Amyloidosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Amyloidosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Amyloidosis US Medical PG Question 1: A 72-year-old African American man presents with progressive fatigue, difficulty breathing on exertion, and lower extremity swelling for 3 months. The patient was seen at the emergency department 2 times before. The first time was because of back pain, and the second was because of fever and cough. He took medications at the emergency room, but he refused to do further tests recommended to him. He does not smoke or drink alcohol. His family history is irrelevant. His vital signs include a blood pressure of 110/80 mm Hg, temperature of 37.2°C (98.9°F), and regular radial pulse of 90/min. On physical examination, the patient looks pale, and his tongue is enlarged. Jugular veins become distended on inspiration. Pitting ankle edema is present on both sides. Bilateral basal crackles are audible on the chest auscultation. Hepatomegaly is present on abdominal palpation. Chest X-ray shows osteolytic lesions of the ribs. ECG shows low voltage waves and echocardiogram shows a speckled appearance of the myocardium with diastolic dysfunction and normal appearance of the pericardium. Which of the following best describes the mechanism of this patient’s illness?
- A. Thickening of the parietal pericardium with dystrophic calcification
- B. Calcification of the aortic valve orifice with obstruction of the left ventricular outflow tract
- C. Concentric hypertrophy of the myocytes with thickening of the interventricular septum
- D. Diastolic cardiac dysfunction with reciprocal variation in ventricular filling with respiration
- E. Deposition of an extracellular fibrillar protein that stains positive for Congo red in the myocardium (Correct Answer)
Amyloidosis Explanation: - ***Deposition of an extracellular fibrillar protein that stains positive for Congo red in the myocardium***
- The patient's presentation with **progressive fatigue, dyspnea, edema, enlarged tongue, jugular venous distention with inspiration** (Kussmaul's sign), **basal crackles, hepatomegaly, osteolytic lesions, low voltage on ECG, and a speckled appearance of the myocardium on echocardiogram with diastolic dysfunction** is highly suggestive of **amyloidosis**.
- **Amyloidosis** involves the deposition of misfolded, insoluble **fibrillar proteins** in various tissues, including the heart, leading to restrictive cardiomyopathy. These amyloid deposits typically stain **positive with Congo red** and demonstrate **apple-green birefringence** under polarized light.
- *Thickening of the parietal pericardium with dystrophic calcification*
- This description is characteristic of **constrictive pericarditis**, which can cause symptoms similar to restrictive cardiomyopathy (e.g., Kussmaul's sign, edema).
- However, the echocardiogram in this patient shows a **speckled appearance of the myocardium** and a **normal pericardium**, ruling out constrictive pericarditis.
- *Calcification of the aortic valve orifice with obstruction of the left ventricular outflow tract*
- This describes **aortic stenosis**, which would lead to signs of left ventricular outflow obstruction, such as a systolic murmur and possibly left ventricular hypertrophy.
- While it can cause dyspnea and fatigue, it does not typically explain the **speckled myocardium**, **enlarged tongue**, or **osteolytic lesions** seen in this patient.
- *Concentric hypertrophy of the myocytes with thickening of the interventricular septum*
- This is characteristic of **hypertensive heart disease** or **hypertrophic cardiomyopathy**.
- While these conditions can cause diastolic dysfunction, they typically do not present with **osteolytic lesions**, **enlarged tongue**, or the **speckled appearance of the myocardium** on echocardiography that is seen in amyloidosis.
- *Diastolic cardiac dysfunction with reciprocal variation in ventricular filling with respiration*
- While **diastolic cardiac dysfunction** is present, this option is too general and describes a physiological consequence rather than the underlying mechanism for the constellation of symptoms.
- **Reciprocal variation in ventricular filling with respiration** can be seen in both restrictive cardiomyopathy and constrictive pericarditis but does not explain the specific findings of **osteolytic lesions** or **enlarged tongue**, which point towards a systemic infiltrative disease like amyloidosis.
Amyloidosis US Medical PG Question 2: A 65-year-old man comes to the physician because of increasing swelling of the legs and face over the past 2 months. He has a history of diastolic heart dysfunction. The liver and spleen are palpable 4 cm below the costal margin. On physical examination, both lower limbs show significant pitting edema extending above the knees and to the pelvic area. Laboratory studies show:
Serum
Cholesterol 350 mg/dL (<200 mg/dL)
Triglycerides 290 mg/dL (35–160 mg/dL)
Calcium 8 mg/dL
Albumin 2.8 g/dL
Urea nitrogen 54 mg/dL
Creatinine 2.5 mg/dL
Urine
Blood 3+
Protein 4+
RBC 15–17/hpf
WBC 1–2/hpf
RBC casts Many
Echocardiography shows concentrically thickened ventricles with diastolic dysfunction. Skeletal survey shows no osteolytic lesions. Which of the following best explains these findings?
- A. Smoldering multiple myeloma
- B. Monoclonal gammopathy of undetermined significance
- C. Waldenstrom’s macroglobulinemia
- D. AL amyloidosis (Correct Answer)
- E. Symptomatic multiple myeloma
Amyloidosis Explanation: ***AL amyloidosis***
- The combination of **nephrotic syndrome** (edema, proteinuria, hypoalbuminemia, hyperlipidemia) with **renal failure** (elevated BUN and creatinine, RBC casts) and **restrictive cardiomyopathy** (diastolic dysfunction, concentrically thickened ventricles) is highly suggestive of **AL (light chain) amyloidosis**.
- **Hepatomegaly** (palpable liver) further supports the diagnosis of systemic amyloidosis due to amyloid deposition in the liver.
*Smoldering multiple myeloma*
- Characterized by high levels of **monoclonal protein** and **plasma cells in the bone marrow** but **without CRAB features** (HyperCalcemia, Renal failure, Anemia, Bone lesions).
- This patient presents with **renal failure** and **cardiac involvement**, which are symptomatic and thus inconsistent with smoldering multiple myeloma.
*Monoclonal gammopathy of undetermined significance*
- Defined by the presence of a **monoclonal protein** in the serum or urine but **without evidence of multiple myeloma, amyloidosis, or related disorders**.
- This patient exhibits significant **organ damage** indicative of systemic disease, ruling out MGUS.
*Waldenstrom's macroglobulinemia*
- A low-grade lymphoma characterized by **IgM monoclonal gammopathy** and **lymphoplasmacytic infiltration of the bone marrow**.
- It often causes **hyperviscosity syndrome**, lymphadenopathy, and peripheral neuropathy, which are not the primary features in this case.
*Symptomatic multiple myeloma*
- Requires evidence of **CRAB features** (HyperCalcemia, Renal failure, Anemia, Bone lesions) in addition to monoclonal protein and bone marrow plasma cells.
- While **renal failure** is present, the prominent **cardiac involvement** (restrictive cardiomyopathy) and the specific nature of the renal disease (nephrotic range proteinuria, RBC casts suggesting glomerular involvement) are more characteristic of AL amyloidosis rather than typical multiple myeloma kidney.
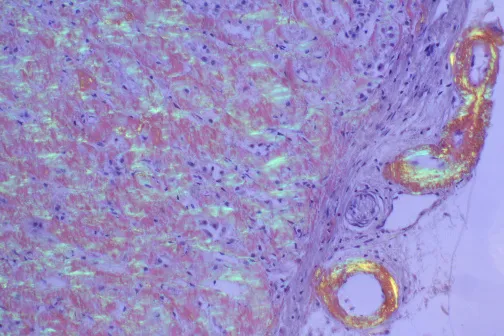
Amyloidosis US Medical PG Question 3: A 79-year-old homeless man is brought to the emergency department by ambulance 30 minutes after being found unresponsive by the police. On arrival, he is apneic and there are no palpable pulses. Despite appropriate life-saving measures, he dies. Examination of the heart during autopsy shows normal ventricles with a sigmoid-shaped interventricular septum. A photomicrograph of a section of the heart obtained at autopsy is shown. Which of the following is the most likely underlying cause for the structure indicated by the arrow?
- A. Accumulation of iron granules
- B. Clumping of defective mitochondria
- C. Deposition of wild-type transthyretin (Correct Answer)
- D. Aggregation of alpha-synuclein
- E. Oxidation of phospholipid molecules
Amyloidosis Explanation: ***Deposition of wild-type transthyretin***
- This photomicrograph likely shows amyloid deposition, and in an elderly patient with heart failure, **wild-type transthyretin (ATTR) amyloidosis** is the most common cause.
- The sigmoid-shaped interventricular septum also suggests age-related changes, often seen with ATTR amyloidosis.
*Accumulation of iron granules*
- **Hemochromatosis** involves iron deposition; however, it typically results in hemosiderin granules, which stain differently (e.g., Prussian blue), and the accompanying heart pathology would be **dilated cardiomyopathy**, not restrictive.
- While iron overload can affect the heart, its microscopic appearance is distinct from that of amyloid, and it is less likely to cause sudden death in this manner without other systemic signs.
*Clumping of defective mitochondria*
- **Mitochondrial myopathies** can cause cardiomyopathy, but the characteristic histological findings are often **ragged red fibers** on Gomori trichrome stain due to subsarcolemmal mitochondrial aggregates, not the diffuse extracellular deposits characteristic of amyloid.
- This is a rare cause of cardiomyopathy in the general elderly population and does not fit the typical macroscopic cardiac findings described.
*Aggregation of alpha-synuclein*
- **Alpha-synuclein aggregation** is characteristic of **Parkinson's disease** and other synucleinopathies, forming **Lewy bodies** primarily in neuronal tissue, not cardiac muscle.
- While autonomic dysfunction can occur in Parkinson's, and sometimes alpha-synuclein can be found in cardiac nerves, it does not cause widespread myocardial deposits leading to fatal restrictive cardiomyopathy.
*Oxidation of phospholipid molecules*
- **Oxidation of phospholipid molecules** is associated with cellular damage and inflammation, such as in **atherosclerosis** or **ischemic injury**.
- While oxidative stress plays a role in various cardiac pathologies, it does not lead to the formation of organized extracellular deposits in the myocardium that would resemble amyloid on histology.
Amyloidosis US Medical PG Question 4: A 63-year-old man presents to the emergency department with periorbital swelling. He states that he was gardening, came inside, looked in the mirror, and then noticed his eyelids were swollen. He denies pain, pruritus, or visual disturbances. He states that he was drinking “a lot of water" to prevent dehydration, because it was hot outside this morning. His medical history is significant for rheumatoid arthritis. He takes methotrexate and acetaminophen as needed. The patient’s temperature is 98°F (36.7°C), blood pressure is 168/108 mmHg, and pulse is 75/min. Physical examination is notable for periorbital edema, hepatomegaly, and bilateral 1+ pitting lower extremity edema. Labs and a urinalysis are obtained, as shown below:
Leukocyte count: 11,000/mm^3
Hemoglobin: 14 g/dL
Serum:
Na: 138 mEq/L
K+: 4.3 mEq/L
Cl-: 104 mEq/L
HCO3-: 25 mEq/L
Urea nitrogen: 26 mg/dL
Creatinine: 1.4 mg/dL
Glucose: 85 mg/dL
Aspartate aminotransferase (AST, GOT): 15 U/L
Alanine aminotransferase (ALT, GPT): 19 U/L
Albumin: 2.0 g/dL
Urine:
Protein: 150 mg/dL
Creatinine: 35 mg/dL
An abdominal ultrasound reveals an enlarged liver with heterogeneous echogenicity and enlarged kidneys with increased echogenicity in the renal parenchyma. A biopsy of the kidney is obtained. Which of the following biopsy findings is associated with the patient’s most likely diagnosis?
- A. Apple green birefringence with Congo red staining (Correct Answer)
- B. Subepithelial dense deposits
- C. Tubulointerstitial fibrosis
- D. Kimmelstiel-Wilson nodules
- E. Glomerular basement membrane splitting
Amyloidosis Explanation: ***Apple green birefringence with Congo red staining***
- The patient's presentation with **periorbital and pitting edema**, **hepatomegaly**, **renal dysfunction** (elevated creatinine, proteinuria), and **low serum albumin** in the setting of chronic **rheumatoid arthritis** suggests **AA amyloidosis**.
- **Congo red staining** followed by examination under polarized light revealing **apple green birefringence** is the classic diagnostic finding for amyloidosis on tissue biopsy.
*Subepithelial dense deposits*
- **Subepithelial dense deposits** are characteristic of **post-streptococcal glomerulonephritis** (PSGN) or other forms of immune-complex glomerulonephritis.
- PSGN typically presents with a recent history of infection and often hematuria, which is not described in this patient.
*Tubulointerstitial fibrosis*
- **Tubulointerstitial fibrosis** is a non-specific finding that can occur in various chronic kidney diseases, including those caused by long-term use of certain medications like **methotrexate** or chronic hypertension.
- While it might be present, it does not explain the widespread systemic findings or the specific cause of the present nephropathy in this case.
*Kimmelstiel-Wilson nodules*
- **Kimmelstiel-Wilson nodules** are pathognomonic for **diabetic nephropathy**, characterized by specific nodular glomerulosclerosis.
- The patient's glucose levels are normal, and there is no mention of diabetes mellitus in his history.
*Glomerular basement membrane splitting*
- **Glomerular basement membrane splitting** is a key feature of **Alport syndrome** and some forms of **membranoproliferative glomerulonephritis**.
- Alport syndrome is a genetic disorder typically presenting earlier in life with hematuria, hearing loss, and ocular abnormalities, none of which are detailed here.
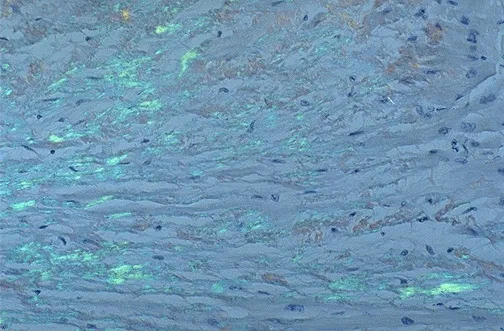
Amyloidosis US Medical PG Question 5: A 64-year-old man comes to the physician because of fatigue and decreased urinary frequency for 6 months. His pulse is 86/min and blood pressure is 150/90 mm Hg. Examination shows 1+ edema on bilateral ankles. His serum creatinine is 2 mg/dL and blood urea nitrogen is 28 mg/dL. Urinalysis shows proteinuria. A photomicrograph of a biopsy specimen from the patient's kidney is shown. Which of the following is the most likely explanation for the patient’s biopsy findings?
- A. Amyloidosis
- B. Recurrent kidney infections
- C. Chronic hyperglycemia (Correct Answer)
- D. Systemic lupus erythematosus
- E. HIV infection
Amyloidosis Explanation: ***Chronic hyperglycemia***
- Chronic hyperglycemia, as seen in **diabetes mellitus**, causes **diabetic nephropathy**, which is characterized by diffuse **glomerulosclerosis** and **nodular glomerulosclerosis** (Kimmelstiel-Wilson lesions) on biopsy.
- The patient's symptoms (fatigue, decreased urinary frequency, edema), elevated **creatinine and BUN**, and **proteinuria** are all consistent with chronic kidney disease secondary to diabetes.
*Amyloidosis*
- **Amyloidosis** would show characteristic **apple-green birefringence** under polarized light after Congo red staining, which is not described.
- While amyloidosis can cause proteinuria and kidney failure, the biopsy findings of diffuse and nodular glomerulosclerosis are classic for diabetic nephropathy.
*Recurrent kidney infections*
- Recurrent kidney infections (pyelonephritis) typically lead to **tubulointerstitial scarring** and inflammation, not predominantly glomerular changes.
- While they can cause chronic kidney disease, the biopsy would show signs of infection and interstitial damage rather than glomerulosclerosis.
*Systemic lupus erythematosus*
- Lupus nephritis manifests with various patterns of **glomerulonephritis**, including proliferative and membranous forms, often with **immune complex deposits**.
- The biopsy findings described (diffuse and nodular glomerulosclerosis) are not characteristic of lupus nephritis.
*HIV infection*
- HIV-associated nephropathy (HIVAN) typically presents as **focal segmental glomerulosclerosis (FSGS)**, often with collapsing glomerulopathy.
- While HIV infection can lead to kidney disease, the characteristic nodular and diffuse glomerulosclerosis seen in this patient points away from HIVAN.
Amyloidosis US Medical PG Question 6: A 55-year-old man comes to the physician because of a 3-day history of decreased urine output, progressively worsening bilateral pedal edema, and fatigue. He has a 4-month history of persistent lower back pain. He has hypercholesterolemia and stable angina pectoris. Current medications include atorvastatin, aspirin, and ibuprofen. His pulse is 80/min, respirations are 16/min, and blood pressure is 150/100 mm Hg. Examination shows periorbital and pedal edema and pallor. There is tenderness of the lumbar spinal vertebrae. Straight leg raise test is negative. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 8.9 g/dl
Serum
Urea nitrogen 20 mg/dl
Creatinine 2.4 mg/dl
Calcium 11.2 mg/dl
Alkaline phosphatase 140 U/L
X-ray of the spine shows diffuse osteopenia and multiple lytic lesions. Which of the following is most likely to confirm the diagnosis?
- A. Bone marrow biopsy (Correct Answer)
- B. Parathyroid hormone levels
- C. Congo red stain of renal tissue
- D. Peripheral blood smear
- E. Skeletal survey
Amyloidosis Explanation: ***Bone marrow biopsy***
- This patient presents with signs highly suggestive of **multiple myeloma**, including **anemia**, **renal insufficiency**, **hypercalcemia**, and **lytic bone lesions** and diffuse osteopenia.
- A **bone marrow biopsy** is the most definitive test to confirm multiple myeloma by identifying an increased percentage of **plasma cells** and their clonality.
*Parathyroid hormone levels*
- While **hypercalcemia** is present, increased parathyroid hormone (PTH) levels would indicate **primary hyperparathyroidism**, which typically causes diffuse osteopenia but not multiple lytic lesions in this pattern.
- In multiple myeloma, hypercalcemia results from **bone destruction** by plasma cells, leading to **suppressed PTH levels**.
*Congo red stain of renal tissue*
- A Congo red stain of renal tissue is used to diagnose **amyloidosis**, which can cause renal failure, proteinuria, and sometimes edema.
- Although amyloidosis can be a complication of multiple myeloma, it is not the primary diagnostic test for the underlying myeloma itself, and this patient's presentation with prominent lytic lesions points more directly to myeloma.
*Peripheral blood smear*
- A peripheral blood smear might show **rouleaux formation** (RBCs stacked like coins) and occasionally **plasma cells**, which are suggestive of multiple myeloma.
- However, these findings are not specific or reliably present in all cases, and a bone marrow biopsy is required for definitive diagnosis.
*Skeletal survey*
- A skeletal survey (X-ray series) is crucial for identifying and characterizing the **lytic bone lesions** and diffuse osteopenia, as seen in this patient.
- While it provides strong evidence of bone involvement, it is an imaging study that supports the diagnosis but does not definitively confirm the underlying hematological malignancy like a bone marrow biopsy does.
Amyloidosis US Medical PG Question 7: A 60-year-old African American woman presents to her family physician with shortness of breath on exertion. She also describes shortness of breath when she lies down to go to bed at night, as well as recent swelling in her ankles. Past medical history is significant for long-standing hypertension, for which she takes amlodipine and lisinopril. Her temperature is 36.8°C (98.2°F), the heart rate is 90/min, the respiratory rate is 15/min, and the blood pressure is 135/80 mm Hg. The physical exam is significant for JVD, lower extremity pitting edema, laterally displaced PMI, left ventricular heave, bilateral pulmonary crackles, and an S4 heart sound. Chest X-ray demonstrates pulmonary vascular congestion, Kerley B lines, and cardiomegaly. Echocardiogram demonstrates a preserved ejection fraction. Kidney biopsy would likely demonstrate which of the following?
- A. Thinning of the intima and media
- B. Onion-skinning
- C. Nodular sclerosis
- D. Intimal thickening and medial hypertrophy (Correct Answer)
- E. Fibrinoid necrosis
Amyloidosis Explanation: ***Intimal thickening and medial hypertrophy***
* The patient's presentation of **heart failure with preserved ejection fraction (HFpEF)**, long-standing **hypertension**, and findings like left ventricular heave and S4 heart sound strongly suggest **hypertensive cardiomyopathy**, which in turn causes **hypertensive nephrosclerosis**.
* **Hypertensive nephrosclerosis** is characterized by **intimal thickening** and **medial hypertrophy** of renal arterioles, leading to **ischemia** and atrophy of glomeruli and tubules.
*Thinning of the intima and media*
* This is not a characteristic pathological change seen in hypertensive nephrosclerosis.
* In hypertension, the vessel walls typically undergo thickening due to **hypertrophy** and **hyperplasia** of smooth muscle cells and increased extracellular matrix, not thinning.
*Onion-skinning*
* **"Onion-skinning"** is a hallmark feature of **malignant hypertension**, characterized by concentric laminar thickening of the arteriolar walls.
* The patient's blood pressure (135/80 mmHg) is not consistent with malignant hypertension, which would typically involve much higher blood pressure readings.
*Nodular sclerosis*
* **Nodular sclerosis** (also known as **Kimmelstiel-Wilson lesions**) is characteristic of **diabetic nephropathy**, not primarily hypertensive nephrosclerosis.
* While diabetes and hypertension often co-exist, the prompt in this case points more directly to long-standing hypertension as the primary cause of renal damage.
*Fibrinoid necrosis*
* **Fibrinoid necrosis** of arterioles is also associated with **malignant hypertension** and some forms of vasculitis.
* This patient's blood pressure is controlled (135/80 mmHg) and does not indicate the severe, rapid increase in blood pressure seen in malignant hypertension.
Amyloidosis US Medical PG Question 8: A 51-year-old African American man with a history of poorly controlled hypertension presents to the emergency room with blurry vision and dyspnea. He reports rapid-onset blurred vision and difficulty breathing 4 hours prior to presentation. He takes lisinopril, hydrochlorothiazide, and spironolactone but has a history of poor medication compliance. He has a 50 pack-year smoking history and drinks 4-6 shots of vodka per day. His temperature is 99.2°F (37.3°C), blood pressure is 195/115 mmHg, pulse is 85/min, and respirations are 20/min. On exam, he is ill-appearing and pale. He is intermittently responsive and oriented to person but not place or time. Fundoscopic examination reveals swelling of the optic disc with blurred margins. A biopsy of this patient’s kidney would most likely reveal which of the following?
- A. Concentrically thickened arteriolar tunica media with abundant nuclei (Correct Answer)
- B. Calcific deposits in the arterial media without luminal narrowing
- C. Fibrous atheromatous plaques in the arterial intima
- D. Anuclear arteriolar thickening
- E. Endothelial proliferation and luminal narrowing with a chronic inflammatory infiltrate
Amyloidosis Explanation: ***Concentrically thickened arteriolar tunica media with abundant nuclei***
- This describes **hyperplastic arteriolosclerosis**, a hallmark of **malignant hypertension**, characterized by severe, rapid-onset blood pressure elevation leading to acute organ damage.
- The patient's **blood pressure of 195/115 mmHg**, **blurry vision** (due to optic disc swelling), and **dyspnea** (suggesting pulmonary edema or cardiac involvement) are classic symptoms of malignant hypertension, which causes "onion-skinning" of arterioles.
*Calcific deposits in the arterial media without luminal narrowing*
- This describes **Mönckeberg arteriolosclerosis**, or medial calcific sclerosis, which involves calcification of the tunica media in muscular arteries.
- It typically occurs in older individuals and is usually **clinically silent** unless complicated by atherosclerosis, and does not cause malignant hypertension.
*Fibrous atheromatous plaques in the arteriolar intima*
- This describes **atherosclerosis**, which involves the formation of plaques in larger arteries, not typically in arterioles, and is a chronic process.
- While the patient has risk factors for atherosclerosis (smoking, hypertension), the acute severe presentation points to a microvascular pathology.
*Anuclear arteriolar thickening*
- This describes **hyaline arteriolosclerosis**, associated with benign (non-malignant) hypertension or diabetes, where plasma proteins leak into the vessel walls, causing uniform, acellular thickening.
- The patient's severe symptoms and optic disc swelling indicate a more aggressive and acute form of vascular damage, not benign hyaline changes.
*Endothelial proliferation and luminal narrowing with a chronic inflammatory infiltrate*
- This pattern is characteristic of **vasculitis** or conditions like **thrombotic microangiopathy**, which can cause luminal narrowing and kidney damage.
- While some features of vasculitis might overlap, the specific context of poorly controlled severe hypertension points more directly to malignant hypertension-induced changes.
Amyloidosis US Medical PG Question 9: A 41-year-old African American woman presents to her primary care physician with a 3-week history of lower extremity edema and shortness of breath. She says that she has also noticed that she gets fatigued more easily and has been gaining weight. Her past medical history is significant for sickle cell disease and HIV infection for which she is currently taking combination therapy. Physical exam is significant for periorbital and lower extremity edema. Laboratory testing is significant for hypoalbuminemia, and urinalysis demonstrates 4+ protein. Which of the following would most likely be seen on kidney biopsy in this patient?
- A. Birefringence under polarized light
- B. Segmental scarring (Correct Answer)
- C. Subepithelial deposits
- D. Expansion of the mesangium
- E. Normal glomeruli
Amyloidosis Explanation: ***Segmental scarring***
- The patient's history of **HIV infection**, symptoms of **nephrotic syndrome** (edema, weight gain, fatigue, hypoalbuminemia, 4+ proteinuria), and African American ethnicity are highly suggestive of **HIV-associated nephropathy (HIVAN)**.
- HIVAN is a form of **collapsing focal segmental glomerulosclerosis (FSGS)**, a condition characterized by **segmental scarring** and collapse of the glomerular tuft. In HIVAN, this scarring is severe and progressive.
*Birefringence under polarized light*
- This finding is characteristic of **amyloidosis**, where protein deposits (amyloid) accumulate in tissues and exhibit apple-green birefringence under Congo red stain and polarized light.
- While amyloidosis can cause nephrotic syndrome, it is not the most common kidney pathology in an HIV-positive patient with these specific features.
*Subepithelial deposits*
- **Subepithelial deposits** with a characteristic "spike and dome" appearance on electron microscopy are pathognomonic for **membranous glomerulonephritis**.
- This type of glomerulonephritis is not typically associated with HIV infection, nor does it typically present with the rapidly progressive decline seen in HIVAN.
*Expansion of the mesangium*
- **Mesangial expansion** is a common feature in several glomerular diseases, including **diabetic nephropathy** and early-stage IgA nephropathy.
- While it can be present in some forms of FSGS, it is not the primary or most characteristic finding for HIVAN, which is better described by collapsing glomeruli and segmental scarring.
*Normal glomeruli*
- Given the patient's profound **proteinuria (4+)**, hypoalbuminemia, and symptoms of **nephrotic syndrome**, it is highly unlikely that the glomeruli would appear normal on biopsy.
- Normal glomeruli would not explain the significant kidney dysfunction and proteinuria observed in this patient.
Amyloidosis US Medical PG Question 10: A 62-year-old man comes to the physician because of a swollen and painful right knee for the last 3 days. He has no history of joint disease. His vital signs are within normal limits. Examination shows erythema and swelling of the right knee, with limited range of motion due to pain. Arthrocentesis of the right knee joint yields 7 mL of cloudy fluid with a leukocyte count of 29,000/mm3 (97% segmented neutrophils). Compensated polarized light microscopy of the aspirate is shown. Which of the following is the most likely underlying mechanism of this patient's knee pain?
- A. Immune complex-mediated cartilage destruction
- B. Calcium pyrophosphate deposition (Correct Answer)
- C. Bacterial infection of the joint
- D. Mechanical stress and trauma
- E. Monosodium urate deposition
Amyloidosis Explanation: ***Calcium pyrophosphate deposition***
- The **cloudy fluid** with a leukocyte count of **29,000/mm³** predominantly composed of **segmented neutrophils** indicates acute inflammation, characteristic of **pseudogout** (calcium pyrophosphate dihydrate crystal deposition disease).
- **Compensated polarized light microscopy** would reveal **weakly positive birefringent rhomboid-shaped crystals**, confirming CPPD deposition.
- The **age** of the patient (62 years), **acute monoarticular involvement of the knee**, and sudden onset support a diagnosis of **pseudogout**.
*Immune complex-mediated cartilage destruction*
- This mechanism is characteristic of **rheumatoid arthritis** or **systemic lupus erythematosus**, which present with **chronic polyarticular involvement** and systemic features.
- The acute monoarticular presentation and synovial fluid findings are inconsistent with an immune complex-mediated process.
*Bacterial infection of the joint*
- Septic arthritis typically presents with **synovial fluid WBC counts >50,000/mm³** (often >100,000), though some overlap exists.
- The **absence of fever** and presence of **crystal findings on polarized microscopy** distinguish pseudogout from bacterial infection.
- Septic arthritis would not show crystals on microscopy and would require immediate Gram stain and culture.
*Mechanical stress and trauma*
- While mechanical injury can cause joint effusion, the **high neutrophil count** and **acute inflammatory findings** indicate a crystal-induced or infectious arthropathy rather than traumatic injury.
- There is no history of **trauma** reported, and traumatic effusions typically have lower WBC counts with predominantly red blood cells.
*Monosodium urate deposition*
- This indicates **gout**, which presents with **strongly negative birefringent needle-shaped crystals** on polarized microscopy (not the weakly positive birefringent rhomboid crystals of pseudogout).
- Gout more commonly affects the **first metatarsophalangeal joint** and typically occurs in younger patients with hyperuricemia risk factors.
- The patient's age and knee involvement are more consistent with **pseudogout**.
More Amyloidosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.