Forensic pathology principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Forensic pathology principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Forensic pathology principles US Medical PG Question 1: A 3-year-old girl is brought to the emergency department by her parents with sudden onset shortness of breath. They tell the emergency physician that their daughter was lying on the bed watching television when she suddenly began gasping for air. They observed a bowl of peanuts lying next to her when they grabbed her up and brought her to the emergency department. Her respirations are 25/min, the pulse is 100/min and the blood pressure is 90/65 mm Hg. The physical findings as of now are apparently normal. She is started on oxygen and is sent in for a chest X-ray. Based on her history and physical exam findings, the cause of her current symptoms would be seen on the X-ray at which of the following sites?
- A. The superior segment of the right lower lobe
- B. The posterior segment of the right lower lobe (Correct Answer)
- C. The lingula of the left upper lobe
- D. The apical segment of the right upper lobe
- E. The apical segment of the left upper lobe
Forensic pathology principles Explanation: ***The posterior segment of the right lower lobe***
- This is the **most common site for foreign body aspiration in a supine or lying down position** due to gravity and anatomical orientation.
- The history explicitly states the child was **"lying on the bed watching television"** when aspiration occurred, making the **posterior segment of the right lower lobe** the most gravity-dependent and therefore most likely location.
- The **right main bronchus** is wider, shorter, and more vertical than the left, making the right lung the predominant site for aspiration, and in supine position, the posterior segment is most dependent [1, 2].
*The superior segment of the right lower lobe*
- The **superior segment of the right lower lobe** is the most common site for aspiration in **upright, standing, or semi-upright positions**, not in a supine position.
- Since the child was lying down (supine), gravity would direct the aspirated peanut to the **posterior segment** rather than the superior segment.
- This would be correct if the child had aspirated while sitting upright.
*The lingula of the left upper lobe*
- The **lingula** is an uncommon site for aspiration because the **left main bronchus** has a sharper angle and smaller diameter compared to the right bronchus [2].
- The anatomical differences make aspiration into the right lung significantly more common than the left lung [2].
- The lingula is not a gravity-dependent area in the supine position.
*The apical segment of the right upper lobe*
- The **apical segment of the right upper lobe** is associated with aspiration when the patient is in **Trendelenburg position** (head lower than feet) or in extreme head-down positions.
- The described scenario of lying flat on the bed does not favor aspiration into apical segments, which are non-gravity-dependent in supine position.
- This location would be contra-gravity in the supine position.
*The apical segment of the left upper lobe*
- Aspiration into the **left upper lobe** is less frequent than the right lung due to the sharper angle of the left main bronchus [2].
- The **apical segment** would require head-down positioning (Trendelenburg) that is not described in this clinical scenario.
- This is the least likely location given both the supine position and left-sided anatomy.
Forensic pathology principles US Medical PG Question 2: A 43-year-old male visits the emergency room around 4 weeks after getting bitten by a bat during a cave diving trip. After cleansing the wound with water, the patient reports that he felt well enough not to seek medical attention immediately following his trip. He does endorse feeling feverish in the past week but a new onset of photophobia and irritability led him to seek help today. What would the post-mortem pathology report show if the patient succumbs to this infection?
- A. Howell-Jolly bodies
- B. Heinz bodies
- C. Psammoma bodies
- D. Pick bodies
- E. Negri bodies (Correct Answer)
Forensic pathology principles Explanation: ***Negri bodies***
- This patient's symptoms (fever, photophobia, irritability) and history of a bat bite point to rabies. **Negri bodies** are eosinophilic inclusions found in the cytoplasm of hippocampal and Purkinje cells in cases of rabies.
- They are **pathognomonic** for rabies infection and represent viral nucleocapsid proteins.
*Howell-Jolly bodies*
- These are **nuclear remnants** found in red blood cells that indicate impaired splenic function or asplenia.
- They are not associated with viral infections like rabies and are observed in conditions like sickle cell disease or after splenectomy.
*Heinz bodies*
- **Heinz bodies** are inclusions within red blood cells composed of denatured hemoglobin.
- They are typically seen in conditions involving **oxidative stress** to red blood cells, such as G6PD deficiency or alpha-thalassemia, not rabies.
*Psammoma bodies*
- These are **calcified, laminated, concentric spherules** found in some tumors (e.g., papillary thyroid carcinoma, meningioma, serous ovarian cystadenocarcinoma).
- They are a marker of specific neoplastic conditions and have no relevance to viral infections.
*Pick bodies*
- **Pick bodies** are aggregates of tau protein found in neurons, characteristic of **Pick's disease**, a type of frontotemporal dementia.
- They are neurodegenerative markers and are unrelated to infectious diseases.
Forensic pathology principles US Medical PG Question 3: A 44-year-old woman presents to the emergency department with a headache, vertigo, confusion, and dyspnea. A relevant history cannot be obtained from the patient because she seems confused and gives incoherent responses to questions. Her husband says that she was cleaning the kitchen this morning until the curtains caught on fire earlier this morning from the stove’s flame. Her vitals include: pulse 100/min, respirations 20/min, blood pressure 130/80 mm Hg, oxygen saturation 97% on room air. On physical examination, the patient is oriented x 0. The skin has a bright cherry-red color. Laboratory testing shows:
pH 7.35
PaO2 90 mm Hg
pCO2 40 mm Hg
HCO3- 26 mEq/L
SpO2 97%
Blood lactate 11 mmol/L
Which of the following is the most likely diagnosis in this patient?
- A. Cyanide poisoning
- B. Polycythemia
- C. Carbon monoxide poisoning (Correct Answer)
- D. High altitude
- E. Anemia
Forensic pathology principles Explanation: ***Carbon monoxide poisoning***
- The patient's presentation with **headache, vertigo, confusion, dyspnea**, and particularly the **cherry-red skin** in the context of **exposure to a kitchen fire**, is highly suggestive of **carbon monoxide (CO) poisoning**. The cherry-red skin coloration is caused by **carboxyhemoglobin** and is a classic (though not always present) sign of CO toxicity.
- The **normal PaO2 (90 mm Hg)** indicates adequate oxygen dissolved in plasma, but pulse oximetry shows **falsely normal SpO2 (97%)** because standard pulse oximeters cannot differentiate between **oxyhemoglobin and carboxyhemoglobin**. This creates a false sense of adequate oxygenation.
- The **elevated lactate (11 mmol/L)** results from **tissue hypoxia** as CO binds hemoglobin with 200-250 times greater affinity than oxygen, preventing oxygen delivery to tissues and causing **cellular hypoxia**.
- **House fires** are the most common source of CO exposure, making this the most likely diagnosis given the clinical context.
*Cyanide poisoning*
- **Cyanide poisoning** can occur from smoke inhalation when synthetic materials burn and can cause confusion, dyspnea, and lactic acidosis due to **inhibition of cytochrome oxidase**, preventing cellular oxygen utilization.
- However, cyanide typically causes **pink or flushed skin** rather than the classic **cherry-red color** seen with carboxyhemoglobin in CO poisoning.
- While both can present with elevated lactate, the **cherry-red skin** is pathognomonic for CO, not cyanide. Additionally, cyanide poisoning would typically show **very high lactate levels** (often >15-20 mmol/L) due to complete blockade of oxidative phosphorylation.
*Polycythemia*
- **Polycythemia** involves an abnormally high concentration of hemoglobin, which can cause symptoms like headache and vertigo but is a **chronic condition**, not an acute presentation following fire exposure.
- The **cherry-red skin** and acute confusion in the context of **smoke exposure** are not features of polycythemia.
*High altitude*
- **High altitude sickness** presents with headache, vertigo, and dyspnea due to **hypobaric hypoxia** causing a **decreased PaO2**, which is not seen in this patient (PaO2 is 90 mm Hg, which is normal).
- The **cherry-red skin** and acute onset after a kitchen fire are completely inconsistent with high altitude sickness.
*Anemia*
- **Anemia** is a deficiency of red blood cells or hemoglobin leading to symptoms like fatigue, dyspnea, and **pallor** (not cherry-red skin).
- The laboratory findings with **normal PaO2 and SpO2** and the acute presentation following fire exposure rule out anemia as the cause.
Forensic pathology principles US Medical PG Question 4: A 78-year-old man with a history of myocardial infarction status post coronary artery bypass grafting and a 60-pack-year history of smoking is found deceased in his apartment after not returning calls to his family for the last 2 days. The man was last known to be alive 3 days ago, when his neighbor saw him getting his mail. The family requests an autopsy. On autopsy, the man is found to have a 100% blockage of his left anterior descending artery of his heart and likely passed from sudden cardiac death 2 days prior. Which of the following findings is expected to be found on histologic examination of his damaged myocardium?
- A. Fat saponification
- B. Cellular debris and lymphocytes
- C. Cystic cavitation
- D. Cellular debris and macrophages
- E. Uniform binding of acidophilic dyes (Correct Answer)
Forensic pathology principles Explanation: ***Uniform binding of acidophilic dyes***
- This finding, often described as **coagulative necrosis**, is characteristic of myocardial infarction 1-3 days after onset, as enzymes denature and bind to eosin more uniformly.
- The patient was found deceased 2 days after his suspected death, placing the myocardial changes within this timeframe.
*Fat saponification*
- **Fat saponification** is a type of fat necrosis, typically seen in the pancreas or breast, resulting from the enzymatic destruction of fat cells.
- It does not occur in the myocardium following an ischemic event.
*Cellular debris and lymphocytes*
- **Lymphocytes** are generally not the predominant inflammatory cells in the initial stages of a myocardial infarction.
- While cellular debris would be present, the primary inflammatory infiltrate in the first 3 days after an MI is typically **neutrophils**, not lymphocytes.
*Cystic cavitation*
- **Cystic cavitation** is a characteristic feature of liquefactive necrosis, which occurs in the brain following an ischemic stroke, but not in the heart.
- The heart undergoes **coagulative necrosis** after an MI.
*Cellular debris and macrophages*
- **Macrophages** become prominent later in the healing process of a myocardial infarction, typically starting around **3-7 days** after the event.
- At the 2-day mark, the dominant cells would still be neutrophils and necrotic myocytes.
Forensic pathology principles US Medical PG Question 5: During the examination of a gunshot wound, the forensic pathologist notes an entrance wound with abrasion collar and soot deposition. The wound shows a stellate-shaped pattern with irregular margins. This pattern most likely indicates which of the following?
- A. Ricochet injury
- B. Long-range firing
- C. Intermediate-range firing
- D. Contact wound (Correct Answer)
Forensic pathology principles Explanation: ***Contact wound***
- A **stellate-shaped pattern with irregular margins** is the pathognomonic feature of a **contact wound** where the muzzle is pressed directly against the skin.
- When the weapon is fired in contact with skin, **hot gases expand beneath the skin surface**, causing it to burst outward in a characteristic **stellate or cruciate laceration pattern**.
- The presence of **soot deposition** and **abrasion collar** further supports a contact or near-contact gunshot wound.
- In contact wounds over bone (e.g., skull), the stellate pattern is most pronounced due to resistance from underlying bone.
*Intermediate-range firing*
- **Intermediate-range firing** (typically 6 inches to 3 feet) shows **powder tattooing** (stippling) and may show soot deposition around a round or oval entrance wound.
- However, intermediate-range wounds do **NOT produce stellate-shaped patterns** because the gases disperse before impact and don't expand beneath the skin.
- The entrance wound remains relatively round with surrounding powder stippling.
*Ricochet injury*
- A **ricochet injury** has an irregular, asymmetrical entrance wound due to bullet deformation and altered trajectory after striking another surface.
- Would not show the characteristic stellate pattern or typical soot distribution of direct firing.
*Long-range firing*
- **Long-range firing** produces only a clean entrance wound with an **abrasion collar**, without soot or powder tattooing.
- The distance is too great for combustion byproducts to reach the target.
- The wound is typically round or oval without stellate laceration.
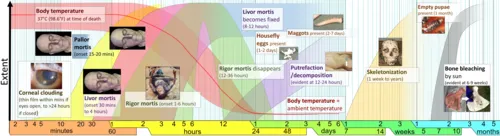
Forensic pathology principles US Medical PG Question 6: A 45-year-old man is found deceased in his bedroom. Time of death needs to be established for legal purposes. The body temperature is 32°C (89.6°F), and the ambient temperature is 20°C (68°F). Rigor mortis is complete in all muscle groups. Assuming normal conditions, which of the following best estimates the postmortem interval?
- A. 24-26 hours
- B. 6-8 hours
- C. 12-14 hours (Correct Answer)
- D. 2-4 hours
Forensic pathology principles Explanation: ***12-14 hours***
- **Complete rigor mortis** in all muscle groups typically occurs between **12-18 hours** postmortem.
- The body temperature of 32°C (89.6°F) with an ambient temperature of 20°C (68°F) indicates significant cooling, suggesting a **postmortem interval of several hours**, consistent with the stages of rigor mortis.
- This timeframe represents the peak of complete rigor mortis across all muscle groups.
*24-26 hours*
- By **24-36 hours**, rigor mortis would typically be **passing or completely absent** due to autolysis and decomposition.
- The body temperature would also be closer to the ambient temperature at this stage, unless other factors were involved.
*6-8 hours*
- At 6-8 hours, rigor mortis would typically be **developing or fully established in smaller muscles** (like the face and neck), but likely **not complete in all muscle groups**.
- Body temperature would be higher than 32°C, as a significant drop to 32°C would take longer.
*2-4 hours*
- At this early stage, rigor mortis would likely be **absent** or only just beginning to develop in the smallest muscles.
- The body temperature would also be much closer to normal body temperature (37°C or 98.6°F), with only a slight drop.
Forensic pathology principles US Medical PG Question 7: A 21-year-old medical student is studying different types of necrosis and tissue injuries. In the pathology laboratory, he observes different dead tissues under the microscope and notices the changes that are occurring as a function of time. After serial observations, he deduced that coagulation necrosis is...?
- A. The result of denaturation of glucose
- B. Characterized by the preservation of cellular shape (Correct Answer)
- C. Characteristic of brain ischemia
- D. Commonly associated with acute pancreatic necrosis
- E. The result of hydrolytic enzymes
Forensic pathology principles Explanation: ***Characterized by the preservation of cellular shape***
* **Coagulation necrosis** results from **protein denaturation**, which prevents the breakdown of the cell's structural proteins and enzymes.
* This preserves the **outline of the cell** and tissue architecture for a period of time, even after cell death, giving it a ghost-like appearance.
*The result of denaturation of glucose*
* **Glucose** is a simple sugar and does not undergo denaturation in the context of necrosis; rather, **proteins** are denatured.
* Denaturation refers to the disruption of the three-dimensional structure of proteins, not carbohydrates.
*Characteristic of brain ischemia*
* **Brain ischemia** typically results in **liquefactive necrosis**, not coagulation necrosis.
* This is due to the brain's high lipid content and the abundance of hydrolytic enzymes that rapidly digest the tissue.
*Commonly associated with acute pancreatic necrosis*
* **Acute pancreatitis** is primarily associated with **fat necrosis** (due to lipase activity) and **hemorrhagic necrosis**, not classic coagulation necrosis.
* The release of activated pancreatic enzymes leads to the digestion of local adipose tissue and blood vessels.
*The result of hydrolytic enzymes*
* While hydrolytic enzymes are involved in various forms of necrosis, **coagulation necrosis** is characterized by the **denaturation of structural proteins and enzymes**, which initially inhibits their proteolytic activity.
* **Liquefactive necrosis**, conversely, is largely driven by the release of powerful hydrolytic enzymes.
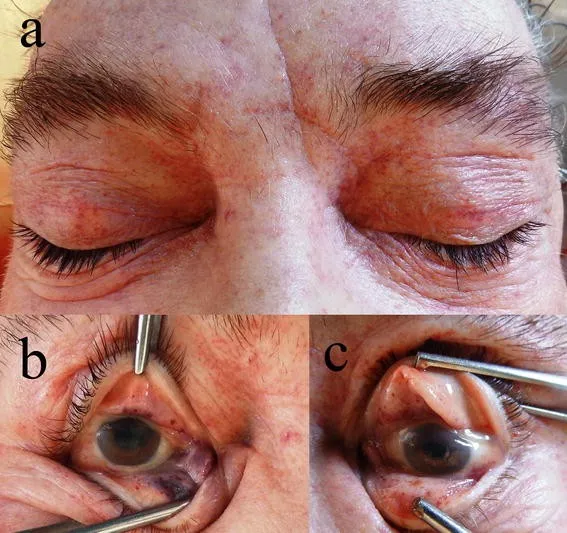
Forensic pathology principles US Medical PG Question 8: A 4-month-old boy is brought to the physician for a well-child examination. He was born at 36 weeks' gestation. The mother has had no prenatal care. His 6-year-old sister has a history of osteosarcoma. He is exclusively breast fed. He is at the 60th percentile for height and weight. Vital signs are within normal limits. Examination shows inward deviation of the right eye. Indirect ophthalmoscopy shows a white reflex in the right eye and a red reflex in the left eye. Which of the following is the most appropriate next step in management?
- A. Screen for galactosemia
- B. Fundus examination (Correct Answer)
- C. Visual training exercises
- D. CT scan of the eye
- E. Serum rubella titers
Forensic pathology principles Explanation: **Fundus examination**
- The presence of a **white reflex (leukocoria)** in the right eye is a critical finding that suggests serious ocular pathology, such as **retinoblastoma**, congenital cataract, or retinopathy of prematurity.
- A prompt **fundus examination** by an ophthalmologist is essential to identify the underlying cause and initiate appropriate treatment to preserve vision and potentially life, especially given the family history of osteosarcoma (which can be associated with retinoblastoma).
*Screen for galactosemia*
- Galactosemia can cause **cataracts**, leading to leukocoria; however, it's typically associated with other symptoms like **vomiting**, poor feeding, and **hepatomegaly**, which are not reported here.
- While screening might be considered, the immediate and most critical step is to investigate the white reflex directly.
*Visual training exercises*
- **Visual training exercises** are typically used for amblyopia or strabismus, a deviation of the eye (which is present here).
- However, they would only be considered *after* ruling out serious underlying causes of leukocoria, as the white reflex indicates a more urgent issue.
*CT scan of the eye*
- A **CT scan of the eye** could be used to evaluate for **intraocular tumors** like retinoblastoma or calcifications.
- However, a **fundus examination** is typically the initial diagnostic step to visualize the retina and determine the nature of the white reflex, guiding subsequent imaging if needed.
*Serum rubella titers*
- **Congenital rubella syndrome** can cause cataracts (leukocoria) and other ocular abnormalities.
- However, there are no other signs suggestive of congenital rubella infection (e.g., microcephaly, congenital heart defects, hearing loss), and testing for it is not the most immediate or highest priority given the acute finding of leukocoria.
Forensic pathology principles US Medical PG Question 9: A 60-year-old African American woman presents to her ophthalmologist with blurry vision. She reports a 2-month history of decreased vision primarily affecting her right eye. Her past medical history is notable for type 1 diabetes and hypertension. She takes insulin and enalapril. She has a 40-pack-year smoking history and drinks a glass of wine at dinner each night. Her family history is notable for glaucoma in her mother and severe diabetes complicated by nephropathy and retinopathy in her father. Her temperature is 99°F (37.2°C), blood pressure is 134/82 mmHg, pulse is 88/min, and respirations are 18/min. On exam, she is well-appearing and in no acute distress. The physician asks the patient to look forward and shines a penlight first in one eye, then the other, alternating quickly to observe the pupillary response to the light. When the light is shined in the right eye, both pupils partially constrict. When the light is shined in the left eye, both pupils constrict further. When the light is moved back to the right eye, both eyes dilate slightly to a partially constricted state. Where is the most likely site of this patient’s lesion?
- A. Lateral geniculate nucleus
- B. Lens
- C. Oculomotor nerve
- D. Ciliary ganglion
- E. Optic nerve (Correct Answer)
Forensic pathology principles Explanation: ***Optic nerve***
- The alternating pupillary response, where shining light in the affected right eye causes less constriction than in the left eye, even though both pupils constrict, points to a **Relative Afferent Pupillary Defect (RAPD)**, also known as a **Marcus Gunn pupil**.
- An RAPD indicates a lesion in the **afferent visual pathway** anterior to the optic chiasm, most commonly the optic nerve, as it reduces the input signal from the affected eye to the brainstem.
*Lateral geniculate nucleus*
- A lesion in the **lateral geniculate nucleus (LGN)** would cause a visual field defect, but typically would not present with an RAPD because the pupillary light reflex pathway largely bypasses the LGN.
- The afferent pupillary fibers synapse in the **pretectal nucleus** before reaching the Edinger-Westphal nucleus, not the LGN.
*Lens*
- Problems with the **lens**, such as cataracts, cause blurry vision due to light scattering but do not affect the afferent pupillary pathway or cause an RAPD.
- The lens focuses light onto the retina; it is not involved in transmitting signals for the pupillary light reflex.
*Oculomotor nerve*
- A lesion in the **oculomotor nerve (CN III)** would affect the efferent pupillary pathway, leading to a **dilated pupil** in the affected eye, often with impaired extraocular movements, which is not described.
- The oculomotor nerve carries parasympathetic fibers responsible for pupillary constriction.
*Ciliary ganglion*
- A lesion in the **ciliary ganglion** would also affect the efferent pupillary pathway, causing a **dilated pupil** and sluggish or absent light reflex on the affected side (tonic pupil).
- This is a post-ganglionic parasympathetic lesion, which would present differently from the observed RAPD.
Forensic pathology principles US Medical PG Question 10: A 16-year-old boy is brought to the emergency department 20 minutes after collapsing while playing basketball. There is no personal or family history of serious illness. On arrival, there is no palpable pulse and no respiratory effort is seen. He is declared dead. The family agrees to an autopsy. Which of the following is most likely to be found in this patient?
- A. Defect in the atrial septum
- B. Interventricular septal hypertrophy (Correct Answer)
- C. Pericardial fluid collection
- D. Postductal narrowing of the aorta
- E. Atheromatous plaque rupture
Forensic pathology principles Explanation: ***Interventricular septal hypertrophy***
- This presentation is highly suggestive of **hypertrophic cardiomyopathy (HCM)**, which is characterized by **left ventricular hypertrophy**, especially of the interventricular septum, leading to outflow obstruction and sudden cardiac arrest, particularly in young athletes.
- **Sudden collapse during strenuous exercise** in a young, otherwise healthy individual with no prior history of illness is a classic presentation of HCM.
*Defect in the atrial septum*
- An **atrial septal defect (ASD)** typically presents with a **murmur** and may lead to heart failure or pulmonary hypertension later in life, but it is an unlikely cause of sudden death in an adolescent during exercise.
- While it can cause cardiac symptoms, sudden collapse without prior symptoms is uncommon, and the primary pathological finding would be a hole, not hypertrophy.
*Pericardial fluid collection*
- A significant pericardial fluid collection that causes sudden collapse would indicate **pericardial tamponade**, which is usually associated with clear signs of circulatory collapse (e.g., **Beck's triad** - muffled heart sounds, jugular venous distension, hypotension) and is often due to trauma, infection, or malignancy, which are not suggested here.
- The sudden, unheralded nature of collapse during exercise points away from conditions that typically have more gradual onset or preceding symptoms.
*Postductal narrowing of the aorta*
- **Coarctation of the aorta** can cause hypertension and may lead to heart failure or aortic rupture, but it typically presents with **blood pressure discrepancies** between the upper and lower extremities and a characteristic murmur, not sudden cardiac death during exercise without prior symptoms.
- While it can be severe, sudden death usually results from complications like aortic dissection or rupture after a period of untreated hypertension, not acute collapse in a seemingly healthy individual.
*Atheromatous plaque rupture*
- **Atherosclerosis** and plaque rupture are the underlying cause of most **myocardial infarctions** in adults, but they are extremely rare in a 16-year-old without significant risk factors or a history of lipid disorders.
- The patient's age and lack of predisposing factors make this an improbable finding for sudden cardiac death.
More Forensic pathology principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.