Endocrine disorders in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Endocrine disorders in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Endocrine disorders in pregnancy US Medical PG Question 1: A 27-year-old G1P0 at 12 weeks estimated gestational age presents for prenatal care. The patient says she has occasional nausea and vomiting and a few episodes of palpitations and diarrhea this last week. Physical examination is unremarkable, except for a heart rate of 145/min. Basic thyroid function tests are shown in the table below. Which of the following additional laboratory tests would be most useful in assessing this patient's condition?
Thyroid-stimulating hormone (TSH)
0.28 mIU/L (0.3–4.5 mIU/L)
Total T4
12 µg/dL (5.4–11.5 µg/dL)
- A. Thyrotropin receptor antibodies (TRAb)
- B. Total triiodothyronine (T3) levels
- C. Thyroid peroxidase (TPO) antibodies
- D. Free thyroxine (T4) levels (Correct Answer)
- E. Thyroxine-binding globulin (TBG) levels
Endocrine disorders in pregnancy Explanation: ***Free thyroxine (T4) levels***
- In pregnancy, **estrogen increases thyroxine-binding globulin (TBG)**, leading to higher **total T4** levels even if free T4 is normal.
- Measuring **free T4 provides a more accurate assessment** of the biologically active thyroid hormone, which is crucial for distinguishing between physiological changes of pregnancy and true hyperthyroidism.
*Thyrotropin receptor antibodies (TRAb)*
- **TRAb are specific for Graves' disease**, which is a cause of hyperthyroidism, but their presence is a confirmatory test after hyperthyroidism has been established.
- The initial step is to confirm the diagnosis of **hyperthyroidism** by evaluating free hormone levels, particularly in pregnancy where total hormone levels are less reliable.
*Total triiodothyronine (T3) levels*
- Similar to total T4, **total T3 levels are also affected by increased TBG in pregnancy**, making them less reliable for initial diagnosis of thyroid dysfunction.
- While T3 is an important thyroid hormone, **free T4 is generally the primary screening test** for hyperthyroidism.
*Thyroid peroxidase (TPO) antibodies*
- **TPO antibodies are indicative of autoimmune thyroiditis**, such as Hashimoto's thyroiditis, which typically causes hypothyroidism, not hyperthyroidism, as suggested by the patient's symptoms and elevated T4.
- Although TPO antibodies can sometimes be positive in Graves' disease, they are **not the primary diagnostic test for active hyperthyroidism**, especially regarding the magnitude of the elevation.
*Thyroxine-binding globulin (TBG) levels*
- While **TBG levels are elevated in pregnancy**, measuring TBG itself doesn't directly assess thyroid function.
- Understanding the physiology of **TBG elevation explains why total T4 is high**, but it doesn't help in determining whether the patient is truly hyperthyroid; for that, free T4 is needed.
Endocrine disorders in pregnancy US Medical PG Question 2: A 25-year-old pregnant woman at 28 weeks gestation presents with a headache. Her pregnancy has been managed by a nurse practitioner. Her temperature is 99.0°F (37.2°C), blood pressure is 164/104 mmHg, pulse is 100/min, respirations are 22/min, and oxygen saturation is 98% on room air. Physical exam is notable for a comfortable appearing woman with a gravid uterus. Laboratory tests are ordered as seen below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 6,700/mm^3 with normal differential
Platelet count: 100,500/mm^3
Serum:
Na+: 141 mEq/L
Cl-: 101 mEq/L
K+: 4.4 mEq/L
HCO3-: 25 mEq/L
BUN: 21 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.0 mg/dL
AST: 32 U/L
ALT: 30 U/L
Urine:
Color: Amber
Protein: Positive
Blood: Negative
Which of the following is the most likely diagnosis?
- A. HELLP syndrome
- B. Acute fatty liver disease of pregnancy
- C. Preeclampsia
- D. Severe preeclampsia (Correct Answer)
- E. Eclampsia
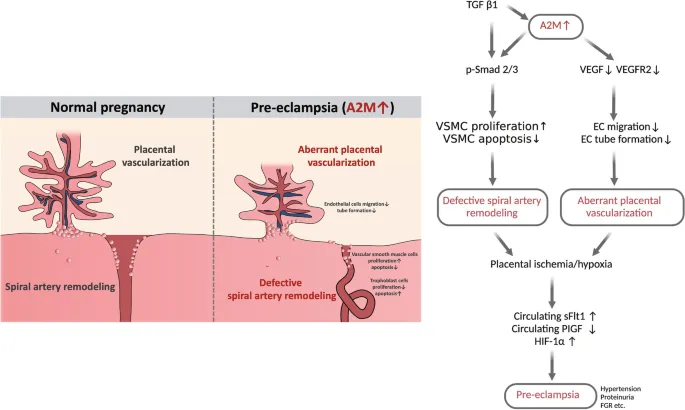
Endocrine disorders in pregnancy Explanation: ***Severe preeclampsia***
- The patient exhibits **hypertension** (BP 164/104 mmHg), **proteinuria** (positive urine protein), and **thrombocytopenia** (platelet count 100,500/mm^3). The elevated BUN and creatinine also suggest **renal dysfunction**.
- The blood pressure reading 164/104 mmHg meets the criteria for **severe range blood pressure** (systolic ≥160 mmHg or diastolic ≥110 mmHg), classifying this as severe preeclampsia. Headaches are also a symptom of severe preeclampsia.
*HELLP syndrome*
- While **thrombocytopenia** is present, the **liver enzymes (AST/ALT)** are not elevated (AST 32 U/L, ALT 30 U/L), which would be a primary diagnostic criterion for HELLP (Hemolysis, Elevated Liver enzymes, Low Platelets).
- There is no evidence of **hemolysis**, such as elevated bilirubin or schistocytes on a peripheral smear, which is also required for HELLP diagnosis.
*Acute fatty liver disease of pregnancy*
- This condition presents with significantly elevated **liver enzymes**, **jaundice**, and often severe **hypoglycemia** and **coagulopathy**, none of which are evident in this patient's lab results.
- While it can cause elevated BUN and creatinine, it typically involves **more prominent liver dysfunction** than seen here.
*Preeclampsia*
- This patient meets the criteria for preeclampsia (hypertension and proteinuria), but her **blood pressure** (164/104 mmHg), **thrombocytopenia** (platelet count 100,500/mm^3), and elevated **creatinine** (1.0 mg/dL) all point to features that classify it as *severe* preeclampsia.
- Preeclampsia without severe features generally involves blood pressure values below 160/110 mmHg and no evidence of significant organ dysfunction or severe laboratory abnormalities.
*Eclampsia*
- Eclampsia is defined as the occurrence of new-onset **grand mal seizures** in a woman with preeclampsia.
- The patient presents with a **headache** but is described as "comfortable appearing" and there is no mention of seizures.
Endocrine disorders in pregnancy US Medical PG Question 3: A 30-year-old woman presents for pregnancy counseling. She says she has an 8-week history of chronic diarrhea. She is also found to be intolerant to heat and has been significantly losing her hair. She denies any recent changes to her diet. The patient is afebrile and her vital signs are within normal limits. Her weight today is 45.0 kg (99.2 lb) which is 4.5 kg (10 lb) less than her weight during her last visit 2 months back. On physical examination, the patient is anxious and has a non-intention tremor. Significant exophthalmos is present. Laboratory findings are significant for a low TSH, elevated free T4 and free T3, and a positive thyroid stimulating immunoglobulin assay. She still wants to conceive a baby and asks for an appropriate treatment that is safe in pregnancy. Which of the following best describes the therapy she will most likely receive during her pregnancy for her thyroid disorder?
- A. Beta-blockers
- B. Thyroidectomy and thyroid replacement
- C. Plasmapheresis
- D. Radiation
- E. Antithyroid drugs (thionamides) (Correct Answer)
Endocrine disorders in pregnancy Explanation: ***Antithyroid drugs (thionamides)***
- **Antithyroid drugs** like **propylthiouracil (PTU)** or **methimazole** are the primary treatment for **hyperthyroidism** during pregnancy, as they reduce thyroid hormone synthesis.
- **PTU** is often preferred in the **first trimester** due to a lower risk of teratogenicity compared to methimazole, although **methimazole** can be used in the **second and third trimesters**.
*Beta-blockers*
- **Beta-blockers** can alleviate **symptomatic hyperthyroidism** (e.g., tremor, palpitations) in the short term but do not address the underlying hormonal imbalance.
- They are generally used as **adjunctive therapy** for symptom control, especially in the initial stages, but are not a definitive treatment for the thyroid disorder itself.
*Thyroidectomy and thyroid replacement*
- **Thyroidectomy** is a surgical option for hyperthyroidism, but it is typically reserved for cases where antithyroid medications are ineffective or contraindicated, or in emergencies like **thyroid storm** not responsive to medical therapy.
- **Surgery during pregnancy** carries significant risks to both the mother and the fetus and is generally avoided unless absolutely necessary, usually during the **second trimester** if unavoidable.
*Plasmapheresis*
- **Plasmapheresis** is a procedure used in severe, life-threatening cases of hyperthyroidism, such as **thyroid storm**, particularly when other treatments have failed or are not tolerated.
- It rapidly reduces circulating thyroid hormones and **thyroid-stimulating immunoglobulins (TSI)** but is not a routine or long-term treatment for pregnancy-associated hyperthyroidism.
*Radiation*
- **Radioactive iodine (RAI) therapy** is effective in destroying overactive thyroid tissue and is a common treatment for hyperthyroidism in non-pregnant individuals.
- However, **RAI is absolutely contraindicated in pregnancy** because it can cross the placenta and ablate the fetal thyroid gland, causing **fetal hypothyroidism**.
Endocrine disorders in pregnancy US Medical PG Question 4: A 31-year-old G3P2 who is at 24 weeks gestation presents for a regular check-up. She has no complaints, no concurrent diseases, and her previous pregnancies were vaginal deliveries with birth weights of 3100 g and 4180 g. The patient weighs 78 kg (172 lb) and is 164 cm (5 ft 5 in) in height. She has gained 10 kg (22 lb) during the current pregnancy. Her vital signs and physical examination are normal. The plasma glucose level is 190 mg/dL after a 75-g oral glucose load. Which of the listed factors contributes to the pathogenesis of the patient’s condition?
- A. Decrease in insulin gene expression
- B. Insulin antagonism of human placental lactogen (Correct Answer)
- C. Production of autoantibodies against pancreatic beta cells
- D. Decrease in insulin sensitivity of maternal tissues caused by alpha-fetoprotein
- E. Point mutations in the gene coding for insulin
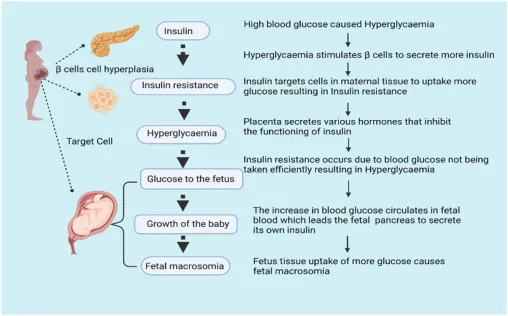
Endocrine disorders in pregnancy Explanation: ***Insulin antagonism of human placental lactogen***
- The patient's elevated plasma glucose indicates **gestational diabetes mellitus (GDM)**, a condition characterized by **insulin resistance** that emerges during pregnancy.
- **Human placental lactogen (hPL)**, secreted by the placenta, is a key hormone that **antagonizes maternal insulin**, contributing significantly to the insulin resistance seen in GDM.
*Decrease in insulin gene expression*
- A decrease in insulin gene expression would lead to **reduced insulin production**, which is not the primary mechanism of insulin resistance in GDM.
- While pancreatic beta cells compensate by increasing insulin secretion in GDM, the underlying problem is the **tissue's reduced response** to insulin.
*Production of autoantibodies against pancreatic beta cells*
- This mechanism is characteristic of **Type 1 diabetes**, where the immune system destroys insulin-producing beta cells, leading to absolute insulin deficiency.
- GDM is primarily a condition of **insulin resistance**, not autoimmune destruction of beta cells.
*Decrease in insulin sensitivity of maternal tissues caused by alpha-fetoprotein*
- **Alpha-fetoprotein (AFP)** is primarily involved in fetal development and is not known to directly cause a decrease in maternal insulin sensitivity.
- The main placental hormones contributing to insulin resistance are **hPL**, progesterone, and cortisol, not AFP.
*Point mutations in the gene coding for insulin*
- **Point mutations** in the insulin gene are rare and would typically manifest as forms of monogenic diabetes or insulin-related disorders, not characteristic GDM.
- GDM is generally a polygenic or multifactorial condition influenced by pregnancy hormones and pre-existing insulin resistance.
Endocrine disorders in pregnancy US Medical PG Question 5: A 23-year-old G1P0 primigravid woman at 28 weeks estimated gestational age presents for a prenatal checkup. She says she has been having occasional headaches but is otherwise fine. The patient says she feels regular fetal movements and mild abdominal pain at times. Her past medical history is unremarkable. Current medications are a prenatal multivitamin and the occasional acetaminophen. Her blood pressure is 148/110 mm Hg today. On her last visit at 24 weeks of gestation, her blood pressure was 146/96 mm Hg. On physical exam, the fundus measures 28 cm above the pubic symphysis. Laboratory findings are significant for the following:
Serum Glucose (fasting) 88 mg/dL
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum Creatinine 0.9 mg/dL
Blood Urea Nitrogen 10 mg/dL
Alanine aminotransferase (ALT) 18 U/L
Aspartate aminotransferase (AST) 16 U/L
Mean Corpuscular Volume (MCV) 85 fL
Leukocyte count 4,200/mm3
Reticulocyte count 1%
Erythrocyte count 5.1 million/mm3
Platelet count 95,000mm3
Urinalysis show:
Proteins 2+
Glucose negative
Ketones negative
Leucocytes negative
Nitrites negative
Red Blood Cells (RBCs) negative
Casts negative
Which of the following medications would be the next best step in the treatment of this patient?
- A. Magnesium sulfate (Correct Answer)
- B. Phenobarbital
- C. Valproic acid
- D. Ethosuximide
- E. Diazepam
Endocrine disorders in pregnancy Explanation: ***Magnesium sulfate***
- The patient presents with **gestational hypertension**, **proteinuria (2+)**, **thrombocytopenia (platelets 95,000/mm³)**, and **headaches at 28 weeks gestation**, indicating severe preeclampsia.
- **Magnesium sulfate** is the drug of choice for the prevention and treatment of **eclampsia-related seizures** in women with severe preeclampsia.
*Phenobarbital*
- **Phenobarbital** is an anticonvulsant but is generally reserved for refractory seizures or in situations where magnesium sulfate is contraindicated.
- It has a risk of **fetal respiratory depression** and neonatal withdrawal symptoms if used close to delivery.
*Valproic acid*
- **Valproic acid** is an anticonvulsant that carries a significant risk of **teratogenicity**, including **neural tube defects**, especially if used in early pregnancy.
- It is not the preferred agent for acute seizure prophylaxis in preeclampsia.
*Ethosuximide*
- **Ethosuximide** is primarily used for **absence seizures** and has no role in the management or prevention of seizures in preeclampsia.
- It would not address the underlying pathology or provide seizure prophylaxis in this patient.
*Diazepam*
- While **diazepam** can be used to abort an active seizure, it is not recommended for routine seizure prophylaxis in preeclampsia due to its **sedative effects** and potential for **fetal depression**.
- Magnesium sulfate is more effective and has a better safety profile for seizure prevention in preeclampsia.
Endocrine disorders in pregnancy US Medical PG Question 6: A 34-year-old woman, who had her first child 2 weeks ago, visits her family physician with concerns about constant fatigue and difficulty with breastfeeding. She was discharged from the intensive care unit after hospitalization for severe postpartum hemorrhage. Since then, she has tried multiple pumps and self-stimulation to encourage breast milk production; however, neither of these strategies has worked. Her blood pressure is 88/56 mm Hg and heart rate is 120/min. Which of the following best explains the underlying condition of this patient?
- A. Pituitary infarction (Correct Answer)
- B. Pituitary infection
- C. Pituitary hemorrhage
- D. Pituitary infiltration by histiocytes
- E. Pituitary stalk epithelial tumor
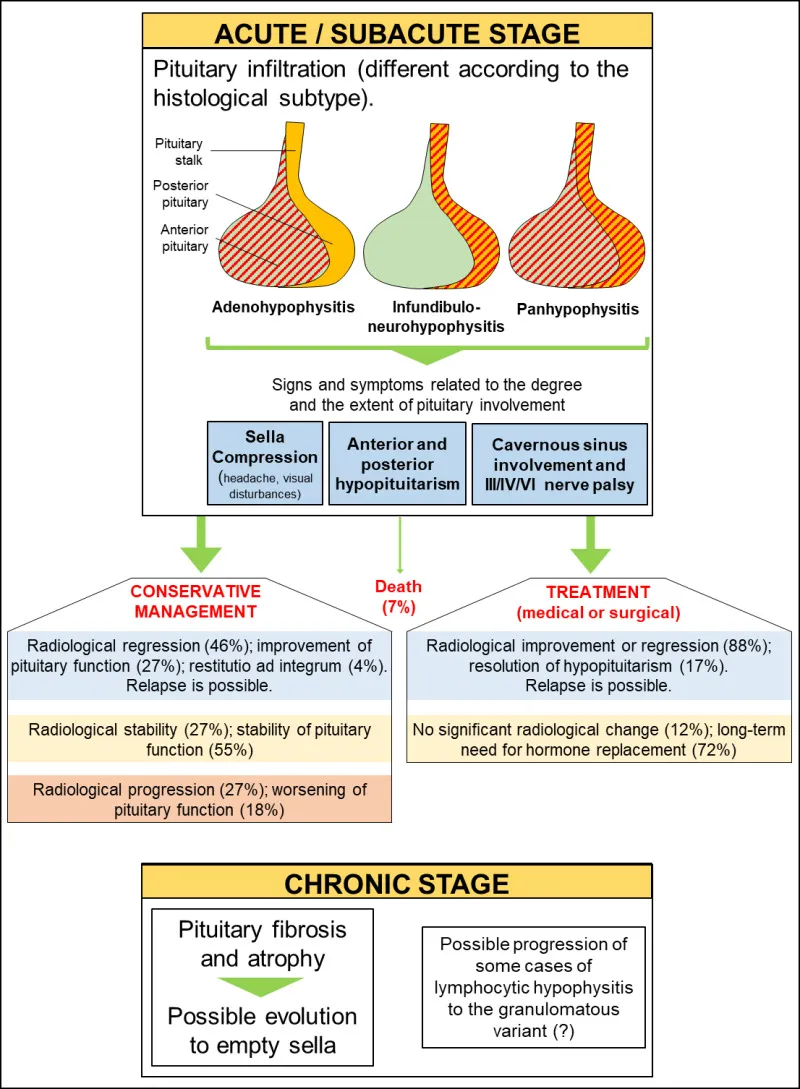
Endocrine disorders in pregnancy Explanation: ***Pituitary infarction***
- The patient's history of **severe postpartum hemorrhage** causing hypovolemic shock, followed by **fatigue**, **difficulty breastfeeding**, **hypotension**, and **tachycardia**, are classic signs of **Sheehan syndrome**, which is caused by ischemic necrosis (infarction) of the pituitary gland.
- The **lactotroph cells** in the anterior pituitary enlarge significantly during pregnancy, making them more vulnerable to ischemia when blood supply is compromised during hemorrhage.
*Pituitary infection*
- **Pituitary infections** (e.g., abscess) are rare and typically present with symptoms of inflammation such as fever, severe headaches, and meningeal signs, which are not described here.
- While an infection could potentially affect pituitary function, it is not the classic presentation following postpartum hemorrhage.
*Pituitary hemorrhage*
- While postpartum hemorrhage is the cause of the pituitary injury, the **pituitary itself is not hemorrhaging** in Sheehan's syndrome; rather, it is undergoing infarction due to global hypoperfusion.
- **Pituitary apoplexy** (hemorrhage into the pituitary) is an acute event with sudden onset of severe headache, visual disturbances, and rapid endocrine dysfunction, typically not related to postpartum hemorrhage directly in this manner.
*Pituitary infiltration by histiocytes*
- **Histiocytic infiltration** can occur in conditions like Langerhans cell histiocytosis or sarcoidosis, affecting pituitary function.
- However, these conditions have distinct clinical features and are not directly linked to a recent history of postpartum hemorrhage as the precipitating event.
*Pituitary stalk epithelial tumor*
- A **pituitary stalk epithelial tumor** would typically cause symptoms due to mass effect or hormonal imbalances, which might include galactorrhea (if prolactin-secreting) or hypopituitarism over time.
- This scenario does not fit the acute onset of symptoms following postpartum hemorrhage, which points to an ischemic event.
Endocrine disorders in pregnancy US Medical PG Question 7: A 26-year-old primigravid woman at 25 weeks' gestation comes to the physician for a prenatal visit. She has no history of serious illness and her only medication is a daily prenatal vitamin. A 1-hour 50-g glucose challenge shows a glucose concentration of 167 mg/dL (N < 135). A 100-g oral glucose tolerance test shows glucose concentrations of 213 mg/dL (N < 180) and 165 mg/dL (N < 140) at 1 and 3 hours, respectively. If she does not receive adequate treatment for her condition, which of the following complications is her infant at greatest risk of developing?
- A. Elevated calcium levels
- B. Decreased hematocrit
- C. Decreased amniotic fluid production
- D. Islet cell hyperplasia (Correct Answer)
- E. Omphalocele
Endocrine disorders in pregnancy Explanation: ***Islet cell hyperplasia***
- The patient's glucose tolerance test results indicate **gestational diabetes mellitus (GDM)**, which leads to increased fetal glucose exposure.
- In response to chronic hyperglycemia, the fetal beta cells undergo **hyperplasia** and hypertrophy to increase insulin production, predisposing the infant to **hypoglycemia** after birth.
*Elevated calcium levels*
- **Hypocalcemia** is a more common electrolyte disturbance in infants of diabetic mothers due to prematurity, asphyxia, or parathyroid hormone suppression.
- **Hypercalcemia** is not typically associated with gestational diabetes.
*Decreased hematocrit*
- Infants of diabetic mothers are at increased risk for **polycythemia** (elevated hematocrit) due to increased erythropoietin production in response to fetal hypoxia.
- **Decreased hematocrit** (anemia) is less common and usually related to other causes.
*Decreased amniotic fluid production*
- Uncontrolled gestational diabetes often leads to **polyhydramnios** (excess amniotic fluid) due to fetal hyperglycemia-induced polyuria.
- **Oligohydramnios** (decreased amniotic fluid) is not a typical complication of GDM.
*Omphalocele*
- **Omphalocele** is a **ventral wall defect** associated with chromosomal abnormalities or other genetic syndromes, not primarily with gestational diabetes.
- While GDM can increase the risk of various birth defects, omphalocele is not one of the more commonly cited or direct consequences.
Endocrine disorders in pregnancy US Medical PG Question 8: A 43-year-old man presents to the emergency department following a work-related accident in which both arms were amputated. The patient lost a substantial amount of blood prior to arrival, and his bleeding is difficult to control due to arterial damage and wound contamination with debris. His complete blood count (CBC) is significant for a hemoglobin (Hgb) level of 5.3 g/dL. The trauma surgery resident initiates the massive transfusion protocol and orders whole blood, O negative, which she explains is the universal donor. The patient receives 6 units of O negative blood prior to admission. He subsequently develops fever, chills, hematuria, and pulmonary edema. Several hours later, the patient goes into hemodynamic shock requiring the emergent administration of vasopressors. Of the following options, which hypersensitivity reaction occurred?
- A. Type 1 hypersensitivity reaction
- B. Combined type 1 and type 4 hypersensitivity reaction
- C. Type 3 hypersensitivity reaction
- D. Type 2 hypersensitivity reaction (Correct Answer)
- E. Type 4 hypersensitivity reaction
Endocrine disorders in pregnancy Explanation: ***Type 2 hypersensitivity reaction***
- This scenario describes an **acute hemolytic transfusion reaction (AHTR)**, a classic example of a **Type II hypersensitivity reaction**. The recipient's antibodies (IgM) recognize and bind to antigens on the transfused red blood cells, leading to their destruction (hemolysis) via complement activation and cellular mechanisms.
- Symptoms like **fever, chills, hematuria (due to hemoglobinuria)**, and subsequent **shock** are characteristic of AHTR, even with O negative blood if other minor blood group antigens (e.g., Kell, Duffy) are incompatible or if the patient developed antibodies against these from previous transfusions or pregnancies.
*Type 1 hypersensitivity reaction*
- This type involves **IgE-mediated mast cell degranulation** and is associated with allergic reactions such as anaphylaxis, asthma, and hives.
- While anaphylaxis can cause shock, the systemic symptoms of **hemolysis and hematuria** are not characteristic of a Type 1 reaction.
*Combined type 1 and type 4 hypersensitivity reaction*
- This combination is uncommon in an acute transfusion setting and does not align with the presented symptoms.
- Type 1 is immediate allergic, and Type 4 is delayed cell-mediated, neither fully explaining the hemolytic features observed.
*Type 3 hypersensitivity reaction*
- This reaction involves the formation of **immune complexes** (antigen-antibody complexes) that deposit in tissues, leading to inflammation and damage (e.g., serum sickness, lupus nephritis).
- While immune complexes can cause systemic symptoms, the prominent hemolytic features and immediate presentation of a transfusion reaction are more indicative of Type 2.
*Type 4 hypersensitivity reaction*
- This is a **delayed type hypersensitivity** reaction mediated by **T cells**, taking 24-72 hours or longer to develop (e.g., contact dermatitis, tuberculin skin test).
- The acute onset of symptoms following transfusion makes a Type 4 reaction highly unlikely.
Endocrine disorders in pregnancy US Medical PG Question 9: As part of a clinical research study, microscopic analysis of tissues obtained from surgical specimens is performed. Some of these tissues have microscopic findings of an increase in the size of numerous cells within the tissue with an increase in the amount of cytoplasm, but the nuclei are uniform in size. Which of the following processes shows such microscopic findings?
- A. Liver following partial resection
- B. Female breasts at puberty
- C. Ovaries following menopause
- D. Uterine myometrium in pregnancy (Correct Answer)
- E. Cervix with chronic inflammation
Endocrine disorders in pregnancy Explanation: ***Uterine myometrium in pregnancy***
- During pregnancy, the uterine myometrial cells undergo significant **hypertrophy** (increase in cell size) in response to hormonal stimulation, primarily *estrogen* and *progesterone*.
- This leads to a marked increase in the amount of **cytoplasm** and overall cell size, while maintaining relatively **uniform nuclei**, which precisely matches the microscopic findings described.
- The smooth muscle cells can increase **10-40 fold** in size, making this the classic example of physiologic hypertrophy.
- Note: Hyperplasia (increased cell number) also occurs but is less prominent; the microscopic findings described emphasize the hypertrophic changes.
*Liver following partial resection*
- The liver primarily undergoes **hyperplasia** (increase in cell number) to regenerate following partial resection.
- While some hypertrophy occurs, the dominant microscopic finding is an increase in hepatocyte **number** through proliferation rather than a marked increase in individual cell size and cytoplasm as the primary feature.
*Female breasts at puberty*
- Breast development at puberty involves both **hyperplasia** of the glandular epithelium and ductal structures and **adipose tissue deposition**, driven by *estrogen* and *progesterone*.
- The findings described (marked increase in cell size and cytoplasm with uniform nuclei) are more characteristic of the extreme cell hypertrophy seen in the gravid uterus rather than the mixed growth and differentiation patterns of pubertal breast development.
*Ovaries following menopause*
- Following menopause, the ovaries undergo **atrophy**, meaning a decrease in size and cellular activity due to declining hormonal production.
- This process involves a **decrease in cell size** and number, which is the opposite of the microscopic findings described in the question.
*Cervix with chronic inflammation*
- Chronic inflammation in the cervix can cause various changes, including **squamous metaplasia** (transformation of columnar epithelium to squamous epithelium) or an influx of inflammatory cells.
- While there might be some reactive cellular changes, it does not typically involve a widespread, uniform increase in cell size and cytoplasm within existing cells as described, but rather a change in cell type or infiltration by inflammatory cells.
Endocrine disorders in pregnancy US Medical PG Question 10: A 38-year-old woman with type 1 diabetes for 20 years presents with diabetic ketoacidosis. She is treated and recovers. Six months later, she develops progressive fatigue, nausea, and hyperpigmentation. Laboratory studies show morning cortisol 3 μg/dL, ACTH 180 pg/mL, TSH 8.2 mIU/L, free T4 0.6 ng/dL, and positive anti-thyroid peroxidase antibodies. She also has positive 21-hydroxylase antibodies. Her 12-year-old daughter was recently diagnosed with type 1 diabetes. Evaluate the pathologic process and most critical monitoring recommendation for the daughter.
- A. Multiple endocrine neoplasia syndrome; screen for pheochromocytoma and medullary thyroid cancer
- B. Autoimmune polyglandular syndrome type 2; screen daughter for adrenal antibodies and thyroid function annually (Correct Answer)
- C. Schmidt syndrome with isolated sporatic occurrence; routine diabetes management only for daughter
- D. Autoimmune polyglandular syndrome type 1; screen for mucocutaneous candidiasis and hypoparathyroidism
- E. Secondary endocrine failure from diabetes complications; optimize glycemic control in daughter
Endocrine disorders in pregnancy Explanation: ***Autoimmune polyglandular syndrome type 2; screen daughter for adrenal antibodies and thyroid function annually***
- The patient presents with **Schmidt syndrome (APS type 2)**, defined by the triad of **Addison's disease** (low cortisol, high ACTH, 21-hydroxylase antibodies), **type 1 diabetes**, and **autoimmune thyroid disease** (Hashimoto's).
- Because APS-2 is **polygenic** and associated with **HLA-DR3/DR4**, first-degree relatives with one component (like the daughter) require screening for other silent autoimmune conditions to prevent **adrenal crisis**.
*Multiple endocrine neoplasia syndrome; screen for pheochromocytoma and medullary thyroid cancer*
- **MEN syndromes** are characterized by **neoplastic** growths (like medullary thyroid cancer or parathyroid adenomas) rather than the **autoimmune destruction** of glands seen here.
- The absence of hypertension or neck masses and the presence of **autoantibodies** directly contradict a diagnosis of MEN.
*Schmidt syndrome with isolated sporatic occurrence; routine diabetes management only for daughter*
- While the patient does have **Schmidt syndrome**, it is incorrect to label it as purely sporadic because it has a strong **familial clustering** component.
- Managing only diabetes in the daughter is insufficient and dangerous, as it ignores her increased risk for life-threatening **primary adrenal insufficiency**.
*Autoimmune polyglandular syndrome type 1; screen for mucocutaneous candidiasis and hypoparathyroidism*
- **APS-1** typically presents in childhood with the triad of **chronic mucocutaneous candidiasis**, **hypoparathyroidism**, and adrenal failure, which does not match this adult patient’s profile.
- APS-1 is caused by a single gene mutation in **AIRE**, whereas this patient's presentation and family history are classic for the polygenic **APS-2**.
*Secondary endocrine failure from diabetes complications; optimize glycemic control in daughter*
- Diabetic complications lead to **microvascular** or **macrovascular** damage, not the **primary gland failure** (indicated by high ACTH and TSH) seen in this patient.
- **Hyperpigmentation** and the presence of **organ-specific antibodies** (21-hydroxylase) confirm an **autoimmune primary failure**, not a secondary metabolic complication.
More Endocrine disorders in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.