Pheochromocytoma and paraganglioma US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pheochromocytoma and paraganglioma. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pheochromocytoma and paraganglioma US Medical PG Question 1: A 27-year-old man comes to the physician because of worsening abdominal pain over the last several months. He has also had recent feelings of sadness and a lack of motivation at work, where he is employed as a computer programmer. He denies suicidal thoughts. He has a history of multiple kidney stones. He has a family history of thyroid cancer in his father and uncle, who both underwent thyroidectomy before age 30. His temperature is 37°C (98°F), blood pressure is 138/86 mm Hg, and pulse is 87/min. Physical examination shows diffuse tenderness over the abdomen and obesity but is otherwise unremarkable. Serum studies show:
Na+ 141 mEq/L
K+ 3.6 mEq/L
Glucose 144 mg/dL
Ca2+ 12.1 mg/dL
Albumin 4.1 g/dL
PTH 226 pg/mL (normal range 12–88 pg/mL)
Results of a RET gene test return abnormal. The physician refers him to an endocrine surgeon. Which of the following is the most appropriate next step in diagnosis?
- A. Thyroidectomy
- B. Urine 5-HIAA
- C. Urine metanephrines (Correct Answer)
- D. Midnight salivary cortisol
- E. Serum gastrin
Pheochromocytoma and paraganglioma Explanation: ***Urine metanephrines***
- The patient's presentation, including **abdominal pain**, **constipation** (implied by pain, mood changes, and high calcium), **hypertension**, **hypercalcemia** with **elevated PTH**, and a family history of **thyroid cancer** with an **abnormal RET gene test**, is highly suggestive of **MEN 2A** (Multiple Endocrine Neoplasia type 2A).
- **MEN 2A** is characterized by **medullary thyroid carcinoma** (MTC), **pheochromocytoma**, and **primary hyperparathyroidism**. Given the strong suspicion of MEN 2A and the presence of hypertension, screening for **pheochromocytoma** with **urine metanephrines** is crucial before any surgical intervention (e.g., thyroidectomy) due to the risk of a hypertensive crisis.
*Thyroidectomy*
- While a **thyroidectomy** is indicated for **medullary thyroid carcinoma** (strongly suggested by the family history of thyroid cancer and abnormal RET gene), it should **not be the immediate next step** before ruling out **pheochromocytoma**.
- Performing a thyroidectomy in a patient with an undiagnosed pheochromocytoma can lead to a **life-threatening hypertensive crisis** during surgery.
*Urine 5-HIAA*
- **Urine 5-HIAA** (5-hydroxyindoleacetic acid) is a test for **carcinoid syndrome**, which presents with flushing, diarrhea, and bronchospasm.
- These symptoms are **not consistent** with the patient's presentation, and carcinoid syndrome is **not a component of MEN 2A**.
*Midnight salivary cortisol*
- **Midnight salivary cortisol** is used to screen for **Cushing's syndrome**, which is characterized by symptoms such as central obesity, moon facies, striae, and muscle weakness.
- While the patient is obese, his other symptoms and laboratory findings are **not suggestive of Cushing's syndrome**, and it is not typically associated with MEN 2A.
*Serum gastrin*
- **Serum gastrin** levels are measured to diagnose **Zollinger-Ellison syndrome**, characterized by severe peptic ulcer disease and diarrhea due to a gastrinoma.
- While gastrinomas can occur in **MEN 1**, they are **not a feature of MEN 2A**, and the patient's symptoms are more consistent with other endocrine dysfunctions.
Pheochromocytoma and paraganglioma US Medical PG Question 2: A previously healthy 61-year-old man comes to the physician because of a 6-month history of morning headaches. He also has fatigue and trouble concentrating on his daily tasks at work. He sleeps for 8 hours every night; his wife reports that he sometimes stops breathing for a few seconds while sleeping. His pulse is 71/min and blood pressure is 158/96 mm Hg. He is 178 cm (5 ft 10 in) tall and weighs 100 kg (220 lb); BMI is 31.6 kg/m2 . Which of the following is the most likely cause of this patient's hypertension?
- A. Proliferation of adrenal chromaffin cells
- B. Overproduction of cortisol
- C. Hypophyseal neoplasm
- D. Nocturnal upper airway obstruction (Correct Answer)
- E. Hypersecretion of aldosterone
Pheochromocytoma and paraganglioma Explanation: ***Nocturnal upper airway obstruction***
- The patient's **obesity (BMI 31.6)**, **morning headaches**, fatigue, difficulty concentrating, and spousal report of **witnessed apneic episodes during sleep** are classic signs of **obstructive sleep apnea (OSA)**.
- OSA causes **intermittent hypoxia and hypercapnia** during sleep, leading to **sympathetic nervous system activation**, increased catecholamine release, and **sustained hypertension** even during waking hours.
- OSA is one of the most common **secondary causes of hypertension**, especially in obese patients.
*Proliferation of adrenal chromaffin cells*
- This describes a **pheochromocytoma**, which typically presents with **paroxysmal hypertension**, severe episodic headaches, palpitations, and diaphoresis (the classic "triad").
- While headaches are present, the **sleep-related breathing disturbances** and obesity are not consistent with pheochromocytoma.
*Overproduction of cortisol*
- This suggests **Cushing's syndrome**, which includes symptoms like central obesity, **moon facies, buffalo hump, purple striae**, muscle weakness, and easy bruising, along with hypertension.
- The patient lacks the classic cushingoid features, and the symptoms are more consistent with sleep-disordered breathing.
*Hypophyseal neoplasm*
- A pituitary tumor could cause hypertension if it leads to conditions like **Cushing's disease** (ACTH-secreting) or **acromegaly** (growth hormone excess).
- However, there are no specific symptoms pointing towards a pituitary tumor (no visual field defects, acromegalic features, or cushingoid appearance), and the prominent **witnessed apneas** fit OSA much better.
*Hypersecretion of aldosterone*
- This is characteristic of **primary hyperaldosteronism (Conn's syndrome)**, which commonly presents with hypertension, often accompanied by **hypokalemia**, muscle weakness, and polyuria.
- The patient's symptoms do not suggest electrolyte abnormalities or other classic signs of mineralocorticoid excess.
Pheochromocytoma and paraganglioma US Medical PG Question 3: A patient presents with periods of severe headaches and flushing however every time they have come to the physician they have not experienced any symptoms. The only abnormal finding is a blood pressure of 175 mmHg/100 mmHg. It is determined that the optimal treatment for this patient is surgical. Prior to surgery which of the following noncompetitive inhibitors should be administered?
- A. Phentolamine
- B. Isoproterenol
- C. Atropine
- D. Propranolol
- E. Phenoxybenzamine (Correct Answer)
Pheochromocytoma and paraganglioma Explanation: ***Phenoxybenzamine***
- This patient likely has a **pheochromocytoma**, which explains the episodic headaches, flushing, and hypertension. **Phenoxybenzamine** is a **non-competitive, irreversible alpha-adrenergic blocker** that is crucial for preoperative preparation to prevent a **hypertensive crisis** during surgery.
- Its **irreversible binding** provides sustained alpha blockade, essential to control blood pressure and avoid catecholamine-induced surges during tumor manipulation.
*Phentolamine*
- **Phentolamine** is a **competitive alpha-adrenergic blocker** used to manage acute hypertensive episodes, but it has a shorter duration of action.
- It is not preferred for sustained preoperative alpha blockade due to its **reversible nature** and potential for drug washout during surgery, which could lead to catecholamine surges.
*Isoproterenol*
- **Isoproterenol** is a **beta-adrenergic agonist** that increases heart rate and contractility, and causes bronchodilation.
- It would be contraindicated in a patient with pheochromocytoma as it could worsen hypertension and cardiac symptoms by stimulating beta receptors that are already overly sensitive to endogenous catecholamines.
*Atropine*
- **Atropine** is a **muscarinic acetylcholine receptor antagonist** that blocks parasympathetic effects, like bradycardia and salivation.
- It has no role in managing hypertension or the catecholamine excess seen in pheochromocytoma.
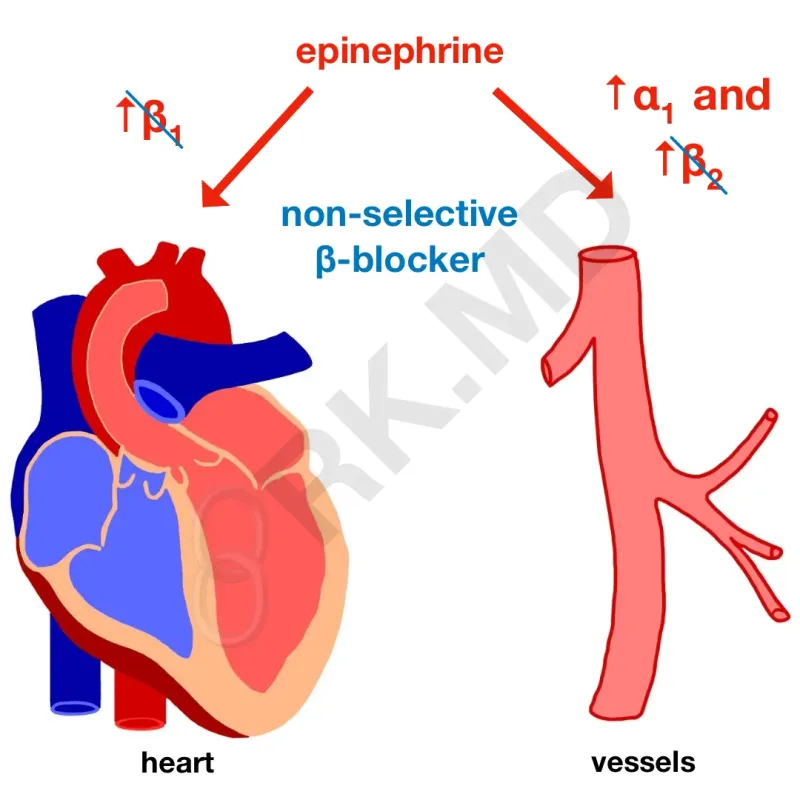
*Propranolol*
- **Propranolol** is a **non-selective beta-adrenergic blocker** that can be used to control tachycardia and arrhythmias in pheochromocytoma, but only *after* adequate alpha-blockade has been established.
- Using **propranolol alone** or before alpha-blockade can lead to **unopposed alpha-adrenergic stimulation**, resulting in a severe, life-threatening hypertensive crisis.
Pheochromocytoma and paraganglioma US Medical PG Question 4: A 30-year-old man comes to the physician for follow-up evaluation for hypertension. He reports a 1-month history of episodic throbbing headaches, palpitations, and paroxysmal sweating. Blood pressure is 160/90 mm Hg. He appears pale but physical examination is otherwise unremarkable. Laboratory studies show elevated urine and plasma metanephrines. A CT scan of the abdomen shows a mass in the left adrenal gland. Which of the following is the most appropriate initial pharmacotherapy for this patient?
- A. Propranolol
- B. Phenoxybenzamine (Correct Answer)
- C. Hydrochlorothiazide
- D. Octreotide
- E. Clonidine
Pheochromocytoma and paraganglioma Explanation: ***Phenoxybenzamine***
- This patient presents with symptoms highly suggestive of a **pheochromocytoma** (episodic throbbing headaches, palpitations, paroxysmal sweating, hypertension), confirmed by **elevated metanephrines** and an **adrenal mass**.
- **Alpha-blockade** with phenoxybenzamine is the initial and crucial step for blood pressure control to prevent a **hypertensive crisis** during surgical tumor removal.
*Propranolol*
- **Beta-blockers** like propranolol should only be administered *after* adequate alpha-blockade has been established.
- Giving a beta-blocker first can lead to **unopposed alpha-adrenergic stimulation**, worsening hypertension and potentially causing a hypertensive crisis.
*Hydrochlorothiazide*
- This is a **thiazide diuretic** used for essential hypertension and is not appropriate for the acute management of a **pheochromocytoma-induced hypertensive crisis**.
- It does not address the underlying catecholamine excess and would be ineffective in preventing a crisis.
*Octreotide*
- **Octreotide** is a somatostatin analog primarily used to treat neuroendocrine tumors like **carcinoid syndrome** or VIPomas.
- It has no role in the management of pheochromocytoma, which arises from chromaffin cells and secretes catecholamines.
*Clonidine*
- **Clonidine** is an **alpha-2 adrenergic agonist** that reduces sympathetic outflow from the central nervous system.
- While it can lower blood pressure, it is not the first-line agent for pheochromocytoma and does not provide the comprehensive, irreversible alpha-blockade needed for surgical preparation.
Pheochromocytoma and paraganglioma US Medical PG Question 5: A 27-year-old man comes to the physician because of a 4-month history of recurrent episodes of headaches, palpitations, and sweating. He was adopted shortly after birth and does not know his biological parents. His pulse is 103/min and blood pressure is 160/105 mm Hg. Physical examination shows multiple soft, yellow papules on the tip of the tongue. There is a 2-cm, firm thyroid nodule. He has long and slender upper extremities, and his elbows and knees can be hyperextended. The most likely cause of this patient's condition is a mutation in which of the following genes?
- A. TSC2
- B. COL5A1
- C. RET (Correct Answer)
- D. MEN1
- E. FBN1
Pheochromocytoma and paraganglioma Explanation: ***Correct Option: RET***
- The patient's symptoms (headaches, palpitations, sweating, hypertension) point to a **pheochromocytoma**, and the thyroid nodule suggests **medullary thyroid carcinoma**. The marfanoid habitus (long, slender extremities, hyperextension) and mucosal neuromas (yellow papules on the tongue) are characteristic features of **Multiple Endocrine Neoplasia type 2B (MEN2B)**.
- **MEN2B** is caused by a germline gain-of-function mutation in the **RET proto-oncogene**, which is involved in cell growth and differentiation.
*Incorrect Option: TSC2*
- Mutations in **TSC2** are associated with **tuberous sclerosis complex**, a neurocutaneous disorder characterized by **facial angiofibromas**, ash-leaf spots, shagreen patches, renal angiomyolipomas, and brain tubers.
- The patient's presentation with pheochromocytoma, medullary thyroid cancer, and marfanoid features is not consistent with tuberous sclerosis.
*Incorrect Option: COL5A1*
- Mutations in **COL5A1** are associated with **Ehlers-Danlos syndrome (classical type)**, which is characterized by **skin hyperextensibility**, joint hypermobility, and tissue fragility.
- While the patient exhibits joint hypermobility, the constellation of pheochromocytoma, medullary thyroid carcinoma, and mucosal neuromas is not a typical feature of Ehlers-Danlos syndrome.
*Incorrect Option: MEN1*
- Mutations in the **MEN1 gene** cause **Multiple Endocrine Neoplasia type 1 (MEN1)**, characterized by tumors of the **parathyroid glands** (leading to hyperparathyroidism), **pituitary gland**, and **pancreatic islet cells**.
- The patient's presentation with medullary thyroid carcinoma and pheochromocytoma, along with mucosal neuromas and marfanoid features, is not consistent with MEN1.
*Incorrect Option: FBN1*
- Mutations in the **FBN1 gene** cause **Marfan syndrome**, characterized by **aortic root dilation**, ectopia lentis, and marfanoid body habitus (long limbs, joint hypermobility).
- While the patient has a marfanoid habitus, the presence of pheochromocytoma, medullary thyroid carcinoma, and mucosal neuromas are not features of Marfan syndrome, differentiating it from MEN2B.
Pheochromocytoma and paraganglioma US Medical PG Question 6: A 21-year-old male college student is very anxious about having thyroid cancer as he found a lump in his neck a few days ago. He has also had diarrhea and a feeling of warmth on his face for 3 days now. His father and uncle both have been diagnosed with thyroid cancer. The lump is about 1 cm in diameter and is fixed and nontender on palpation. Physical examination is otherwise unremarkable. Ultrasound shows a non-cystic cold nodule that requires fine needle aspiration for diagnosis. Thyroid functions tests are normal, and his calcitonin level is 346 ug/ml. Which of the following genetic mutations would warrant thyroidectomy in this patient?
- A. A loss of function of PPARɣ
- B. MEN1 gene mutation
- C. Down expression of the Ras protooncogene
- D. RET gene mutation (Correct Answer)
- E. Activating mutation of the BRAF gene
Pheochromocytoma and paraganglioma Explanation: ***RET gene mutation***
- The patient's symptoms (neck lump, flushing, diarrhea, elevated calcitonin, family history of thyroid cancer) are highly suggestive of **medullary thyroid carcinoma (MTC)**. MTC is strongly associated with **activating germline mutations in the RET proto-oncogene**, which warrant prophylactic thyroidectomy.
- An elevated **calcitonin level** is a key biochemical marker for MTC, and a positive family history, especially with features of MEN 2 syndrome, points towards a germline RET mutation.
*A loss of function of PPARɣ*
- **PPARɣ (Peroxisome Proliferator-Activated Receptor gamma)** loss of function is not directly associated with medullary thyroid carcinoma or the symptoms described.
- Mutations in PPARG are occasionally seen in follicular thyroid carcinoma, but not MTC.
*MEN1 gene mutation*
- **MEN1 gene mutations** are associated with **Multiple Endocrine Neoplasia Type 1 (MEN 1)**, which includes parathyroid hyperplasia, pituitary adenomas, and pancreatic endocrine tumors, but generally **not medullary thyroid carcinoma**.
- While MEN1 can cause endocrine tumors, it does not typically present with the significantly elevated calcitonin or the specific type of thyroid cancer seen in this patient.
*Down expression of the Ras protooncogene*
- **RAS gene mutations** (like HRAS, KRAS, NRAS) are commonly found in **follicular and papillary thyroid carcinomas**, but not in medullary thyroid carcinoma.
- "Down expression" or reduced expression of a proto-oncogene would typically reduce its oncogenic potential, which is less likely to cause a rapidly growing, aggressively presenting tumor like MTC.
*Activating mutation of the BRAF gene*
- **BRAF V600E mutation** is the most common genetic alteration in **papillary thyroid carcinoma (PTC)**. BRAF is a serine/threonine kinase involved in the MAPK signaling pathway.
- While PTC is a common thyroid cancer, the patient's presentation with flushing, diarrhea, and high calcitonin is classic for **medullary thyroid carcinoma**, not papillary thyroid carcinoma.
Pheochromocytoma and paraganglioma US Medical PG Question 7: A 51-year-old African American man with a history of poorly controlled hypertension presents to the emergency room with blurry vision and dyspnea. He reports rapid-onset blurred vision and difficulty breathing 4 hours prior to presentation. He takes lisinopril, hydrochlorothiazide, and spironolactone but has a history of poor medication compliance. He has a 50 pack-year smoking history and drinks 4-6 shots of vodka per day. His temperature is 99.2°F (37.3°C), blood pressure is 195/115 mmHg, pulse is 85/min, and respirations are 20/min. On exam, he is ill-appearing and pale. He is intermittently responsive and oriented to person but not place or time. Fundoscopic examination reveals swelling of the optic disc with blurred margins. A biopsy of this patient’s kidney would most likely reveal which of the following?
- A. Concentrically thickened arteriolar tunica media with abundant nuclei (Correct Answer)
- B. Calcific deposits in the arterial media without luminal narrowing
- C. Fibrous atheromatous plaques in the arterial intima
- D. Anuclear arteriolar thickening
- E. Endothelial proliferation and luminal narrowing with a chronic inflammatory infiltrate
Pheochromocytoma and paraganglioma Explanation: ***Concentrically thickened arteriolar tunica media with abundant nuclei***
- This describes **hyperplastic arteriolosclerosis**, a hallmark of **malignant hypertension**, characterized by severe, rapid-onset blood pressure elevation leading to acute organ damage.
- The patient's **blood pressure of 195/115 mmHg**, **blurry vision** (due to optic disc swelling), and **dyspnea** (suggesting pulmonary edema or cardiac involvement) are classic symptoms of malignant hypertension, which causes "onion-skinning" of arterioles.
*Calcific deposits in the arterial media without luminal narrowing*
- This describes **Mönckeberg arteriolosclerosis**, or medial calcific sclerosis, which involves calcification of the tunica media in muscular arteries.
- It typically occurs in older individuals and is usually **clinically silent** unless complicated by atherosclerosis, and does not cause malignant hypertension.
*Fibrous atheromatous plaques in the arteriolar intima*
- This describes **atherosclerosis**, which involves the formation of plaques in larger arteries, not typically in arterioles, and is a chronic process.
- While the patient has risk factors for atherosclerosis (smoking, hypertension), the acute severe presentation points to a microvascular pathology.
*Anuclear arteriolar thickening*
- This describes **hyaline arteriolosclerosis**, associated with benign (non-malignant) hypertension or diabetes, where plasma proteins leak into the vessel walls, causing uniform, acellular thickening.
- The patient's severe symptoms and optic disc swelling indicate a more aggressive and acute form of vascular damage, not benign hyaline changes.
*Endothelial proliferation and luminal narrowing with a chronic inflammatory infiltrate*
- This pattern is characteristic of **vasculitis** or conditions like **thrombotic microangiopathy**, which can cause luminal narrowing and kidney damage.
- While some features of vasculitis might overlap, the specific context of poorly controlled severe hypertension points more directly to malignant hypertension-induced changes.
Pheochromocytoma and paraganglioma US Medical PG Question 8: A 38-year-old woman with type 1 diabetes for 20 years presents with diabetic ketoacidosis. She is treated and recovers. Six months later, she develops progressive fatigue, nausea, and hyperpigmentation. Laboratory studies show morning cortisol 3 μg/dL, ACTH 180 pg/mL, TSH 8.2 mIU/L, free T4 0.6 ng/dL, and positive anti-thyroid peroxidase antibodies. She also has positive 21-hydroxylase antibodies. Her 12-year-old daughter was recently diagnosed with type 1 diabetes. Evaluate the pathologic process and most critical monitoring recommendation for the daughter.
- A. Multiple endocrine neoplasia syndrome; screen for pheochromocytoma and medullary thyroid cancer
- B. Autoimmune polyglandular syndrome type 2; screen daughter for adrenal antibodies and thyroid function annually (Correct Answer)
- C. Schmidt syndrome with isolated sporatic occurrence; routine diabetes management only for daughter
- D. Autoimmune polyglandular syndrome type 1; screen for mucocutaneous candidiasis and hypoparathyroidism
- E. Secondary endocrine failure from diabetes complications; optimize glycemic control in daughter
Pheochromocytoma and paraganglioma Explanation: ***Autoimmune polyglandular syndrome type 2; screen daughter for adrenal antibodies and thyroid function annually***
- The patient presents with **Schmidt syndrome (APS type 2)**, defined by the triad of **Addison's disease** (low cortisol, high ACTH, 21-hydroxylase antibodies), **type 1 diabetes**, and **autoimmune thyroid disease** (Hashimoto's).
- Because APS-2 is **polygenic** and associated with **HLA-DR3/DR4**, first-degree relatives with one component (like the daughter) require screening for other silent autoimmune conditions to prevent **adrenal crisis**.
*Multiple endocrine neoplasia syndrome; screen for pheochromocytoma and medullary thyroid cancer*
- **MEN syndromes** are characterized by **neoplastic** growths (like medullary thyroid cancer or parathyroid adenomas) rather than the **autoimmune destruction** of glands seen here.
- The absence of hypertension or neck masses and the presence of **autoantibodies** directly contradict a diagnosis of MEN.
*Schmidt syndrome with isolated sporatic occurrence; routine diabetes management only for daughter*
- While the patient does have **Schmidt syndrome**, it is incorrect to label it as purely sporadic because it has a strong **familial clustering** component.
- Managing only diabetes in the daughter is insufficient and dangerous, as it ignores her increased risk for life-threatening **primary adrenal insufficiency**.
*Autoimmune polyglandular syndrome type 1; screen for mucocutaneous candidiasis and hypoparathyroidism*
- **APS-1** typically presents in childhood with the triad of **chronic mucocutaneous candidiasis**, **hypoparathyroidism**, and adrenal failure, which does not match this adult patient’s profile.
- APS-1 is caused by a single gene mutation in **AIRE**, whereas this patient's presentation and family history are classic for the polygenic **APS-2**.
*Secondary endocrine failure from diabetes complications; optimize glycemic control in daughter*
- Diabetic complications lead to **microvascular** or **macrovascular** damage, not the **primary gland failure** (indicated by high ACTH and TSH) seen in this patient.
- **Hyperpigmentation** and the presence of **organ-specific antibodies** (21-hydroxylase) confirm an **autoimmune primary failure**, not a secondary metabolic complication.
Pheochromocytoma and paraganglioma US Medical PG Question 9: A 29-year-old man presents with severe headaches and episodic palpitations, sweating, and anxiety. During an episode, blood pressure is 240/130 mmHg. Between episodes, blood pressure is 135/85 mmHg. 24-hour urine shows metanephrines 4.2 mg (normal: <1.0). MRI reveals a 4 cm right adrenal mass. His brother died suddenly at age 25 from an intracranial hemorrhage, and his father had thyroid cancer. Genetic testing reveals a RET proto-oncogene mutation. Evaluate the pathologic syndrome and preoperative management priority.
- A. MEN 2A with pheochromocytoma; alpha-blockade then beta-blockade before thyroid evaluation and surgery (Correct Answer)
- B. MEN 2A with pheochromocytoma; screen for medullary thyroid cancer before any surgery
- C. Isolated familial pheochromocytoma; genetic counseling after tumor resection
- D. MEN 2B with pheochromocytoma; proceed directly to adrenalectomy for blood pressure control
- E. Von Hippel-Lindau syndrome; screen for CNS hemangioblastomas before surgery
Pheochromocytoma and paraganglioma Explanation: ***MEN 2A with pheochromocytoma; alpha-blockade then beta-blockade before thyroid evaluation and surgery***
- The presence of a **RET proto-oncogene** mutation, family history of thyroid cancer, and a **pheochromocytoma** (elevated metanephrines) confirms **Multiple Endocrine Neoplasia type 2A (MEN 2A)**.
- Medical management must prioritize **alpha-blockade** followed by **beta-blockade** to prevent a lethal **hypertensive crisis** during any subsequent surgical intervention.
*MEN 2A with pheochromocytoma; screen for medullary thyroid cancer before any surgery*
- While screening for **medullary thyroid cancer (MTC)** is necessary in MEN 2A, the immediate clinical priority is stabilizing the patient's blood pressure.
- Performing a thyroid evaluation or surgery before controlling the **catecholamine surge** from the pheochromocytoma carries a high risk of intraoperative mortality.
*Isolated familial pheochromocytoma; genetic counseling after tumor resection*
- This diagnosis is incorrect because the **RET mutation** and family history of thyroid cancer specifically define a **MEN 2 syndrome**, not an isolated condition.
- Genetic counseling and screening of family members are critical, but managing the active **endocrine emergency** takes precedence over post-operative counseling.
*MEN 2B with pheochromocytoma; proceed directly to adrenalectomy for blood pressure control*
- **MEN 2B** is typically characterized by **mucosal neuromas** and a marfanoid habitus, which are not described in this patient.
- Proceeding directly to surgery without **preoperative alpha-blockade** is contraindicated as it can trigger a massive release of catecholamines during tumor manipulation.
*Von Hippel-Lindau syndrome; screen for CNS hemangioblastomas before surgery*
- **Von Hippel-Lindau (VHL)** is associated with the VHL gene mutation on chromosome 3, whereas this patient has a confirmed **RET mutation**.
- While VHL patients do develop pheochromocytomas, the family history of thyroid cancer strongly points toward **MEN 2** rather than VHL.
Pheochromocytoma and paraganglioma US Medical PG Question 10: A 62-year-old man presents with confusion and severe muscle weakness. He recently started treatment for small cell lung cancer. Laboratory studies show sodium 118 mEq/L, serum osmolality 245 mOsm/kg, urine osmolality 520 mOsm/kg, and urine sodium 85 mEq/L. He is clinically euvolemic with blood pressure 125/80 mmHg. Serum cortisol and TSH are normal. Evaluate the pathophysiologic mechanism and most appropriate initial management given the clinical context.
- A. Primary polydipsia with sodium restriction; liberalize sodium intake
- B. Cerebral salt wasting from brain metastases; treat with hypertonic saline
- C. Adrenal insufficiency from lung cancer; administer hydrocortisone
- D. SIADH from ectopic ADH production; restrict fluids and use vaptans (Correct Answer)
- E. Reset osmostat from chemotherapy; observation only
Pheochromocytoma and paraganglioma Explanation: ***SIADH from ectopic ADH production; restrict fluids and use vaptans***
- The patient presents with **hypotonic hyponatremia**, **euvolemia**, and inappropriately **concentrated urine** (>100 mOsm/kg), which are classic hallmarks of **SIADH**.
- **Small cell lung cancer** is a well-known cause of **ectopic ADH production**, leading to water retention and secondary **natriuresis** (elevated urine sodium >40 mEq/L).
*Primary polydipsia with sodium restriction; liberalize sodium intake*
- In primary polydipsia, the **urine osmolality** would be very low (typically <100 mOsm/kg) as the body attempts to excrete excess water.
- This patient's urine osmolality is **520 mOsm/kg**, indicating an inability to dilute urine due to excessive **ADH activity**.
*Cerebral salt wasting from brain metastases; treat with hypertonic saline*
- **Cerebral salt wasting (CSW)** presents with **hypovolemia**, whereas this patient is clinically **euvolemic**.
- CSW typically occurs following **neurosurgery or head trauma**, not as a primary presentation of lung cancer without neurological intervention.
*Adrenal insufficiency from lung cancer; administer hydrocortisone*
- While lung cancer can metastasize to the adrenals, this patient has a **normal serum cortisol**, which effectively rules out **adrenal insufficiency**.
- Adrenal insufficiency would more likely present with **hyperkalemia** and signs of **volume depletion** (hypovolemia).
*Reset osmostat from chemotherapy; observation only*
- **Reset osmostat** is a variant of SIADH where the body regulates sodium at a lower set point, but the **urine osmolality** usually fluctuates with water intake.
- This patient's profound **hyponatremia (118 mEq/L)** and severe symptoms (confusion, weakness) necessitate active management rather than mere **observation**.
More Pheochromocytoma and paraganglioma US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.