Diabetes mellitus pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diabetes mellitus pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diabetes mellitus pathology US Medical PG Question 1: A 19-year-old man with a history of type 1 diabetes presents to the emergency department for the evaluation of a blood glucose level of 492 mg/dL. Laboratory examination revealed a serum bicarbonate level of 13 mEq/L, serum sodium level of 122 mEq/L, and ketonuria. Arterial blood gas demonstrated a pH of 6.9. He is admitted to the hospital and given bicarbonate and then started on an insulin drip and intravenous fluid. Seven hours later when his nurse is making rounds, he is confused and complaining of a severe headache. Repeat sodium levels are unchanged, although his glucose level has improved. His vital signs include a temperature of 36.6°C (98.0°F), pulse 50/min, respiratory rate 13/min and irregular, and blood pressure 177/95 mm Hg. What other examination findings would be expected in this patient?
- A. Hypoglycemia
- B. Pupillary constriction
- C. Papilledema (Correct Answer)
- D. Pancreatitis
- E. Peripheral edema
Diabetes mellitus pathology Explanation: ***Papilledema***
- This patient's symptoms (confusion, severe headache, bradycardia, irregular respiration, hypertension) following treatment for **diabetic ketoacidosis (DKA)** are highly suggestive of **cerebral edema**.
- **Papilledema** is a retinal finding resulting from increased intracranial pressure (ICP), which is a characteristic sign of cerebral edema.
*Hypoglycemia*
- While the patient's glucose level has improved, it is not described as being low enough to cause hypoglycemia, and the symptoms are more consistent with **increased ICP**.
- Symptoms of hypoglycemia (e.g., tremors, sweating, hunger, anxiety) are different from the patient's current presentation of confusion and severe headache.
*Pupillary constriction*
- **Pupillary constriction** (miosis) is typically not associated with cerebral edema; instead, **pupillary dilation** (mydriasis) can occur with severe increase in ICP due to uncal herniation.
- The combination of bradycardia, irregular respiration, and hypertension (Cushing's triad) is indicative of increased ICP, which would likely cause pupillary changes related to brainstem compression.
*Pancreatitis*
- Pancreatitis is a known complication of DKA, but it typically presents with **severe abdominal pain**, nausea, and vomiting, rather than cerebral symptoms.
- Although the patient had DKA, the current neurological symptoms point directly to an intracranial process rather than an abdominal issue.
*Peripheral edema*
- **Peripheral edema** results from fluid accumulation in peripheral tissues and is not a direct consequence or expected finding in cerebral edema.
- While fluid administration can cause some peripheral fluid retention, it typically does not lead to the acute neurological deterioration seen in this patient.
Diabetes mellitus pathology US Medical PG Question 2: A 13-year-old girl presents after losing consciousness during class 30 minutes ago. According to her friends, she was doing okay since morning, and nobody noticed anything abnormal. The patient’s mother says that her daughter does not have any medical conditions. She also says that the patient has always been healthy but has recently lost weight even though she was eating as usual. Her vital signs are a blood pressure of 100/78 mm Hg, a pulse of 89/min, and a temperature of 37.2°C (99.0°F). Her breathing is rapid but shallow. Fingerstick glucose is 300 mg/dL. Blood is drawn for additional lab tests, and she is started on intravenous insulin and normal saline. Which of the following HLA subtypes is associated with this patient’s most likely diagnosis?
- A. DR3 (Correct Answer)
- B. A3
- C. B8
- D. DR5
- E. B27
Diabetes mellitus pathology Explanation: ***DR3***
- The patient's presentation with **recent weight loss despite normal eating**, rapid but shallow breathing (**Kussmaul respiration** hinting at **metabolic acidosis**), elevated blood glucose (300 mg/dL), and loss of consciousness strongly suggests **Type 1 Diabetes Mellitus (T1DM)** presenting as **diabetic ketoacidosis (DKA)**.
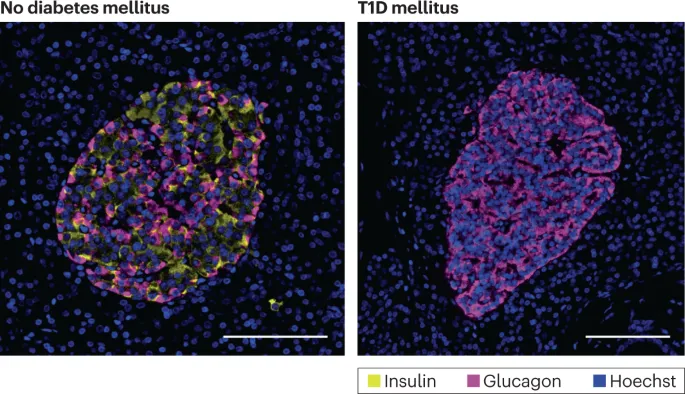
- **HLA-DR3** and **HLA-DR4** are the primary genetic markers most strongly associated with an increased susceptibility to Type 1 Diabetes Mellitus, an **autoimmune disease** affecting pancreatic beta cells.
- **HLA-DR3** is the most direct answer as it is one of the two strongest HLA-DR associations with T1DM.
*A3*
- **HLA-A3** is primarily associated with **hemochromatosis**, a disorder of iron metabolism, and is not a common genetic marker for Type 1 Diabetes Mellitus.
- The symptoms described in the patient (weight loss, hyperglycemia, DKA) are not characteristic of hemochromatosis.
*B8*
- **HLA-B8** is actually associated with Type 1 Diabetes Mellitus as part of the **extended haplotype A1-B8-DR3**, which shows strong linkage disequilibrium.
- However, **HLA-B8 is not as directly or specifically associated with T1DM** as the HLA-DR subtypes (DR3 and DR4), which are considered the primary genetic markers.
- When asking about HLA subtypes associated with T1DM, **DR3 or DR4** are the best answers as they show the strongest and most direct association.
- HLA-B8 is also associated with other autoimmune conditions like **myasthenia gravis** and **Graves' disease**.
*DR5*
- While part of the **HLA-DR family**, **HLA-DR5** is less commonly associated with **Type 1 Diabetes Mellitus** compared to DR3 and DR4.
- This subtype is more frequently linked with conditions like **pernicious anemia** or increased risk of certain infections.
*B27*
- **HLA-B27** is strongly associated with **seronegative spondyloarthropathies**, such as **ankylosing spondylitis** and **reactive arthritis**.
- It has no known direct association with **Type 1 Diabetes Mellitus**.
Diabetes mellitus pathology US Medical PG Question 3: An 18-year-old Caucasian female presents to your clinic because of a recent increase in thirst and hunger. Urinalysis demonstrates elevated glucose. The patient's BMI is 20. Which of the following is the most common cause of death in persons suffering from this patient's illness?
- A. Coma
- B. Peripheral neuropathy
- C. Infection
- D. Renal failure
- E. Myocardial infarction (Correct Answer)
Diabetes mellitus pathology Explanation: ***Myocardial infarction***
- **Cardiovascular disease, particularly myocardial infarction, is the leading cause of death in Type 1 Diabetes Mellitus**, accounting for approximately 40% of mortality.
- Patients with Type 1 diabetes develop **accelerated atherosclerosis** due to chronic hyperglycemia, dyslipidemia, endothelial dysfunction, and increased oxidative stress.
- Even young patients with T1DM have significantly elevated cardiovascular risk compared to age-matched controls, with risk increasing proportionally with disease duration and glycemic control.
- While acute complications like DKA are immediately life-threatening, modern medical management has reduced DKA mortality to <1%, making chronic cardiovascular complications the predominant cause of death.
*Coma*
- **Diabetic ketoacidosis (DKA)** leading to coma is indeed a serious acute complication of Type 1 diabetes.
- However, with contemporary medical care and improved access to insulin, DKA mortality is less than 1% in developed countries.
- While DKA may be the presenting feature or an immediate threat, it is not the most common cause of death over the lifetime of T1DM patients.
*Peripheral neuropathy*
- Diabetic peripheral neuropathy is a common chronic complication affecting up to 50% of long-standing diabetics.
- While it significantly impacts quality of life and can lead to foot ulcers, infections, and amputations, it is not a direct cause of death.
- Autonomic neuropathy can contribute to sudden cardiac death, but this is still categorized under cardiovascular mortality.
*Infection*
- Diabetes does increase susceptibility to certain infections due to impaired neutrophil function, reduced chemotaxis, and hyperglycemia promoting bacterial growth.
- While infections can be serious (e.g., necrotizing fasciitis, mucormycosis), they are not the leading cause of mortality in T1DM.
- Infection-related deaths are far less common than cardiovascular deaths.
*Renal failure*
- **Diabetic nephropathy** is the second most common cause of death in Type 1 diabetes, affecting approximately 20-30% of patients.
- End-stage renal disease develops over many years and contributes significantly to mortality.
- However, cardiovascular disease remains more common, and many patients with diabetic nephropathy ultimately die from cardiovascular events rather than renal failure alone.
Diabetes mellitus pathology US Medical PG Question 4: A patient presents to the emergency room in an obtunded state. The patient is a known nurse within the hospital system and has no history of any medical problems. A finger stick blood glucose is drawn showing a blood glucose of 25 mg/dL.
The patient's daughter immediately arrives at the hospital stating that her mother has been depressed recently and that she found empty syringes in the bathroom at the mother's home. Which of the following is the test that will likely reveal the diagnosis?
- A. Fasting blood glucose
- B. Urine metanephrines
- C. Genetic testing
- D. 24 hr cortisol
- E. C-peptide level (Correct Answer)
Diabetes mellitus pathology Explanation: ***C-peptide level***
- A **low C-peptide level** in the presence of **hypoglycemia** and high insulin levels confirms the diagnosis of **exogenous insulin administration** (factitious hypoglycemia).
- **C-peptide** is cleaved from **proinsulin** in equimolar amounts with endogenous insulin, making it an excellent marker to differentiate endogenous insulin production from exogenous insulin injection.
- In this case: **Low C-peptide + High insulin + Hypoglycemia** = exogenous insulin administration.
*Fasting blood glucose*
- The patient already has documented **hypoglycemia (25 mg/dL)**, so an additional fasting blood glucose test would not provide further diagnostic information about the **cause** of hypoglycemia.
- A single fasting blood glucose level indicates current glucose status but **does not differentiate** between endogenous insulin overproduction (insulinoma) and exogenous insulin administration.
*Urine metanephrines*
- **Urine metanephrines** are used to diagnose **pheochromocytoma**, a catecholamine-secreting tumor of the adrenal medulla.
- Pheochromocytoma presents with **hypertension**, palpitations, headaches, and diaphoresis—**not hypoglycemia**.
- This test is not relevant to the differential diagnosis of hypoglycemia.
*Genetic testing*
- **Genetic testing** might be considered for rare hereditary causes of hypoglycemia, such as congenital hyperinsulinism or genetic insulinoma syndromes (e.g., MEN1).
- Given the clinical context (depressed nurse with access to insulin and empty syringes found at home), **exogenous insulin administration** is far more likely than a genetic condition.
- Genetic testing is not the appropriate initial diagnostic step in this scenario.
*24 hr cortisol*
- A **24-hour urinary cortisol** test is used to diagnose **Cushing's syndrome** (cortisol excess), not hypoglycemia.
- While **adrenal insufficiency** (cortisol deficiency) can cause hypoglycemia, it typically presents with **hypotension**, **hyponatremia**, **hyperkalemia**, and **hyperpigmentation**—features not described in this case.
- The clinical presentation strongly suggests insulin-related hypoglycemia rather than adrenal insufficiency.
Diabetes mellitus pathology US Medical PG Question 5: A 76-year-old female with a past medical history of obesity, coronary artery disease status post stent placement, hypertension, hyperlipidemia, and insulin dependent diabetes comes to your outpatient clinic for regular checkup. She has not been very adherent to her diabetes treatment regimen. She has not been checking her sugars regularly and frequently forgets to administer her mealtime insulin. Her Hemoglobin A1c three months ago was 14.1%. As a result of her diabetes, she has developed worsening diabetic retinopathy and neuropathy. Based on her clinical presentation, which of the following is the patient most at risk for developing?
- A. Stress incontinence
- B. Hemorrhoids
- C. Rectal prolapse
- D. Overflow incontinence (Correct Answer)
- E. Uterine prolapse
Diabetes mellitus pathology Explanation: ***Overflow incontinence***
- The patient's **poorly controlled diabetes** can lead to **diabetic autonomic neuropathy**, affecting bladder function and causing **neurogenic bladder**.
- This results in the bladder not emptying completely, leading to **urinary retention** and leakage as the bladder overfills, which defines **overflow incontinence**.
*Stress incontinence*
- This type of incontinence is typically caused by **weakening of pelvic floor muscles** and **urethral sphincter**, leading to leakage with increased abdominal pressure (e.g., coughing, sneezing).
- While obesity is a risk factor, the patient's severe, uncontrolled diabetes points more strongly to neuropathy affecting bladder emptying rather than just sphincter weakness.
*Hemorrhoids*
- Hemorrhoids are **swollen veins in the rectum or anus**, often associated with straining during bowel movements, chronic constipation, or obesity.
- While common in this demographic, there is no direct link between uncontrolled diabetes and the development of hemorrhoids.
*Rectal prolapse*
- Rectal prolapse involves the **protrusion of the rectum through the anus**, often due to weakened pelvic floor muscles or chronic straining.
- Although the patient's age and obesity could be contributing factors, poorly controlled diabetes does not directly cause rectal prolapse.
*Uterine prolapse*
- Uterine prolapse occurs when the **uterus descends into the vagina**, typically due to weakened pelvic floor muscles, often following childbirth or with age and obesity.
- Uncontrolled diabetes does not directly cause uterine prolapse, although shared risk factors like obesity might be present.
Diabetes mellitus pathology US Medical PG Question 6: A 36-year-old primigravida presents to her obstetrician for antenatal care. She is at 24 weeks of gestation and does not have any current complaint except for occasional leg cramps. She does not smoke or drink alcohol. Family history is irrelevant. Her temperature is 36.9°C (98.42°F), blood pressure is 100/60 mm Hg, and pulse of 95/minute. Her body mass index is 21 kg/m² (46 pounds/m²). Physical examination reveals a palpable uterus above the umbilicus with no other abnormalities. Which of the following screening tests is suitable for this patient?
- A. Fasting and random glucose testing for gestational diabetes mellitus
- B. HbA1C for gestational diabetes mellitus
- C. Oral glucose tolerance test for gestational diabetes mellitus (Correct Answer)
- D. Complete blood count for iron deficiency anemia
- E. Wet mount microscopy of vaginal secretions for bacterial vaginosis
Diabetes mellitus pathology Explanation: ***Oral glucose tolerance test for gestational diabetes mellitus***
- The **oral glucose tolerance test (OGTT)**, typically performed between **24 and 28 weeks of gestation**, is the gold standard for screening and diagnosing **gestational diabetes mellitus (GDM)**. This patient is at 24 weeks, making it the appropriate time for this screening.
- GDM, if undiagnosed and untreated, can lead to significant maternal and fetal complications, including **macrosomia**, **preeclampsia**, **neonatal hypoglycemia**, and **shoulder dystocia**.
*Fasting and random glucose testing for gestational diabetes mellitus*
- While **fasting** or **random glucose** values can indicate hyperglycemia, they are **not sensitive or specific enough** on their own to reliably screen for or diagnose GDM.
- A single elevated reading might prompt further testing, but it's not the primary or most suitable screening method.
*HbA1C for gestational diabetes mellitus*
- **HbA1c** reflects **average blood glucose levels over the past 2-3 months** and is primarily used for diagnosing and monitoring **pre-existing diabetes** or assessing glycemic control in non-pregnant individuals.
- Due to the **physiological changes in red blood cell turnover during pregnancy** and the acute onset nature of GDM, HbA1c is **not recommended** as a first-line screening tool for GDM.
*Complete blood count for iron deficiency anemia*
- While **complete blood count (CBC)** is a routine prenatal screening test to check for **anemia**, it is typically done earlier in pregnancy and again in the third trimester. There are no specific symptoms in this patient that strongly suggest immediate concern for anemia beyond routine.
- The question specifically asks for the "most suitable" screening test at this gestational age, and the **GDM screening** takes precedence given the timing.
*Wet mount microscopy of vaginal secretions for bacterial vaginosis*
- There are **no symptoms of vaginal infection** (e.g., unusual discharge, itching, odor) mentioned in the patient's presentation that would warrant immediate screening for **bacterial vaginosis (BV)** at this visit.
- While BV can be associated with adverse pregnancy outcomes, routine asymptomatic screening by wet mount is **not universally recommended** at 24 weeks gestation without other indications.
Diabetes mellitus pathology US Medical PG Question 7: A 43-year-old woman comes to the physician for an annual health maintenance examination. On questioning, she has had fatigue and headaches for the last month. A few weeks ago, she had to have her wedding ring resized because it had become too small for her finger. She has mild persistent asthma and anxiety disorder. She drinks 2–3 glasses of red wine per night and has smoked one pack of cigarettes daily for 16 years. She works a desk job in accounting and has recently been working long hours due to an upcoming company merger. Her father has a history of a pituitary adenoma. Current medications include alprazolam, a fluticasone inhaler, and an albuterol inhaler. She is 160 cm (5 ft 3 in) tall and weighs 81.6 kg (180 lb); her BMI is 32 kg/m2. Her temperature is 37.2°C (99°F), pulse is 92/min, and blood pressure is 132/80 mm Hg. Examination shows no abnormalities. Fasting laboratory studies show:
Hemoglobin 13 g/dL
Serum
Na+ 135 mEq/L
K+
4.6 mEq/L
Cl- 105 mEq/L
HCO3- 22 mEq/L
Urea nitrogen 17 mg/dL
Glucose 160 mg/dL
Creatinine 0.9 mg/dL
Which of the following is the most likely underlying mechanism of this patient's hyperglycemia?
- A. Decreased insulin production
- B. Adverse effect of medication
- C. Stress
- D. Insulin resistance (Correct Answer)
- E. Hypersecretion of ACTH
Diabetes mellitus pathology Explanation: ***Insulin resistance***
- The patient's **obesity (BMI 32 kg/m2)**, **sedentary lifestyle**, and **fasting hyperglycemia** (glucose 160 mg/dL) indicate **insulin resistance**, which is the underlying mechanism of hyperglycemia in **type 2 diabetes**.
- The **ring resizing due to finger enlargement**, **fatigue**, **headaches**, and **family history of pituitary adenoma** raise suspicion for **acromegaly** (growth hormone excess), which also causes hyperglycemia through **insulin resistance** - growth hormone antagonizes insulin action at peripheral tissues.
- Regardless of whether this represents type 2 diabetes or acromegaly, **insulin resistance is the direct mechanism** causing the hyperglycemia in this patient.
*Decreased insulin production*
- Decreased insulin production is characteristic of **type 1 diabetes** or late-stage type 2 diabetes with beta-cell exhaustion.
- The patient's **obesity** and typical metabolic risk factors suggest **insulin resistance** rather than decreased production as the primary mechanism.
- No clinical features suggest autoimmune destruction or significant pancreatic damage.
*Adverse effect of medication*
- The patient's medications (**alprazolam**, **fluticasone inhaler**, **albuterol**) are unlikely to cause significant fasting hyperglycemia.
- While high-dose systemic **corticosteroids** can cause hyperglycemia, **inhaled fluticasone** at typical asthma doses has minimal systemic absorption and is not a common cause of sustained hyperglycemia.
- **Alprazolam** and **albuterol** do not typically cause hyperglycemia.
*Stress*
- **Acute stress** can transiently elevate blood glucose through counter-regulatory hormones (cortisol, catecholamines).
- However, the **fasting glucose of 160 mg/dL** suggests a chronic metabolic derangement rather than acute stress response alone.
- Work-related stress may be a contributing factor but is not the primary underlying mechanism.
*Hypersecretion of ACTH*
- **ACTH hypersecretion** (Cushing's disease) causes excess cortisol production, leading to hyperglycemia, weight gain, and fatigue.
- This patient lacks classic features of Cushing's syndrome: **central obesity with thin extremities**, **moon facies**, **buffalo hump**, **purple striae**, **skin thinning**, or **easy bruising**.
- While the patient is obese, the distribution appears generalized rather than the characteristic centripetal pattern of Cushing's syndrome.
Diabetes mellitus pathology US Medical PG Question 8: A 21-year-old woman comes to the physician for a routine physical examination. She feels well. She is 163 cm (5 ft 4 in) tall and weighs 54 kg (120 lb); BMI is 20.3 kg/m2. Physical examination shows no abnormalities. Her fasting serum glucose concentration is 132 mg/dL. Serum insulin concentration 30 minutes after oral glucose administration is 20 mIU/L (N: 30–230). Her hemoglobin A1C concentration is 7.1%. After a thorough workup, the physician concludes that the patient has a chronic condition that can likely be managed with diet only and that she is not at a significantly increased risk of micro- or macrovascular complications. Which of the following is the most likely cause of the patient's condition?
- A. Mutation in hepatocyte nuclear factor 1
- B. Defect in expression of glucokinase gene (Correct Answer)
- C. Resistance to insulin-mediated glucose uptake
- D. Increased endogenous cortisol production
- E. Autoantibodies to pancreatic beta cells
Diabetes mellitus pathology Explanation: ***Defect in expression of glucokinase gene***
- The patient's presentation with **mild, stable hyperglycemia** (fasting glucose 132 mg/dL, HbA1c 7.1%) since a young age, without features of typical type 1 or type 2 diabetes, is highly suggestive of **Maturity-Onset Diabetes of the Young (MODY)**.
- Specifically, **MODY2**, caused by a defect in the **glucokinase gene (GCK-MODY)**, is characterized by a slightly elevated fasting glucose that is often present from birth, minimally progressive, and typically managed with diet due to the negligible risk of complications.
*Mutation in hepatocyte nuclear factor 1*
- Mutations in **hepatocyte nuclear factor 1-alpha (HNF1A-MODY or MODY3)** and **HNF4A (HNF4A-MODY or MODY1)** are also common forms of MODY, but they usually lead to more progressive hyperglycemia and often require sulfonylurea treatment due to impaired insulin secretion.
- These forms of MODY are associated with a higher risk of diabetic complications compared to GCK-MODY, which contradicts the physician's conclusion of a low complication risk.
*Resistance to insulin-mediated glucose uptake*
- This describes **insulin resistance**, a hallmark of **Type 2 Diabetes Mellitus**.
- However, the patient's normal BMI (20.3 kg/m2) and relatively low insulin level after glucose challenge (20 mIU/L, within range of "normal" for some labs, but significantly lower than the expected robust response in early T2DM) make significant insulin resistance unlikely as the primary cause.
*Increased endogenous cortisol production*
- Increased cortisol, as seen in **Cushing's syndrome**, can cause hyperglycemia due to increased gluconeogenesis and insulin resistance.
- However, the patient presents with no other signs or symptoms of Cushing's syndrome (e.g., central obesity, moon facies, striae, hypertension), making this diagnosis improbable.
*Autoantibodies to pancreatic beta cells*
- The presence of autoantibodies (e.g., anti-GAD, islet cell antibodies) is characteristic of **Type 1 Diabetes Mellitus**, an autoimmune condition leading to destruction of pancreatic beta cells and usually presents with more severe hyperglycemia and insulin dependency.
- The patient's mild, stable hyperglycemia and the physician's conclusion of a low complication risk and diet-only management contradict the typical progression and management of Type 1 Diabetes.
Diabetes mellitus pathology US Medical PG Question 9: A 28-year-old woman comes to the physician because of a 1-year history of intermittent buzzing in both her ears. She says she sometimes has episodes of mild dizziness which resolve spontaneously. She has a 15-year history of type 1 diabetes mellitus and episodes of low back pain. She does not smoke or drink alcohol. Current medications include insulin and aspirin. She works as a trombonist for a symphony orchestra. Her vital signs are within normal limits. On otoscopic examination, the tympanic membrane appears normal. Bone conduction is greater than air conduction in both ears. Weber test shows no lateralization. Which of the following is the most likely diagnosis?
- A. Presbycusis
- B. Diabetic otopathy
- C. Drug-induced ototoxicity
- D. Otosclerosis (Correct Answer)
- E. Endolymphatic hydrops
Diabetes mellitus pathology Explanation: ***Otosclerosis***
- The combination of **conductive hearing loss** (**bone conduction > air conduction**), **intermittent buzzing (tinnitus)**, and mild dizziness in a young adult is characteristic of otosclerosis. The normal tympanic membrane further supports this diagnosis as it indicates no external or middle ear infection/perforation.
- **Weber test shows no lateralization** because the conductive hearing loss is **symmetric and bilateral**, meaning both ears are equally affected.
*Presbycusis*
- This is an age-related **sensorineural hearing loss** that typically affects older individuals, usually over 50-60 years old, not a 28-year-old.
- Presbycusis usually presents with **air conduction > bone conduction** (sensorineural pattern) and affects high frequencies first, not conductive hearing loss.
*Diabetic otopathy*
- While patients with long-standing diabetes can develop hearing loss, it is typically a **sensorineural hearing loss** due to microvascular damage, not conductive hearing loss.
- The symptoms in diabetic otopathy usually involve high-frequency hearing loss and are not typically associated with bone conduction exceeding air conduction.
*Drug-induced ototoxicity*
- **Aspirin** can cause tinnitus and sensorineural hearing loss, but the presented case demonstrates **conductive hearing loss** (bone conduction > air conduction).
- Aspirin ototoxicity typically causes reversible sensorineural hearing loss and tinnitus, not the conductive pattern seen here.
*Endolymphatic hydrops*
- Also known as **Meniere's disease**, this condition causes episodic **vertigo, tinnitus, and sensorineural hearing loss**.
- The hearing loss is typically **sensorineural** and often fluctuating, while this patient presents with signs of **conductive hearing loss**.
Diabetes mellitus pathology US Medical PG Question 10: A 68-year-old man comes to the physician for a routine health maintenance examination. Over the past six months, he has had an increase in the frequency of his bowel movements and occasional bloody stools. He has hypertension, coronary artery disease, and chronic obstructive pulmonary disease. He has smoked one pack of cigarettes daily for 40 years. His current medications include aspirin, lisinopril, and salmeterol. His temperature is 37°C (98.6°F), pulse is 75/min, and blood pressure is 128/75 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no murmurs, rubs, or gallops. The abdomen is soft with no organomegaly. Digital rectal examination shows a large internal hemorrhoid. Test of the stool for occult blood is positive. Which of the following is the most appropriate next step in the management of this patient?
- A. Capsule endoscopy
- B. Rubber band ligation
- C. Hemorrhoidectomy
- D. Barium enema
- E. Colonoscopy (Correct Answer)
Diabetes mellitus pathology Explanation: ***Colonoscopy***
- This patient presents with **changes in bowel habits** (increased frequency) and **rectal bleeding** (bloody stools, positive fecal occult blood test), which are classic alarm symptoms for **colorectal cancer**.
- A **colonoscopy** is the most appropriate next step because it allows for direct visualization of the entire colon, biopsy of suspicious lesions, and removal of polyps, which is crucial for diagnosing or ruling out colorectal cancer and other colon pathologies.
*Capsule endoscopy*
- **Capsule endoscopy** is primarily used to evaluate the **small bowel** for obscure GI bleeding, Crohn's disease, or small bowel tumors.
- It is **not effective** for evaluating the colon as it cannot be controlled to visualize the colonic lining thoroughly and cannot perform biopsies.
*Rubber band ligation*
- **Rubber band ligation** is a procedure used to treat **hemorrhoids**, particularly problematic internal hemorrhoids.
- While the patient has an internal hemorrhoid, his new onset of bowel changes and bloody stools warrants a more comprehensive evaluation to rule out other serious conditions like **colorectal cancer** before attributing symptoms solely to hemorrhoids, especially given his age and risk factors.
*Hemorrhoidectomy*
- **Hemorrhoidectomy** is a surgical procedure for treating severe or refractory hemorrhoids.
- Similar to rubber band ligation, performing a hemorrhoidectomy without a prior **colonoscopy** would be inappropriate given the patient's alarm symptoms, as it might delay the diagnosis of a more serious underlying condition.
*Barium enema*
- A **barium enema** is a radiological study that can identify large polyps or masses in the colon, but it has **lower sensitivity** than colonoscopy, especially for smaller lesions.
- It **does not allow for biopsy** of suspicious areas or removal of polyps, which limits its diagnostic and therapeutic utility compared to colonoscopy for these symptoms.
More Diabetes mellitus pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.