Endocrine effects of non-endocrine tumors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Endocrine effects of non-endocrine tumors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Endocrine effects of non-endocrine tumors US Medical PG Question 1: A 61-year-old man presents to the urgent care clinic complaining of cough and unintentional weight loss over the past 3 months. He works as a computer engineer, and he informs you that he has been having to meet several deadlines recently and has been under significant stress. His medical history is significant for gout, hypertension, hypercholesterolemia, diabetes mellitus type 2, and pulmonary histoplasmosis 10 years ago. He currently smokes 2 packs of cigarettes/day, drinks a 6-pack of beer/day, and he endorses a past history of cocaine use back in the early 2000s but currently denies any drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 87/min, and respiratory rate 18/min. His physical examination shows minimal bibasilar rales, but otherwise clear lungs on auscultation, grade 2/6 holosystolic murmur, and a benign abdominal physical examination. However, on routine lab testing, you notice that his sodium is 127 mEq/L. His chest X-ray is shown in the picture. Which of the following is the most likely underlying diagnosis?
- A. Large cell lung cancer
- B. Squamous cell carcinoma
- C. Non-small cell lung cancer
- D. Adenocarcinoma
- E. Small cell lung cancer (Correct Answer)
Endocrine effects of non-endocrine tumors Explanation: ***Small cell lung cancer***
- The patient's presentation with **cough**, **unintentional weight loss**, **hyponatremia (Na 127 mEq/L)**, and a significant smoking history (2 packs/day) are highly suggestive of **small cell lung cancer (SCLC)**.
- SCLC is **strongly associated with paraneoplastic syndromes**, particularly **syndrome of inappropriate antidiuretic hormone secretion (SIADH)**, which causes **euvolemic hyponatremia** - the key diagnostic clue in this case.
- The chest x-ray findings would typically show a **central mass** with **mediastinal widening**, characteristic of SCLC.
- SCLC accounts for approximately 15% of lung cancers but has the strongest association with paraneoplastic SIADH.
*Large cell lung cancer*
- While strongly associated with smoking, **large cell carcinoma** more commonly presents as a **peripheral mass** and is **less frequently associated with paraneoplastic syndromes like SIADH**.
- It's a diagnosis of exclusion and less likely to cause prominent hyponatremia compared to SCLC.
*Squamous cell carcinoma*
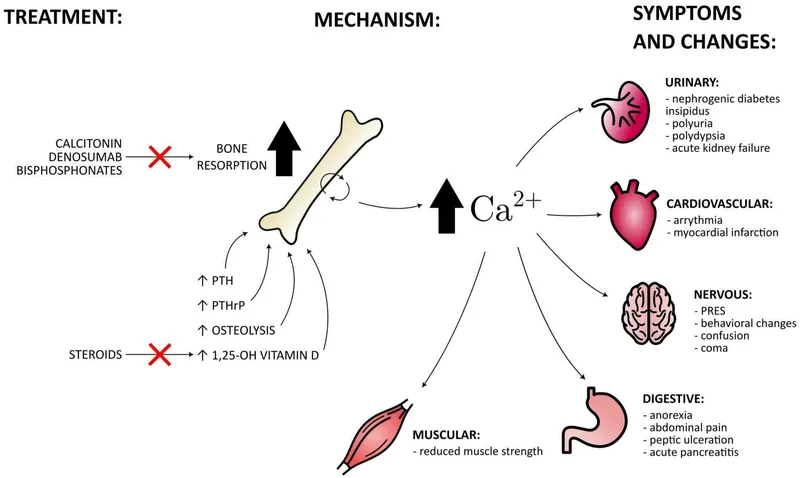
- **Squamous cell carcinoma** often presents with **hemoptysis** and can cause **hypercalcemia** (not hyponatremia) due to paraneoplastic **PTHrP secretion**.
- While it's centrally located and linked to smoking, **hyponatremia from SIADH is much less common** than in SCLC.
*Non-small cell lung cancer*
- This is a broad category that includes adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. While specific types within NSCLC can cause various symptoms, the highly characteristic presentation of **cough, weight loss, and hyponatremia (suggesting SIADH)** in a heavy smoker points more specifically to SCLC.
- This option is too general; the clinical picture allows for a more specific diagnosis.
*Adenocarcinoma*
- **Adenocarcinoma** is typically a **peripheral lung cancer** and is the most common type in non-smokers, though it can occur in smokers.
- It is **less commonly associated with paraneoplastic hyponatremia (SIADH)** compared to small cell lung cancer.
- Would not typically present with the prominent hyponatremia seen in this patient.
Endocrine effects of non-endocrine tumors US Medical PG Question 2: A 54-year-old man comes to the emergency department because of abdominal distension for the past 3 weeks. He also complains of generalized abdominal discomfort associated with nausea and decreased appetite. He was discharged from the hospital 3 months ago after an inguinal hernia repair with no reported complications. He has a history of type 2 diabetes mellitus, congestive heart failure, and untreated hepatitis C. His current medications include aspirin, atorvastatin, metoprolol, lisinopril, and metformin. His father has a history of alcoholic liver disease. He has smoked one pack of cigarettes daily for 30 years but quit 5 years ago. He drinks 3–4 beers daily. He appears cachectic. His vital signs are within normal limits. Examination shows a distended abdomen and shifting dullness. There is no abdominal tenderness or palpable masses. There is a well-healed surgical scar in the right lower quadrant. Examination of the heart and lung shows no abnormalities. He has 1+ bilateral lower extremity nonpitting edema. Diagnostic paracentesis is performed. Laboratory studies show:
Hemoglobin 10 g/dL
Leukocyte count 14,000/mm3
Platelet count 152,000/mm3
Serum
Total protein 5.8 g/dL
Albumin 3.5 g/dL
AST 18 U/L
ALT 19 U/L
Total bilirubin 0.8 mg/dL
HbA1c 8.1%
Peritoneal fluid analysis
Color Cloudy
Cell count 550/mm3 with lymphocytic predominance
Total protein 3.5 g/dL
Albumin 2.6 g/dL
Glucose 60 mg/dL
Triglycerides 360 mg/dL
Peritoneal fluid Gram stain is negative. Culture and cytology results are pending. Which of the following is the most likely cause of this patient's symptoms?
- A. Lymphoma (Correct Answer)
- B. Acute decompensated heart failure
- C. Infection with gram-positive bacteria
- D. Recent surgery
- E. Nephrotic syndrome
Endocrine effects of non-endocrine tumors Explanation: ***Lymphoma***
- This patient has **chylous ascites**, evidenced by peritoneal fluid **triglycerides >200 mg/dL (360 mg/dL)**, **lymphocytic predominance**, and **cloudy appearance** from chylomicrons.
- Chylous ascites results from lymphatic obstruction or leakage, most commonly due to **malignancy (especially lymphoma)**, trauma, or cirrhosis with lymphatic dysfunction.
- The **cachexia**, **low SAAG (0.9 g/dL)**, and systemic signs support an underlying **malignancy causing lymphatic obstruction** rather than portal hypertension alone.
- Hepatitis C is a risk factor for lymphoma, and the clinical picture (weight loss, ascites without typical stigmata of advanced cirrhosis, lymphocytic fluid) points toward lymphoma as the underlying cause.
*Acute decompensated heart failure*
- While this patient has a history of CHF, his **vital signs are normal** and **cardiac exam shows no abnormalities**.
- Heart failure causes **transudative ascites with high SAAG (>1.1 g/dL)**, not the low SAAG (0.9 g/dL) and chylous characteristics seen here.
- The markedly **elevated triglycerides and lymphocytic predominance** are not features of cardiac ascites.
*Infection with gram-positive bacteria*
- **Gram stain is negative**, and bacterial peritonitis typically presents with **neutrophilic predominance** (PMN >250/mm³), not lymphocytic.
- The elevated triglycerides and chronic presentation over 3 weeks are inconsistent with acute bacterial peritonitis.
- This represents a chronic lymphatic process rather than acute infection.
*Recent surgery*
- The inguinal hernia repair was **3 months ago with no complications**.
- Post-surgical complications would present much sooner and would not cause chylous ascites with this fluid profile.
- The lymphatic obstruction pattern and systemic features suggest an unrelated systemic process.
*Nephrotic syndrome*
- Nephrotic syndrome requires **severe hypoalbuminemia (<2.5 g/dL)** to cause ascites.
- This patient's serum albumin is **3.5 g/dL**, insufficient to cause significant third-spacing.
- Nephrotic syndrome does not cause **elevated peritoneal triglycerides** or the lymphatic obstruction pattern seen here.
Endocrine effects of non-endocrine tumors US Medical PG Question 3: A 70-year-old male is brought to the emergency department from a nursing home due to worsening mental status. His nurse reports that the patient has been very lethargic and sleeping more than usual for the past week. She found him confused and difficult to arouse this morning and decided to bring him to the ER. His past medical history is significant for small cell carcinoma of the lung for which he is receiving chemotherapy. He is also on lithium and bupropion for bipolar disorder. Other medications include metoprolol, valsartan, metformin, and insulin. On admission, blood pressure is 130/70 mm Hg, pulse rate is 100/min, respiratory rate is 17/min, and temperature is 36.5°C (97.7°F). He is drowsy and disoriented. Physical examination is normal. Finger-stick glucose level is 110 mg/dL. Other laboratory studies show:
Na+ 120 mEq/L (136—145 mEq/L)
K+ 3.5 mEq/L (3.5—5.0 mEq/L)
Cl- 107 mEq/L (95—105 mEq/L)
Creatinine 0.8 mg/dL (0.6—1.2 mg/dL)
Serum osmolality 250 mOsm/kg (275—295 mOsm/kg)
Urine Na+ 70 mEq/L
Urine osmolality 340 mOsm/kg
He is admitted to the hospital for further management. Which of the following is the most likely cause of this patient's condition?
- A. Psychogenic polydipsia
- B. Lithium
- C. Infection
- D. Carcinoma (Correct Answer)
- E. Bupropion
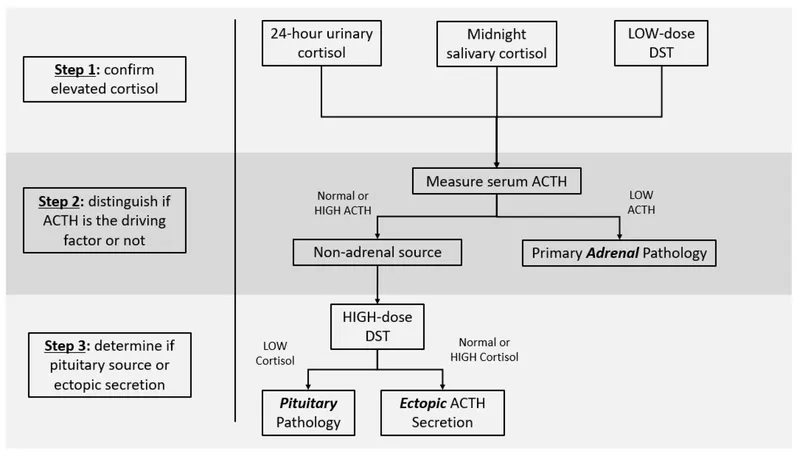
Endocrine effects of non-endocrine tumors Explanation: ***Carcinoma***
- This patient's **small cell lung carcinoma** is the most likely cause of his presentation, as it is one of the **most common causes of paraneoplastic SIADH**.
- The laboratory findings are **classic for SIADH**: euvolemic hyponatremia (Na+ 120 mEq/L), low serum osmolality (250 mOsm/kg), inappropriately concentrated urine (urine osmolality 340 mOsm/kg), and elevated urine sodium (70 mEq/L).
- The **altered mental status** (lethargy, confusion) is consistent with severe hyponatremia.
- Small cell lung cancer accounts for approximately **15% of all SIADH cases** and should always be considered in this clinical context.
*Psychogenic polydipsia*
- While excessive water intake can cause hyponatremia, it typically presents with **very dilute urine** (low urine osmolality <100 mOsm/kg) and **low urine sodium** (<20 mEq/L).
- This patient has **concentrated urine** (340 mOsm/kg) and **elevated urine sodium** (70 mEq/L), which are inconsistent with psychogenic polydipsia.
*Lithium*
- Lithium toxicity can cause neurological symptoms but typically causes **nephrogenic diabetes insipidus**, leading to **hypernatremia** or normal sodium levels, not hyponatremia.
- Lithium-induced SIADH is exceedingly rare and would not be the most likely diagnosis in a patient with known small cell lung cancer.
- The patient's creatinine is normal (0.8 mg/dL), making significant lithium toxicity less likely.
*Infection*
- Infections (particularly pneumonia, meningitis, or CNS infections) can cause SIADH and altered mental status.
- However, this patient has **no fever** (temperature 36.5°C), and there are no other signs suggesting active infection.
- The **direct paraneoplastic association** between small cell lung cancer and SIADH makes carcinoma the more likely primary cause.
*Bupropion*
- Bupropion has been rarely associated with SIADH in case reports, but this is an **uncommon adverse effect**.
- Given the patient's **well-established risk factor** (small cell lung carcinoma) for SIADH, the malignancy is a far more likely cause than medication effect.
Endocrine effects of non-endocrine tumors US Medical PG Question 4: A 75-year-old gentleman is brought to the ED with confusion that started earlier this morning. His family notes that he was complaining of feeling weak last night and also had a slight tremor at the time. He is afebrile and he has no known chronic medical conditions. Physical exam reveals a cooperative but confused gentleman. His mucous membranes are moist, he has no focal neurological deficits, and his skin turgor is within normal limits. His lab results are notable for:
Serum Na+: 123 mEq/L
Plasma osmolality: 268 mOsm/kg
Urine osmolality: 349 mOsm/kg
Urine Na+: 47 mEq/L
Which of the following malignancies is most likely to be responsible for this patient's presentation?
- A. Gastric adenocarcinoma
- B. Small cell lung cancer (Correct Answer)
- C. Esophageal squamous cell carcinoma
- D. Non-seminomatous germ cell tumor
- E. Rib osteosarcoma
Endocrine effects of non-endocrine tumors Explanation: ***Small cell lung cancer***
- This patient's laboratory values (hyponatremia, low plasma osmolality, and inappropriately high urine osmolality with elevated urine sodium) are classic for the **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- **Small cell lung cancer** is the most common malignancy associated with paraneoplastic SIADH due to its ability to ectopically produce ADH.
*Gastric adenocarcinoma*
- While gastric adenocarcinomas can cause paraneoplastic syndromes, SIADH is an **uncommon** paraneoplastic manifestation of this type of cancer.
- Other paraneoplastic syndromes, such as **Trousseau's syndrome** (migratory thrombophlebitis), are more classically associated with gastric adenocarcinoma.
*Esophageal squamous cell carcinoma*
- Esophageal cancer, including squamous cell carcinoma, is **rarely associated** with SIADH.
- Its paraneoplastic manifestations are less defined and not prominent for ADH production.
*Non-seminomatous germ cell tumor*
- Germ cell tumors, particularly non-seminomatous types, are more commonly associated with paraneoplastic syndromes involving **human chorionic gonadotropin (hCG)** or **alpha-fetoprotein (AFP)** production.
- While some germ cell tumors *can* release ADH, it is **not a primary cause** of SIADH compared to small cell lung cancer.
*Rib osteosarcoma*
- Osteosarcoma is a primary bone tumor and is **not typically associated** with paraneoplastic syndromes like SIADH.
- Its primary clinical manifestations are related to local bone destruction and metastasis.
Endocrine effects of non-endocrine tumors US Medical PG Question 5: A 65-year-old man comes to the physician for evaluation of a neck mass and weight loss. He first noticed the growing mass 2 months ago. The mass is not painful. He also has decreased appetite and intermittent abdominal pain. He has lost 10 kg (22 lb) of weight over the past 3 months. Sometimes, he wakes up in the morning drenched in sweat. He takes daily over-the-counter multivitamins. He appears pale. His pulse is 65/min, blood pressure is 110/70 mm Hg, and temperature is 38.1°C (100.6°F). Physical exam shows a painless, golf ball-sized mass in the anterior triangle of the neck. A biopsy shows large cells with a bilobed nucleus that are CD15-positive and CD30-positive. Laboratory analysis of serum shows a calcium level of 14.5 mg/dL and a parathyroid hormone level of 40 pg/mL. Which of the following is the most likely explanation of this patient's laboratory findings?
- A. Ectopic vitamin D production
- B. Osteolytic metastasis
- C. Ectopic PTH-related protein production (Correct Answer)
- D. Multivitamin overdose
- E. Osteoblastic metastasis
Endocrine effects of non-endocrine tumors Explanation: ***Ectopic PTH-related protein production***
- The patient's symptoms (neck mass, weight loss, night sweats, fever) and biopsy findings (CD15+ and CD30+ large cells with bilobed nucleus) are highly suggestive of **Hodgkin lymphoma** with classic Reed-Sternberg cells.
- **Hypercalcemia (14.5 mg/dL)** with **inappropriately normal PTH (40 pg/mL)** in the context of malignancy points to **humoral hypercalcemia of malignancy (HHM)**, mediated by **PTH-related protein (PTHrP)** produced ectopically by tumor cells.
- PTH should be suppressed (<20 pg/mL) in the setting of hypercalcemia, so a level of 40 pg/mL indicates autonomous calcium elevation from a non-PTH source.
*Ectopic vitamin D production*
- While some lymphomas can produce **1,25-dihydroxyvitamin D** (through activated macrophages), leading to hypercalcemia, this would also cause **suppressed PTH**.
- This mechanism occurs in Hodgkin lymphoma but is less common than PTHrP-mediated hypercalcemia in most cases of malignancy-associated hypercalcemia.
*Osteolytic metastasis*
- **Osteolytic metastases** (e.g., from multiple myeloma or breast cancer) can cause hypercalcemia by directly destroying bone and releasing calcium.
- The biopsy is consistent with Hodgkin lymphoma, not a solid tumor that typically produces purely lytic bone metastases.
- While Hodgkin lymphoma can involve bone, systemic hypercalcemia due to direct bone destruction is less common than HHM through PTHrP.
*Multivitamin overdose*
- Overdosing on multivitamins could potentially lead to **vitamin D toxicity** and hypercalcemia if the supplements contained extremely high doses of vitamin D.
- However, the patient's symptoms, neck mass, fever, and biopsy findings clearly indicate a malignancy (Hodgkin lymphoma), making multivitamin overdose an unlikely cause of his profound hypercalcemia.
*Osteoblastic metastasis*
- **Osteoblastic metastases** (e.g., from prostate cancer) stimulate new bone formation and typically cause **elevated alkaline phosphatase** with normal or slightly elevated calcium, not profound hypercalcemia.
- Furthermore, the biopsy findings (Reed-Sternberg cells) are not consistent with a tumor type that causes osteoblastic metastases.
Endocrine effects of non-endocrine tumors US Medical PG Question 6: A lung mass of a 50 pack-year smoker is biopsied. If ADH levels were grossly increased, what would most likely be the histologic appearance of this mass?
- A. Layered squamous cells with keratin pearls
- B. Pleomorphic giant cells with leukocyte fragments in cytoplasm
- C. Hyperplasia of mucin producing glandular tissue
- D. Tall columnar cells bordering the alveolar septum
- E. Sheets of small round cells with hyperchromatic nuclei (Correct Answer)
Endocrine effects of non-endocrine tumors Explanation: ***Sheets of small round cells with hyperchromatic nuclei***
- Grossly increased **ADH levels** in a smoker suggest **syndrome of inappropriate antidiuretic hormone (SIADH)**, which is commonly associated with **small cell lung carcinoma (SCLC)**.
- SCLC is characterized histologically by sheets of **small (lymphocyte-like) cells** with scant cytoplasm and **hyperchromatic nuclei**.
*Layered squamous cells with keratin pearls*
- This description corresponds to **squamous cell carcinoma**, which is associated with smoking but typically causes **hypercalcemia** due to parathyroid hormone-related peptide (PTHrP) production, not elevated ADH.
- Key histological features are **keratin pearls** and **intercellular bridges**.
*Pleomorphic giant cells with leukocyte fragments in cytoplasm*
- This describes **large cell carcinoma**, which is a diagnosis of exclusion and does not typically manifest with paraneoplastic SIADH.
- **Large cell carcinoma** is characterized by large, anaplastic cells without differentiation towards squamous, glandular, or small cell features.
*Hyperplasia of mucin producing glandular tissue*
- This appearance is characteristic of **adenocarcinoma**, which often arises in non-smokers and is not typically associated with SIADH.
- **Adenocarcinoma** exhibits glandular differentiation and often produces mucin.
*Tall columnar cells bordering the alveolar septum*
- This refers to **lepidic growth pattern** often seen in some subtypes of **adenocarcinoma (e.g., adenocarcinoma in situ or minimally invasive adenocarcinoma)**.
- While it is a type of lung cancer, it is not primarily associated with SIADH as a paraneoplastic syndrome.
Endocrine effects of non-endocrine tumors US Medical PG Question 7: A 38-year-old female presents to her primary care physician with complaints of several episodes of palpitations accompanied by panic attacks over the last month. She also is concerned about many instances over the past few weeks where food has been getting stuck in her throat and she has had trouble swallowing. She denies any prior medical problems and reports a family history of cancer in her mother and maternal grandfather but cannot recall any details regarding the type of cancer(s) or age of diagnosis. Her vital signs at today's visit are as follows: T 37.6 deg C, HR 106, BP 158/104, RR 16, SpO2 97%. Physical examination is significant for a nodule on the anterior portion of the neck that moves with swallowing, accompanied by mild lymphadenopathy. A preliminary work-up is initiated, which shows hypercalcemia, elevated baseline calcitonin, and an inappropriately elevated PTH level. Diagnostic imaging shows bilateral adrenal lesions on an MRI of the abdomen/pelvis. Which of the following is the most likely diagnosis in this patient?
- A. Familial medullary thyroid cancer (FMTC)
- B. Li-Fraumeni syndrome
- C. Multiple endocrine neoplasia (MEN) IIa (Correct Answer)
- D. Multiple endocrine neoplasia (MEN) I
- E. Multiple endocrine neoplasia (MEN) IIb
Endocrine effects of non-endocrine tumors Explanation: ***Multiple endocrine neoplasia (MEN) IIa***
- This patient presents with **medullary thyroid cancer** (due to the thyroid nodule, elevated calcitonin, and family history of cancer), **pheochromocytoma** (indicated by palpitations, panic attacks, hypertension, and adrenal lesions), and **primary hyperparathyroidism** (evidenced by hypercalcemia and inappropriately elevated PTH). These three conditions are the classic triad of MEN IIa.
- The symptoms of food getting stuck in her throat are also consistent with the presence of a **thyroid nodule**.
*Familial medullary thyroid cancer (FMTC)*
- While the patient has **medullary thyroid cancer**, FMTC is typically characterized solely by medullary thyroid carcinoma without the associated pheochromocytoma or primary hyperparathyroidism seen in this case.
- This patient's presentation includes **adrenal lesions** and **hyperparathyroidism**, which are not features of isolated FMTC.
*Li-Fraumeni syndrome*
- This syndrome is associated with a high risk of various cancers, including sarcomas, breast cancer, brain tumors, and adrenocortical carcinoma, but it is not typically associated with **medullary thyroid cancer, pheochromocytoma, or primary hyperparathyroidism** as a primary presentation.
- The genetic basis is a mutation in the **TP53 gene**, and the clinical picture does not match the specific endocrine tumors observed here.
*Multiple endocrine neoplasia (MEN) I*
- MEN I is characterized by tumors of the **parathyroid, pituitary, and pancreas** (the 3 Ps).
- This patient's presentation of medullary thyroid cancer, pheochromocytoma, and primary hyperparathyroidism does not include pituitary or pancreatic tumors, and medullary thyroid cancer and pheochromocytoma are not part of the MEN I spectrum.
*Multiple endocrine neoplasia (MEN) IIb*
- MEN IIb includes **medullary thyroid cancer** and **pheochromocytoma**, which are present in this patient.
- However, MEN IIb also classically presents with characteristic **mucosal neuromas** and a **marfanoid habitus**, and *lacks* primary hyperparathyroidism, which this patient clearly exhibits.
Endocrine effects of non-endocrine tumors US Medical PG Question 8: A 10-year-old girl is brought to the physician by her parents due to 2 months of a progressively worsening headache. The headaches were initially infrequent and her parents attributed them to stress from a recent move. However, over the last week the headaches have gotten significantly worse and she had one episode of vomiting this morning when she woke up. Her medical history is remarkable for a hospitalization during infancy for bacterial meningitis. On physical exam, the patient has difficulty looking up. The lower portion of her pupil is covered by the lower eyelid and there is sclera visible below the upper eyelid. A magnetic resonance imaging (MRI) of the brain is shown. Which of the following is the most likely diagnosis?
- A. Ependymoma
- B. Medulloblastoma
- C. Craniopharyngioma
- D. Pinealoma (Correct Answer)
- E. Pituitary Adenoma
Endocrine effects of non-endocrine tumors Explanation: ***Pinealoma***
- The constellation of a progressively worsening headache, vomiting, and difficulty looking up (Parinaud's syndrome or **dorsal midbrain syndrome**) with **hydrocephalus** visible on MRI points strongly to a **pineal region tumor** that compresses the **tectal plate** and obstructs CSF flow. The visible sclera below the upper eyelid is due to **retraction of the upper eyelids**, a component of Parinaud's syndrome.
- The MRI shows significant **ventricular dilation**, particularly of the lateral and third ventricles, indicating **obstructive hydrocephalus**, which is consistent with a mass in the pineal region compressing the **cerebral aqueduct**.
*Ependymoma*
- Ependymomas most commonly occur in the **fourth ventricle** in children and can cause hydrocephalus by obstructing CSF flow at that level.
- However, typical symptoms would be more associated with **cerebellar dysfunction** (ataxia, nystagmus), and Parinaud's syndrome is not characteristic.
*Medulloblastoma*
- Medulloblastomas are highly malignant **cerebellar tumors** in children, typically arising from the vermis, and often cause **ataxia**, truncal instability, and hydrocephalus due to fourth ventricle obstruction.
- While they cause hydrocephalus and headaches, they do not typically present with Parinaud's syndrome.
*Craniopharyngioma*
- Craniopharyngiomas are **suprasellar tumors** that originate from Rathke's pouch remnants and can cause headaches, visual field defects (**bitemporal hemianopsia**), and **endocrine dysfunction** (e.g., growth delays, diabetes insipidus).
- They are typically located anteriorly, compressing the **optic chiasm** and hypothalamus, not directly obstructing the cerebral aqueduct to cause Parinaud's syndrome.
*Pituitary Adenoma*
- Pituitary adenomas are rare in children and typically cause symptoms related to **hormonal overproduction** or compression of adjacent structures, such as **visual field defects** (bitemporal hemianopsia).
- While large adenomas can cause headaches, they are not typically associated with **Parinaud's syndrome** or rapid-onset **obstructive hydrocephalus** in this manner.
Endocrine effects of non-endocrine tumors US Medical PG Question 9: A 40-year-old man presents with a painless firm mass in the right breast. Examination shows retraction of the nipple and the skin is fixed to the underlying mass. The axillary nodes are palpable. Which of the following statements is FALSE regarding the above condition?
- A. Lobular cancer is the most common breast cancer in males (Correct Answer)
- B. BRCA2 mutations are associated with increased risk
- C. These are positive for estrogen receptor
- D. Endocrine therapy plays an important role in treatment
- E. Gynecomastia may be caused by certain medications
Endocrine effects of non-endocrine tumors Explanation: ***Lobular cancer is the most common breast cancer in males***
- This statement is **FALSE** and is the correct answer. The most common type of breast cancer in males is **invasive ductal carcinoma (IDC)**, accounting for about 80-90% of cases.
- **Invasive lobular carcinoma** is rare in men because men have very few lobules in their breast tissue.
*Gynecomastia may be caused by certain medications*
- This statement is **TRUE**. Medications such as spironolactone, cimetidine, finasteride, antipsychotics, and anabolic steroids can cause gynecomastia.
- However, the clinical presentation described (firm mass, nipple retraction, skin fixation, axillary nodes) is consistent with **malignancy**, not gynecomastia.
*BRCA2 mutations are associated with increased risk*
- This statement is **TRUE**. Male breast cancer is strongly associated with **BRCA2 mutations** (and less commonly BRCA1), which are hereditary.
- Men with BRCA2 mutations have a 5-10% lifetime risk of developing breast cancer, compared to less than 0.1% in the general male population.
*These are positive for estrogen receptor*
- This statement is **TRUE**. A vast majority (over 90%) of male breast cancers are **estrogen receptor (ER) positive**, which makes them responsive to endocrine therapy.
- This high rate of ER positivity is even greater than in female breast cancers.
*Endocrine therapy plays an important role in treatment*
- This statement is **TRUE**. Given the high prevalence of ER positivity (over 90%), endocrine therapy such as **tamoxifen** or aromatase inhibitors is a cornerstone of treatment for male breast cancer.
- Endocrine therapy is used in both adjuvant and metastatic settings for hormone receptor-positive disease.
Endocrine effects of non-endocrine tumors US Medical PG Question 10: A neurophysiologist describes the mechanism of a specific type of synaptic transmission to his students. While illustrating this, he points out that when the action potential reaches the presynaptic terminal of a chemical synapse, the voltage-gated Ca2+ channels open. Ca2+ ions trigger the release of neurotransmitters from vesicles in the presynaptic terminal. In this type of synaptic transmission, increased cytosolic Ca2+ levels cause the release of a neurotransmitter from small vesicles with dense cores. Which of the following neurotransmitters is most likely to be the one that is released into the synaptic cleft in this type of synapse?
- A. Epinephrine
- B. Glutamate
- C. Glycine
- D. GABA (γ-amino butyric acid)
- E. Norepinephrine (Correct Answer)
Endocrine effects of non-endocrine tumors Explanation: ***Norepinephrine***
- **Norepinephrine** is the primary catecholamine neurotransmitter stored in **small vesicles with dense cores** (dense-core vesicles).
- It is released from **sympathetic postganglionic neurons** and central nervous system neurons, particularly from the **locus coeruleus**.
- Dense-core vesicles are the hallmark of catecholaminergic neurons, and norepinephrine is the most abundant neuronal catecholamine.
- The description perfectly matches noradrenergic synaptic transmission.
*Epinephrine*
- While epinephrine is also a catecholamine stored in dense-core vesicles, it functions primarily as a **hormone** released from the **adrenal medulla** (not a neurotransmitter).
- Only a **very small number** of CNS neurons use epinephrine as a neurotransmitter (mainly in medullary regions).
- In the context of synaptic transmission, norepinephrine is far more common.
*Glutamate*
- **Glutamate** is the primary excitatory neurotransmitter in the CNS but is stored in **small, clear synaptic vesicles**, not dense-core vesicles.
- It does not fit the description of dense-core vesicle storage.
*Glycine*
- **Glycine** is an inhibitory neurotransmitter stored in **small, clear synaptic vesicles**.
- Found predominantly in the **spinal cord** and brainstem, not in dense-core vesicles.
*GABA (γ-amino butyric acid)*
- **GABA** is the main inhibitory neurotransmitter stored in **small, clear synaptic vesicles**.
- Not associated with dense-core vesicle storage.
More Endocrine effects of non-endocrine tumors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.