Parathyroid disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Parathyroid disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Parathyroid disorders US Medical PG Question 1: A 71-year-old man comes to the emergency department because of a 2-month history of severe muscle cramps and back pain. He says that he is homeless and has not visited a physician in the past 20 years. He is 183 cm (6 ft 0 in) tall and weighs 62 kg (137 lb); BMI is 18.5 kg/m2. His blood pressure is 154/88 mm Hg. Physical examination shows pallor, multiple cutaneous excoriations, and decreased sensation over the lower extremities. Serum studies show:
Calcium 7.2 mg/dL
Phosphorus 5.1 mg/dL
Glucose 221 mg/dL
Creatinine 4.5 mg/dL
An x-ray of the spine shows alternating sclerotic and radiolucent bands in the lumbar and thoracic vertebral bodies. Which of the following is the most likely explanation for these findings?
- A. Primary hypoparathyroidism
- B. Secondary hyperparathyroidism (Correct Answer)
- C. Multiple myeloma
- D. Pseudohypoparathyroidism
- E. Tertiary hyperparathyroidism
Parathyroid disorders Explanation: ***Secondary hyperparathyroidism***
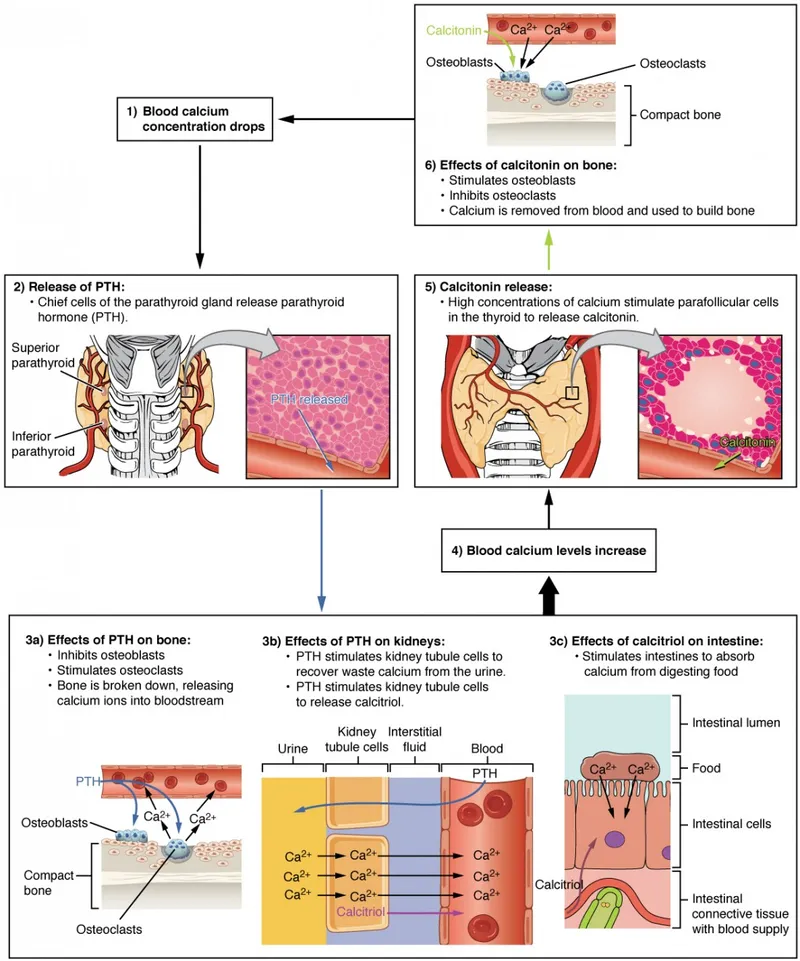
- This patient presents with **hypocalcemia** (7.2 mg/dL) and **hyperphosphatemia** (5.1 mg/dL) in the context of **renal insufficiency** (creatinine 4.5 mg/dL), which are hallmarks of chronic kidney disease (CKD).
- **Secondary hyperparathyroidism** is a common complication of CKD, where the parathyroid glands overproduce PTH in response to low serum calcium and impaired phosphate excretion, leading to characteristic bone changes like **osteomalacia** and **osteitis fibrosa**, which can manifest as alternating sclerotic and radiolucent bands on X-ray (rugger-jersey spine).
*Primary hypoparathyroidism*
- This condition is characterized by **low PTH**, leading to both **hypocalcemia** and **hyperphosphatemia**.
- However, it would not typically present with the severe **renal insufficiency** seen in this patient, and the bone changes would differ.
*Multiple myeloma*
- Multiple myeloma is a plasma cell malignancy that often causes **hypercalcemia** due to bone destruction.
- It would not typically present with **hypocalcemia** and hyperphosphatemia, nor would it cause the specific rugger-jersey spine appearance (alternating sclerotic and radiolucent bands).
*Pseudohypoparathyroidism*
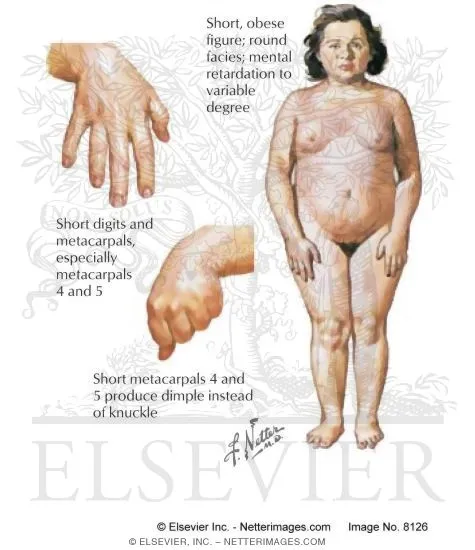
- This is a rare genetic disorder where target tissues are resistant to PTH, resulting in **hypocalcemia** and **hyperphosphatemia** despite **high PTH levels**.
- While it shares some lab findings, it is typically diagnosed in childhood and often associated with specific physical features (e.g., short stature, brachydactyly), which are not mentioned.
*Tertiary hyperparathyroidism*
- This condition develops in patients with long-standing **secondary hyperparathyroidism** where the parathyroid glands become autonomous, leading to **hypercalcemia** and **hyperphosphatemia** or normal phosphate levels.
- The patient's **hypocalcemia** makes tertiary hyperparathyroidism unlikely, as it typically involves elevated calcium levels due to uncontrolled PTH secretion.
Parathyroid disorders US Medical PG Question 2: A 1-year-old boy presents to pediatrics clinic for a well-child visit. He has no complaints. He has a cleft palate and an abnormal facial appearance. He has been riddled with recurrent infections and is followed by cardiology for a ventricular septal defect (VSD). Vital signs are stable, and the patient's physical exam is benign. If this patient's medical history is part of a larger syndrome, what might one also discover that is consistent with the manifestations of this syndrome?
- A. Kidney stones
- B. A positive Chvostek's sign (Correct Answer)
- C. B-cell deficiency
- D. Hypoactive deep tendon reflexes
- E. A shortened QT Interval
Parathyroid disorders Explanation: ***A positive Chvostek's sign***
- The constellation of **cleft palate**, **abnormal facial appearance**, **recurrent infections**, and a **ventricular septal defect (VSD)** strongly suggests **DiGeorge syndrome**.
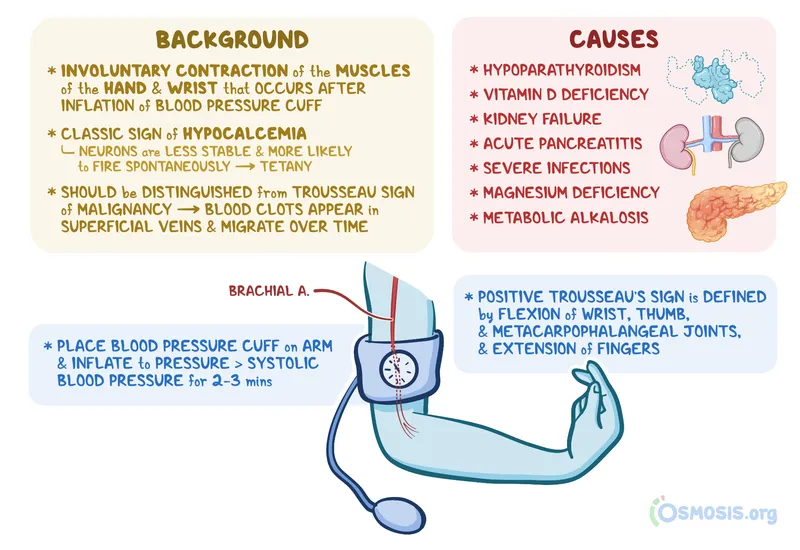
- In DiGeorge syndrome, hypoparathyroidism leads to **hypocalcemia**, which can manifest as neuromuscular irritability, including a positive **Chvostek's sign** (facial muscle twitching upon tapping the facial nerve).
*Kidney stones*
- **Kidney stones** are typically associated with **hypercalcemia** or other metabolic disorders, not hypocalcemia seen in DiGeorge syndrome.
- While DiGeorge patients can have renal anomalies, **nephrolithiasis** is not a characteristic feature of the syndrome.
*B-cell deficiency*
- DiGeorge syndrome is characterized by **T-cell deficiency** due to thymic hypoplasia or aplasia, not primarily B-cell deficiency.
- While **B cells** may be secondarily affected due to lack of T-cell help, the primary immunodeficiency is related to T-lymphocytes.
*Hypoactive deep tendon reflexes*
- **Hypocalcemia** typically causes **hyperactive deep tendon reflexes** and increased neuromuscular excitability, not hypoactivity.
- **Hypoactive reflexes** might suggest conditions like hypothyroidism or certain neurological disorders.
*A shortened QT Interval*
- **Hypocalcemia** is associated with a **prolonged QT interval** on an electrocardiogram, not a shortened one.
- A **shortened QT interval** can occur in conditions like hypercalcemia or genetic channelopathies.
Parathyroid disorders US Medical PG Question 3: A 17-year-old boy comes to the physician for a follow-up examination. Two months ago, he suffered a spinal fracture after a fall from the roof. He feels well. His father has multiple endocrine neoplasia type 1. Vital signs are within normal limits. Examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.7 g/dL
Serum
Creatinine 0.7 mg/dL
Proteins
Total 7.0 g/dL
Albumin 4.1 g/dL
Calcium 11.4 mg/dL
Phosphorus 5.3 mg/dL
Alkaline phosphatase 100 U/L
Which of the following is the most likely cause of these findings?
- A. Immobilization (Correct Answer)
- B. Parathyroid adenoma
- C. Paraneoplastic syndrome
- D. Sarcoidosis
- E. Pseudohypercalcemia
Parathyroid disorders Explanation: ***Immobilization***
- Prolonged **immobilization**, especially after a spinal fracture, leads to **bone resorption**, releasing calcium and phosphorus into the bloodstream, causing **hypercalcemia** and **hyperphosphatemia**.
- Though calcium and phosphorus are elevated, the **alkaline phosphatase** is normal, which is consistent with immobilization-induced bone resorption rather than primary bone disease.
*Parathyroid adenoma*
- A **parathyroid adenoma** causes primary **hyperparathyroidism**, characterized by **hypercalcemia** and **hypophosphatemia** (due to increased renal phosphate excretion), which contradicts the elevated phosphorus level seen here.
- Although the father has MEN1, a personal history of parathyroid adenoma is not indicated by the lab results.
*Paraneoplastic syndrome*
- **Paraneoplastic syndrome** causing hypercalcemia is typically due to ectopic production of **parathyroid hormone-related peptide (PTHrP)**, leading to **hypercalcemia** with **low PTH** and generally **low phosphorus** levels.
- This condition most commonly occurs with malignancies, such as squamous cell carcinoma, which is not indicated in this healthy-appearing young man with a recent fracture.
*Sarcoidosis*
- **Sarcoidosis** causes hypercalcemia due to increased synthesis of **1,25-dihydroxyvitamin D** by activated macrophages, leading to increased intestinal calcium absorption.
- This typically results in **hypercalcemia** with **normal or low PTH** and **normal or low phosphorus** levels; it is not associated with elevated phosphorus.
*Pseudohypercalcemia*
- **Pseudohypercalcemia** is an artifactual elevation of total calcium, usually due to **severe dehydration** or **elevated protein** levels, particularly **albumin** or **immunoglobulins**.
- In this case, the albumin and total protein levels are within the normal range, making pseudohypercalcemia unlikely.
Parathyroid disorders US Medical PG Question 4: A 37-year-old female presents to her primary care physician with constipation and abdominal pain. She notes that the pain has been present for several days and is not related to food. She also reports increased urinary frequency without incontinence, as well as increased thirst. She takes no medications, but notes taking vitamin supplements daily. Her vital signs are: BP 130/72 mmHg, HR 82 bpm, T 97.0 degrees F, and RR 12 bpm. Lab studies reveal: Na 139, K 4.1, Cl 104, HCO3 25, Cr 0.9, and Ca 12.4. Further studies show an increased ionized calcium, decreased PTH, and normal phosphate. What is the most likely cause of this patient's symptoms?
- A. Vitamin overdose (Correct Answer)
- B. Vitamin deficiency
- C. Inherited disorder
- D. Plasma cell neoplasm
- E. Primary endocrine dysfunction
Parathyroid disorders Explanation: ***Vitamin overdose***
- The patient's symptoms of **constipation**, **abdominal pain**, **increased urinary frequency**, and **thirst** are classic signs of **hypercalcemia**.
- The lab findings of **hypercalcemia (Ca 12.4)**, **increased ionized calcium**, **decreased PTH**, and increased phosphate, coupled with a history of daily vitamin supplements, strongly suggest **Vitamin D toxicity** from overdose, which leads to increased calcium absorption and bone resorption.
*Vitamin deficiency*
- Vitamin deficiencies typically do not cause **hypercalcemia**; in fact, severe **Vitamin D deficiency** can lead to **hypocalcemia** and **secondary hyperparathyroidism**.
- Symptoms associated with common vitamin deficiencies (e.g., scurvy, rickets) are not consistent with this patient's presentation.
*Inherited disorder*
- While some **inherited disorders** (e.g., **Familial Hypocalciuric Hypercalcemia**) can cause hypercalcemia, the distinguishing feature is typically a **normal or mildly elevated PTH** and **low urinary calcium excretion**, which is not entirely aligned with the presented PTH and phosphate levels and the acute onset suggested by symptoms.
- The patient's history of **vitamin supplement** use provides a more direct and likely explanation for acute hypercalcemia.
*Plasma cell neoplasm*
- **Plasma cell neoplasms** like **multiple myeloma** can cause **hypercalcemia** due to increased bone resorption from osteoclast-activating factors.
- However, hypercalcemia from these conditions is often accompanied by other signs of malignancy such as **renal failure**, **anemia**, or **bone lesions**, which are not reported in this case, and the **decreased PTH** points away from malignancy-associated humorally mediated hypercalcemia.
*Primary endocrine dysfunction*
- **Primary hyperparathyroidism** is a common cause of **hypercalcemia**, but it is characterized by **elevated or inappropriately normal PTH levels** in the presence of hypercalcemia, which contradicts the **decreased PTH** found in this patient.
- Other endocrine causes of hypercalcemia, such as **thyrotoxicosis** or **adrenal insufficiency**, present with distinct clinical features not described here.
Parathyroid disorders US Medical PG Question 5: A 33-year-old woman presents to her primary care provider for a normal check-up. She reports she has been feeling intermittently fatigued over the past 3 months, but she attributes it to her work as a corporate lawyer and balancing family life. She is otherwise healthy and takes no medications. She was adopted and has no information about her biological family. She has 2 children and has been married for 7 years. She drinks 4-5 glasses of wine per week and does not smoke. Her temperature is 99.2°F (37.3°C), blood pressure is 125/65 mmHg, pulse is 78/min, and respirations are 18/min. On exam, she is well-appearing and in no acute distress. A complete blood count is within normal limits. Additional workup is shown below:
Serum:
Na+: 139 mEq/L
Cl-: 99 mEq/L
K+: 3.9 mEq/L
HCO3-: 23 mEq/L
BUN: 18 mg/dL
Glucose: 110 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 11.1 mg/dL
Parathyroid hormone: 700 pg/mL
Urine:
Na+: 100 mEq/L/24h
Ca2+: 100 mg/24h
Osmolality: 400 mOsmol/kg H2O
Which of the following is the most likely underlying cause of this patient's condition?
- A. Over-secretion of parathyroid hormone
- B. Decreased sensitivity to parathyroid hormone
- C. Gain-of-function mutation in the parathyroid hormone receptor gene
- D. Impaired tubular calcium reabsorption
- E. Loss-of-function mutation in the calcium-sensing receptor (Correct Answer)
Parathyroid disorders Explanation: ***Loss-of-function mutation in the calcium-sensing receptor***
- The patient presents with **hypercalcemia** (Ca2+ 11.1 mg/dL) and **elevated parathyroid hormone (PTH)** (700 pg/mL), which is inappropriate given the high calcium. This combination is highly suggestive of **familial hypocalciuric hypercalcemia (FHH)**.
- FHH is caused by an inactivating mutation in the **calcium-sensing receptor (CaSR)**, leading to a "reset" of the calcium set point. The parathyroid glands and renal tubules perceive normal calcium levels as low, resulting in increased PTH secretion and increased renal tubular calcium reabsorption, despite hypercalcemia.
*Over-secretion of parathyroid hormone*
- While PTH is elevated, simply stating "over-secretion" doesn't explain why this is occurring in the setting of hypercalcemia, which should normally suppress PTH.
- This option would typically describe **primary hyperparathyroidism**, but the urinary calcium excretion in this patient (100 mg/24h) is in the low-normal range for hypercalcemia, making FHH a more likely diagnosis than primary hyperparathyroidism.
*Decreased sensitivity to parathyroid hormone*
- **Decreased sensitivity to PTH** would typically lead to **hypocalcemia** or normal calcium levels, not the hypercalcemia seen in this patient.
- Conditions like **pseudohypoparathyroidism** involve PTH resistance but present with hypocalcemia and hyperphosphatemia.
*Gain-of-function mutation in the parathyroid hormone receptor gene*
- A **gain-of-function mutation** in the PTH receptor would lead to enhanced sensitivity to PTH, causing **hypercalcemia** and **hypophosphatemia**.
- However, the PTH level would typically be **suppressed or low** due to feedback inhibition from hypercalcemia, which is contrary to the elevated PTH seen in this patient.
*Impaired tubular calcium reabsorption*
- **Impaired tubular calcium reabsorption** would lead to **hypercalciuria** (high urinary calcium) and likely normal or low serum calcium as calcium is excessively excreted.
- This patient exhibits relatively **low urinary calcium excretion** (100 mg/24h) despite hypercalcemia, which is characteristic of FHH.
Parathyroid disorders US Medical PG Question 6: A 52-year-old man comes to the physician because of a 4-month history of fatigue, weakness, constipation, decreased appetite, and intermittent flank pain. He takes ibuprofen for knee and shoulder pain. Physical examination shows mild tenderness bilaterally in the costovertebral areas. His serum calcium concentration is 11.2 mg/dL, phosphorus concentration is 2.5 mg/dL, and N-terminal parathyroid hormone concentration is 830 pg/mL. Which of the following steps in vitamin D metabolism is most likely increased in this patient?
- A. Ergocalciferol → 25-hydroxyergocalciferol
- B. 7-dehydrocholesterol → cholecalciferol
- C. 25-hydroxycholecalciferol → 1,25-dihydroxycholecalciferol (Correct Answer)
- D. 25-hydroxycholecalciferol → 24,25-dihydroxycholecalciferol
- E. Cholecalciferol → 25-hydroxycholecalciferol
Parathyroid disorders Explanation: ***25-hydroxycholecalciferol → 1,25-dihydroxycholecalciferol***
- This patient presents with **hypercalcemia** (11.2 mg/dL), **hypophosphatemia** (2.5 mg/dL), and a markedly **elevated N-terminal parathyroid hormone (PTH)** concentration (830 pg/mL), which are classic findings for **primary hyperparathyroidism**.
- In primary hyperparathyroidism, elevated PTH directly stimulates the **renal 1-alpha-hydroxylase enzyme**, increasing the conversion of **25-hydroxycholecalciferol** (calcidiol) to its active form, **1,25-dihydroxycholecalciferol** (calcitriol), which raises calcium levels.
*Ergocalciferol → 25-hydroxyergocalciferol*
- This step involves the **hepatic 25-hydroxylase enzyme** converting dietary vitamin D2 (ergocalciferol) to its storage form, which is not primarily regulated by PTH in the context of hyperparathyroidism.
- While essential for vitamin D activation, this conversion rate is usually adequate and not the primary increased step responsible for the hypercalcemic state in this patient's presentation.
*7-dehydrocholesterol → cholecalciferol*
- This process is the **cutaneous synthesis of vitamin D3 (cholecalciferol)**, which is dependent on UV light exposure and is not directly regulated by PTH.
- This initial step of vitamin D synthesis occurs in the skin and is upstream of the metabolic pathway influenced by PTH.
*25-hydroxycholecalciferol → 24,25-dihydroxycholecalciferol*
- This conversion produces an **inactive form of vitamin D** and is catalyzed by the **24-hydroxylase enzyme**.
- This enzyme activity is typically **suppressed by high PTH** and **increased by high levels of 1,25-dihydroxycholecalciferol**, serving to degrade excess active vitamin D; therefore, this step would likely be decreased, not increased, in primary hyperparathyroidism.
*Cholecalciferol → 25-hydroxycholecalciferol*
- This is the **hepatic 25-hydroxylation** of vitamin D3, producing 25-hydroxycholecalciferol (calcidiol), the major circulating form of vitamin D.
- While critical for producing the substrate for further activation, this step is not the *most likely increased* step in response to high PTH in primary hyperparathyroidism.
Parathyroid disorders US Medical PG Question 7: A 20-year-old woman visits the clinic for her annual physical examination. She does not have any complaints during this visit. The past medical history is insignificant. She follows a healthy lifestyle with a balanced diet and moderate exercise schedule. She does not smoke or drink alcohol. She does not take any medications currently. The family history is significant for her grandfather and uncle who had their parathyroid glands removed. The vital signs include: blood pressure:122/88 mm Hg, pulse 88/min, respirations 17/min, and temperature 36.7°C (98.0°F). The physical exam is within normal limits. The lab test results are as follows:
Blood Urea Nitrogen 12 mg/dL
Serum Creatinine 1.1 mg/dL
Serum Glucose (Random) 88 mg/dL
Serum chloride 107 mmol/L
Serum potassium 4.5 mEq/L
Serum sodium 140 mEq/L
Serum calcium 14.5 mg/dL
Serum albumin 4.4 gm/dL
Parathyroid Hormone (PTH) 70 pg/mL (Normal: 10-65 pg/mL)
24-Hr urinary calcium 85 mg/day (Normal: 100–300 mg/day)
Which of the following is the next best step in the management of this patient?
- A. No treatment is necessary (Correct Answer)
- B. Start IV fluids to keep her hydrated
- C. Start her on pamidronate
- D. Give glucocorticoids
- E. Parathyroidectomy
Parathyroid disorders Explanation: ***No treatment is necessary***
- This patient has **familial hypocalciuric hypercalcemia (FHH)**, a benign autosomal dominant condition caused by inactivating mutations in the calcium-sensing receptor (CaSR).
- The key diagnostic triad is: **elevated serum calcium** (14.5 mg/dL), **mildly elevated or inappropriately normal PTH** (70 pg/mL), and **LOW 24-hour urinary calcium** (<100 mg/day).
- The family history of parathyroid surgery in relatives suggests they may have been misdiagnosed with primary hyperparathyroidism.
- **FHH is a benign condition that requires no treatment**. Patients are typically asymptomatic and do not develop complications of hypercalcemia.
- The calcium-creatinine clearance ratio (CCCR) is typically <0.01 in FHH, which helps distinguish it from primary hyperparathyroidism (CCCR >0.02).
*Parathyroidectomy*
- **Parathyroidectomy is contraindicated in FHH** and is a common error in management.
- Surgery does not correct the hypercalcemia in FHH because the defect is in the calcium-sensing receptor throughout the body, not in the parathyroid glands.
- Parathyroidectomy can lead to **permanent hypoparathyroidism** without resolving the underlying condition.
- Surgery is indicated for **primary hyperparathyroidism**, which differs from FHH by having normal or elevated urinary calcium excretion.
*Start IV fluids to keep her hydrated*
- IV fluids are used for **acute symptomatic hypercalcemia** or hypercalcemic crisis.
- This patient is **asymptomatic** with stable vital signs and does not require acute intervention.
- Fluids do not address the underlying pathophysiology of FHH and are unnecessary in this benign condition.
*Start her on pamidronate*
- Bisphosphonates like pamidronate are used for **hypercalcemia of malignancy** or severe symptomatic primary hyperparathyroidism.
- They are **ineffective in FHH** because the hypercalcemia is due to altered calcium sensing, not increased bone resorption.
- Pamidronate is not indicated for chronic management of asymptomatic hypercalcemia due to FHH.
*Give glucocorticoids*
- Glucocorticoids treat hypercalcemia from **granulomatous diseases** (sarcoidosis), **vitamin D intoxication**, or **hematologic malignancies** (lymphoma, multiple myeloma).
- They work by decreasing intestinal calcium absorption and are ineffective in FHH.
- This patient's clinical presentation and laboratory findings do not suggest any of these conditions.
Parathyroid disorders US Medical PG Question 8: A 28-year-old man comes to the physician for a follow-up examination after a previous visit showed an elevated serum calcium level. He has a history of bipolar disorder. His mother had a parathyroidectomy in her 30s. The patient does not drink alcohol or smoke. Current medications include lithium and a daily multivitamin. His vital signs are within normal limits. Physical examination shows no abnormalities. Laboratory studies show:
Serum
Sodium 146 mEq/L
Potassium 3.7 mEq/L
Calcium 11.2 mg/dL
Magnesium 2.3 mEq/L
PTH 610 pg/mL
Albumin 4.2 g/dL
24-hour urine
Calcium 23 mg
Which of the following is the most likely cause of this patient’s findings?
- A. Lithium toxicity
- B. Parathyroid adenoma
- C. Excess calcium intake
- D. Excess vitamin D intake
- E. Abnormal calcium sensing receptors (Correct Answer)
Parathyroid disorders Explanation: ***Abnormal calcium sensing receptors***
- The patient's **hypocalciuric hypercalcemia** (high serum calcium, low urine calcium) in the presence of an **elevated PTH** suggests a defect in calcium sensing.
- The family history of parathyroidectomy in the mother is consistent with an inherited condition affecting **calcium-sensing receptors (CaSRs)**, such as **familial hypocalciuric hypercalcemia (FHH)**.
*Lithium toxicity*
- **Lithium** can cause hypercalcemia by increasing the set point for calcium at the parathyroid gland, leading to increased PTH secretion.
- However, lithium typically does not lead to **hypocalciuria** to the extent seen in FHH, as it does not directly affect the kidney's CaSR in the same manner.
*Parathyroid adenoma*
- A **parathyroid adenoma** would cause **primary hyperparathyroidism**, characterized by hypercalcemia and elevated PTH.
- However, primary hyperparathyroidism typically presents with **hypercalciuria** due to the PTH-mediated increase in renal calcium reabsorption being overwhelmed by the increased filtered calcium load, unlike the hypocalciuria seen here.
*Excess calcium intake*
- **Excess calcium intake** could lead to hypercalcemia, but this would typically suppress PTH (unless it's a milk-alkali syndrome variant).
- It would also lead to **hypercalciuria** as the kidneys attempt to excrete the excess calcium, which is not observed here with a suppressed 24-hour urine calcium.
*Excess vitamin D intake*
- **Excess vitamin D intake** causes hypercalcemia by increasing intestinal calcium absorption and bone resorption, and would typically lead to **suppressed PTH** levels.
- It would also typically result in **hypercalciuria** due to the increased filtered calcium load, contrasting with the low urine calcium in this patient.
Parathyroid disorders US Medical PG Question 9: A 36-year-old man is admitted to the hospital because of a 1-day history of epigastric pain and vomiting. He has had similar episodes of epigastric pain in the past. He drinks 8 oz of vodka daily. Five days after admission, the patient develops aspiration pneumonia and sepsis. Despite appropriate therapy, the patient dies. At autopsy, the pancreas appears gray, enlarged, and nodular. Microscopic examination of the pancreas shows localized deposits of calcium. This finding is most similar to an adaptive change that can occur in which of the following conditions?
- A. Primary hyperparathyroidism
- B. Sarcoidosis
- C. Multiple myeloma
- D. Congenital CMV infection
- E. Chronic kidney disease (Correct Answer)
Parathyroid disorders Explanation: ***Chronic kidney disease***
- The pancreatic finding represents **dystrophic calcification** (calcium deposition in damaged tissue with normal serum calcium levels), a consequence of chronic pancreatitis.
- **Chronic kidney disease** is the most similar condition because it also involves pathologic calcification as an adaptive/pathologic change, though through a different mechanism called **metastatic calcification**.
- In CKD, **hyperphosphatemia** and secondary **hyperparathyroidism** elevate the serum calcium-phosphate product, leading to calcium deposition in **normal tissues** (blood vessels, kidneys, lungs, gastric mucosa).
- Both conditions demonstrate **pathologic calcification as a tissue response** to metabolic derangement, making CKD the best answer among the options provided.
*Primary hyperparathyroidism*
- Causes **hypercalcemia** and **hypophosphatemia** due to excess PTH secretion.
- Can lead to **metastatic calcification** in normal tissues, but is less commonly associated with widespread tissue calcification compared to CKD.
- The mineral imbalance pattern differs from CKD (high calcium, low phosphate vs. high phosphate, variable calcium).
*Sarcoidosis*
- Causes **hypercalcemia** due to increased 1,25-dihydroxyvitamin D production by activated macrophages in granulomas.
- Can result in **metastatic calcification**, particularly nephrocalcinosis.
- However, this is less common and less extensive than the calcification seen in CKD.
*Multiple myeloma*
- Produces **hypercalcemia** through osteolytic bone destruction and cytokine-mediated bone resorption.
- Can theoretically cause **metastatic calcification**, but this is not a typical or prominent feature of the disease.
- The hypercalcemia is usually addressed before significant tissue calcification occurs.
*Congenital CMV infection*
- Causes **dystrophic calcification** in damaged tissues, typically **periventricular intracranial calcifications**.
- While this involves the same type of calcification (dystrophic), CMV infection is not characterized by systemic or progressive calcification as an adaptive metabolic response.
- The calcifications are focal sequelae of viral tissue damage, not a widespread metabolic derangement.
Parathyroid disorders US Medical PG Question 10: A 21-year-old male college student is very anxious about having thyroid cancer as he found a lump in his neck a few days ago. He has also had diarrhea and a feeling of warmth on his face for 3 days now. His father and uncle both have been diagnosed with thyroid cancer. The lump is about 1 cm in diameter and is fixed and nontender on palpation. Physical examination is otherwise unremarkable. Ultrasound shows a non-cystic cold nodule that requires fine needle aspiration for diagnosis. Thyroid functions tests are normal, and his calcitonin level is 346 ug/ml. Which of the following genetic mutations would warrant thyroidectomy in this patient?
- A. A loss of function of PPARɣ
- B. MEN1 gene mutation
- C. Down expression of the Ras protooncogene
- D. RET gene mutation (Correct Answer)
- E. Activating mutation of the BRAF gene
Parathyroid disorders Explanation: ***RET gene mutation***
- The patient's symptoms (neck lump, flushing, diarrhea, elevated calcitonin, family history of thyroid cancer) are highly suggestive of **medullary thyroid carcinoma (MTC)**. MTC is strongly associated with **activating germline mutations in the RET proto-oncogene**, which warrant prophylactic thyroidectomy.
- An elevated **calcitonin level** is a key biochemical marker for MTC, and a positive family history, especially with features of MEN 2 syndrome, points towards a germline RET mutation.
*A loss of function of PPARɣ*
- **PPARɣ (Peroxisome Proliferator-Activated Receptor gamma)** loss of function is not directly associated with medullary thyroid carcinoma or the symptoms described.
- Mutations in PPARG are occasionally seen in follicular thyroid carcinoma, but not MTC.
*MEN1 gene mutation*
- **MEN1 gene mutations** are associated with **Multiple Endocrine Neoplasia Type 1 (MEN 1)**, which includes parathyroid hyperplasia, pituitary adenomas, and pancreatic endocrine tumors, but generally **not medullary thyroid carcinoma**.
- While MEN1 can cause endocrine tumors, it does not typically present with the significantly elevated calcitonin or the specific type of thyroid cancer seen in this patient.
*Down expression of the Ras protooncogene*
- **RAS gene mutations** (like HRAS, KRAS, NRAS) are commonly found in **follicular and papillary thyroid carcinomas**, but not in medullary thyroid carcinoma.
- "Down expression" or reduced expression of a proto-oncogene would typically reduce its oncogenic potential, which is less likely to cause a rapidly growing, aggressively presenting tumor like MTC.
*Activating mutation of the BRAF gene*
- **BRAF V600E mutation** is the most common genetic alteration in **papillary thyroid carcinoma (PTC)**. BRAF is a serine/threonine kinase involved in the MAPK signaling pathway.
- While PTC is a common thyroid cancer, the patient's presentation with flushing, diarrhea, and high calcitonin is classic for **medullary thyroid carcinoma**, not papillary thyroid carcinoma.
More Parathyroid disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.