Thyroid diseases (hyper/hypothyroidism) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thyroid diseases (hyper/hypothyroidism). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 1: A 37-year-old man presents to his primary care physician because he has had constipation for the last several weeks. He has also been feeling lethargic and complains that this winter has been particularly cold. He also complains that he has been gaining weight despite no change in his normal activities. He reveals that two months prior to presentation he had what felt like the flu for which he took Tylenol and did not seek medical attention. Several days after this he developed anterior neck pain. Which of the following findings would most likely be seen on biopsy of this patient's abnormality?
- A. Focal hyperplasia
- B. Germinal follicles
- C. Scalloped clear areas
- D. Fibrous tissue
- E. Granulomatous inflammation (Correct Answer)
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Granulomatous inflammation***
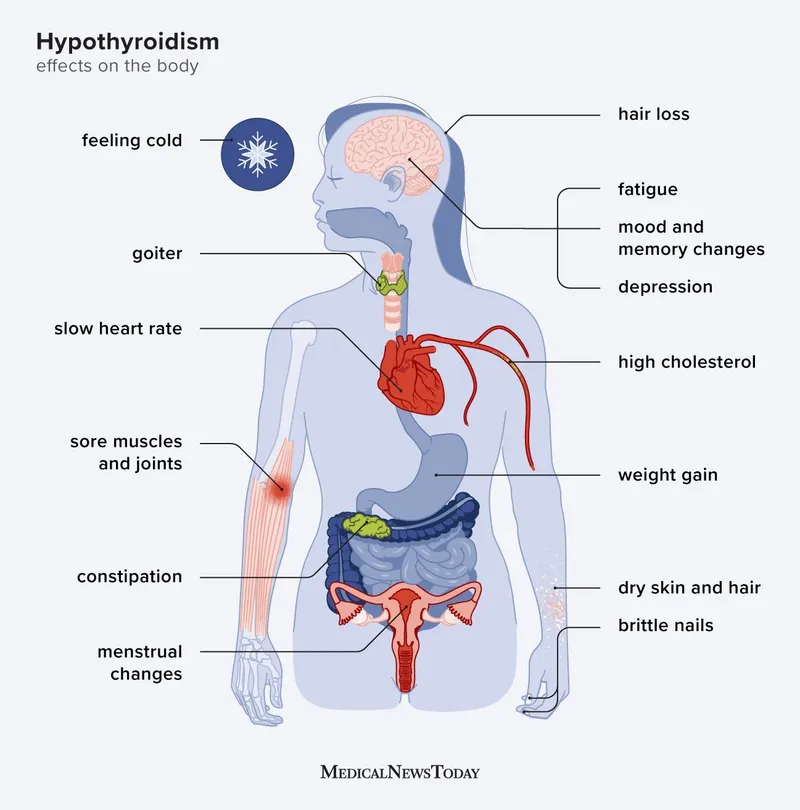
- The patient's presentation with **constipation**, **lethargy**, **cold intolerance**, and **weight gain** after a flu-like illness followed by **anterior neck pain** is highly suggestive of **subacute granulomatous thyroiditis (de Quervain thyroiditis)**.
- A biopsy of the thyroid in cases of de Quervain thyroiditis typically reveals **granulomatous inflammation** with scattered **giant cells** and lymphocytes, reflecting the destructive inflammatory process.
*Focal hyperplasia*
- **Focal hyperplasia** is characterized by an increase in the number of thyroid follicular cells and is seen in conditions like **Graves' disease** or **multinodular goiter**, particularly when the gland is overstimulated.
- This finding would not be expected in subacute granulomatous thyroiditis, where the primary pathology is destruction rather than proliferation.
*Germinal follicles*
- **Germinal follicles** are characteristic of chronic lymphocytic thyroiditis (**Hashimoto's thyroiditis**), an autoimmune condition where the thyroid gland is infiltrated by lymphocytes, plasma cells, and macrophages.
- While Hashimoto's can cause hypothyroidism, the preceding flu-like illness and acute neck pain make de Quervain thyroiditis a more likely diagnosis.
*Scalloped clear areas*
- **Scalloped clear areas** at the colloid-epithelial interface, also known as **colloid resorption vacuoles**, are a histological feature of **hyperactive thyroid follicles**, typically seen in conditions causing hyperthyroidism like **Graves' disease**.
- The patient's symptoms of lethargy, cold intolerance, and weight gain indicate hypothyroidism, which can follow the initial hyperthyroid phase of de Quervain thyroiditis but are not indicative of active hyperfunction on biopsy at this stage.
*Fibrous tissue*
- An increased amount of **fibrous tissue** is characteristic of **Riedel's thyroiditis**, a rare condition characterized by dense fibrosis that replaces normal thyroid parenchyma and can extend into surrounding neck structures.
- This patient's presentation with a preceding febrile illness and neck pain is not typical for Riedel's thyroiditis, which usually presents as a hard, fixed mass without an antecedent viral infection.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 2: A 42-year-old man is referred for an endocrinology consult because of decreased triiodothyronine (T3) hormone levels. He presented to the emergency department 1 week prior to this consultation with pneumonia and was admitted to a medicine service for management of his infection. He has since recovered from his infection after intravenous antibiotic administration. He currently has no symptoms and denies feeling cold or lethargic. A panel of laboratory tests are obtained with the following results:
Thyroid-stimulating hormone: 4.7 µU/mL
Thyroxine (T4): 6 µg/dL
Triiodothyronine (T3): 68 ng/dL
Which of the following additional findings would most likely also be seen in this patient?
- A. Increased free T3 concentration
- B. Increased reverse T3 concentration (Correct Answer)
- C. Decreased free T3 concentration
- D. Normal free and reverse T3 concentration
- E. Decreased reverse T3 concentration
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Increased reverse T3 concentration***
- The patient's presentation including recent severe illness (pneumonia), normal TSH, slightly low T4, and low T3, with no symptoms of hypothyroidism, is classic for **euthyroid sick syndrome** (also known as non-thyroidal illness syndrome).
- In euthyroid sick syndrome, there is a characteristic increase in the peripheral conversion of T4 to **inactive reverse T3 (rT3)** rather than to active T3, due to altered deiodinase activity (decreased type 1 deiodinase and increased type 3 deiodinase).
- **Elevated rT3 is the most specific finding** that distinguishes euthyroid sick syndrome from primary hypothyroidism.
*Increased free T3 concentration*
- This would contradict the initial finding of **decreased total T3** and the typical pattern of euthyroid sick syndrome, where free T3 is usually decreased or low-normal.
- An increased free T3 level would suggest **hyperthyroidism**, which is inconsistent with the patient's clinical picture and other lab values.
*Decreased free T3 concentration*
- While free T3 would indeed be decreased in euthyroid sick syndrome along with total T3, this finding is **less specific** than elevated reverse T3.
- Decreased free T3 can be seen in **primary hypothyroidism, central hypothyroidism, and euthyroid sick syndrome**, making it less diagnostically useful.
- The question asks for the "most likely" additional finding, and **elevated reverse T3 is the hallmark biochemical marker** that best characterizes euthyroid sick syndrome and differentiates it from true hypothyroidism.
*Normal free and reverse T3 concentration*
- This would be inconsistent with the primary finding of **decreased T3** and the clinical context of recent severe illness, which almost invariably alters thyroid hormone metabolism.
- Normal levels would imply that the initial T3 finding was an anomaly or that the patient does not have euthyroid sick syndrome.
*Decreased reverse T3 concentration*
- A decreased reverse T3 concentration is typically seen in conditions like **hyperthyroidism** or during recovery phases of severe illness, not during the acute phase where rT3 is elevated.
- This finding would contradict the metabolic adaptations seen in **euthyroid sick syndrome**, where T4 is preferentially converted to rT3 (via type 3 deiodinase) to conserve energy during critical illness.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 3: A 39-year-old female presents to the clinic with the complaints of dry skin for a few months. She adds that she also has constipation for which she started eating vegetables and fruits but with no improvement. She lives with her husband and children who often complain when she turns the air conditioning to high as she cannot tolerate low temperatures. She has gained 5 kgs (11.2 lb) since her last visit 2 months back although her diet has not changed much. Her past medical history is relevant for cardiac arrhythmias and diabetes. She is on several medications currently. Her temperature is 98.6° F (37° C), respirations are 15/min, pulse is 57/min and blood pressure is 132/98 mm Hg. A physical examination is within normal limits. Thyroid function test results are given below:
Serum
TSH: 13.0 μU/mL
Thyroxine (T4): 3.0 μg/dL
Triiodothyronine (T3): 100 ng/dL
Which of the following medications is most likely to be responsible for her symptoms?
- A. Amiodarone (Correct Answer)
- B. Digoxin
- C. Metformin
- D. Theophylline
- E. Warfarin
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Amiodarone***
- Amiodarone is a known cause of both **hypothyroidism** and **hyperthyroidism** due to its iodine content and direct toxic effects on the thyroid gland. The patient's symptoms (dry skin, constipation, **cold intolerance**, **weight gain**, bradycardia) and thyroid function tests (high TSH, low T4, low T3) are highly consistent with drug-induced hypothyroidism.
- The patient's history of **cardiac arrhythmias** makes amiodarone a plausible medication she would be taking, as it is a common antiarrhythmic drug.
*Digoxin*
- Digoxin is primarily used to treat **heart failure** and certain arrhythmias, but it does not typically cause thyroid dysfunction.
- Its common side effects include gastrointestinal upset, visual disturbances, and various arrhythmias, which do not align with the patient's predominant symptoms of hypothyroidism.
*Metformin*
- Metformin is an oral hypoglycemic agent used to treat **Type 2 diabetes**, a condition the patient also has.
- It does not have substantial effects on thyroid hormone synthesis or metabolism and is not associated with hypothyroidism or hyperthyroidism.
*Theophylline*
- Theophylline is a bronchodilator used in the treatment of **asthma** and **COPD**.
- It is not known to cause thyroid dysfunction, and its side effects mainly involve the central nervous system, gastrointestinal tract, and cardiovascular system.
*Warfarin*
- Warfarin is an **anticoagulant** prescribed to prevent blood clots.
- It has no direct known interaction with thyroid hormone synthesis or metabolism and is not associated with thyroid dysfunction.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 4: An investigator is studying a drug that acts on the thyroid hormone pathway. Levels of serum free T3 and T4 in healthy participants are measured before and after administration of the drug. After administration, there is a decrease in the average serum free T3 level, while the average serum free T4 level is increased compared to initial serum studies. Inhibition of which of the following is the most likely mechanism of action of this drug?
- A. Thyroid-stimulating hormone
- B. Follicular iodotyrosine deiodinase
- C. Follicular thyroid peroxidase
- D. Peripheral 5'-deiodinase (Correct Answer)
- E. Follicular thyroid proteases
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Peripheral 5'-deiodinase***
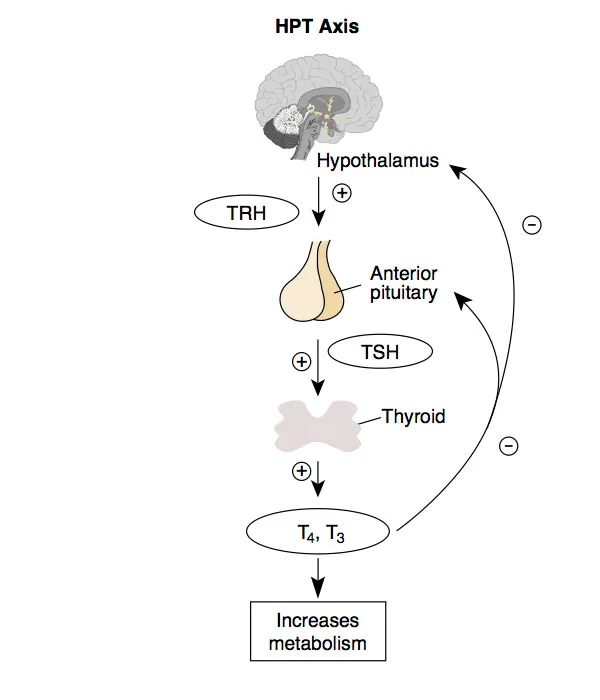
- Inhibition of **peripheral 5'-deiodinase** would decrease the conversion of **T4 to T3** in the periphery, resulting in lower **free T3** and higher **free T4** levels.
- This enzyme is crucial for activating T4 into the more potent T3, and its blockade explains the observed changes in hormone levels.
*Thyroid-stimulating hormone*
- Inhibition of **TSH** would lead to a decrease in the production and release of both **T3 and T4** from the thyroid gland.
- This contradicts the observed increase in **free T4** levels.
*Follicular iodotyrosine deiodinase*
- This enzyme is involved in recycling iodine from **monoiodotyrosine (MIT)** and **diiodotyrosine (DIT)** within the thyroid follicular cells, which is important for efficient thyroid hormone synthesis.
- Its inhibition would primarily affect iodine availability and synthesis, not directly lead to increased T4 and decreased T3 in the periphery.
*Follicular thyroid peroxidase*
- **Thyroid peroxidase (TPO)** is critical for the **iodination of tyrosine residues** on thyroglobulin and the **coupling of MIT and DIT** to form T3 and T4.
- Inhibition of TPO would decrease the synthesis of both **T3 and T4**, contrary to the observed increase in **free T4**.
*Follicular thyroid proteases*
- **Thyroid proteases** cleave thyroglobulin to release mature **T3 and T4** into the bloodstream.
- Inhibition of these proteases would lead to a decrease in the release of both **T3 and T4**, which does not align with the observed increase in **free T4**.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 5: A 39-year-old woman with type 1 diabetes mellitus comes to the physician because of a 2-month history of fatigue and hair loss. She has smoked one pack of cigarettes daily for the past 15 years. Her only medication is insulin. Her pulse is 59/min and blood pressure is 102/76 mm Hg. Physical examination shows dry skin, coarse hair, and a nontender, diffuse neck swelling in the anterior midline. Further evaluation of this patient is most likely to show which of the following findings?
- A. DR5 subtype on HLA haplotype analysis
- B. Biphasic spindle cells on biopsy of the swelling
- C. Diffusely increased uptake on a radioactive iodine scan
- D. B8 subtype on HLA haplotype analysis
- E. Antimicrosomal antibodies in serum (Correct Answer)
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Antimicrosomal antibodies in serum***
- The patient's symptoms (fatigue, hair loss, dry skin, coarse hair, bradycardia, diffuse neck swelling) and history (type 1 diabetes) are highly suggestive of **Hashimoto's thyroiditis**, an autoimmune thyroid disease.
- **Antimicrosomal antibodies (anti-TPO antibodies)** are characteristic markers for Hashimoto's thyroiditis, indicating autoimmune destruction of thyroid tissue.
*DR5 subtype on HLA haplotype analysis*
- While type 1 diabetes is associated with certain HLA subtypes (e.g., DR3, DR4), **DR5** is not typically linked to Hashimoto's thyroiditis.
- This option is less specific and less directly indicative of the present thyroid pathology compared to antimicrosomal antibodies.
*Biphasic spindle cells on biopsy of the swelling*
- **Biphasic spindle cells** are characteristic of **solitary fibrous tumors** or **synovial sarcomas**, neither of which fits the clinical picture of a diffuse, nontender neck swelling associated with hypothyroidism.
- A biopsy of a typical Hashimoto's goiter would show **lymphocytic infiltration** and **Hürthle cells**.
*Diffusely increased uptake on a radioactive iodine scan*
- **Diffusely increased uptake** on a radioactive iodine scan is characteristic of **Graves' disease** (hyperthyroidism), where the thyroid gland is overactive.
- In Hashimoto's thyroiditis, especially in the hypothyroid phase, uptake is typically **reduced** or normal, as the gland's function is impaired.
*B8 subtype on HLA haplotype analysis*
- **HLA-B8** is associated with certain autoimmune conditions like **Graves' disease** and **myasthenia gravis**, but it is not a primary or direct indicator for Hashimoto's thyroiditis.
- As with other HLA subtypes, serological markers are more directly diagnostic for thyroid diseases.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 6: A 31-year-old female presents to the clinic with excessive anxiety and palpitations for a month. She also mentions loss of 2.72 kg (6 lb) of her weight over the last month. Her past medical history is insignificant. She does not smoke nor does she drink alcohol. Her temperature is 37°C (98.6°F), pulse is 81/min, respiratory rate is 23/min, and blood pressure is 129/88 mm Hg. On examination, mild exophthalmos is noted. Heart and lung examination is normal including cardiac auscultation. What is the most likely cause of her symptoms?
- A. Thyroid stimulating antibodies (Correct Answer)
- B. Inadequate iodine in her diet
- C. Lithium use
- D. Use of propylthiouracil
- E. Medullary carcinoma of the thyroid
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Thyroid stimulating antibodies***
- The patient's symptoms of **anxiety**, **palpitations**, **weight loss**, and **exophthalmos** are characteristic of **hyperthyroidism**, specifically **Graves' disease**.
- **Graves' disease** is an autoimmune condition caused by **thyroid-stimulating immunoglobulins (TSI)**, which act as agonists at the TSH receptor, leading to excessive thyroid hormone production.
*Inadequate iodine in her diet*
- **Iodine deficiency** is a common cause of **hypothyroidism** and **goiter**, where the thyroid gland is unable to produce sufficient thyroid hormones.
- This condition presents with symptoms such as **fatigue, weight gain, constipation**, and **cold intolerance**, which are opposite to the patient's presentation.
*Lithium use*
- **Lithium** is primarily used as a mood stabilizer and is known to cause **hypothyroidism** or, less commonly, euthyroid goiter due to its interference with thyroid hormone synthesis and release.
- This would not explain the patient's hyperthyroid symptoms of anxiety, palpitations, and weight loss.
*Use of propylthiouracil*
- **Propylthiouracil (PTU)** is an **antithyroid medication** used to treat hyperthyroidism by inhibiting thyroid hormone synthesis.
- Its use would lead to a reduction in thyroid hormone levels and would not be the cause of the patient's hyperthyroid symptoms.
*Medullary carcinoma of the thyroid*
- **Medullary thyroid carcinoma** is a neuroendocrine tumor that arises from parafollicular C cells and secretes **calcitonin**.
- It typically presents as a thyroid nodule and usually does not cause symptoms of hyperthyroidism unless very advanced and aggressive.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 7: A 34-year-old woman presents to the physician because of fever and sore throat for 2 days. She also reports generalized body pain and fatigue over this period. She was diagnosed with Graves’ disease 6 months ago. Because of arthralgias and rash due to methimazole 3 months ago, her physician switched methimazole to PTU. She appears ill. The vital signs include: temperature 38.4℃ (101.1℉), pulse 88/min, respiratory rate 12/min, and blood pressure 120/80 mm Hg. A 1 × 1 cm ulcer is seen on the side of the tongue and is painful with surrounding erythema. Examination of the neck, lungs, heart, and abdomen shows no abnormalities. She had normal liver aminotransferases last week. Which of the following is the most important diagnostic study at this time?
- A. No further testing is indicated
- B. Complete blood count with differential (Correct Answer)
- C. Erythrocyte sedimentation rate
- D. Thyroid-stimulating hormone
- E. Alanine aminotransferase
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Complete blood count with differential***
- The patient's history of **Grave's disease** managed with **propylthiouracil (PTU)**, combined with symptoms of fever, sore throat, and oral ulcer, points to a high suspicion for **agranulocytosis**.
- A **CBC with differential** is critical to assess the **neutrophil count**, which would be severely low in agranulocytosis.
*No further testing is indicated*
- This statement is incorrect because the patient's symptoms (fever, sore throat, oral ulcer) in the context of PTU use are highly concerning for **adverse drug reactions**, particularly **agranulocytosis**, which requires immediate investigation.
- Delaying testing could lead to severe, potentially life-threatening complications due to **neutropenia** and increased susceptibility to infection.
*Erythrocyte sedimentation rate*
- While an **ESR** would likely be elevated due to the inflammatory response from fever and infection, it is a **non-specific marker** of inflammation.
- It would not provide the crucial information about the **neutrophil count** needed to diagnose or rule out agranulocytosis.
*Thyroid-stimulating hormone*
- The patient's **Graves' disease** is already diagnosed, and she is undergoing treatment. Her current symptoms are acute and unlikely to be directly related to fluctuations in **TSH levels**.
- A **TSH test** would not help diagnose the acute febrile illness or potential adverse drug reaction she is experiencing.
*Alanine aminotransferase*
- Although **PTU** can cause **hepatotoxicity**, the patient's **ALT** levels were normal last week, and her primary symptoms (fever, sore throat, oral ulcer) are not typical for acute liver injury.
- While liver function might be monitored periodically in patients on PTU, it is not the most immediate or relevant diagnostic study for her current acute presentation.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 8: A 19-year-old African American male with a history of bipolar I disorder presents to the psychiatrist for a follow-up visit. During the session, the patient explains that for the past 2 months he has felt significantly fatigued and constipated. He is always complaining of feeling cold and has gained several pounds although his diet has not changed. A blood sample was sent for analysis, revealing the following: TSH - 6 mIU/L (nl = 0.4-4.0 mIU/L), free T4 - 0.4 ng/dL (nl = 0.7-1.9 ng/dL), and serum T4 - 2.1 mcg/dL (nl = 4.6-12 mcg/dL). Which of the following is responsible for these abnormalities?
- A. Valproic acid
- B. Lamotrigine
- C. Lithium (Correct Answer)
- D. Olanzapine
- E. Carbamazepine
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Lithium***
- The patient's symptoms (fatigue, constipation, cold intolerance, weight gain) and lab results (**elevated TSH** and **low free T4/T4**) are consistent with **hypothyroidism**.
- **Lithium** is a known mood stabilizer used in bipolar disorder that can induce hypothyroidism by interfering with thyroid hormone synthesis and release.
*Valproic acid*
- Valproic acid can cause several side effects, including **hepatotoxicity**, **pancreatitis**, and **thrombocytopenia**, but it does not typically cause hypothyroidism.
- It works by increasing GABA levels in the brain and is not known to directly affect thyroid function in a manner that would cause these symptoms and lab findings.
*Lamotrigine*
- Lamotrigine is an anticonvulsant and mood stabilizer primarily associated with dermatological side effects like **Stevens-Johnson syndrome (SJS)**.
- It is not commonly linked to thyroid dysfunction or the development of hypothyroidism.
*Olanzapine*
- Olanzapine is an atypical antipsychotic known for metabolic side effects such as **weight gain**, **hyperglycemia**, and **dyslipidemia**.
- While it can cause weight gain, it does not typically lead to the specific constellation of symptoms and thyroid hormone abnormalities seen in this patient.
*Carbamazepine*
- Carbamazepine is an anticonvulsant that can cause side effects like **hyponatremia** (due to SIADH) and **agranulocytosis**.
- Although it can rarely lead to thyroid abnormalities, it’s less commonly associated with symptomatic hypothyroidism and the specific lab profile presented compared to lithium.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 9: A previously healthy 27-year-old man comes to the physician because of a 3-week history of anxiety, diarrhea, and a 4.1-kg (9-lb) weight loss. On questioning, he also reports that he noticed a painless mass on his left testicle 2 weeks ago. His pulse is 110/min and irregular and blood pressure is 150/70 mm Hg. Examination shows diaphoresis and a fine tremor of the outstretched fingers. Testicular examination shows a 3-cm, firm, nontender mass on the left scrotum that does not transilluminate. This patient's underlying condition is most likely to be associated with which of the following findings?
- A. Elevated serum AFP
- B. Elevated serum hCG (Correct Answer)
- C. Elevated serum TSH
- D. Proptosis on exophthalmometry
- E. Positive urine metanephrines
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Elevated serum hCG***
- The patient presents with symptoms of **hyperthyroidism** (anxiety, weight loss, tachycardia, tremor, diaphoresis) and a **testicular mass**.
- Some **testicular germ cell tumors**, particularly **choriocarcinoma** and some **mixed germ cell tumors**, can produce **hCG**, which has structural similarity to TSH and can stimulate the thyroid gland, leading to **paraneoplastic hyperthyroidism**.
- **Serum hCG** is an important tumor marker for germ cell tumors and would be elevated in this clinical scenario.
*Elevated serum AFP*
- **Alpha-fetoprotein (AFP)** is a tumor marker often elevated in **non-seminomatous germ cell tumors** like **yolk sac tumors** and **embryonal carcinomas**.
- While AFP may be elevated in some testicular tumors, it does not explain the hyperthyroid symptoms, as hCG (not AFP) has TSH-like activity.
*Elevated serum TSH*
- In **hyperthyroidism**, the **thyroid stimulating hormone (TSH)** level is typically **suppressed** due to negative feedback from high thyroid hormone levels.
- An elevated TSH would indicate **primary hypothyroidism**, which contradicts the patient's clinical presentation.
*Proptosis on exophthalmometry*
- **Proptosis** (exophthalmos) is a common finding in **Graves' disease**, an autoimmune cause of hyperthyroidism.
- However, the presence of a **testicular mass** strongly suggests a paraneoplastic etiology for the hyperthyroidism, making Graves' disease less likely as the primary underlying condition.
*Positive urine metanephrines*
- **Urine metanephrines** are markers elevated in **pheochromocytoma**, a tumor of the adrenal medulla that secretes catecholamines.
- While pheochromocytoma can cause hypertension, tachycardia, and anxiety, it does not typically present with a testicular mass or directly cause weight loss through a thyroid-like mechanism.
Thyroid diseases (hyper/hypothyroidism) US Medical PG Question 10: A 28-year-old woman comes to the physician because of a 1-year history of intermittent buzzing in both her ears. She says she sometimes has episodes of mild dizziness which resolve spontaneously. She has a 15-year history of type 1 diabetes mellitus and episodes of low back pain. She does not smoke or drink alcohol. Current medications include insulin and aspirin. She works as a trombonist for a symphony orchestra. Her vital signs are within normal limits. On otoscopic examination, the tympanic membrane appears normal. Bone conduction is greater than air conduction in both ears. Weber test shows no lateralization. Which of the following is the most likely diagnosis?
- A. Presbycusis
- B. Diabetic otopathy
- C. Drug-induced ototoxicity
- D. Otosclerosis (Correct Answer)
- E. Endolymphatic hydrops
Thyroid diseases (hyper/hypothyroidism) Explanation: ***Otosclerosis***
- The combination of **conductive hearing loss** (**bone conduction > air conduction**), **intermittent buzzing (tinnitus)**, and mild dizziness in a young adult is characteristic of otosclerosis. The normal tympanic membrane further supports this diagnosis as it indicates no external or middle ear infection/perforation.
- **Weber test shows no lateralization** because the conductive hearing loss is **symmetric and bilateral**, meaning both ears are equally affected.
*Presbycusis*
- This is an age-related **sensorineural hearing loss** that typically affects older individuals, usually over 50-60 years old, not a 28-year-old.
- Presbycusis usually presents with **air conduction > bone conduction** (sensorineural pattern) and affects high frequencies first, not conductive hearing loss.
*Diabetic otopathy*
- While patients with long-standing diabetes can develop hearing loss, it is typically a **sensorineural hearing loss** due to microvascular damage, not conductive hearing loss.
- The symptoms in diabetic otopathy usually involve high-frequency hearing loss and are not typically associated with bone conduction exceeding air conduction.
*Drug-induced ototoxicity*
- **Aspirin** can cause tinnitus and sensorineural hearing loss, but the presented case demonstrates **conductive hearing loss** (bone conduction > air conduction).
- Aspirin ototoxicity typically causes reversible sensorineural hearing loss and tinnitus, not the conductive pattern seen here.
*Endolymphatic hydrops*
- Also known as **Meniere's disease**, this condition causes episodic **vertigo, tinnitus, and sensorineural hearing loss**.
- The hearing loss is typically **sensorineural** and often fluctuating, while this patient presents with signs of **conductive hearing loss**.
More Thyroid diseases (hyper/hypothyroidism) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.