Thyroiditis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thyroiditis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thyroiditis US Medical PG Question 1: A 37-year-old man presents to his primary care physician because he has had constipation for the last several weeks. He has also been feeling lethargic and complains that this winter has been particularly cold. He also complains that he has been gaining weight despite no change in his normal activities. He reveals that two months prior to presentation he had what felt like the flu for which he took Tylenol and did not seek medical attention. Several days after this he developed anterior neck pain. Which of the following findings would most likely be seen on biopsy of this patient's abnormality?
- A. Focal hyperplasia
- B. Germinal follicles
- C. Scalloped clear areas
- D. Fibrous tissue
- E. Granulomatous inflammation (Correct Answer)
Thyroiditis Explanation: ***Granulomatous inflammation***
- The patient's presentation with **constipation**, **lethargy**, **cold intolerance**, and **weight gain** after a flu-like illness followed by **anterior neck pain** is highly suggestive of **subacute granulomatous thyroiditis (de Quervain thyroiditis)**.
- A biopsy of the thyroid in cases of de Quervain thyroiditis typically reveals **granulomatous inflammation** with scattered **giant cells** and lymphocytes, reflecting the destructive inflammatory process.
*Focal hyperplasia*
- **Focal hyperplasia** is characterized by an increase in the number of thyroid follicular cells and is seen in conditions like **Graves' disease** or **multinodular goiter**, particularly when the gland is overstimulated.
- This finding would not be expected in subacute granulomatous thyroiditis, where the primary pathology is destruction rather than proliferation.
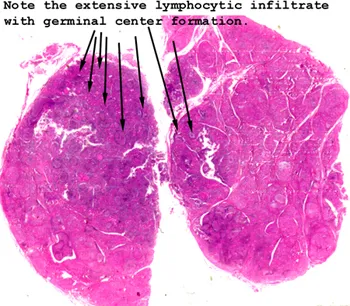
*Germinal follicles*
- **Germinal follicles** are characteristic of chronic lymphocytic thyroiditis (**Hashimoto's thyroiditis**), an autoimmune condition where the thyroid gland is infiltrated by lymphocytes, plasma cells, and macrophages.
- While Hashimoto's can cause hypothyroidism, the preceding flu-like illness and acute neck pain make de Quervain thyroiditis a more likely diagnosis.
*Scalloped clear areas*
- **Scalloped clear areas** at the colloid-epithelial interface, also known as **colloid resorption vacuoles**, are a histological feature of **hyperactive thyroid follicles**, typically seen in conditions causing hyperthyroidism like **Graves' disease**.
- The patient's symptoms of lethargy, cold intolerance, and weight gain indicate hypothyroidism, which can follow the initial hyperthyroid phase of de Quervain thyroiditis but are not indicative of active hyperfunction on biopsy at this stage.
*Fibrous tissue*
- An increased amount of **fibrous tissue** is characteristic of **Riedel's thyroiditis**, a rare condition characterized by dense fibrosis that replaces normal thyroid parenchyma and can extend into surrounding neck structures.
- This patient's presentation with a preceding febrile illness and neck pain is not typical for Riedel's thyroiditis, which usually presents as a hard, fixed mass without an antecedent viral infection.
Thyroiditis US Medical PG Question 2: A 43-year-old woman presents to the physician with the complaint of worsening fatigue over the past several months. She has found that she requires nearly double the amount of coffee consumption each day to stay awake at work and that despite maintaining a balanced, healthy diet, she has experienced significant weight gain. A blood test confirms the presence of anti-thyroid peroxidase antibodies. Which of the following additional findings would be most consistent with the underlying pathophysiology of her condition?
- A. Galactorrhea (Correct Answer)
- B. Constipation
- C. Brisk deep tendon reflexes
- D. Diarrhea
- E. Heat intolerance
Thyroiditis Explanation: ***Galactorrhea***
- This patient has **Hashimoto's thyroiditis**, an autoimmune hypothyroidism, given the fatigue, weight gain, and positive **anti-thyroid peroxidase antibodies**.
- **Hypothyroidism** can lead to **hyperprolactinemia** due to increased **TRH** (thyrotropin-releasing hormone), which stimulates both TSH and prolactin release from the anterior pituitary.
- Elevated prolactin can manifest as **galactorrhea**, representing a less commonly recognized endocrine consequence of primary hypothyroidism.
*Constipation*
- **Constipation** is a common symptom of **hypothyroidism** due to decreased gastrointestinal motility.
- While consistent with hypothyroidism, it is a direct consequence of reduced metabolic activity rather than a secondary endocrine effect.
- This is a well-known, expected finding rather than an additional pathophysiologic manifestation.
*Brisk deep tendon reflexes*
- **Hypothyroidism** typically causes **delayed relaxation of deep tendon reflexes** (hung-up reflexes), not brisk reflexes.
- **Brisk reflexes** are characteristic of **hyperthyroidism** due to increased neuromuscular excitability.
*Diarrhea*
- **Diarrhea** is typically associated with **hyperthyroidism** due to increased gastrointestinal motility from elevated metabolic rate.
- **Hypothyroidism** more commonly causes **constipation** due to decreased GI motility.
*Heat intolerance*
- **Heat intolerance** is a classic symptom of **hyperthyroidism** due to an elevated metabolic rate and increased thermogenesis.
- Patients with **hypothyroidism** usually experience **cold intolerance** due to decreased metabolic heat production.
Thyroiditis US Medical PG Question 3: A 25-year-old woman presents to her primary care clinic for a general checkup. She states she's been a bit more fatigued lately during finals season but is otherwise well. Her mother and sister have hypothyroidism. She denies weight gain, cold intolerance, constipation, heavy or irregular menses, or changes in the quality of her hair, skin, or nails. Physical exam is unremarkable. Laboratory studies are ordered as seen below.
Hemoglobin: 14 g/dL
Hematocrit: 40%
Leukocyte count: 5,500/mm^3 with normal differential
Platelet count: 188,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 102 mEq/L
K+: 4.4 mEq/L
HCO3-: 24 mEq/L
BUN: 20 mg/dL
Glucose: 99 mg/dL
Creatinine: 0.8 mg/dL
Ca2+: 10.2 mg/dL
Antithyroid peroxidase Ab: Positive
AST: 12 U/L
ALT: 10 U/L
Which of the following laboratory values is most likely in this patient?
- A. Elevated TSH and low T4
- B. Elevated TSH and elevated T4
- C. Normal TSH and low T4
- D. Normal TSH and normal T4 (Correct Answer)
- E. Low TSH and elevated T4
Thyroiditis Explanation: ***Normal TSH and normal T4***
- The patient has a **positive antithyroid peroxidase antibody**, indicating **Hashimoto's thyroiditis**, but she is currently **euthyroid** as evidenced by the absence of typical hypothyroid symptoms.
- In the initial stages of Hashimoto's thyroiditis, the thyroid gland often functions normally, leading to **normal TSH and T4 levels**, even with positive antibodies.
*Elevated TSH and low T4*
- This pattern indicates **overt hypothyroidism**, which would be expected to cause symptoms like **weight gain, cold intolerance, and constipation**, none of which are present in this patient.
- While Hashimoto's thyroiditis can progress to this stage, the patient's current presentation is subclinical, without biochemical evidence of hypofunction.
*Elevated TSH and elevated T4*
- This combination is rare and typically suggests **TSH-producing pituitary adenoma** or **thyroid hormone resistance**, neither of which is indicated by the patient's symptoms or family history.
- An elevated TSH would normally stimulate the thyroid to produce more T4, but if TSH is also elevated, it points to a problem at the pituitary level.
*Normal TSH and low T4*
- This pattern is highly suggestive of **central (secondary) hypothyroidism**, where the pituitary gland is not producing enough TSH to stimulate the thyroid.
- Given the patient's family history of hypothyroidism and positive antithyroid peroxidase antibodies (suggesting a primary thyroid issue), central hypothyroidism is less likely.
*Low TSH and elevated T4*
- This indicates **hyperthyroidism** (e.g., Graves' disease or toxic goiter), which would present with symptoms like **weight loss, heat intolerance, and tachycardia**, which are absent in this patient.
- While positive antithyroid antibodies can sometimes be seen in Graves' disease, the patient's lack of hyperthyroid symptoms rules out this state.
Thyroiditis US Medical PG Question 4: A 27-year-old G1P0 at 12 weeks estimated gestational age presents for prenatal care. The patient says she has occasional nausea and vomiting and a few episodes of palpitations and diarrhea this last week. Physical examination is unremarkable, except for a heart rate of 145/min. Basic thyroid function tests are shown in the table below. Which of the following additional laboratory tests would be most useful in assessing this patient's condition?
Thyroid-stimulating hormone (TSH)
0.28 mIU/L (0.3–4.5 mIU/L)
Total T4
12 µg/dL (5.4–11.5 µg/dL)
- A. Thyrotropin receptor antibodies (TRAb)
- B. Total triiodothyronine (T3) levels
- C. Thyroid peroxidase (TPO) antibodies
- D. Free thyroxine (T4) levels (Correct Answer)
- E. Thyroxine-binding globulin (TBG) levels
Thyroiditis Explanation: ***Free thyroxine (T4) levels***
- In pregnancy, **estrogen increases thyroxine-binding globulin (TBG)**, leading to higher **total T4** levels even if free T4 is normal.
- Measuring **free T4 provides a more accurate assessment** of the biologically active thyroid hormone, which is crucial for distinguishing between physiological changes of pregnancy and true hyperthyroidism.
*Thyrotropin receptor antibodies (TRAb)*
- **TRAb are specific for Graves' disease**, which is a cause of hyperthyroidism, but their presence is a confirmatory test after hyperthyroidism has been established.
- The initial step is to confirm the diagnosis of **hyperthyroidism** by evaluating free hormone levels, particularly in pregnancy where total hormone levels are less reliable.
*Total triiodothyronine (T3) levels*
- Similar to total T4, **total T3 levels are also affected by increased TBG in pregnancy**, making them less reliable for initial diagnosis of thyroid dysfunction.
- While T3 is an important thyroid hormone, **free T4 is generally the primary screening test** for hyperthyroidism.
*Thyroid peroxidase (TPO) antibodies*
- **TPO antibodies are indicative of autoimmune thyroiditis**, such as Hashimoto's thyroiditis, which typically causes hypothyroidism, not hyperthyroidism, as suggested by the patient's symptoms and elevated T4.
- Although TPO antibodies can sometimes be positive in Graves' disease, they are **not the primary diagnostic test for active hyperthyroidism**, especially regarding the magnitude of the elevation.
*Thyroxine-binding globulin (TBG) levels*
- While **TBG levels are elevated in pregnancy**, measuring TBG itself doesn't directly assess thyroid function.
- Understanding the physiology of **TBG elevation explains why total T4 is high**, but it doesn't help in determining whether the patient is truly hyperthyroid; for that, free T4 is needed.
Thyroiditis US Medical PG Question 5: An otherwise healthy 47-year-old woman comes to the physician for the evaluation of a 4-month history of worsening fatigue and constipation. She has also noticed that her cheeks appear fuller and her voice has become hoarse. Her temperature is 36.3°C (97.3°F) and pulse is 59/min. Examination of the neck shows a painless, mildly enlarged thyroid gland. Her skin is dry and cool and her nails appear brittle. Serum studies show antibodies against thyroid peroxidase. A biopsy of the thyroid gland is most likely to show which of the following?
- A. Tall follicular cells, scalloped colloid, and vascular congestion
- B. Lymphocytic infiltration, Hürthle cells, and germinal centers (Correct Answer)
- C. Large, irregular nuclei, nuclear grooves, and Psammoma bodies
- D. Spindle cells, pleomorphic giant cells, and mitotic figures
- E. Multinucleated giant cells, macrophages, and degenerated follicular cells
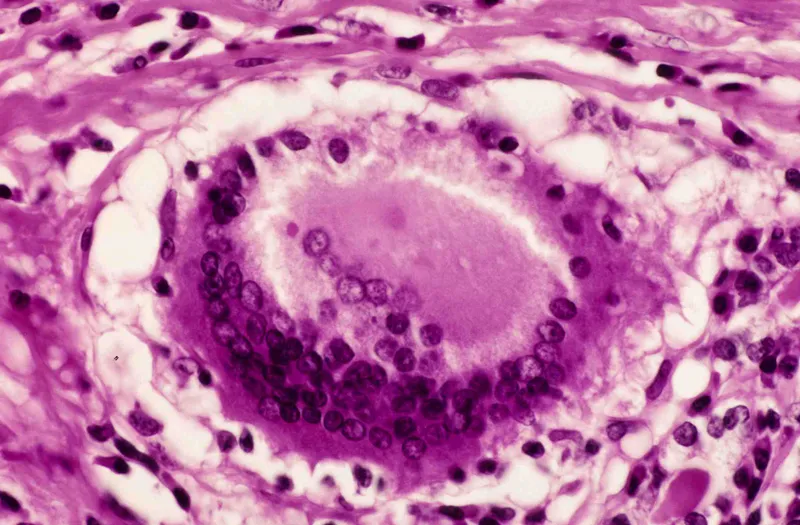
Thyroiditis Explanation: ***Lymphocytic infiltration, Hürthle cells, and germinal centers***
- The patient's symptoms (fatigue, constipation, fuller cheeks, hoarse voice, dry and cool skin, brittle nails, bradycardia, mildly enlarged thyroid gland) are classic for **hypothyroidism**. The presence of **anti-thyroid peroxidase antibodies** confirms an autoimmune etiology, specifically **Hashimoto's thyroiditis**.
- **Hashimoto's thyroiditis** is characterized pathologically by extensive **lymphocytic infiltration** of the thyroid parenchyma, the presence of **Hürthle cells** (metaplastic follicular cells with abundant eosinophilic cytoplasm), and the formation of **germinal centers** within the thyroid gland.
*Tall follicular cells, scalloped colloid, and vascular congestion*
- This description is characteristic of **Graves' disease**, an autoimmune cause of **hyperthyroidism**.
- The patient's symptoms and signs (e.g., bradycardia, dry skin, constipation) are consistent with **hypothyroidism**, not hyperthyroidism.
*Large, irregular nuclei, nuclear grooves, and Psammoma bodies*
- These are classic histological features of **papillary thyroid carcinoma**, the most common type of thyroid cancer.
- While thyroid nodules can occur in Hashimoto's, the overall clinical picture points strongly to a benign autoimmune inflammatory process, not malignancy.
*Spindle cells, pleomorphic giant cells, and mitotic figures*
- This describes **anaplastic thyroid carcinoma**, a highly aggressive and undifferentiated thyroid malignancy.
- Anaplastic carcinoma typically presents as a rapidly enlarging, painful neck mass in older individuals, which is not consistent with this patient's chronic, milder presentation.
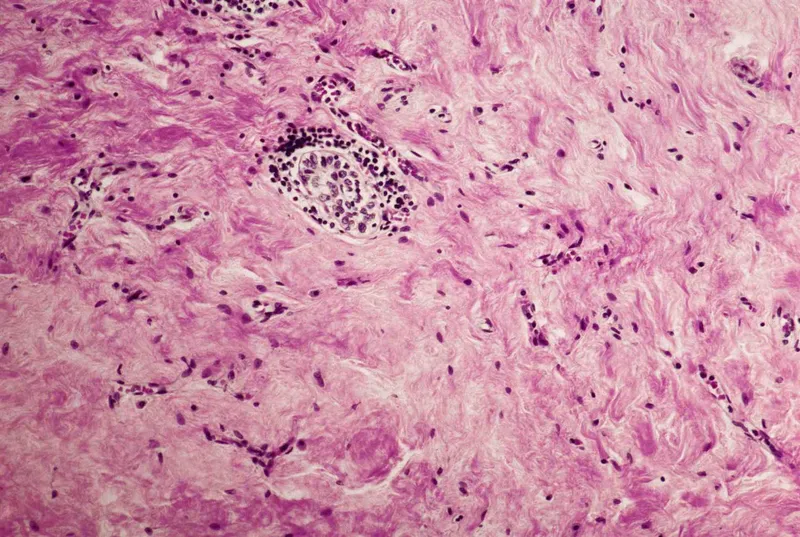
*Multinucleated giant cells, macrophages, and degenerated follicular cells*
- This histological pattern is characteristic of **subacute granulomatous thyroiditis (de Quervain's thyroiditis)**.
- Subacute thyroiditis typically presents with painful thyroid enlargement and often follows a viral infection, which is not suggested by the patient's symptoms or antibody findings.
Thyroiditis US Medical PG Question 6: A 33-year-old woman comes to the physician because of a 4-day history of fever, anterior neck pain, and throat swelling. She has no history of serious illness. Her temperature is 38.1°C (100.6°F) and pulse is 109/min. Physical examination shows diaphoresis and a fine tremor of the outstretched hands. The thyroid gland is enlarged, firm, and tender to palpation. Serum thyroid stimulating hormone level is 0.06 μU/mL and erythrocyte sedimentation rate is 65 mm/h. 123I scan shows an enlarged thyroid gland with diffusely decreased uptake. Histologic examination of a thyroid biopsy specimen is most likely to show which of the following findings?
- A. Undifferentiated giant cells with areas of necrosis and hemorrhage
- B. Noncaseating granulomas with multinucleated giant cells (Correct Answer)
- C. Lymphocytic infiltration with germinal follicle formation
- D. Follicular epithelial cell hyperplasia
- E. Concentric intracellular lamellar calcifications
Thyroiditis Explanation: ***Noncaseating granulomas with multinucleated giant cells***
- This finding is characteristic of **subacute granulomatous (de Quervain) thyroiditis**, which is supported by the patient's symptoms: anterior neck pain, fever, elevated ESR, and tender thyroid.
- The **low TSH and decreased radioactive iodine uptake** indicate thyroid damage with release of preformed thyroid hormones, typical of the initial thyrotoxic phase of this condition.
*Undifferentiated giant cells with areas of necrosis and hemorrhage*
- This description is more consistent with **anaplastic thyroid carcinoma**, a highly aggressive malignancy, which is unlikely in a 33-year-old woman presenting with a 4-day history of symptoms.
- Anaplastic carcinoma would typically cause a rapidly enlarging, fixed, and firm mass, often with obstructive symptoms, rather than a tender gland with signs of thyrotoxicosis.
*Lymphocytic infiltration with germinal follicle formation*
- This is the histological hallmark of **Hashimoto's thyroiditis**, an autoimmune condition leading to hypothyroidism.
- Patients with Hashimoto's typically present with hypothyroidism, goiter, and positive thyroid antibodies, not acute pain, fever, or the transient thyrotoxicosis seen here.
*Follicular epithelial cell hyperplasia*
- This is seen in conditions causing chronic stimulation of the thyroid gland, such as **diffuse toxic goiter (Graves' disease)** or in patients with iodine deficiency.
- Graves' disease would present with hyperthyroidism and diffuse uptake on a radioactive iodine scan, which contradicts the "diffusely decreased uptake" seen in this patient.
*Concentric intracellular lamellar calcifications*
- These are known as **Psammoma bodies** and are characteristic of **papillary thyroid carcinoma**.
- Papillary thyroid carcinoma is typically a slow-growing, painless mass and is not associated with acute inflammatory symptoms like fever, pain, and a very elevated ESR.
Thyroiditis US Medical PG Question 7: A 50-year-old woman comes to the physician for the evaluation of fatigue over the past 6 months. During this period, the patient has also had a 5 kg (11-lb) weight loss. She has a history of Hashimoto thyroiditis. She is sexually active with her husband only. She does not smoke. She drinks one glass of wine per day. She does not use illicit drugs. Her only medication is levothyroxine. Temperature is 37°C (98.6°F), pulse is 70/min, and blood pressure is 110/70 mm Hg. Abdominal examination shows tenderness in the right upper quadrant with no rebound or guarding. Laboratory studies show a serum alanine aminotransferase level of 190 U/L, serum aspartate aminotransferase level of 250 U/L, and serum total bilirubin level of 0.6 mg/dL. Liver biopsy shows plasma cell infiltration and areas of periportal piecemeal necrosis. Further evaluation of this patient is most likely to show which of the following findings?
- A. Positive anti-smooth muscle antibodies (Correct Answer)
- B. Elevated serum transferrin saturation
- C. Positive anti-HCV antibodies
- D. Positive anti-mitochondrial antibodies
- E. Positive HBV surface antigen
Thyroiditis Explanation: ***Positive anti-smooth muscle antibodies***
- The patient's history of **Hashimoto thyroiditis**, fatigue, weight loss, elevated transaminases, and liver biopsy showing **plasma cell infiltration** and **periportal piecemeal necrosis** are classic features of **autoimmune hepatitis**.
- **Type 1 autoimmune hepatitis**, accounting for about 80% of cases, is strongly associated with the presence of **anti-smooth muscle antibodies (ASMA)** and **antinuclear antibodies (ANA)**.
*Elevated serum transferrin saturation*
- **Elevated transferrin saturation** is a hallmark of **hemochromatosis**, a disorder of iron overload.
- While hemochromatosis can cause liver damage, the biopsy findings of plasma cell infiltration and periportal piecemeal necrosis are not consistent with iron deposition.
*Positive anti-HCV antibodies*
- **Positive anti-HCV antibodies** indicate exposure to the **hepatitis C virus**, which can cause chronic hepatitis and cirrhosis.
- However, the biopsy findings, particularly the **plasma cell infiltration**, are more characteristic of autoimmune hepatitis than viral hepatitis.
*Positive anti-mitochondrial antibodies*
- **Anti-mitochondrial antibodies (AMAs)** are the serological hallmark of **primary biliary cholangitis (PBC)**.
- PBC primarily affects the small bile ducts, leading to cholestasis, and typically presents with signs like **pruritus** and elevated **alkaline phosphatase**, which are not reported here.
*Positive HBV surface antigen*
- **Positive hepatitis B virus (HBV) surface antigen** indicates either acute or chronic **hepatitis B infection**.
- While HBV can cause chronic liver inflammation, the biopsy findings of **plasma cell infiltration** are not typical for viral hepatitis, making autoimmune hepatitis a more likely diagnosis given the clinical context.
Thyroiditis US Medical PG Question 8: A 43-year-old woman comes to the physician because of a 6-week history of hoarseness and difficulty swallowing. She also has a history of lower back pain treated with ibuprofen. She is 162 cm (5 ft 4 in) tall and weighs 77 kg (169 lb); BMI is 29 kg/m2. Her pulse is 64/min and blood pressure is 130/86 mm Hg. Physical examination shows dry skin, swelling of the lower extremities, and a hard nontender anterior neck swelling that does not move with swallowing. Femoral and pedal pulses are decreased bilaterally. A biopsy of the neck swelling is most likely to show which of the following findings?
- A. Atypical nuclei and concentric lamellar calcifications
- B. Giant cells and noncaseating granulomas
- C. Lymphocytic infiltrate and germinal center formation
- D. Collagen deposition and decreased number of follicles (Correct Answer)
- E. Spindle cells and areas of focal necrosis
Thyroiditis Explanation: ***Collagen deposition and decreased number of follicles***
- The patient's symptoms of **hoarseness**, **difficulty swallowing**, **dry skin**, **lower extremity swelling**, and **decreased pulses** suggest **hypothyroidism**.
- The presence of a **hard, nontender anterior neck swelling that does not move with swallowing** points towards a **fibrotic thyroiditis**, specifically **Riedel's thyroiditis**, which is characterized by extensive **collagen deposition** and a reduction in normal thyroid follicles.
*Atypical nuclei and concentric lamellar calcifications*
- This describes **psammoma bodies** and atypical nuclei, which are characteristic of **papillary thyroid carcinoma**.
- While thyroid cancer can cause hoarseness and dysphagia, the diffuse, hard, nontender neck swelling, and systemic symptoms of hypothyroidism are less typical for papillary carcinoma.
*Giant cells and noncaseating granulomas*
- This histological finding is characteristic of **De Quervain's (subacute) thyroiditis**, which typically presents with a **painful** thyroid gland and often precedes a transient hypothyroid phase.
- The patient's thyroid swelling is explicitly described as **nontender**, ruling out De Quervain's.
*Lymphocytic infiltrate and germinal center formation*
- This describes **Hashimoto's thyroiditis**, which is an autoimmune cause of hypothyroidism and diffuse goiter, but the goiter is usually **rubbery** and not typically described as **hard** and fixed like in this case.
- While it causes hypothyroidism, the fibrotic nature of the mass and lack of mobility suggest a more chronic, sclerosing process.
*Spindle cells and areas of focal necrosis*
- This is a description more consistent with an **anaplastic thyroid carcinoma**, a highly aggressive malignancy.
- While anaplastic carcinoma can cause rapid neck swelling, hoarseness, and dysphagia, the other systemic signs of hypothyroidism are less directly indicative of anaplastic carcinoma itself.
Thyroiditis US Medical PG Question 9: A 50-year-old man presents to a clinic with oliguria. Four weeks ago, he had a kidney transplant. Postoperative follow-up was normal. He is currently on cyclosporine and admits that sometimes he forgets to take his medication. On physical examination, the vital signs include: temperature 37.1°C (98.8°F), blood pressure 165/110 mm Hg, heart rate 80/min, and respiratory rate 16/min. There is mild tenderness on renal palpation. His serum creatinine level is 4 mg/dL, well above his baseline level after the transplant. Which of the following best describes the histological finding if a biopsy is taken from the transplanted kidney?
- A. Lymphocytic infiltration of graft vessels and endothelial damage (Correct Answer)
- B. Thrombosis and occlusion of vessels
- C. Atherosclerosis on angiography
- D. Necrosis with granulation tissue
- E. Thickening of blood vessels, fibrosis of graft vessels, and parenchymal atrophy
Thyroiditis Explanation: ***Lymphocytic infiltration of graft vessels and endothelial damage***
- The patient's presentation with **oliguria**, elevated **creatinine**, and **hypertension** following a recent kidney transplant, especially with a history of non-adherence to **cyclosporine** (an immunosuppressant), strongly indicates **acute rejection**.
- Histologically, acute rejection is characterized by **lymphocytic infiltration** of the graft vessels (often referred to as **vasculitis** or **endotheliitis**) and associated **endothelial damage**.
*Thrombosis and occlusion of vessels*
- This finding is more characteristic of **hyperacute rejection**, which typically occurs within minutes to hours of transplantation, not weeks later.
- Hyperacute rejection is mediated by **pre-formed antibodies** and leads to severe, rapid graft failure due to widespread intravascular thrombosis.
*Atherosclerosis on angiography*
- While post-transplant patients can develop accelerated atherosclerosis (a form of **chronic rejection**), it is typically a long-term complication developing months to years after transplantation.
- The acute presentation with rapid creatinine elevation is not typical for primary atherosclerosis.
*Necrosis with granulation tissue*
- **Necrosis** with **granulation tissue** is a general healing response to significant tissue injury or inflammation.
- While some cellular necrosis can occur in severe rejection, it's not the defining feature, and granulation tissue indicates a more prolonged, subacute process rather than the primary histological hallmark of acute rejection.
*Thickening of blood vessels, fibrosis of graft vessels, and parenchymal atrophy*
- These are classic features of **chronic rejection**, which manifests months to years after transplantation as a gradual decline in graft function.
- **Chronic rejection** involves progressive damage leading to vasculopathy, interstitial fibrosis, and tubular atrophy, rather than the acute inflammatory cellular infiltrate seen here.
Thyroiditis US Medical PG Question 10: Two hours after undergoing allogeneic kidney transplantation for polycystic kidney disease, a 14-year-old girl has lower abdominal pain. Examination shows tenderness to palpation in the area the donor kidney was placed. Ultrasound of the donor kidney shows diffuse tissue edema. Serum creatinine begins to increase and dialysis is initiated. Which of the following is the most likely cause of this patient's symptoms?
- A. Preformed antibodies against class I HLA molecules (Correct Answer)
- B. Immune complex deposition in donor tissue
- C. T-lymphocyte activation by donor HLA peptides
- D. Irreversible intimal fibrosis and obstruction of vessels
- E. Proliferation of donor T lymphocytes
Thyroiditis Explanation: ***Preformed antibodies against class I HLA molecules***
- This scenario describes **hyperacute rejection**, a rapid and severe immune response occurring minutes to hours post-transplant.
- It is mediated by **preformed antibodies** (often anti-HLA antibodies) in the recipient's circulation that bind to donor antigens, leading to complement activation, endothelial damage, and graft thrombosis.
*Immune complex deposition in donor tissue*
- This mechanism is characteristic of **Type III hypersensitivity** reactions, which are not typically involved in hyperacute rejection.
- Immune complex deposition is more common in conditions like **lupus nephritis** or **post-streptococcal glomerulonephritis**, not immediate graft failure.
*T-lymphocyte activation by donor HLA peptides*
- This describes the mechanism of **acute cellular rejection**, which is mediated by host T-lymphocytes recognizing donor HLA antigens.
- Acute rejection typically occurs days to weeks or months after transplantation, not within hours.
*Irreversible intimal fibrosis and obstruction of vessels*
- This process is characteristic of **chronic rejection**, which develops months to years after transplantation.
- Chronic rejection is a slow, progressive decline in graft function due to vascular damage, fibrosis, and ultimately graft failure.
*Proliferation of donor T lymphocytes*
- Proliferation of donor T lymphocytes is not a mechanism of transplant rejection but rather relevant to **graft-versus-host disease (GVHD)**.
- GVHD occurs when immunocompetent T-cells in the donor tissue (e.g., bone marrow transplant) attack recipient tissues.
More Thyroiditis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.