Laboratory techniques in pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Laboratory techniques in pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Laboratory techniques in pathology US Medical PG Question 1: An investigator studying the molecular characteristics of various malignant cell lines collects tissue samples from several families with a known mutation in the TP53 tumor suppressor gene. Immunohistochemical testing performed on one of the cell samples stains positive for desmin. This sample was most likely obtained from which of the following neoplasms?
- A. Squamous cell carcinoma
- B. Rhabdomyosarcoma (Correct Answer)
- C. Prostate cancer
- D. Endometrial carcinoma
- E. Melanoma
Laboratory techniques in pathology Explanation: ***Rhabdomyosarcoma***
- **Desmin** is an intermediate filament present in **muscle cells**, and its positive staining is a definitive marker for tumors of muscle origin
- A **rhabdomyosarcoma** is a malignant tumor of **skeletal muscle** differentiation, thus explaining the positive desmin staining.
*Squamous cell carcinoma*
- **Squamous cell carcinomas** are epithelial tumors that typically stain positive for **cytokeratin**, not desmin, as they originate from epithelial cells.
- They are characterized by features such as **intercellular bridges** and **keratinization**.
*Prostate cancer*
- **Prostate cancer** is an adenocarcinoma, meaning it's derived from glandular epithelial cells, and would stain positive for markers like **PSA (prostate-specific antigen)**, not desmin.
- This tumor type is characterized by glandular differentiation.
*Endometrial carcinoma*
- **Endometrial carcinomas** are adenocarcinomas of the uterine lining, derived from glandular epithelial cells, and would express **cytokeratins**, not desmin.
- Histologically, they show glandular structures and atypical endometrial cells.
*Melanoma*
- **Melanomas** are malignant tumors of melanocytes and would stain positive for markers such as **S-100**, **HMB-45**, and **Mart-1**, not desmin.
- These tumors originate from neural crest cells and are not muscle-derived.
Laboratory techniques in pathology US Medical PG Question 2: During an experiment, the immunophenotypes of different cells in a sample are determined. The cells are labeled with fluorescent antibodies specific to surface proteins, and a laser is then focused on the samples. The intensity of fluorescence created by the laser beam is then plotted on a scatter plot. The result shows most of the cells in the sample to be positive for CD8 surface protein. Which of the following cell types is most likely represented in this sample?
- A. Mature cytotoxic T lymphocytes (Correct Answer)
- B. Activated regulatory T lymphocytes
- C. Inactive B lymphocytes
- D. Dendritic cells
- E. Mature helper T lymphocytes
Laboratory techniques in pathology Explanation: ***Mature cytotoxic T lymphocytes***
- **CD8** is a characteristic surface marker for **cytotoxic T lymphocytes**, indicating their immune function in directly killing infected or cancerous cells.
- The "mature" designation implies they have fully developed and are ready to exert their effector functions.
*Activated regulatory T lymphocytes*
- **Regulatory T lymphocytes** are typically identified by the expression of **CD4** and **CD25**, along with the intracellular transcription factor **FOXP3**, not CD8.
- Their primary role is immune suppression, not direct cytotoxicity.
*Inactive B lymphocytes*
- **B lymphocytes** are characterized by the expression of **CD19**, **CD20**, and surface immunoglobulins, which are distinct from the CD8 marker.
- Their main function is antibody production.
*Dendritic cells*
- **Dendritic cells** are primarily **antigen-presenting cells** and are identified by markers such as **CD11c** and **MHC class II molecules**, not CD8.
- While some rare subsets of dendritic cells can express CD8α, it is not their predominant or defining marker.
*Mature helper T lymphocytes*
- **Helper T lymphocytes** are defined by the expression of **CD4** and play a crucial role in coordinating the immune response.
- They do not express CD8, which is characteristic of cytotoxic T cells.
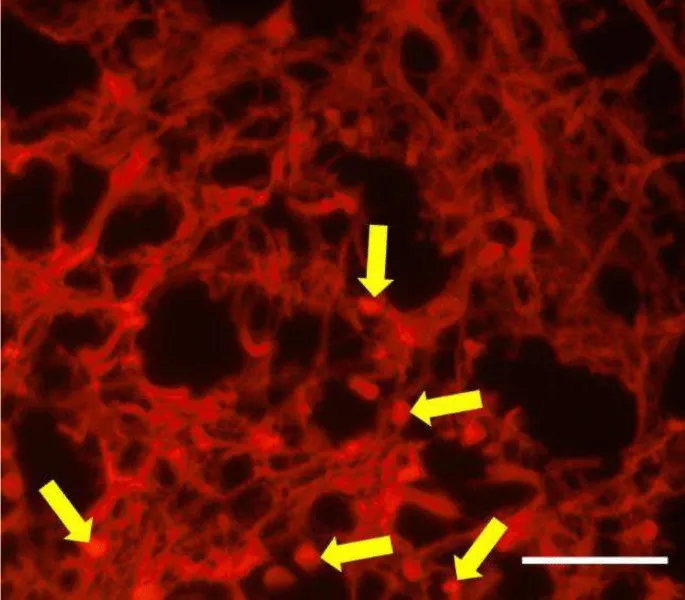
Laboratory techniques in pathology US Medical PG Question 3: A 16-year-old boy presents to the emergency department after a skateboarding accident. He fell on a broken bottle and received a 4 cm wound on the dorsal aspect of his left hand. His vitals are stable and he was evaluated by the surgeon on call who determined that suturing was not required. After several weeks the wound has almost completely healed (see image). Which of the following is the correct description of this patient's wound before healing?
- A. Incised wound (Correct Answer)
- B. Abrasion
- C. Laceration
- D. Avulsion
- E. Puncture
Laboratory techniques in pathology Explanation: ***Incised wound***
- An **incised wound** is caused by a sharp object, such as a broken bottle, resulting in a clean, straight cut with well-defined edges and minimal tissue damage.
- The characteristics of the injury (sharp object mechanism, 4 cm linear wound) and the clinical decision that suturing was not required suggest a relatively clean incised wound with edges that could approximate well.
- Incised wounds typically heal with **fine linear scars** as shown in the image, especially when the edges are well-approximated.
*Abrasion*
- An abrasion is a **superficial wound** caused by friction or scraping, leading to removal of the epidermis and sometimes the superficial dermis.
- This mechanism does not match the described injury from a broken bottle, and abrasions produce broad, shallow wounds rather than deep linear cuts.
- Abrasions heal with minimal scarring and would not produce the linear scar pattern shown.
*Laceration*
- A laceration is a wound with **irregular, torn edges** typically caused by blunt force trauma or crushing injury.
- While broken glass can sometimes cause lacerations, the description of a clean "4 cm wound" from falling on a broken bottle more strongly suggests a sharp cutting mechanism rather than tearing.
- Lacerations have jagged edges with more tissue damage and typically require debridement or careful closure.
*Avulsion*
- An **avulsion** involves forcible tearing away of tissue, often resulting in significant tissue loss with irregular, gaping wounds.
- This injury pattern is much more severe than described and would typically require complex surgical management, including possible skin grafting.
- The mechanism (falling on broken glass) and the relatively straightforward healing do not support an avulsion injury.
*Puncture*
- A puncture wound is caused by a **pointed object** penetrating the skin, creating a small entry hole with depth greater than width.
- The description of a "4 cm wound" indicates a linear length, not a deep narrow penetration typical of puncture wounds.
- Puncture wounds carry high infection risk and would not produce the linear scar pattern shown in the image.
Laboratory techniques in pathology US Medical PG Question 4: An investigator is processing a blood sample from a human subject. A reagent is added to the sample and the solution is heated to break the hydrogen bonds between complementary base pairs. This solution is then cooled to allow artificial DNA primers in the solution to attach to the separated strands of the sample DNA molecules. An enzyme derived from the thermophilic bacterium Thermus aquaticus is added and the solution is reheated. These steps are repeated multiple times until the aim of the test is achieved. The investigator most likely used which of the following laboratory procedures on the test sample?
- A. Northern blot
- B. Western blot
- C. Polymerase chain reaction (Correct Answer)
- D. Immunohistochemistry
- E. Fluorescence in-situ hybridization
Laboratory techniques in pathology Explanation: ***Polymerase chain reaction***
- The process described, including **denaturation** by heating, **annealing** of primers upon cooling, and **extension** by a heat-stable DNA polymerase (like from *Thermus aquaticus*), are the hallmark steps of **Polymerase Chain Reaction (PCR)**.
- PCR is used to **amplify specific DNA sequences** exponentially, making it possible to detect and analyze even minute amounts of genetic material.
*Northern blot*
- **Northern blot** is a laboratory technique used to detect specific **RNA molecules** among a mixture of RNA. It involves electrophoresis, transfer to a membrane, and hybridization with a probe.
- It does not involve repetitive heating, cooling, or the use of DNA primers and heat-stable polymerases for amplification.
*Western blot*
- **Western blot** is a widely used analytical technique in molecular biology and immunogenetics to detect specific **proteins** in a sample of tissue homogenate or extract.
- This method separates proteins by size using gel electrophoresis, transfers them to a membrane, and then detects the target protein using specific antibodies. It does not involve DNA denaturation or amplification.
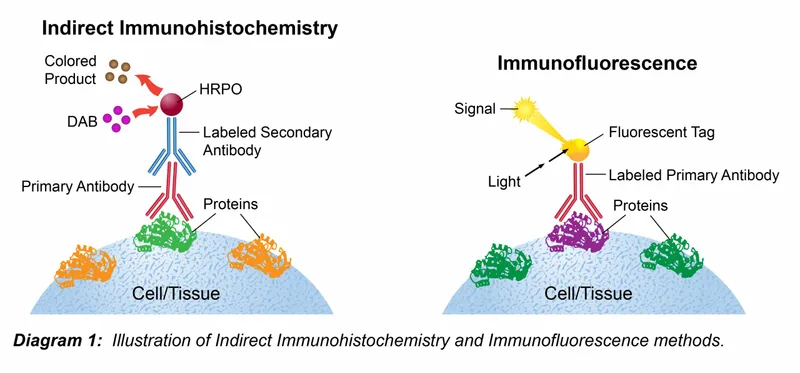
*Immunohistochemistry*
- **Immunohistochemistry (IHC)** is a histological technique that uses the principle of specific antibody-antigen binding to **detect specific antigens (proteins) in cells or tissues**.
- It involves staining tissues with antibodies labeled with a chromogenic reporter or fluorophore to visualize the location and distribution of target proteins within preserved tissue sections.
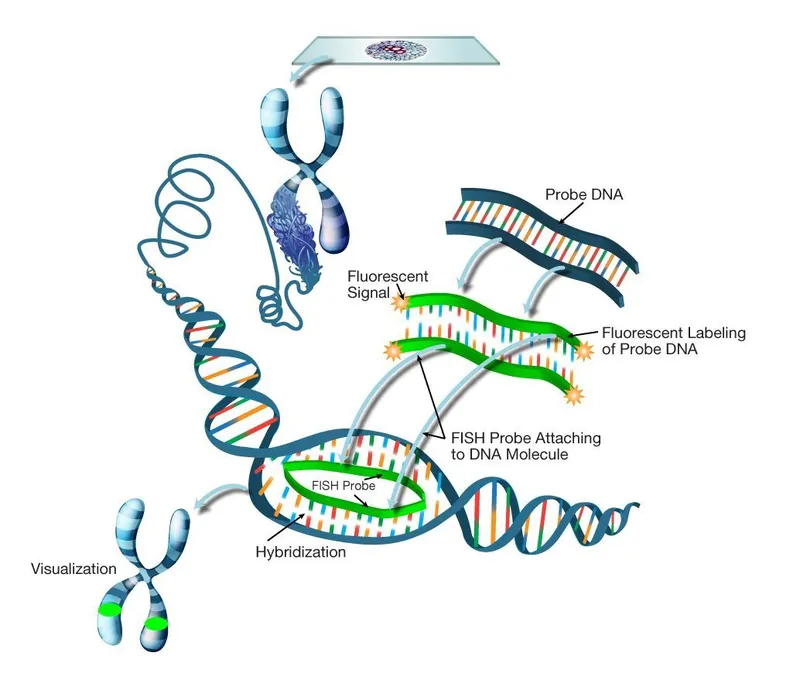
*Fluorescence in-situ hybridization*
- **Fluorescence in-situ hybridization (FISH)** is a cytogenetic technique used to detect and **localize specific DNA or RNA sequences within cells or tissues** using fluorescent probes that bind to parts of the chromosome.
- While it involves hybridization, it is primarily for visualizing genetic material within its cellular context, not for amplifying DNA like PCR.
Laboratory techniques in pathology US Medical PG Question 5: A pathologist receives a patient sample for analysis. Cells in the sample are first labeled with fluorescent antibodies and then passed across a laser beam in a single file of particles. The light scatter and fluorescent intensity of the particles are plotted on a graph; this information is used to characterize the sample. This laboratory method would be most useful to establish the diagnosis of a patient with which of the following?
- A. Ventricular septal defect and facial dysmorphism with low T-lymphocyte count
- B. Painless generalized lymphadenopathy with monomorphic cells and interspersed benign histiocytes on histology
- C. Pancytopenia and deep vein thrombosis with intermittent hemoglobinuria (Correct Answer)
- D. Multiple opportunistic infections with decreased CD4 counts
- E. Vesicular lesions with dermatomal distribution and dendritic corneal ulcers
Laboratory techniques in pathology Explanation: ***Pancytopenia and deep vein thrombosis with intermittent hemoglobinuria***
- The described laboratory method is **flow cytometry**, which is the **gold standard for diagnosing paroxysmal nocturnal hemoglobinuria (PNH)** by detecting the absence of **CD55** and **CD59** on red blood cells due to impaired GPI anchor synthesis.
- PNH classically presents with **pancytopenia**, **hemolytic anemia** (leading to hemoglobinuria), and a high risk of **thrombosis** (e.g., deep vein thrombosis).
*Ventricular septal defect and facial dysmorphism with low T-lymphocyte count*
- This clinical picture suggests **DiGeorge syndrome**, which involves a developmental defect of the **third and fourth pharyngeal pouches**, leading to thymic hypoplasia and **T-cell deficiency**.
- While flow cytometry is used to quantify T-lymphocyte subsets (e.g., CD3, CD4, CD8), the primary method for diagnosing DiGeorge syndrome is **fluorescent in situ hybridization (FISH)** for a **22q11 deletion**, making it less ideal for flow cytometry diagnosis.
*Painless generalized lymphadenopathy with monomorphic cells and interspersed benign histiocytes on histology*
- This description with "**monomorphic cells**" is more consistent with certain **non-Hodgkin lymphomas** (e.g., Burkitt lymphoma) rather than Hodgkin lymphoma, which typically shows a **polymorphic** cellular infiltrate.
- While flow cytometry can be useful in characterizing lymphomas by identifying cell surface markers, the diagnosis is primarily established by **lymph node biopsy and histopathology** with **immunohistochemistry**, making flow cytometry a supplementary rather than primary diagnostic tool.
*Multiple opportunistic infections with decreased CD4 counts*
- This presentation is highly suggestive of **HIV infection leading to AIDS**. The "decreased CD4 counts" are a key diagnostic and prognostic marker.
- While flow cytometry is used to **monitor CD4 cell counts** in HIV patients, the initial diagnosis of HIV is established via **antibody/antigen combination tests** and confirmed by **Western blot** or **PCR for viral load**, not by flow cytometry.
*Vesicular lesions with dermatomal distribution and dendritic corneal ulcers*
- This clinical presentation points to **herpes zoster ophthalmicus** (shingles affecting the eye due to **varicella-zoster virus** reactivation).
- Diagnosis is primarily **clinical** based on the characteristic rash and eye findings, although **PCR** of vesicular fluid can confirm VZV infection. Flow cytometry has no role in this diagnosis.
Laboratory techniques in pathology US Medical PG Question 6: A 32-year-old man visits his family physician for 10 months of persistent left flank pain, weight loss, and fatigue. Also, he has had hematuria a couple of times in the last month. His mother was diagnosed and treated for a pheochromocytoma when she was 36 years old, and his father died at 45 years due to myocardial infarction. His personal medical history is not relevant. He does not smoke and used to be a varsity athlete in high school and university. Physical examination shows temporal wasting, pale mucous membranes and palms, a palpable mass in the left flank, and a varicocele that does not reduce upon recumbency. His family physician sends the patient to the emergency department for an abdominal computed tomography (CT) scan, which shows a complex left renal mass and a hemangioblastoma in T10. A biopsy of the renal mass is ordered by the oncology team, which demonstrates compact cells with prominent nucleoli, eosinophilic cytoplasm within a network of a small and thin-walled vasculature. What is the most likely type of tumor in this patient?
- A. Collecting duct carcinoma
- B. Clear-cell carcinoma (Correct Answer)
- C. Oncocytic carcinoma
- D. Papillary carcinoma
- E. Chromophobe carcinoma
Laboratory techniques in pathology Explanation: ***Clear-cell carcinoma***
- This patient's presentation with a **renal mass**, hemangioblastoma, a family history of **pheochromocytoma** (his mother), and an early death of his father (likely from heart disease associated with pheochromocytoma) is highly suggestive of **Von Hippel-Lindau (VHL) syndrome**. **Clear cell renal cell carcinoma** is the most common renal tumor associated with VHL syndrome.
- The biopsy description of **compact cells with prominent nucleoli**, **eosinophilic cytoplasm**, and a **network of small and thin-walled vasculature** is characteristic of clear cell renal cell carcinoma.
*Collecting duct carcinoma*
- This is a rare and aggressive subtype of **renal cell carcinoma** that typically presents with a mass in the renal medulla, often with central necrosis.
- Its histological features involve atypical cells arranged in **tubules or ducts**, which does not match the description of compact cells with eosinophilic cytoplasm.
*Oncocytic carcinoma*
- **Oncocytic carcinoma** is a rare and generally benign tumor. It is characterized histologically by cells with abundant, granular eosinophilic cytoplasm.
- While it has eosinophilic cytoplasm, it lacks the prominent nucleoli and compact cell arrangement seen in the biopsy, and it is not typically associated with VHL syndrome.
*Papillary carcinoma*
- **Papillary carcinoma** is characterized by cells arranged in papillary formations or tubular structures. It is generally associated with different genetic syndromes (e.g., hereditary papillary renal carcinoma).
- The histological description provided, particularly the "compact cells" and vasculature, does not fit the typical papillary architecture.
*Chromophobe carcinoma*
- **Chromophobe carcinoma** is characterized by large cells with distinct cell borders and pale, flocculent cytoplasm. It typically has a good prognosis.
- This type of carcinoma is generally not associated with VHL syndrome and its histological features do not align with the biopsy description of compact cells with eosinophilic cytoplasm and prominent nucleoli.
Laboratory techniques in pathology US Medical PG Question 7: A 72-year-old man goes to his primary care provider for a checkup after some blood work showed lymphocytosis 3 months ago. He says he has been feeling a bit more tired lately but doesn’t complain of any other symptoms. Past medical history is significant for hypertension and hyperlipidemia. He takes lisinopril, hydrochlorothiazide, and atorvastatin. Additionally, his right hip was replaced three years ago due to osteoarthritis. Family history is noncontributory. He drinks socially and does not smoke. Today, he has a heart rate of 95/min, respiratory rate of 17/min, blood pressure of 135/85 mm Hg, and temperature of 36.8°C (98.2°F). On physical exam, he looks well. His heartbeat has a regular rate and rhythm and lungs that are clear to auscultation bilaterally. Additionally, he has mild lymphadenopathy of his cervical lymph nodes. A complete blood count with differential shows the following:
Leukocyte count 5,000/mm3
Red blood cell count 3.1 million/mm3
Hemoglobin 11.0 g/dL
MCV 95 um3
MCH 29 pg/cell
Platelet count 150,000/mm3
Neutrophils 40%
Lymphocytes 40%
Monocytes 5%
A specimen is sent for flow cytometry that shows a population that is CD 5, 19, 20, 23 positive. Which of the following is the most likely diagnosis?
- A. Chronic lymphocytic leukemia (Correct Answer)
- B. Immune thrombocytopenic purpura
- C. Aplastic anemia
- D. Acute lymphoblastic leukemia
- E. Tuberculosis
Laboratory techniques in pathology Explanation: ***Chronic lymphocytic leukemia***
- The patient presents with mild **lymphadenopathy**, a **history of lymphocytosis**, and a **flow cytometry** showing cells positive for **CD5, CD19, CD20, and CD23**, which is pathognomonic for **CLL**.
- While the total leukocyte count is within normal limits due to the absolute neutrophil decrease, the persistent lymphocytosis and characteristic immunophenotype are highly indicative of CLL.
*Immune thrombocytopenic purpura*
- This condition is characterized by **isolated thrombocytopenia** caused by autoantibody-mediated platelet destruction, which is not supported by the patient's normal platelet count (150,000/mm3).
- While it can cause fatigue, it doesn't explain the lymphocytosis or the specific **CD marker profile**.
*Aplastic anemia*
- Aplastic anemia involves **pancytopenia** (decreased red blood cells, white blood cells, and platelets) due to bone marrow failure, which is not consistent with the patient's normal-range leukocyte and platelet counts.
- The patient's presentation with lymphocytosis and lymphadenopathy further makes this diagnosis unlikely.
*Acute lymphoblastic leukemia*
- **ALL** typically presents with symptoms related to **bone marrow failure** (anemia, thrombocytopenia, infections) and often very **high blast counts** in the peripheral blood and bone marrow.
- While it involves lymphocytes, the specific **CD5/19/20/23 co-expression** is characteristic of CLL, and ALL usually involves more aggressive symptoms and a different immunophenotype.
*Tuberculosis*
- **Tuberculosis** is an infectious disease that can cause **lymphadenopathy** and systemic symptoms like fatigue, but it is typically associated with a **caseating granulomatous inflammation** and is diagnosed via cultures or PCR rather than flow cytometry.
- It would not explain the specific **B-cell lymphocytosis** with the described immunophenotype.
Laboratory techniques in pathology US Medical PG Question 8: A 13-year-old boy is brought to the physician because of swelling around his eyes for the past 2 days. His mother also notes that his urine became gradually darker during this time. Three weeks ago, he was treated for bacterial tonsillitis. His temperature is 37.6°C (99.7°F), pulse is 79/min, and blood pressure is 158/87 mm Hg. Examination shows periorbital swelling. Laboratory studies show:
Serum
Urea nitrogen 9 mg/dL
Creatinine 1.7 mg/dL
Urine
Protein 2+
RBC 12/hpf
RBC casts numerous
A renal biopsy would most likely show which of the following findings?
- A. Effacement of podocyte foot processes on electron microscopy
- B. Granular deposits of IgG, IgM, and C3 on immunofluorescence (Correct Answer)
- C. Splitting and alternating thickening and thinning of the glomerular basement membrane on light microscopy
- D. Mesangial IgA deposits on immunofluorescence
- E. "Spike-and-dome" appearance of subepithelial deposits on electron microscopy
Laboratory techniques in pathology Explanation: ***Granular deposits of IgG, IgM, and C3 on immunofluorescence***
- This finding is characteristic of **post-streptococcal glomerulonephritis (PSGN)**, supported by the history of recent tonsillitis, periorbital swelling, dark urine, hypertension, and features of nephritic syndrome (RBC casts, proteinuria).
- The granular deposition pattern reflects the immune complex-mediated nature of PSGN, where **antigen-antibody complexes** deposit in the glomeruli.
*Effacement of podocyte foot processes on electron microscopy*
- This is the hallmark finding in **minimal change disease**, which typically presents with abrupt onset of nephrotic syndrome (severe proteinuria, hypoalbuminemia, edema) without hematuria or hypertension.
- The patient's presentation with **dark urine** (hematuria), hypertension, and RBC casts is inconsistent with minimal change disease.
*Splitting and alternating thickening and thinning of the glomerular basement membrane on light microscopy*
- This describes the characteristic changes seen in **Alport syndrome**, an inherited disorder affecting collagen IV.
- Alport syndrome presents with **hematuria**, progressive renal failure, and often includes hearing loss and ocular abnormalities, which are not mentioned in this acute presentation.
*Mesangial IgA deposits on immunofluorescence*
- This is the diagnostic feature of **IgA nephropathy (Berger's disease)**.
- IgA nephropathy often presents with **recurrent macroscopic hematuria** occurring concurrent with or shortly after an upper respiratory infection, rather than 2-3 weeks later like PSGN.
*"Spike-and-dome" appearance of subepithelial deposits on electron microscopy*
- This appearance is characteristic of **membranous nephropathy**, which is a common cause of **nephrotic syndrome** in adults.
- Membranous nephropathy typically presents with significant proteinuria and edema, and it is less common in children with acute nephritic symptoms like those described.
Laboratory techniques in pathology US Medical PG Question 9: A 63-year-old man comes to the physician because of increasing generalized fatigue for 3 months. He is having more difficulty with keeping up with his activities of daily living and has lost 2.5 kg (5.5 lb) over the past month. He has hypertension and hyperlipidemia. He does not smoke and drinks two to three beers on weekends. His medications include lisinopril, hydrochlorothiazide, and atorvastatin. His temperature is 37.1°C (98.8°F), pulse is 85/min, respirations are 15/min, and blood pressure is 125/73 mm Hg. Examination shows pale conjunctivae. The remainder of the examination shows no abnormalities. His hematocrit is 27.3%, leukocyte count is 4500/mm3, and platelet count is 102,000/mm3. A peripheral blood smear shows numerous blast cells that stain positive for myeloperoxidase, CD33, and CD34. Which of the following is the most likely diagnosis?
- A. Non-Hodgkin lymphoma
- B. Acute myeloid leukemia (Correct Answer)
- C. Hairy cell leukemia
- D. Chronic lymphocytic leukemia
- E. Acute lymphoblastic leukemia
Laboratory techniques in pathology Explanation: ***Acute myeloid leukemia***
- The presence of **numerous blast cells** that stain positive for **myeloperoxidase (MPO)** and **CD33** is highly characteristic of **acute myeloid leukemia (AML)**.
- The patient's symptoms of **fatigue**, **weight loss**, **pale conjunctivae (anemia)**, and **pancytopenia** (low hematocrit, leukopenia, thrombocytopenia) are consistent with bone marrow infiltration by leukemic blasts.
*Non-Hodgkin lymphoma*
- Characterized by **lymphadenopathy** and systemic 'B' symptoms (fever, night sweats, weight loss), which are not prominent features here.
- While it can cause cytopenias, the presence of **myeloperoxidase-positive blasts** would point away from lymphoma, which involves lymphocytes.
*Hairy cell leukemia*
- Typically presents with **pancytopenia**, **splenomegaly**, and characteristic **hairy cells** on peripheral smear.
- These cells are **CD103, CD123, and CD25 positive** and tartrate-resistant acid phosphatase (TRAP) positive, which differs from the findings in this case.
*Chronic lymphocytic leukemia*
- Characterized by an accumulation of **mature-appearing lymphocytes** (not blasts) in the blood, bone marrow, and lymph nodes.
- These cells typically express **CD5 and CD20**, and **myeloperoxidase** would be negative.
*Acute lymphoblastic leukemia*
- Involves **lymphoblasts**, which are typically **MPO-negative** and express lymphoid markers like **CD10, CD19, and CD22**.
- While it can present with similar symptoms and pancytopenia as AML, the **MPO positivity rules it out**.
Laboratory techniques in pathology US Medical PG Question 10: A 47-year-old woman comes to the physician because of a 2-month history of a lump on her neck and a 1-week history of hoarseness. Examination shows a 3-cm, firm, non-tender nodule on the anterior neck. Further evaluation confirms a thyroid malignancy, and she undergoes thyroidectomy. Histopathologic examination of the surgical specimen shows lymphatic invasion. Genetic analysis shows an activating mutation in the RET/PTC genes. Microscopic examination of the surgical specimen is most likely to also show which of the following?
- A. Pleomorphic giant cells with numerous atypical mitotic figures
- B. Cuboidal cells arranged spherically around colloid lakes
- C. Hyperplastic epithelium with colloid scalloping
- D. Calcified spherules and large oval cells with empty-appearing nuclei (Correct Answer)
- E. Sheets of polygonal cells surrounding amyloid deposition
Laboratory techniques in pathology Explanation: ***Calcified spherules and large oval cells with empty-appearing nuclei***
- The presence of an **activating mutation in RET/PTC genes**, **lymphatic invasion**, and a new neck lump with hoarseness (suggesting nerve involvement) are highly characteristic of **papillary thyroid carcinoma**.
- Microscopic features of papillary thyroid carcinoma include **Psammoma bodies (calcified spherules)**, **Orphan Annie eye nuclei (large oval cells with empty-appearing nuclei)**, and nuclear grooves.
*Pleomorphic giant cells with numerous atypical mitotic figures*
- This description typically refers to **anaplastic thyroid carcinoma**, a highly aggressive and undifferentiated tumor.
- While anaplastic carcinoma can present with rapid growth and hoarseness, it is less commonly associated with a **RET/PTC mutation** (BRAF mutations are more common) and typically has a much poorer prognosis, often presenting with a rapidly enlarging mass rather than a 2-month history suggestive of a more indolent tumor.
*Cuboidal cells arranged spherically around colloid lakes*
- This morphology is characteristic of **follicular thyroid carcinoma** or **follicular adenoma**.
- While follicular tumors can have RET/PTC mutations in some variants, the classic features described (empty-appearing nuclei and psammoma bodies) are absent here.
*Hyperplastic epithelium with colloid scalloping*
- This describes the histologic features seen in **Graves' disease** or **diffuse toxic goiter**, a benign condition.
- It is not indicative of malignancy, and the patient's presentation with a solitary nodule and hoarseness points to a malignant process.
*Sheets of polygonal cells surrounding amyloid deposition*
- This is the classic microscopic appearance of **medullary thyroid carcinoma**.
- Medullary thyroid carcinoma is also associated with **RET mutations**, but these are typically **germline or somatic RET point mutations** (e.g., RET M918T), not RET/PTC rearrangements, and it arises from parafollicular C cells, producing calcitonin, not thyroid hormones.
More Laboratory techniques in pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.