nucleic acids, it is primarily used for **molecular diagnosis** and not directly for confirming the identity of a cultured organism visualized on gram stain.
- **RT-PCR** is generally used for direct detection from clinical samples and is particularly useful in situations where culture is difficult or unavailable.
*Culture in TCBS agar*
- **TCBS (Thiosulfate Citrate Bile Salts Sucrose) agar** is a selective medium primarily used for the isolation of *Vibrio* species, which are not typically associated with pelvic inflammatory disease or characterized as gram-negative diplococci.
- This medium is designed to differentiate between different *Vibrio* species based on sucrose fermentation.
*Obtain an acid fast stain*
- An **acid-fast stain** (e.g., Ziehl-Neelsen stain) is used to identify bacteria with a **waxy cell wall**, such as *Mycobacterium* species (e.g., *Mycobacterium tuberculosis*).
- *Neisseria gonorrhoeae* is not acid-fast, and this stain would not be appropriate for its identification.
*Culture in Bordet-Gengou agar*
- **Bordet-Gengou agar** is a specialized culture medium used for the isolation of *Bordetella pertussis*, the causative agent of whooping cough.
- This medium is not suitable for the isolation of *Neisseria gonorrhoeae*.
Molecular diagnostic methods US Medical PG Question 3: An investigator is processing a blood sample from a human subject. A reagent is added to the sample and the solution is heated to break the hydrogen bonds between complementary base pairs. This solution is then cooled to allow artificial DNA primers in the solution to attach to the separated strands of the sample DNA molecules. An enzyme derived from the thermophilic bacterium Thermus aquaticus is added and the solution is reheated. These steps are repeated multiple times until the aim of the test is achieved. The investigator most likely used which of the following laboratory procedures on the test sample?
- A. Northern blot
- B. Western blot
- C. Polymerase chain reaction (Correct Answer)
- D. Immunohistochemistry
- E. Fluorescence in-situ hybridization
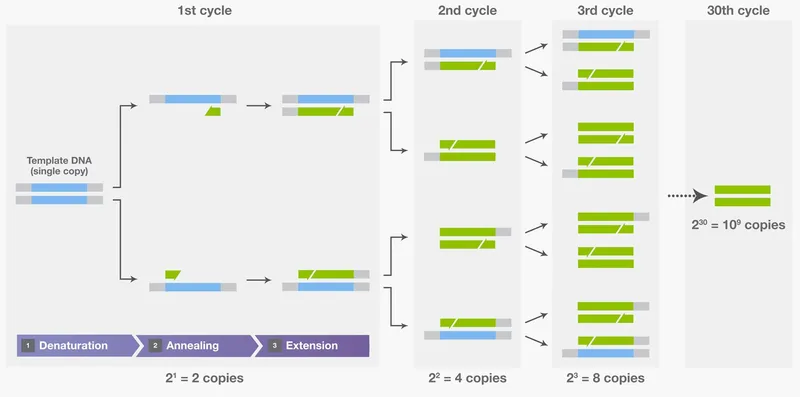
Molecular diagnostic methods Explanation: ***Polymerase chain reaction***
- The process described, including **denaturation** by heating, **annealing** of primers upon cooling, and **extension** by a heat-stable DNA polymerase (like from *Thermus aquaticus*), are the hallmark steps of **Polymerase Chain Reaction (PCR)**.
- PCR is used to **amplify specific DNA sequences** exponentially, making it possible to detect and analyze even minute amounts of genetic material.
*Northern blot*
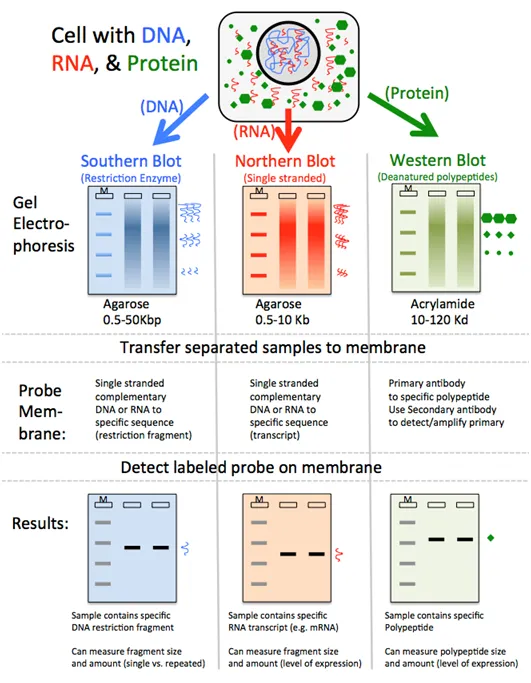
- **Northern blot** is a laboratory technique used to detect specific **RNA molecules** among a mixture of RNA. It involves electrophoresis, transfer to a membrane, and hybridization with a probe.
- It does not involve repetitive heating, cooling, or the use of DNA primers and heat-stable polymerases for amplification.
*Western blot*
- **Western blot** is a widely used analytical technique in molecular biology and immunogenetics to detect specific **proteins** in a sample of tissue homogenate or extract.
- This method separates proteins by size using gel electrophoresis, transfers them to a membrane, and then detects the target protein using specific antibodies. It does not involve DNA denaturation or amplification.
*Immunohistochemistry*
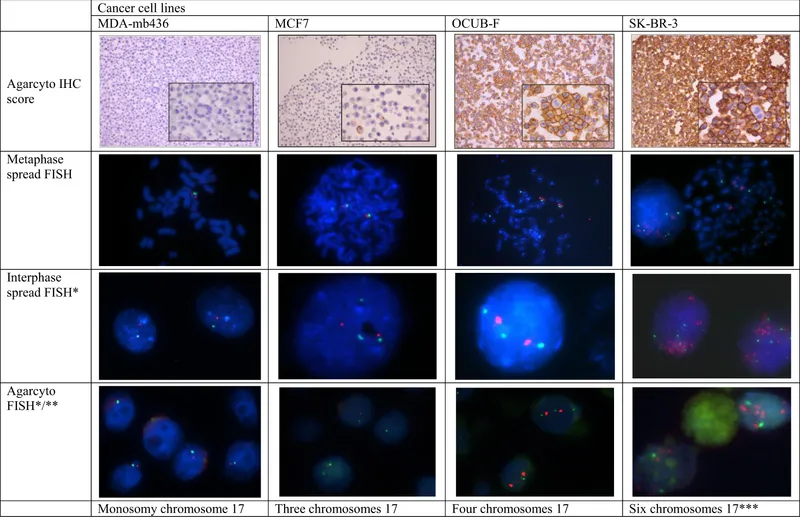
- **Immunohistochemistry (IHC)** is a histological technique that uses the principle of specific antibody-antigen binding to **detect specific antigens (proteins) in cells or tissues**.
- It involves staining tissues with antibodies labeled with a chromogenic reporter or fluorophore to visualize the location and distribution of target proteins within preserved tissue sections.
*Fluorescence in-situ hybridization*
- **Fluorescence in-situ hybridization (FISH)** is a cytogenetic technique used to detect and **localize specific DNA or RNA sequences within cells or tissues** using fluorescent probes that bind to parts of the chromosome.
- While it involves hybridization, it is primarily for visualizing genetic material within its cellular context, not for amplifying DNA like PCR.
Molecular diagnostic methods US Medical PG Question 4: A group of microbiological investigators is studying bacterial DNA replication in E. coli colonies. While the cells are actively proliferating, the investigators stop the bacterial cell cycle during S phase and isolate an enzyme involved in DNA replication. An assay of the enzyme's exonuclease activity determines that it is active on both intact and demethylated thymine nucleotides. Which of the following enzymes have the investigators most likely isolated?
- A. DNA ligase
- B. Telomerase
- C. Primase
- D. DNA topoisomerase
- E. DNA polymerase I (Correct Answer)
Molecular diagnostic methods Explanation: ***DNA polymerase I***
- **DNA polymerase I** possesses **5' to 3' exonuclease activity**, which is crucial for removing **RNA primers** (intact nucleotides) laid down by primase during DNA replication.
- This 5' to 3' exonuclease activity also allows it to excise damaged DNA, including DNA containing **demethylated thymine nucleotides**.
- It also has 3' to 5' exonuclease activity for proofreading.
- **Key distinction:** While DNA polymerase III (the main replicative enzyme) only has 3' to 5' exonuclease activity, DNA polymerase I has **both** 3' to 5' and 5' to 3' exonuclease activities, making it essential for primer removal and DNA repair.
*DNA ligase*
- **DNA ligase** functions to form a **phosphodiester bond** between adjacent nucleotides to seal nicks in the DNA backbone, but it does not have exonuclease activity.
- Its primary role is in joining Okazaki fragments and repairing single-strand breaks.
*Telomerase*
- **Telomerase** is a specialized reverse transcriptase that extends the telomeres at the ends of eukaryotic chromosomes, but is not present in prokaryotes like *E. coli*.
- It uses an RNA template to synthesize DNA, and it lacks exonuclease activity.
*Primase*
- **Primase** is an RNA polymerase that synthesizes short **RNA primers** on the DNA template, providing a starting point for DNA synthesis.
- It is involved in synthesizing primers, not in removing or excising nucleotides, and has no exonuclease activity.
*DNA topoisomerase*
- **DNA topoisomerases** relieve supercoiling in DNA during replication and transcription by cutting and rejoining DNA strands.
- While they act on DNA, their function is to manage topological stress, and they do not exhibit exonuclease activity on nucleotides.
Molecular diagnostic methods US Medical PG Question 5: A 3-year-old boy is brought to his pediatrician by his parents for a follow-up visit. Several concerning traits were observed at his last physical, 6 months ago. He had developmental delay, a delay in meeting gross and fine motor control benchmarks, and repetitive behaviors. At birth, he was noted to have flat feet, poor muscle tone, an elongated face with large, prominent ears, and enlarged testicles. He takes a chewable multivitamin every morning. There is one other member of the family, on the mother’s side, with a similar condition. Today, his blood pressure is 110/65 mm Hg, heart rate is 90/min, respiratory rate is 22/min, and temperature of 37.0°C (98.6°F). On physical exam, the boy repetitively rocks back and forth and has difficulty following commands. His heart has a mid-systolic click, followed by a late systolic murmur and his lungs are clear to auscultation bilaterally. Several vials of whole blood are collected for analysis. Which of the following studies should be conducted as part of the diagnostic screening protocol?
- A. Northern blot with RNA probes
- B. Two-dimensional gel electrophoresis
- C. Southern blot with DNA probes (Correct Answer)
- D. Western blot
- E. PCR followed by northern blot with RNA probes
Molecular diagnostic methods Explanation: ***Southern blot with DNA probes***
- The patient's presentation with developmental delay, repetitive behaviors, flat feet, hypotonia, elongated face, prominent ears, and macroorchidism (*enlarged testicles*) is highly suggestive of **Fragile X syndrome**.
- **Fragile X syndrome** is caused by an abnormal expansion of a **CGG trinucleotide repeat** in the *FMR1* gene on the X chromosome, which leads to hypermethylation and silencing of the gene. **Southern blot analysis with DNA probes** is the gold standard for detecting these expansions, as it can measure the size of the *CGG* repeat and the methylation status of the gene.
*Northern blot with RNA probes*
- **Northern blot analysis** is used to detect and quantify specific **RNA molecules**.
- While the *FMR1* gene's mRNA expression is affected in Fragile X syndrome, northern blot is not the primary diagnostic test for detecting the underlying **DNA repeat expansion** and methylation.
*Two-dimensional gel electrophoresis*
- **Two-dimensional gel electrophoresis** is a technique used to separate **proteins** based on their **isoelectric point** and then by **molecular weight**.
- This method is used for proteomic studies and is not relevant for diagnosing a genetic disorder caused by a DNA repeat expansion.
*Western blot*
- **Western blot analysis** is used to detect specific **proteins** in a sample.
- In Fragile X syndrome, the *FMR1* gene product, **FMRP (Fragile X Mental Retardation Protein)**, is absent or reduced, which could be theoretically detected by Western blot. However, the definitive diagnosis relies on identifying the genetic mutation (CGG expansion and methylation) in the DNA, for which Southern blot is superior.
*PCR followed by northern blot with RNA probes*
- **PCR (Polymerase Chain Reaction)** is used to amplify specific **DNA sequences**. While *PCR* can detect smaller *CGG* expansions, it often fails to accurately size the full mutations found in Fragile X syndrome due to the large repeat numbers.
- Combining *PCR* with **northern blot (RNA detection)** would still not be the primary diagnostic approach for the DNA-based *CGG* repeat expansion and methylation status, which is essential for diagnosing Fragile X.
Molecular diagnostic methods US Medical PG Question 6: A 19-year-old male from rural West Virginia presents to his family medicine doctor to discuss why he is having trouble getting his wife pregnant. On exam, he is 6 feet 2 inches with a frail frame and broad hips for a male his size. He is noted to have mild gynecomastia, no facial hair, and small, underdeveloped testes. He claims that although he has a lower libido than most of his friends, he does have unprotected sex with his wife. His past medical history is notable for developmental delay and difficulties in school. What is the most likely chromosomal abnormality in this patient?
- A. Trisomy 13
- B. 45: XO
- C. Trisomy 21
- D. 47: XYY
- E. 47: XXY (Correct Answer)
Molecular diagnostic methods Explanation: ***47: XXY***
- The patient's presentation with **infertility**, small testes, **gynecomastia**, eunuchoid body habitus (tall, frail frame, broad hips), lack of facial hair, and **developmental delay** are classic features of **Klinefelter syndrome (47, XXY)**.
- This chromosomal abnormality leads to primary **hypogonadism** due to the presence of an extra X chromosome in males.
*Trisomy 13*
- Trisomy 13, or **Patau syndrome**, is characterized by severe developmental anomalies, including **cleft lip and palate**, polydactyly, and severe neurological defects.
- Infants with Trisomy 13 rarely survive beyond the first year and do not present with the described signs of hypogonadism or gynecomastia in adolescence.
*45: XO*
- **45, XO** or **Turner syndrome** affects females and is characterized by **short stature**, primary amenorrhea, webbed neck, and **gonadal dysgenesis (streak gonads)**.
- This karyotype is incompatible with a male phenotype and the symptoms described.
*Trisomy 21*
- Trisomy 21, or **Down syndrome**, is associated with distinct facial features, intellectual disability, and congenital heart defects.
- While individuals with Down syndrome may have fertility issues, they do not typically present with the specific combination of **gynecomastia**, eunuchoid habitus, and **small testes** seen in this patient.
*47: XYY*
- **47, XYY syndrome** is associated with increased height and potentially some learning difficulties, but typically does not cause the significant **hypogonadism**, **gynecomastia**, or **small testes** seen in this patient.
- Men with 47, XYY usually have normal sexual development and fertility, though some may experience learning disabilities or behavioral problems.
Molecular diagnostic methods US Medical PG Question 7: A 35-year-old woman with no significant past medical, past surgical, family or social history presents to clinic with a recently identified area of flat, intact, pigmented skin. The patient believes that this is a large freckle, and she states that it becomes darker during the summer when she is outdoors. On physical examination, you measure the lesion to be 6 mm in diameter. Which of the following is the best descriptor of this patient’s skin finding?
- A. Wheal
- B. Papule
- C. Ulcer
- D. Plaque
- E. Macule (Correct Answer)
Molecular diagnostic methods Explanation: ***Macule***
- A **macule** is a **flat, discolored lesion** that is less than 1 cm in diameter, which fits the description of a **flat, pigmented skin area** that is 6 mm in diameter.
- The darkening of the lesion with sun exposure is characteristic of a **freckle**, which is a type of macule caused by increased melanin production without an increase in melanocyte numbers.
*Wheal*
- A **wheal** is a **transient, elevated lesion** caused by dermal edema, typically seen in allergic reactions like hives.
- This patient's lesion is described as a **flat, pigmented area**, not an elevated, transient swelling.
*Papule*
- A **papule** is a **solid, elevated lesion** that is less than 1 cm in diameter.
- The patient's skin finding is explicitly described as **flat** and intact, not elevated.
*Ulcer*
- An **ulcer** is a **loss of epidermis and dermis**, resulting in an open sore; it is not a flat, intact pigmented lesion.
- The description of the lesion as **intact** rules out an ulcer, which involves a break in the skin surface.
*Plaque*
- A **plaque** is a **flat-topped, elevated lesion** that is larger than 1 cm in diameter.
- While flat-topped, a plaque is **elevated**, and the patient's lesion is described as **flat**, not elevated.
Molecular diagnostic methods US Medical PG Question 8: A 68-year-old male is brought to his primary care physician by his wife who is concerned that the patient seems more confused and irritable than usual. Three months ago, she started noticing that he appeared confused while doing simple tasks and seemed to be off balance. He has fallen several times over that time period. She has also noticed that if he is startled by one of their grandchildren, his arm starts to twitch uncontrollably. His past medical history is notable for transient ischemic attacks, hypertension, and hyperlipidemia. He takes aspirin, enalapril, hydrochlorothiazide, and rosuvastatin. He has a 30 pack-year smoking history. His family history is notable for Alzheimer’s disease in his mother and maternal uncle. His temperature is 98.6°F (37°C), blood pressure is 130/70 mmHg, pulse is 95/min, and respirations are 16/min. Physical examination reveals dysmetria and an ataxic gait. This patient’s condition is most strongly associated with which of the following findings on brain autopsy?
- A. Intracellular rounded hyperphosphorylated tau
- B. Extracellular accumulation of amyloid beta
- C. Multifocal ischemic changes
- D. Accumulations of beta-pleated sheets (Correct Answer)
- E. Intracellular aggregates of alpha-synuclein
Molecular diagnostic methods Explanation: ***Accumulations of beta-pleated sheets***
- This patient's presentation with **rapidly progressive dementia**, confusion, ataxia, **myoclonus** (twitching arm when startled), and falls, without significant family history of early-onset Alzheimer's, strongly points towards **Creutzfeldt-Jakob disease (CJD)**.
- CJD is characterized pathologically by the accumulation of abnormally folded **prion proteins (PrPSc)**, which form **beta-pleated sheets** and cause spongiform changes in the brain.
*Intracellular rounded hyperphosphorylated tau*
- This finding is characteristic of **Alzheimer's disease (neurofibrillary tangles)**, which typically presents with a more gradual onset of memory loss and cognitive decline, rather than the rapid progression, prominent motor symptoms (ataxia, myoclonus), and falls seen in this patient.
- While there is a family history of Alzheimer's, the **rapid progression** and specific neurological signs make CJD a more likely diagnosis in this case.
*Extracellular accumulation of amyloid beta*
- This describes **amyloid plaques**, another hallmark of **Alzheimer's disease**.
- Similar to tau pathology, this finding would be more consistent with a gradual, progressive memory impairment, and less with the pronounced and rapid neurological deficits observed.
*Multifocal ischemic changes*
- While the patient has vascular risk factors (**hypertension, hyperlipidemia, TIA history, smoking**), multifocal ischemic changes (as seen in **vascular dementia**) usually lead to a stepwise cognitive decline and may cause focal neurological deficits, but typically do not present with the characteristic myoclonus and rapidly progressive ataxia seen here.
- The constellation of symptoms is more indicative of a **prion disease** than purely vascular dementia.
*Intracellular aggregates of alpha-synuclein*
- This pathology is characteristic of **Lewy body dementia** or **Parkinson's disease dementia**.
- Symptoms would include progressive cognitive decline, **fluctuating cognition**, prominent **visual hallucinations**, and parkinsonism. While some motor symptoms like falls are present, the myoclonus and rapid progression make CJD a more fitting diagnosis.
Molecular diagnostic methods US Medical PG Question 9: A 21-year-old man comes to the physician because of painful, firm, dark bumps on his neck and jawline. He has no history of serious illness and takes no medications. His brother had a similar rash. A photograph of the rash is shown. Which of the following is the most likely underlying mechanism of this patient's condition?
- A. Trichophyton infection of the superficial hair follicle
- B. Interfollicular penetration of the skin by distal end of hair (Correct Answer)
- C. Bacterial infection of the superficial or deep hair follicle
- D. Follicular obstruction with subsequent duct rupture
- E. Cutibacterium acnes colonization of the pilosebaceous unit
Molecular diagnostic methods Explanation: ***Interfollicular penetration of the skin by distal end of hair***
- The description of painful, firm, dark bumps on the neck and jawline, particularly in a young man, is classic for **pseudofolliculitis barbae**, often caused by the distal end of hair penetrating the skin after shaving.
- This condition is common in individuals with **curly hair** where shaved hairs re-enter the skin, causing a foreign body inflammatory reaction.
*Trichophyton infection of the superficial hair follicle*
- This would typically present as **tinea barbae** or **tinea capitis**, characterized by scaling, erythema, and pustules, often with hair breakage, not firm dark bumps from embedded hairs.
- While fungal infections can cause folliculitis, the clinical presentation and family history of improvement with erythromycin (an antibacterial) make this less likely.
*Bacterial infection of the superficial or deep hair follicle*
- **Bacterial folliculitis** (e.g., *Staphylococcus aureus*) usually presents as pustules, papules, and sometimes carbuncles, which are typically red, inflamed, and often pus-filled.
- The family history of improvement with erythromycin might suggest a bacterial component, but the primary mechanism described (firm, dark bumps) points away from primary bacterial infection and more towards a physical cause like pseudofolliculitis barbae, which can then become secondarily infected.
*Follicular obstruction with subsequent duct rupture*
- This mechanism is characteristic of **acne vulgaris** (comedones, papules, pustules, cysts) or **hidradenitis suppurativa** (deep-seated nodules, abscesses affecting intertriginous areas), which are different in appearance and location from the described lesions.
- While related to follicular issues, the specific description of "dark bumps" and the context of shaving make embedded hairs more likely than a primary obstruction and rupture.
*Cutibacterium acnes colonization of the pilosebaceous unit*
- This is the primary bacterial contributor to **acne vulgaris**, leading to comedones, inflamed papules, and pustules, often affecting the face, chest, and back.
- Although the jawline is a common area for acne, the "firm, dark bumps" are less typical of classic acne and more consistent with ingrown hairs.
Molecular diagnostic methods US Medical PG Question 10: Two weeks after undergoing low anterior resection for rectal cancer, a 52-year-old man comes to the physician because of swelling in both feet. He has not had any fever, chills, or shortness of breath. His temperature is 36°C (96.8°F) and pulse is 88/min. Physical examination shows a normal thyroid and no jugular venous distention. Examination of the lower extremities shows bilateral non-pitting edema that extends from the feet to the lower thigh, with deep flexion creases. His skin is warm and dry, and there is no erythema or rash. Microscopic examination of the interstitial space in this patient's lower extremities would be most likely to show the presence of which of the following?
- A. Neutrophilic, protein-rich fluid
- B. Lymphocytic, hemosiderin-rich fluid
- C. Lipid-rich, protein-rich fluid (Correct Answer)
- D. Protein-rich, glycosaminoglycan-rich fluid
- E. Acellular, protein-poor fluid
Molecular diagnostic methods Explanation: ***Lipid-rich, protein-rich fluid***
- The presentation of bilateral non-pitting edema extending to the thigh, with deep flexion creases, in a patient post-**low anterior resection** for rectal cancer, strongly suggests **lymphedema**.
- Lymphedema results from impaired lymphatic drainage, leading to the accumulation of **protein-rich fluid**, **macromolecules**, and **adipose tissue** in the interstitial space, which eventually becomes lipid-rich due to chronic inflammation and fibroblasts stimulating adipogenesis.
*Neutrophilic, protein-rich fluid*
- This description is characteristic of **inflammatory edema** or **purulent exudate**, typically seen in infections.
- The patient's lack of fever, chills, erythema, or warmth makes an infectious or acute inflammatory process unlikely.
*Lymphocytic, hemosiderin-rich fluid*
- **Hemosiderin deposits** are indicative of chronic **venous insufficiency** or recurrent hemorrhages, leading to red blood cell extravasation and breakdown.
- While lymphocytes can be present in chronic inflammation, the primary issue here is lymphatic obstruction, not venous stasis or bleeding.
*Protein-rich, glycosaminoglycan-rich fluid*
- While lymphedema is indeed **protein-rich**, the primary accumulation in mature lymphedema involves **adipose tissue** and fibrosis.
- **Glycosaminoglycans** accumulate significantly in conditions like **myxedema** (hypothyroidism), which was ruled out by the normal thyroid examination.
*Acellular, protein-poor fluid*
- This describes a **transudate**, typically seen in conditions like **heart failure**, **liver cirrhosis**, or **nephrotic syndrome** where there's an imbalance of hydrostatic and oncotic pressures.
- The edema in this case is **non-pitting**, suggesting a higher protein content and tissue changes characteristic of lymphatic dysfunction, not systemic fluid overload leading to protein-poor fluid.
More Molecular diagnostic methods US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.