Hemodynamic disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hemodynamic disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hemodynamic disorders US Medical PG Question 1: A 26-year-old man presents with a 2-day history of worsening right lower leg pain. He states that he believes his right leg is swollen when compared to his left leg. Past medical history is significant for generalized anxiety disorder, managed effectively with psychotherapy. He smokes a pack of cigarettes daily but denies alcohol and illicit drug use. His father died of a pulmonary embolism at the age of 43. His vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, respiratory rate 14/min. On physical examination, the right lower leg is warmer than the left, and dorsiflexion of the right foot produces pain. Which of the following conditions is most likely responsible for this patient’s presentation?
- A. Vitamin K deficiency
- B. Hemophilia A
- C. von Willebrand disease
- D. Factor V Leiden (Correct Answer)
- E. Factor XI deficiency
Hemodynamic disorders Explanation: ***Factor V Leiden***
- The patient presents with classic symptoms of a **deep vein thrombosis (DVT)** in the right lower leg: pain, swelling, warmth, and pain on dorsiflexion (**Homans' sign**). His history of smoking and a family history of **pulmonary embolism (PE)** in a young father strongly suggest an underlying **thrombophilia**.
- **Factor V Leiden** is the most common inherited thrombophilia, predisposing individuals to venous thromboembolism. The constellation of symptoms and risk factors points directly to this condition.
*Vitamin K deficiency*
- **Vitamin K deficiency** primarily leads to impaired production of clotting factors II, VII, IX, and X, resulting in a **bleeding diathesis**, not thrombotic events.
- Patients would typically present with **bruising, petechiae, gastrointestinal bleeding, or hematuria**, which are not seen here.
*Hemophilia A*
- **Hemophilia A** is an X-linked recessive disorder characterized by a deficiency of **Factor VIII**, leading to severe **bleeding**.
- Symptoms include **spontaneous or prolonged bleeding** into joints (hemarthrosis), muscles, or following trauma, which is the opposite of the patient's presentation.
*von Willebrand disease*
- **Von Willebrand disease (vWD)** is the most common inherited bleeding disorder, caused by a deficiency or defect in **von Willebrand factor**.
- It primarily causes **mucocutaneous bleeding**, such as epistaxis, menorrhagia, and easy bruising, not thrombotic episodes.
*Factor XI deficiency*
- **Factor XI deficiency** is a rare inherited bleeding disorder that typically causes **mild to moderate bleeding**, often associated with trauma or surgery.
- It is not associated with an increased risk of thrombosis and would present with bleeding, not a DVT.
Hemodynamic disorders US Medical PG Question 2: A 70-year-old woman is on hospital day 2 in the medical intensive care unit. She was admitted from the emergency department for a 2-day history of shortness of breath and fever. In the emergency department, her temperature is 39.4°C (103.0°F), the pulse is 120/min, the blood pressure is 94/54 mm Hg, the respiratory rate is 36/min, and oxygen saturation was 82% while on 4L of oxygen via a non-rebreather mask. Chest X-ray shows a right lower lobe consolidation. She was intubated, sedated, and started on broad-spectrum antibiotics for sepsis of pulmonary origin and intravenous norepinephrine for blood pressure support. Since then, her clinical condition has been stable, though her vasopressor and oxygen requirements have not improved. Today, her physician is called to the bedside because her nurse noted some slow bleeding from her intravenous line sites and around her urinary catheter. Which of the following most likely represents the results of coagulation studies for this patient?
- A. D-dimer: negative, fibrinogen level: low, platelet count: low
- B. D-dimer: elevated, fibrinogen level: normal, platelet count: normal
- C. D-dimer: elevated, fibrinogen level: low, platelet count: low (Correct Answer)
- D. D-dimer: negative, fibrinogen level: elevated, platelet count: elevated
- E. D-dimer: negative, fibrinogen level: normal, platelet count: normal
Hemodynamic disorders Explanation: ***D-dimer: elevated, fibrinogen level: low, platelet count: low***
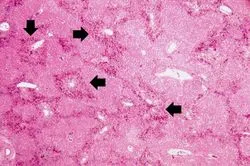
- The patient's presentation with **sepsis** requiring intubation and vasopressors, along with diffuse **bleeding from IV sites and urinary catheter**, strongly suggests **disseminated intravascular coagulation (DIC)**.
- In DIC, widespread activation of the coagulation cascade leads to consumption of **platelets** and **clotting factors (including fibrinogen)**, resulting in thrombocytopenia and hypofibrinogenemia. The breakdown of clots produces **elevated D-dimer** levels.
*D-dimer: negative, fibrinogen level: low, platelet count: low*
- A **negative D-dimer** would contradict the diagnosis of DIC, as D-dimer is a product of fibrin degradation and is almost always elevated in DIC due to extensive clot formation and subsequent fibrinolysis.
- While low fibrinogen and platelet count are characteristic of DIC, the negative D-dimer makes this option unlikely in the context of active bleeding from multiple sites.
*D-dimer: elevated, fibrinogen level: normal, platelet count: normal*
- While an **elevated D-dimer** is consistent with fibrinolysis occurring in DIC, normal **fibrinogen** and **platelet counts** would argue against the consumptive coagulopathy that defines DIC.
- The presence of diffuse bleeding in a patient with sepsis usually indicates significant depletion of clotting factors and platelets.
*D-dimer: negative, fibrinogen level: elevated, platelet count: elevated*
- This profile suggests an **inflammatory state** or a hypercoagulable state without significant fibrinolysis or consumption of clotting factors.
- A **negative D-dimer** and **elevated fibrinogen/platelets** contradict the signs and symptoms of DIC with active bleeding.
*D-dimer: negative, fibrinogen level: normal, platelet count: normal*
- This result would be inconsistent with **DIC** and the patient's clinical picture of widespread bleeding.
- In DIC, there is active coagulation and fibrinolysis, leading to consumption of platelets and fibrinogen and production of D-dimers.
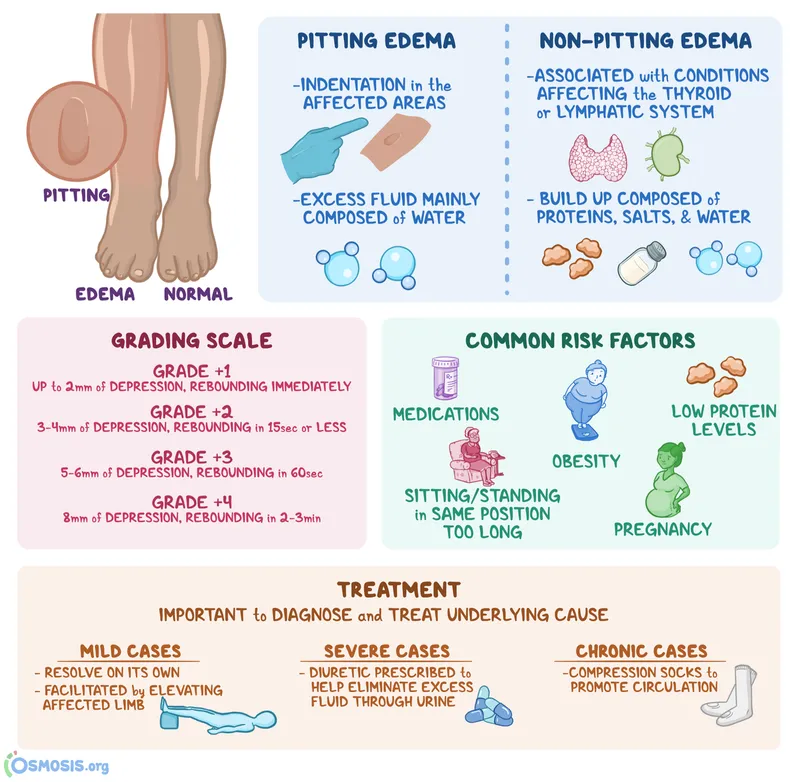
Hemodynamic disorders US Medical PG Question 3: A 72-year-old woman with hypertension comes to the physician because of swelling and pain in both legs for the past year. The symptoms are worse at night and improve in the morning. Current medications include losartan and metoprolol. Her temperature is 36°C (96.8°F), pulse is 67/min, and blood pressure is 142/88 mm Hg. Examination shows normal heart sounds; there is no jugular venous distention. Her abdomen is soft and the liver edge is not palpable. Examination of the lower extremities shows bilateral pitting edema and prominent superficial veins. The skin is warm and there is reddish-brown discoloration of both ankles. Laboratory studies show a normal serum creatinine and normal urinalysis. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Decreased arteriolar resistance
- B. Increased venous valve reflux (Correct Answer)
- C. Decreased intravascular oncotic pressure
- D. Decreased lymphatic flow
- E. Increased capillary permeability
Hemodynamic disorders Explanation: ***Increased venous valve reflux***
- The patient presents with **bilateral pitting edema**, **prominent superficial veins**, and **reddish-brown discoloration of the ankles**, which are classic signs of **chronic venous insufficiency**.
- **Venous valve reflux** leads to increased hydrostatic pressure in the capillaries, causing fluid transudation into the interstitial space, leading to edema that is worse at night and improves with elevation.
*Decreased arteriolar resistance*
- **Decreased arteriolar resistance** can lead to increased blood flow to the capillaries, but it typically causes edema that is **warm and erythematous**, often in the context of inflammation or certain medications (e.g., dihydropyridine calcium channel blockers), which is not the primary mechanism here.
- While some medications can cause edema, the full clinical picture points more specifically to venous stasis.
*Decreased intravascular oncotic pressure*
- **Decreased intravascular oncotic pressure** (e.g., due to low albumin from liver disease or nephrotic syndrome) causes **generalized edema** that is often symmetrical, but it would not typically cause prominent superficial veins or reddish-brown ankle discoloration.
- The patient's normal liver exam and creatinine/urinalysis make this less likely.
*Decreased lymphatic flow*
- **Decreased lymphatic flow** results in **lymphedema**, which is typically **non-pitting**, unilateral, and does not cause prominent superficial veins or pigment changes initially.
- Lymphedema often leads to a "woody" texture and can be associated with skin thickening over time.
*Increased capillary permeability*
- **Increased capillary permeability** can cause edema, often due to **inflammation**, allergic reactions, or sepsis, and typically presents with warmth, erythema, and localized swelling.
- This mechanism is usually acute and does not primarily explain the chronic skin changes and prominent veins seen in this patient.
Hemodynamic disorders US Medical PG Question 4: A 72-year-old man presents with shortness of breath and right-sided chest pain. Physical exam reveals decreased breath sounds and dull percussion at the right lung base. Chest X-ray reveals a right-sided pleural effusion. A thoracentesis was performed, removing 450 mL of light pink fluid. Pleural fluid analysis reveals:
Pleural fluid to serum protein ratio: 0.35
Pleural fluid to serum LDH ratio: 0.49
Lactate dehydrogenase (LDH): 105 IU (serum LDH Reference: 100–190)
Which of the following disorders is most likely in this patient?
- A. Congestive heart failure (Correct Answer)
- B. Uremia
- C. Chylothorax
- D. Pancreatitis
- E. Sarcoidosis
Hemodynamic disorders Explanation: ***Congestive heart failure***
- The **pleural fluid to serum protein ratio of 0.35** and **LDH ratio of 0.49** fall within the criteria for a **transudative effusion** (ratios < 0.5 for protein and < 0.6 for LDH).
- **Congestive heart failure (CHF)** is a common cause of transudative pleural effusions due to increased hydrostatic pressure.
*Uremia*
- **Uremic pleuritis** typically causes an **exudative effusion**, characterized by higher protein and LDH levels in the pleural fluid.
- While patients with uremia may have pleural effusions, the fluid analysis here is not consistent with that diagnosis.
*Chylothorax*
- A **chylothorax** is characterized by a **milky-white fluid** with very high triglyceride levels (>110 mg/dL), resulting from lymphatic leakage.
- The described fluid is "light pink" and does not have the typical biochemical profile of a chylothorax.
*Pancreatitis*
- **Pancreatitis-induced pleural effusions** are almost always **exudative** and typically have **elevated amylase levels**.
- The transudative nature of the effusion rules out pancreatitis as the most likely cause.
*Sarcoidosis*
- **Sarcoidosis** can cause **pleural effusions**, but these are usually **exudative** and often accompanied by other systemic manifestations like lymphadenopathy or skin lesions.
- The presented fluid analysis does not support a diagnosis of sarcoidosis.
Hemodynamic disorders US Medical PG Question 5: A 38-year-old male is brought to the emergency department by ambulance after a motor vehicle collision. He is found to have a broken femur and multiple soft tissue injuries and is admitted to the hospital. During the hospital course, he is found to have lower extremity swelling, redness, and pain, so he is given an infusion of a medication. The intravenous medication is discontinued in favor of an oral medication in preparation for discharge; however, the patient leaves against medical advice prior to receiving the full set of instructions. The next day, the patient is found to have black lesions on his trunk and his leg. The protein involved in this patient's underlying abnormality most likely affects the function of which of the following factors?
- A. Factor II only
- B. Factors II, VII, IX, and X
- C. Factors II and X
- D. Factors V and VIII (Correct Answer)
- E. Factor V only
Hemodynamic disorders Explanation: ***Factors V and VIII***
- The patient's initial presentation of **lower extremity swelling, redness, and pain** after trauma and immobilization is highly suggestive of **deep vein thrombosis (DVT)**, for which he received IV anticoagulation. The subsequent development of **black lesions on his trunk and leg** after switching to an oral anticoagulant and leaving against medical advice points to **warfarin-induced skin necrosis (WISN)**.
- **Warfarin-induced skin necrosis** develops in patients with a congenital deficiency of **protein C** or, less commonly, **protein S**. Protein C, in its activated form (APC), functions to inactivate **Factor V (Va)** and **Factor VIII (VIIIa)**, which are crucial cofactors in the coagulation cascade. A deficiency means these factors remain active, leading to a **procoagulant state**.
*Factor II only*
- **Factor II (prothrombin)** is inactivated by protein C, but a deficiency in protein C primarily affects the inactivation of **Factors V and VIII**, which are the specific targets of activated protein C.
- While factor II is part of the coagulation cascade, its regulation is not the primary mechanism by which protein C deficiency leads to the hypercoagulable state seen in WISN.
*Factors II, VII, IX, and X*
- These factors are **vitamin K-dependent coagulation factors**, which are inhibited by warfarin. While a deficiency in protein C can lead to an initial hypercoagulable state when warfarin is started (due to the faster drop in protein C levels compared to these factors), the primary function of protein C is to inactivate **Factors V and VIII**.
- The problem described is a **protein C deficiency**, which specifically impacts the inactivation of factors V and VIII, not directly these other vitamin K-dependent factors.
*Factors II and X*
- Similar to Factor II only, these are **vitamin K-dependent factors** inhibited by warfarin. The core issue in warfarin-induced skin necrosis is a deficiency in protein C, which normally inactivates **Factors V and VIII**, leading to a transient prothrombotic state.
- While Factor X is affected by warfarin, the direct regulatory role of protein C is predominantly on factors V and VIII.
*Factor V only*
- While **Factor V** is indeed a target of activated protein C inactivation, **Factor VIII** is also a critical target. Inactivating both **Factor V** and **Factor VIII** is essential for effective anticoagulation by protein C.
- A deficiency in protein C affects both of these crucial cofactors, making the combined option more accurate.
Hemodynamic disorders US Medical PG Question 6: A 56-year-old man presents to his general practitioner with frequent episodes of facial flushing for the past 2 weeks. He says the episodes are associated with mild headaches and a sensation of fullness in his head and neck. Additionally, he has developed recurrent, often severe, itching after taking a hot shower. The patient denies any smoking history but says he drinks alcohol socially. His blood pressure is 160/90 mm Hg, and his temperature is 37.0°C (98.6°F). On physical examination, his face and neck appear red. Cardiac examination reveals a regular rate and rhythm. Lungs are clear to auscultation bilaterally. The spleen is noted to be palpable just below the costal margin. A complete blood count shows a hemoglobin level of 19.5 g/dL, a total leukocyte count of 12,000/mm3, and a platelet count of 450,000/mm3. Which of the following sets of abnormalities is most likely present in this patient?
- A. ↑ Blood viscosity, ↓ blood flow with an M-spike of immunoglobulin G
- B. ↑ Blood viscosity, ↓ blood flow, ↓ erythropoietin (Correct Answer)
- C. ↑ Blood viscosity, ↓ blood flow with blast cells
- D. ↑ Blood viscosity, ↓ blood flow with an M-spike of immunoglobulin M
- E. ↓ Blood viscosity, ↑ blood flow, ↓ erythropoietin, ↑ ferritin
Hemodynamic disorders Explanation: ***↑ Blood viscosity, ↓ blood flow, ↓ erythropoietin***
- The patient's symptoms (facial flushing, headaches, fullness in head/neck, **post-shower pruritus**) and lab findings (hemoglobin **19.5 g/dL**, elevated WBC and platelets) are classic for **polycythemia vera (PV)**.
- In polycythemia vera, the increased red blood cell mass leads to **increased blood viscosity** and thus **decreased blood flow**, causing hyperviscosity symptoms.
- The excess RBC production is driven by autonomous proliferation (typically due to **JAK2 V617F mutation**), which occurs independently of erythropoietin. The elevated RBC mass suppresses **erythropoietin** levels through negative feedback from the kidneys.
- Post-shower pruritus (aquagenic pruritus) is pathognomonic for PV and results from basophil and mast cell degranulation triggered by temperature changes.
*↑ Blood viscosity, ↓ blood flow with an M-spike of immunoglobulin G*
- While increased blood viscosity and decreased blood flow occur in polycythemia vera, an **M-spike of immunoglobulin G** is characteristic of **multiple myeloma**, not polycythemia vera.
- Multiple myeloma presents with anemia (not erythrocytosis), bone pain, hypercalcemia, and renal dysfunction.
*↑ Blood viscosity, ↓ blood flow with blast cells*
- The presence of **blast cells** in peripheral blood would suggest **acute leukemia**, which is not supported by this clinical picture.
- Polycythemia vera is a chronic myeloproliferative neoplasm; blast cells are generally absent in the peripheral blood unless there is transformation to acute leukemia (rare complication).
*↑ Blood viscosity, ↓ blood flow with an M-spike of immunoglobulin M*
- An **M-spike of immunoglobulin M** is a hallmark of **Waldenström macroglobulinemia**, a lymphoplasmacytic lymphoma.
- While Waldenström can cause hyperviscosity syndrome, it presents with anemia, not erythrocytosis, along with lymphadenopathy and hepatosplenomegaly from lymphoid infiltration.
*↓ Blood viscosity, ↑ blood flow, ↓ erythropoietin, ↑ ferritin*
- **Decreased blood viscosity** and **increased blood flow** would occur in anemia, which is the opposite of this patient's presentation with significantly elevated hemoglobin.
- While erythropoietin is indeed decreased in polycythemia vera, **↑ ferritin** is not a primary feature and would be more suggestive of iron overload (hemochromatosis) or an acute phase response to inflammation.
Hemodynamic disorders US Medical PG Question 7: An 8-year-old boy is shifted to a post-surgical floor following neck surgery. The surgeon has restricted his oral intake for the next 24 hours. He does not have diarrhea, vomiting, or dehydration. His calculated fluid requirement is 1500 mL/day. However, he receives 2000 mL of intravenous isotonic fluids over 24 hours. Which of the following physiological parameters in the boy’s circulatory system is most likely to be increased?
- A. Interstitial oncotic pressure
- B. Interstitial hydrostatic pressure
- C. Capillary wall permeability
- D. Capillary oncotic pressure
- E. Capillary hydrostatic pressure (Correct Answer)
Hemodynamic disorders Explanation: ***Capillary hydrostatic pressure***
- Giving 2000 mL of intravenous isotonic fluids when the calculated requirement is 1500 mL/day leads to a **positive fluid balance** and **fluid overload**.
- This excess fluid directly increases the **intravascular volume**, thereby raising the **capillary hydrostatic pressure**, which pushes fluid out of the capillaries.
*Interstitial oncotic pressure*
- This pressure is primarily determined by the **protein concentration** in the interstitial fluid.
- While fluid overload can dilute interstitial proteins, it generally does not directly increase interstitial oncotic pressure; rather, it might decrease it due to fluid movement.
*Interstitial hydrostatic pressure*
- As fluid moves out of the capillaries due to increased capillary hydrostatic pressure, the **interstitial hydrostatic pressure** will also increase.
- However, the primary driving force for this change, and thus the most direct consequence of fluid overload, is the increase in capillary hydrostatic pressure.
*Capillary wall permeability*
- This parameter refers to the ease with which substances, including fluid and proteins, can cross the capillary wall.
- Fluid overload does not typically affect **capillary wall permeability** unless there is an underlying condition causing inflammation or damage to the capillary endothelium.
*Capillary oncotic pressure*
- This pressure is mainly determined by the **protein concentration** within the capillaries.
- In a state of fluid overload with isotonic fluids, the plasma proteins are diluted, leading to a **decrease** in capillary oncotic pressure, not an increase.
Hemodynamic disorders US Medical PG Question 8: A 27-year-old man is brought to the emergency department by emergency medical services. The patient was an unrestrained passenger in a head-on collision that occurred 15 minutes ago and is currently unresponsive. His temperature is 99.5°F (37.5°C), blood pressure is 60/33 mmHg, pulse is 180/min, respirations are 17/min, and oxygen saturation is 95% on room air. A FAST exam demonstrates fluid in Morrison’s pouch. Laboratory values are drawn upon presentation to the ED and sent off. The patient is started on IV fluids and an initial trauma survey is started. Twenty minutes later, his blood pressure is 95/65 mmHg, and his pulse is 110/min. The patient is further stabilized and is scheduled for emergency surgery. Which of the following best represents this patient’s most likely initial laboratory values?
- A. Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3
- B. Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3
- C. Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3
- D. Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3 (Correct Answer)
- E. Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3
Hemodynamic disorders Explanation: ***Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3***
- The patient experienced significant trauma and is experiencing **hemorrhagic shock**, as evidenced by his initial **hypotension** (BP 60/33 mmHg), **tachycardia** (pulse 180/min), and positive **FAST exam** for fluid in Morrison's pouch, indicating intra-abdominal bleeding.
- The initial hemoglobin and hematocrit could be mildly decreased due to acute blood loss, but significant drops are often *not immediately apparent* as plasma volume has not yet moved into the intravascular compartment to dilute the remaining red blood cells. A hemoglobin of 11 g/dL and hematocrit of 33% are consistent with **acute blood loss** before significant hemodilution occurs. MCV of 88 µm^3 is within the normal range for **normocytic anemia** seen in acute hemorrhage.
*Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3*
- While a hemoglobin of 10 g/dL and hematocrit of 30% are consistent with anemia due to blood loss, an **MCV of 110 µm^3** (macrocytic) is not typically seen in acute hemorrhage.
- Macrocytic anemia usually results from conditions like **B12 or folate deficiency**, alcoholism, or liver disease, which are not suggested by the acute traumatic scenario.
*Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3*
- This indicates **polycythemia** (abnormally high red blood cell count), which is the opposite of what would be expected in a patient experiencing acute hemorrhagic shock.
- These values would suggest conditions like **polycythemia vera** or severe dehydration, which are not relevant in this acute trauma setting.
*Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3*
- While a hemoglobin of 7 g/dL and hematocrit of 21% represent significant anemia consistent with major blood loss, these values are typically seen *later* as **hemodilution** occurs, or in cases of chronic blood loss.
- An **MCV of 75 µm^3** (microcytic) is generally indicative of **iron deficiency anemia** or thalassemia, which develops over time and is not characteristic of acute traumatic blood loss.
*Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3*
- These values are within the **normal range** for hemoglobin and hematocrit, which would not be expected in a patient presenting with signs of **hemorrhagic shock** and a positive FAST exam indicating significant internal bleeding.
- This would suggest either very minor blood loss or that the values were taken before any bleeding had occurred or before hemodilution had a chance to manifest.
Hemodynamic disorders US Medical PG Question 9: A 25-year-old woman comes to the physician because of recurrent episodes of reddish discoloration of her urine. She also has a 3-month history of intermittent abdominal pain, yellowish discoloration of the skin and eyes, and fatigue. Physical examination shows pallor and scleral icterus. The spleen is not palpable. Her hemoglobin concentration is 7.8 g/dL, leukocyte count is 2,000/mm3, and platelet count is 80,000/mm3. Serum LDH and unconjugated bilirubin concentrations are elevated. Addition of a serum containing anti-human globulins to a blood sample shows no agglutination. A urine dipstick shows blood; urinalysis shows no RBCs. A CT scan of the abdomen shows a thrombus in a distal branch of the superior mesenteric vein. Which of the following is the most likely cause of this patient's condition?
- A. Activation and consumption of platelets and coagulation factors
- B. Absence of protective factors against destruction by complement (Correct Answer)
- C. Replacement of a single amino acid in a β-globin chain
- D. Formation of IgG antibodies against glycoprotein IIb/IIIa
- E. Endothelial cell dysfunction from bacterial toxin production
Hemodynamic disorders Explanation: ***Absence of protective factors against destruction by complement***
- The patient's presentation is **classic for Paroxysmal Nocturnal Hemoglobinuria (PNH)**: hemoglobinuria (positive urine dipstick with no RBCs), intravascular hemolysis (elevated LDH/unconjugated bilirubin), pancytopenia, negative Coombs test, and venous thrombosis.
- PNH is caused by an acquired **PIGA gene mutation** leading to deficiency of **GPI-anchored proteins CD55 and CD59** on hematopoietic cells.
- Without these complement regulatory proteins, red blood cells undergo uncontrolled **complement-mediated hemolysis**, and platelet activation leads to thrombotic complications.
*Activation and consumption of platelets and coagulation factors*
- This describes **Disseminated Intravascular Coagulation (DIC)**, which presents with both bleeding and thrombosis, prolonged PT/aPTT, decreased fibrinogen, and elevated D-dimer.
- While PNH can cause thrombosis, the primary pathophysiology is complement dysregulation, not consumption coagulopathy. The negative Coombs test, hemoglobinuria pattern, and pancytopenia point to PNH rather than DIC.
*Replacement of a single amino acid in a β-globin chain*
- This describes **sickle cell disease** (glutamic acid → valine substitution in β-globin), causing RBC sickling under hypoxic conditions.
- Sickle cell typically presents with painful vaso-occlusive crises, acute chest syndrome, and splenic sequestration. The hemoglobinuria without RBCs, pancytopenia, and mesenteric vein thrombosis are characteristic of PNH, not sickle cell disease.
*Formation of IgG antibodies against glycoprotein IIb/IIIa*
- This describes **Immune Thrombocytopenic Purpura (ITP)**, characterized by isolated thrombocytopenia with mucocutaneous bleeding.
- ITP does not cause hemolytic anemia, leukopenia, hemoglobinuria, or thrombosis—features central to this patient's presentation.
*Endothelial cell dysfunction from bacterial toxin production*
- This describes **Hemolytic Uremic Syndrome (HUS)**, typically caused by Shiga toxin-producing E. coli, presenting with the classic triad: microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury.
- HUS features schistocytes on blood smear and renal failure, not pancytopenia or the typical venous thrombosis pattern seen in PNH.
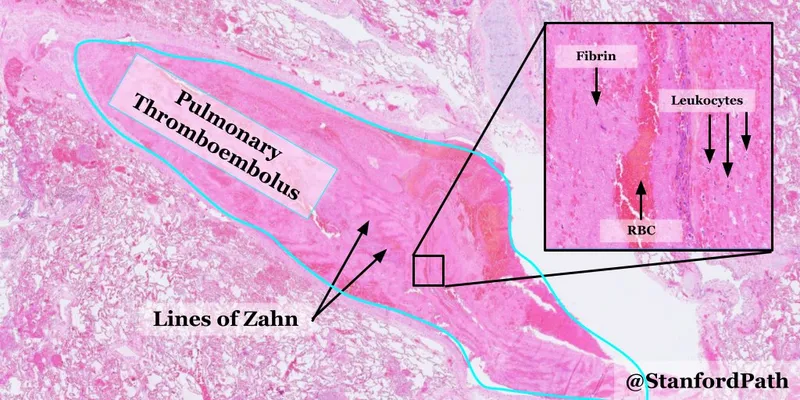
Hemodynamic disorders US Medical PG Question 10: A 73-year-old man with coronary artery disease and hypertension is brought to the emergency department by ambulance 90 minutes after the acute onset of substernal chest pain and dyspnea. He has smoked 2 packs of cigarettes daily for 52 years. Shortly after arriving at the hospital, he loses consciousness and is pulseless. Despite attempts at cardiopulmonary resuscitation, he dies. Examination of the heart at autopsy shows complete occlusion of the left anterior descending artery with a red thrombus overlying a necrotic plaque. Which of the following pathophysiologic mechanisms is most likely responsible for this patient's acute coronary condition?
- A. Influx of lipids into the endothelium
- B. Secretion of matrix metalloproteinases (Correct Answer)
- C. Release of platelet-derived growth factor
- D. Type III collagen deposition
- E. Proliferation of smooth muscle cells
Hemodynamic disorders Explanation: ***Secretion of matrix metalloproteinases***
- **Matrix metalloproteinases (MMPs)** degrade the **extracellular matrix** within the fibrous cap of an atherosclerotic plaque, leading to its **destabilization and rupture**.
- Plaque rupture then exposes the highly thrombogenic lipid core, initiating thrombus formation and acute coronary events like the **red thrombus** seen in the **left anterior descending artery (LAD)**.
*Influx of lipids into the endothelium*
- This process is characteristic of the **initial stages of atherosclerosis**, leading to **fatty streak formation**, not the acute plaque rupture and thrombosis described.
- While essential for plaque development, lipid influx alone does not directly explain aggressive plaque rupture and acute thrombus formation.
*Release of platelet-derived growth factor*
- **Platelet-derived growth factor (PDGF)** is primarily involved in **smooth muscle cell proliferation** and migration, contributing to plaque growth and thickening.
- Its role is more chronic and proliferative, not immediate plaque destabilization and rupture leading to acute thrombosis.
*Type III collagen deposition*
- **Type III collagen** is characteristic of early, developing atherosclerotic plaques and granulation tissue, contributing to plaque stability.
- Plaque vulnerability associated with rupture involves a **thin fibrous cap** with reduced **collagen content**, often due to increased collagen degradation.
*Proliferation of smooth muscle cells*
- **Smooth muscle cell proliferation** occurs during chronic atherosclerosis, contributing to the **fibrous cap formation** and overall plaque stability.
- In the context of acute plaque rupture, it is the *erosion* of the fibrous cap, often due to degradation, rather than proliferation, that is the immediate cause.
More Hemodynamic disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.