Pituitary disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pituitary disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pituitary disorders US Medical PG Question 1: A 28-year-old woman presents to her primary care physician complaining of intense thirst and frequent urination for the past 2 weeks. She says that she constantly feels the urge to drink water and is also going to the bathroom to urinate frequently throughout the day and multiple times at night. She was most recently hospitalized 1 month prior to presentation following a motor vehicle accident in which she suffered severe impact to her head. The physician obtains laboratory tests, with the results shown below:
Serum:
Na+: 149 mEq/L
Cl-: 103 mEq/L
K+: 3.5 mEq/L
HCO3-: 24 mEq/L
BUN: 20 mg/dL
Glucose: 105 mg/dL
Urine Osm: 250 mOsm/kg
The patient’s condition is most likely caused by inadequate hormone secretion from which of the following locations?
- A. Adrenal cortex
- B. Anterior pituitary
- C. Preoptic nucleus of the hypothalamus
- D. Suprachiasmatic nucleus of the hypothalamus
- E. Posterior pituitary (Correct Answer)
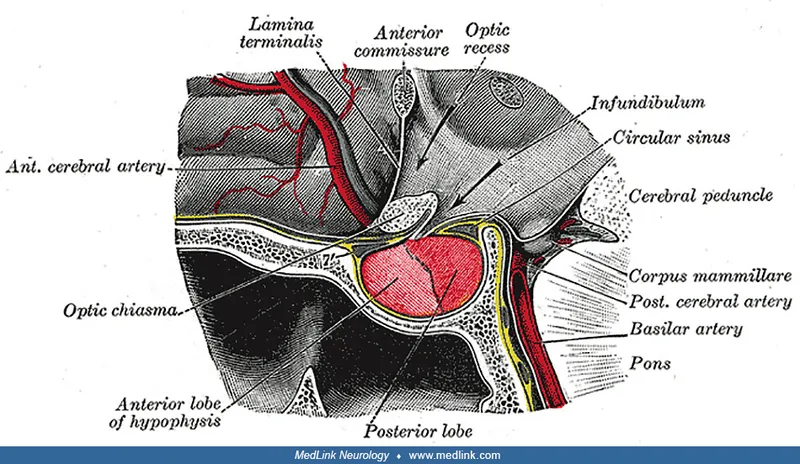
Pituitary disorders Explanation: ***Posterior pituitary***
- The patient's symptoms of **polydipsia** and **polyuria**, coupled with **hypernatremia** and **low urine osmolality**, are classic signs of **diabetes insipidus (DI)**.
- The **posterior pituitary gland** is responsible for releasing **antidiuretic hormone (ADH)**, which, when inadequately secreted (neurogenic DI), leads to these findings. The prior **head trauma** is a common cause of damage to this region.
*Adrenal cortex*
- The adrenal cortex produces **mineralocorticoids** (e.g., **aldosterone**), **glucocorticoids** (e.g., **cortisol**), and **androgens**.
- Deficiencies or excesses of these hormones lead to conditions like **Addison's disease** (adrenal insufficiency) or **Cushing's syndrome**, which have different clinical presentations than those described.
*Anterior pituitary*
- The anterior pituitary produces hormones such as **GH, TSH, ACTH, FSH, LH**, and **prolactin**.
- Dysfunction of the anterior pituitary would lead to a range of hormonal imbalances impacting growth, metabolism, and reproduction, but not directly cause diabetes insipidus.
*Preoptic nucleus of the hypothalamus*
- The **preoptic nucleus** is involved in **thermoregulation**, **sleep**, and **hypothalamic control** of reproduction.
- While part of the hypothalamus, its primary functions do not directly involve ADH synthesis or release, thereby not causing diabetes insipidus.
*Suprachiasmatic nucleus of the hypothalamus*
- The **suprachiasmatic nucleus (SCN)** is the body's primary **circadian rhythm** pacemaker.
- Damage to the SCN would disrupt the sleep-wake cycle and other circadian functions, but would not directly lead to symptoms of diabetes insipidus.
Pituitary disorders US Medical PG Question 2: A 45-year-old woman comes to the physician because of fatigue, irregular menses, and recurrent respiratory infections for the past 6 months. Her blood pressure is 151/82 mm Hg. Physical examination shows a round face, thinning of the skin, and multiple bruises on her arms. Further studies confirm the diagnosis of an ACTH-secreting pituitary adenoma. This patient is at greatest risk for which of the following?
- A. Weight loss
- B. Eosinophilia
- C. Bitemporal hemianopsia
- D. Hypoglycemia
- E. Pathologic fracture (Correct Answer)
Pituitary disorders Explanation: ***Pathologic fracture***
- This patient has **Cushing's disease** due to an **ACTH-secreting pituitary adenoma**, leading to excess cortisol.
- **Excess cortisol** causes **osteoporosis** by increasing bone resorption and decreasing bone formation, significantly raising the risk of **pathologic fractures**.
- This is the **greatest risk** because **all patients** with chronic hypercortisolism develop bone loss, making fractures highly likely.
*Weight loss*
- Patients with Cushing's disease typically experience **weight gain**, particularly centrally (truncal obesity), due to **cortisol-induced fat redistribution**.
- **Fatigue** is common, but weight loss is not a characteristic feature of Cushing's syndrome.
*Eosinophilia*
- **Hypercortisolism** (Cushing's syndrome) usually causes **eosinopenia** (decreased eosinophil count) and **lymphopenia**, not eosinophilia.
- Cortisol has an anti-inflammatory and immunosuppressive effect, leading to a reduction in circulating eosinophils and lymphocytes.
*Bitemporal hemianopsia*
- While an **ACTH-secreting pituitary adenoma** is present, **bitemporal hemianopsia** occurs only when a pituitary tumor becomes a **macroadenoma** (>10mm) and compresses the **optic chiasm**.
- Most ACTH-secreting adenomas are **microadenomas** (<10mm) that cause symptoms through **hormonal excess**, not mass effect.
- The clinical picture here reflects **Cushing's syndrome** from hypercortisolism, which affects **all patients** regardless of tumor size, whereas visual field defects occur only with large tumors.
*Hypoglycemia*
- **Excess cortisol** **increases gluconeogenesis** and **insulin resistance**, leading to **hyperglycemia**, not hypoglycemia.
- This is a common metabolic complication of Cushing's syndrome, often progressing to **steroid-induced diabetes mellitus**.
Pituitary disorders US Medical PG Question 3: Four months after giving birth, a young woman presents to the hospital complaining of lack of breast milk secretion. The patient complains of constantly feeling tired. Physical exam reveals that she is slightly hypotensive and has lost a significant amount of weight since giving birth. The patient states that she has not experienced menstruation since the birth. Which of the following is likely to have contributed to this patient's presentation?
- A. Primary empty sella syndrome
- B. Increased anterior pituitary perfusion
- C. Obstetric hemorrhage (Correct Answer)
- D. Pregnancy-induced decrease in anterior pituitary size
- E. Prolactinoma
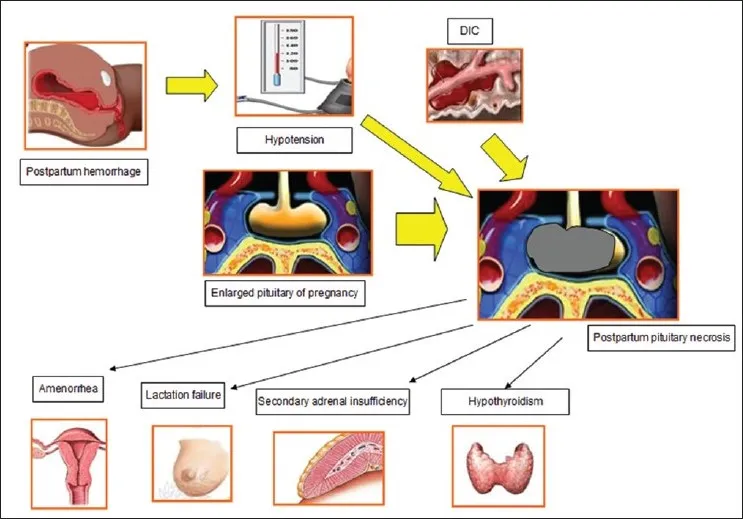
Pituitary disorders Explanation: ***Obstetric hemorrhage***
- This patient's presentation with **lack of breast milk secretion** (agalactia), **fatigue**, **hypotension**, **weight loss**, and **amenorrhea** after childbirth is characteristic of **Sheehan's syndrome**.
- **Sheehan's syndrome** is caused by ischemic necrosis of the pituitary gland due to **massive obstetric hemorrhage** and subsequent hypovolemic shock, which sensitizes the already hypertrophied pituitary gland to ischemia.
*Primary empty sella syndrome*
- This condition involves herniation of the **arachnoid mater** and cerebrospinal fluid into the sella turcica, compressing the pituitary gland, but it is typically not associated with a **postpartum hemorrhage**.
- Symptoms are often non-specific or mild, and while it can cause pituitary dysfunction, the timeline and specific symptoms (e.g., agalactia, profound hypotension) do not align with a post-hemorrhage ischemic event.
*Increased anterior pituitary perfusion*
- **Increased perfusion** would generally lead to a healthier, more functional pituitary gland, rather than one suffering from ischemic damage and subsequent hormone deficiencies.
- The symptoms described are indicative of **insufficient pituitary hormone production**, which would be worsened by decreased or compromised perfusion.
*Pregnancy-induced decrease in anterior pituitary size*
- During pregnancy, the anterior pituitary actually **increases significantly in size** (hypertrophy) due to estrogen stimulation to produce prolactin.
- This **enlarged gland** becomes more vulnerable to ischemia if blood supply is compromised, as seen in Sheehan's syndrome.
*Prolactinoma*
- A **prolactinoma** is a benign tumor that would lead to **excessive prolactin production**, causing **galactorrhea** (inappropriate milk production) rather than a lack of breast milk secretion.
- While it can cause amenorrhea due to inhibition of GnRH, the other symptoms like hypotension, weight loss, and fatigue point to widespread pituitary hormone deficiencies, not isolated prolactin excess.
Pituitary disorders US Medical PG Question 4: A previously healthy 46-year-old man comes to the physician for an 8-month history of headache that is more severe in the mornings. His blood pressure is 151/92 mm Hg. Examination shows enlargement of the nose, forehead, and jaw as well as the hands, fingers, and feet. Ophthalmologic examination shows impaired vision in the outer peripheral fields of both eyes. Laboratory studies show a serum glucose concentration of 225 mg/dL. Which of the following findings is most likely to confirm the diagnosis?
- A. Elevated urine cortisol level
- B. Low serum growth hormone level
- C. Low serum insulin level
- D. Elevated serum insulin-like growth factor-1 level (Correct Answer)
- E. Elevated serum prolactin level
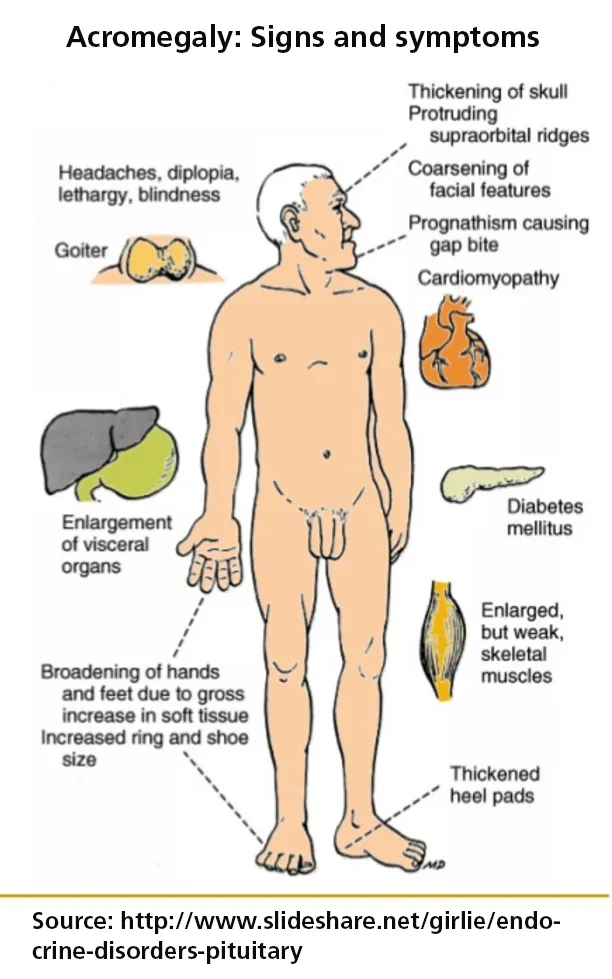
Pituitary disorders Explanation: ***Elevated serum insulin-like growth factor-1 level***
- The patient's symptoms (enlargement of nose, forehead, jaw, hands, and feet; headaches; hypertension; diabetes; bitemporal hemianopsia) are classic for **acromegaly**.
- **Insulin-like growth factor-1 (IGF-1)** is the most reliable screening test for acromegaly because its levels are stable throughout the day and reflect integrated GH secretion; elevated levels significantly confirm the diagnosis.
*Elevated urine cortisol level*
- This would be indicative of **Cushing's syndrome**, which shares some features like hypertension and diabetes, but does not explain the characteristic acral and facial enlargement or the visual field defects.
- The primary diagnostic test for Cushing's is via **cortisol measurement** (e.g., 24-hour urinary free cortisol, late-night salivary cortisol).
*Low serum growth hormone level*
- A **low serum growth hormone (GH) level** would rule out acromegaly, as acromegaly is caused by excessive GH production, typically from a pituitary adenoma.
- While GH levels fluctuate, they are typically high in acromegaly, and a low level would be inconsistent with the clinical picture.
*Low serum insulin level*
- The patient has **diabetes mellitus**, which can be caused by various factors, but a low insulin level is characteristic of **Type 1 diabetes** or late-stage Type 2 diabetes with pancreatic burnout.
- In acromegaly, **insulin resistance** is common due to excess GH, often leading to elevated or normal insulin levels to try and compensate for high glucose.
*Elevated serum prolactin level*
- An elevated serum prolactin level indicates **hyperprolactinemia**, which may coincide with acromegaly if the pituitary adenoma co-secretes prolactin (a mixed tumor) or if the GH-secreting tumor compresses the pituitary stalk.
- However, **prolactin elevation alone** would not explain the acral growth and metabolic abnormalities specific to acromegaly.
Pituitary disorders US Medical PG Question 5: A 34-year-old woman, who had her first child 2 weeks ago, visits her family physician with concerns about constant fatigue and difficulty with breastfeeding. She was discharged from the intensive care unit after hospitalization for severe postpartum hemorrhage. Since then, she has tried multiple pumps and self-stimulation to encourage breast milk production; however, neither of these strategies has worked. Her blood pressure is 88/56 mm Hg and heart rate is 120/min. Which of the following best explains the underlying condition of this patient?
- A. Pituitary infarction (Correct Answer)
- B. Pituitary infection
- C. Pituitary hemorrhage
- D. Pituitary infiltration by histiocytes
- E. Pituitary stalk epithelial tumor
Pituitary disorders Explanation: ***Pituitary infarction***
- The patient's history of **severe postpartum hemorrhage** causing hypovolemic shock, followed by **fatigue**, **difficulty breastfeeding**, **hypotension**, and **tachycardia**, are classic signs of **Sheehan syndrome**, which is caused by ischemic necrosis (infarction) of the pituitary gland.
- The **lactotroph cells** in the anterior pituitary enlarge significantly during pregnancy, making them more vulnerable to ischemia when blood supply is compromised during hemorrhage.
*Pituitary infection*
- **Pituitary infections** (e.g., abscess) are rare and typically present with symptoms of inflammation such as fever, severe headaches, and meningeal signs, which are not described here.
- While an infection could potentially affect pituitary function, it is not the classic presentation following postpartum hemorrhage.
*Pituitary hemorrhage*
- While postpartum hemorrhage is the cause of the pituitary injury, the **pituitary itself is not hemorrhaging** in Sheehan's syndrome; rather, it is undergoing infarction due to global hypoperfusion.
- **Pituitary apoplexy** (hemorrhage into the pituitary) is an acute event with sudden onset of severe headache, visual disturbances, and rapid endocrine dysfunction, typically not related to postpartum hemorrhage directly in this manner.
*Pituitary infiltration by histiocytes*
- **Histiocytic infiltration** can occur in conditions like Langerhans cell histiocytosis or sarcoidosis, affecting pituitary function.
- However, these conditions have distinct clinical features and are not directly linked to a recent history of postpartum hemorrhage as the precipitating event.
*Pituitary stalk epithelial tumor*
- A **pituitary stalk epithelial tumor** would typically cause symptoms due to mass effect or hormonal imbalances, which might include galactorrhea (if prolactin-secreting) or hypopituitarism over time.
- This scenario does not fit the acute onset of symptoms following postpartum hemorrhage, which points to an ischemic event.
Pituitary disorders US Medical PG Question 6: A 9-year-old boy is brought to the physician for evaluation of 2 months of progressive clumsiness, falls, and increased urinary frequency. Physical examination shows bilateral temporal visual field loss. An MRI of the head shows a small calcified suprasellar mass. The patient undergoes surgery with complete removal of the mass. Pathological examination of the specimen shows a lobular tumor composed of cysts filled with oily, brownish-yellow fluid. This mass is most likely derived from which of the following structures?
- A. Arachnoid cells
- B. Ventricular ependyma
- C. Lactotroph cells
- D. Rathke pouch (Correct Answer)
- E. Astroglial cells
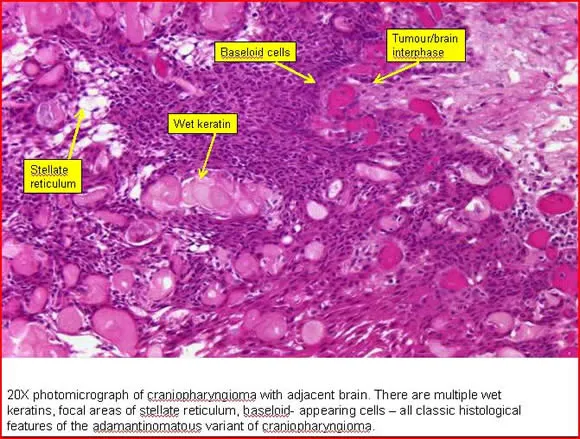
Pituitary disorders Explanation: ***Rathke pouch***
- The combination of **suprasellar mass**, visual field deficits (bitemporal hemianopsia due to optic chiasm compression), **calcification**, and cystic components filled with **oily, brownish-yellow fluid** in a child points strongly to a **craniopharyngioma**.
- **Craniopharyngiomas** are benign tumors derived from remnants of **Rathke's pouch**, which is an embryonic evagination of the stomodeum that gives rise to the anterior pituitary.
*Arachnoid cells*
- Tumors arising from **arachnoid cells** are typically **meningiomas**, which are more common in adults and usually present as dural-based masses, often without significant cystic components.
- While meningiomas can calcify, their characteristic histology (whorled patterns, psammoma bodies) and typical presentation differ from craniopharyngiomas.
*Ventricular ependyma*
- Tumors derived from **ependyma** are **ependymomas**, which typically arise within the ventricles of the brain or spinal cord.
- They are less common in the suprasellar region and their characteristic cystic or fluid content is usually not described as oily and brownish-yellow.
*Lactotroph cells*
- **Lactotroph cells** are found in the **anterior pituitary gland**, and tumors arising from them are **prolactinomas**.
- While prolactinomas can present with visual field defects due to suprasellar extension, they are typically solid pituitary adenomas, rarely calcified, and do not contain oily, brownish-yellow fluid.
*Astroglial cells*
- Tumors originating from **astroglial cells** include **astrocytomas** and **glioblastomas**, which are highly variable in presentation but are typically solid or have pseudocystic areas, not an oily, brownish-yellow fluid-filled cyst.
- While some astrocytomas can calcify, their microscopic appearance and characteristic fluid content are different from what is described.
Pituitary disorders US Medical PG Question 7: A 47-year-old woman complains of weight gain and irregular menses for the past 2 years. She has gained 13 kg (28.6 lb) and feels that most of the weight gain is in her abdomen and face. She has type 2 diabetes and hypertension for 1 year, and they are difficult to control with medications. Vital signs include a temperature of 36.9°C (98.4°F), blood pressure of 160/100 mm Hg, and pulse of 95/min. The patient's late-night salivary cortisol is elevated. Morning plasma ACTH is high. Brain magnetic resonance imaging shows a 2 cm pituitary adenoma. Which of the following is the optimal therapy for this patient?
- A. Unilateral adrenalectomy
- B. Bilateral adrenalectomy
- C. Pituitary radiotherapy
- D. Medical therapy
- E. Transsphenoidal pituitary adenomectomy (Correct Answer)
Pituitary disorders Explanation: ***Transsphenoidal pituitary adenomectomy***
- This patient presents with **Cushing's disease**, characterized by **elevated late-night salivary cortisol** and **high morning plasma ACTH**, coupled with a **pituitary adenoma** on MRI. **Transsphenoidal pituitary adenomectomy** is the first-line and most effective treatment for Cushing's disease, offering the highest chance of remission by directly removing the adenoma.
- Successful surgical removal of the tumor can quickly normalize **ACTH** and **cortisol** levels, leading to significant improvement in symptoms like **weight gain**, **hypertension**, **diabetes**, and **menstrual irregularities**.
*Unilateral adrenalectomy*
- This procedure treats **adrenal adenomas** causing Cushing's syndrome (primary adrenal hypercortisolism), which is characterized by **low or undetectable ACTH levels**. This patient has **high ACTH**, indicating a pituitary source.
- Performing a unilateral adrenalectomy in this case would not address the underlying **pituitary tumor** and would not cure Cushing's disease.
*Bilateral adrenalectomy*
- This is a treatment for severe, refractory Cushing's disease, or as a palliative measure, when **pituitary surgery** has failed or is contraindicated.
- While it effectively removes the source of **cortisol**, it leads to **adrenal insufficiency**, requiring lifelong corticosteroid replacement, and carries the risk of **Nelson's Syndrome** (rapid pituitary tumor growth due to loss of negative feedback).
*Pituitary radiotherapy*
- **Pituitary radiotherapy** is a secondary treatment option, typically used when **transsphenoidal surgery** fails to achieve remission, or if there is residual tumor.
- It has a slower onset of action (months to years) compared to surgery, and the patient's severe symptoms require more immediate control.
*Medical therapy*
- **Medical therapies** (e.g., **ketoconazole**, **mifepristone**, **pasireotide**) are often used as bridging therapy before surgery, when surgery is contraindicated, or for patients with persistent disease after surgery.
- They help control **hypercortisolism** but do not cure the underlying **pituitary adenoma**, making **surgical removal** the preferred definitive treatment.
Pituitary disorders US Medical PG Question 8: A 52-year-old woman presents to her primary care physician complaining of 3 weeks of persistent thirst despite consumption of increased quantities of water. She also admits that she has had increased frequency of urination during the same time period. A basic metabolic panel is performed which reveals mild hypernatremia and a normal glucose level. Urine electrolytes are then obtained which shows a very low urine osmolality that does not correct when a water deprivation test is performed. Blood tests reveal an undetectable level of antidiuretic hormone (ADH). Based on this information, what is the most likely cause of this patient's symptoms?
- A. Diabetes mellitus
- B. Central diabetes insipidus (Correct Answer)
- C. Primary polydipsia
- D. Surreptitious diuretic use
- E. Nephrogenic diabetes insipidus
Pituitary disorders Explanation: ***Central diabetes insipidus***
- The patient presents with **polyuria**, **polydipsia**, **hypernatremia**, and a **low urine osmolality** that does not correct with a **water deprivation test**.
- An **undetectable ADH level** confirms a defect in ADH production or release from the pituitary, which is characteristic of central diabetes insipidus.
*Diabetes mellitus*
- This condition is characterized by **hyperglycemia**, which is ruled out by the **normal glucose level** in the basic metabolic panel.
- While it causes polyuria and polydipsia, the underlying mechanism is **osmotic diuresis due to glucose**, not a defect in ADH or renal response to ADH.
*Primary polydipsia*
- In primary polydipsia, patients consume excessive amounts of water, leading to **dilutional hyponatremia** rather than hypernatremia.
- The **ADH levels would be appropriately suppressed** in a patient with primary polydipsia, not undetectable.
*Surreptitious diuretic use*
- Diuretic use would typically lead to **low blood pressure**, **electrolyte imbalances** (e.g., hypokalemia), and a **high urine sodium concentration**, none of which are explicitly mentioned here.
- It would also not result in an **undetectable ADH level** in the absence of an underlying ADH deficiency.
*Nephrogenic diabetes insipidus*
- This condition involves the **kidneys' inability to respond to ADH**, leading to similar symptoms of polyuria and polydipsia with low urine osmolality.
- However, in nephrogenic diabetes insipidus, the **ADH levels would be high or normal** as the pituitary is producing ADH, but the kidneys are not responding.
Pituitary disorders US Medical PG Question 9: A 48-year-old man is brought to the emergency department by his neighbor, who found him lying unconscious at the door of his house. The patient lives alone and no further history is available. On physical examination, his temperature is 37.2ºC (98.9ºF), pulse rate is 114/min, blood pressure is 116/78 mm Hg, and respiratory rate is 22/min. His Glasgow Coma Scale score is 7 and the patient is intubated. A stat serum osmolality is reported at 260 mmol/kg. Based on the provided information, which of the following conditions is most likely present in this patient?
- A. Syndrome of inappropriate antidiuretic hormone (Correct Answer)
- B. Diabetic ketoacidosis
- C. Acute ethanol intoxication
- D. Central diabetes insipidus
- E. Nonketotic hyperosmolar hyperglycemic coma
Pituitary disorders Explanation: ***Syndrome of inappropriate antidiuretic hormone (SIADH)***
- The patient's **unconsciousness** and Glasgow Coma Scale of 7 suggest significant neurological impairment. A serum osmolality of **260 mmol/kg** is low, indicating **hypotonicity** which is characteristic of SIADH due to excess water retention.
- While other causes of altered consciousness exist, the combination of **hyponatremia** (implied by low osmolality) and neurological symptoms points strongly towards SIADH, especially in an unknown medical history setting where various conditions can trigger ADH release.
*Diabetic ketoacidosis (DKA)*
- DKA typically presents with **hyperglycemia**, **acidosis**, and **ketonuria**, which would result in a high serum osmolality, not the low osmolality seen in this patient.
- While DKA can cause altered mental status, the **serum osmolality of 260 mmol/kg** rules it out as the primary cause here.
*Acute ethanol intoxication*
- Acute ethanol intoxication can cause **unconsciousness** and respiratory depression. However, it usually leads to **mild or no change in serum osmolality**, or occasionally a slightly elevated osmolality due to ethanol itself and associated dehydration, not a significantly low value of 260 mmol/kg.
- The physiological changes associated with pure ethanol intoxication do not typically include the marked **hypotonicity** indicated by such a low serum osmolality.
*Central diabetes insipidus*
- Central diabetes insipidus is characterized by an inability to produce ADH, leading to **polyuria**, **polydipsia**, and frequently **hypernatremia** and **high serum osmolality** due to free water loss.
- It would not cause the **hypotonic state** with a serum osmolality of 260 mmol/kg, making it inconsistent with the clinical picture.
*Nonketotic hyperosmolar hyperglycemic coma (NKHHC)*
- NKHHC is characterized by **extreme hyperglycemia** and **severe dehydration**, leading to a much **higher serum osmolality** (typically >320 mOsm/kg) than observed in this patient.
- Although it causes altered mental status, the reported **low serum osmolality of 260 mmol/kg** makes NKHHC an unlikely diagnosis.
Pituitary disorders US Medical PG Question 10: A 71-year-old male presents to the emergency department after having a generalized tonic-clonic seizure. His son reports that he does not have a history of seizures but has had increasing confusion and weakness over the last several weeks. An electrolyte panel reveals a sodium level of 120 mEq/L and a serum osmolality of 248 mOsm/kg. His urine is found to have a high urine osmolality. His temperature is 37° C (98.6° F), respirations are 15/min, pulse is 67/min, and blood pressure is 122/88 mm Hg. On examination he is disoriented, his pupils are round and reactive to light and accommodation and his mucous membranes are moist. His heart has a regular rhythm without murmurs, his lungs are clear to auscultation bilaterally, the abdomen is soft, and his extremities have no edema but his muscular strength is 3/5 bilaterally. There is hyporeflexia of all four extremities. What is the most likely cause of his symptoms?
- A. Hereditary diabetes insipidus
- B. Sheehan’s syndrome
- C. Syndrome of Inappropriate Antidiuretic Hormone (SIADH) (Correct Answer)
- D. Diabetic ketoacidosis
- E. Lithium use
Pituitary disorders Explanation: ***Syndrome of Inappropriate Antidiuretic Hormone (SIADH)***
- This patient presents with **hypotonic hyponatremia** (serum Na 120 mEq/L, osmolality 248 mOsm/kg) in the setting of a **high urine osmolality**, indicating the kidney is inappropriately concentrating urine despite low plasma osmolality.
- The symptoms of **confusion, weakness, generalized tonic-clonic seizure**, and **hyporeflexia** are consistent with severe hyponatremia affecting neurological function.
*Hereditary diabetes insipidus*
- This condition is characterized by the inability to concentrate urine, leading to **polyuria** and **polydipsia**, and often hypernatremia, which is the opposite of this patient's presentation.
- Patients typically have **low urine osmolality** and high serum osmolality due to excessive water loss.
*Sheehan's syndrome*
- This syndrome is a cause of **hypopituitarism** due to postpartum hemorrhage, leading to deficiencies in various pituitary hormones, including ADH if the posterior pituitary is affected.
- ADH deficiency would lead to **diabetes insipidus-like symptoms** (high serum osmolality, low urine osmolality, polyuria) and not the hyponatremia seen in this patient unless there's profound adrenal insufficiency (cortisol deficiency), but the primary lab findings contradict ADH excess.
*Diabetic ketoacidosis*
- This condition is characterized by **hyperglycemia**, metabolic acidosis, and ketonemia, often leading to polyuria and polydipsia, and can cause **hypernatremia** or pseudohyponatremia.
- The patient's blood pressure, heart rate, and lack of symptoms like Kussmaul respirations or fruity breath do not support DKA, and his sodium is low, not high.
*Lithium use*
- Chronic lithium use can cause **nephrogenic diabetes insipidus** by interfering with ADH action in the renal tubules, leading to an inability to concentrate urine.
- This would result in **polyuria, polydipsia**, and potentially hypernatremia and low urine osmolality, which is inconsistent with the patient's findings of hyponatremia and high urine osmolality.
More Pituitary disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.