Adrenal medullary disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Adrenal medullary disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Adrenal medullary disorders US Medical PG Question 1: A 3-year-old boy presents to the clinic for evaluation of leg pain. This has been persistent for the past 3 days and accompanied by difficulty walking. He has also had some erythema and ecchymoses in the periorbital region over the same time period. The vital signs are unremarkable. The physical exam notes the above findings, as well as some swelling of the upper part of the abdomen. The laboratory results are as follows:
Erythrocyte count 3.3 million/mm3
Leukocyte count 3,000/mm3
Neutrophils 54%
Eosinophils 1%
Basophils 1%
Lymphocytes 43%
Monocytes 3%
Platelet count 80,000/mm3
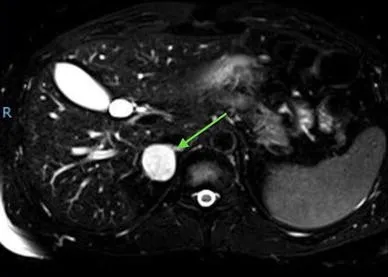
A magnetic resonance image (MRI) scan of the abdomen shows a mass of adrenal origin. Which of the following is the most likely cause of this patient's symptoms?
- A. Hepatoblastoma
- B. Rhabdomyosarcoma
- C. Neuroblastoma (Correct Answer)
- D. Wilms tumor
- E. Retinoblastoma
Adrenal medullary disorders Explanation: ***Neuroblastoma***
- This diagnosis is strongly suggested by the combination of **an adrenal mass**, **periorbital ecchymoses** (often called "raccoon eyes" due to orbital metastases), and **bone pain/difficulty walking** (indicating bone marrow involvement).
- The **pancytopenia** (low erythrocyte, leukocyte, and platelet counts) further supports widespread bone marrow infiltration by metastatic disease, a common feature of advanced neuroblastoma.
*Hepatoblastoma*
- This is a primary **liver tumor** that typically presents with an abdominal mass and elevated alpha-fetoprotein.
- It does not typically cause periorbital ecchymoses or widespread bone pain/marrow suppression as seen in this patient.
*Rhabdomyosarcoma*
- This is a **soft tissue sarcoma** that can occur in various locations but does not commonly originate in the adrenal gland or present with the classic periorbital ecchymoses of neuroblastoma.
- While it can metastasize, the specific pattern of an adrenal mass with orbital and bone marrow involvement is less typical.
*Wilms tumor*
- This is a **kidney tumor** (nephroblastoma) that usually presents as a palpable abdominal mass and can sometimes cause hypertension or hematuria.
- It originates in the kidney, not the adrenal gland, and does not typically cause periorbital ecchymoses or widespread bone marrow metastasis leading to pancytopenia.
*Retinoblastoma*
- This is a **malignant tumor of the retina** in the eye, usually presenting with leukocoria (white pupillary reflex) or strabismus.
- It does not present with an adrenal mass, leg pain, or periorbital ecchymoses, although genetic predisposition can be associated with other cancers.
Adrenal medullary disorders US Medical PG Question 2: A 35-year-old woman presents with increased anxiety and a reeling sensation. Her complaint started 30 minutes ago with increased sweating and palpitations and is gradually worsening. On examination, the blood pressure was found to be 194/114 mm Hg. She had normal blood pressure at the local pharmacy 5 days ago. She currently works as an event manager and her job involves a lot of stress. The family history is significant for thyroid carcinoma in her father. Which of the following is most likely in this person?
- A. Increased urine metanephrines (Correct Answer)
- B. Decreased C-peptide
- C. Decreased hemoglobin
- D. Decreased TSH levels
- E. Increased serum serotonin
Adrenal medullary disorders Explanation: ***Increased urine metanephrines***
- The patient's symptoms (anxiety, reeling sensation, sweating, palpitations, and paroxysmal hypertension) are highly suggestive of a **pheochromocytoma**, which is a tumor of the adrenal medulla that secretes catecholamines.
- **Metanephrines** (metabolism products of catecholamines) are often elevated in urine and plasma samples from patients with pheochromocytoma, making this the most likely finding.
*Decreased C-peptide*
- **Decreased C-peptide** levels are indicative of reduced endogenous insulin production, typically seen in type 1 diabetes, which does not align with the patient's acute presentation of paroxysmal hypertension and anxiety.
- Her symptoms are not consistent with **hypoglycemia** or **diabetes mellitus**.
*Decreased hemoglobin*
- **Decreased hemoglobin** indicates anemia, which would present with fatigue, pallor, and shortness of breath, not the acute hypertensive crisis and anxiety described.
- There is no clinical information in the vignette to suggest **blood loss** or **red blood cell destruction**.
*Decreased TSH levels*
- **Decreased TSH levels** would suggest hyperthyroidism, which can cause anxiety and palpitations, but the sudden onset and extreme hypertension (194/114 mm Hg) are more characteristic of a **catecholamine surge** than typical hyperthyroidism.
- While there is a family history of **thyroid carcinoma**, the acute presentation points away from purely thyroid-related issues as the primary cause.
*Increased serum serotonin*
- **Increased serum serotonin** is associated with carcinoid syndrome, which typically presents with flushing, diarrhea, bronchospasm, and valvular heart disease, not the predominant features of anxiety, palpitations, and paroxysmal hypertension seen in this patient.
- The symptoms are more consistent with an acute release of **catecholamines**, not serotonin.
Adrenal medullary disorders US Medical PG Question 3: A researcher is studying receptors that respond to epinephrine in the body and discovers a particular subset that is expressed in presynaptic adrenergic nerve terminals. She discovers that upon activation, these receptors will lead to decreased sympathetic nervous system activity. She then studies the intracellular second messenger changes that occur when this receptor is activated. She records these changes and begins searching for analogous receptor pathways. Which of the following receptors would cause the most similar set of intracellular second messenger changes?
- A. Muscarinic cholinoreceptors in the gastrointestinal tract
- B. Growth hormone receptors in the musculoskeletal system
- C. Vasopressin receptors in the kidney
- D. Dopamine receptors in the brain (Correct Answer)
- E. Aldosterone receptors in the kidney
Adrenal medullary disorders Explanation: ***Dopamine receptors in the brain***
- The described presynaptic receptors for epinephrine that decrease sympathetic activity are **alpha-2 adrenergic receptors**, which are **G inhibitory protein (Gi)-coupled receptors**.
- Gi-coupled receptors **inhibit adenylyl cyclase**, leading to a **decrease in intracellular cAMP**, a signaling pathway shared by **D2 dopamine receptors**.
*Muscarinic cholinoreceptors in the gastrointestinal tract*
- Most muscarinic receptors (M1 and M3) in the GI tract are **Gq-coupled**, leading to an **increase in phospholipase C (PLC) activity**, ultimately increasing intracellular **IP3 and DAG** and promoting smooth muscle contraction.
- This mechanism is distinct from the **Gi-mediated inhibition of cAMP** described for the presynaptic adrenergic receptor.
*Growth hormone receptors in the musculoskeletal system*
- Growth hormone receptors are **tyrosine kinase-associated receptors** (specifically, they are linked to **JAK/STAT pathways**), not G protein-coupled receptors.
- Their intracellular signaling involves **protein phosphorylation cascades**, which are fundamentally different from second messenger changes involving cAMP.
*Vasopressin receptors in the kidney*
- Vasopressin (ADH) acts on **V2 receptors** in the kidney, which are **G stimulatory protein (Gs)-coupled receptors**.
- Activation of V2 receptors leads to an **increase in adenylyl cyclase activity** and thus an **increase in intracellular cAMP**, the opposite effect of the described Gi-coupled receptor.
*Aldosterone receptors in the kidney*
- Aldosterone receptors are **intracellular steroid hormone receptors** that directly bind to DNA and regulate gene transcription.
- They do not engage in rapid intracellular second messenger changes like G protein-coupled receptors, but rather alter **protein synthesis** over hours to days.
Adrenal medullary disorders US Medical PG Question 4: A newborn is brought to the pediatric clinic by his mother because she has noticed a swelling in the belly while dressing her baby. On physical examination, the newborn is found to have a non-tender upper abdominal mass. The clinician also noticed absent irises and undescended testes in this baby. A magnetic resonance image (MRI) scan of the abdomen shows a mass of intra-renal origin. Which 1 of the following genetic disorders is most probably the cause of this neonate’s symptoms and signs?
- A. WT-1 missense mutation
- B. Deletion 11-p-13 (Correct Answer)
- C. Duplication of 11-p-15
- D. Amplification of MYCN (N-myc) proto-oncogene
- E. Trisomy 18
Adrenal medullary disorders Explanation: ***Deletion 11-p-13***
* This describes the genetic abnormality associated with **WAGR syndrome**, which stands for **Wilms tumor**, **Aniridia**, **Genitourinary anomalies** (like undescended testes), and **intellectual disability** (though not explicitly mentioned, it's part of the syndrome).
* The presence of a **nephroblastoma (Wilms tumor)**, **absent irises (aniridia)**, and **undescended testes** in a newborn strongly points to WAGR syndrome, caused by a deletion on chromosome 11 at band p13, affecting the *WT1* gene locus.
*WT-1 missense mutation*
* While *WT1* gene mutations are associated with Wilms tumor, a **missense mutation** specifically in *WT1* is more commonly linked to **Denys-Drash syndrome**, which presents with Wilms tumor, diffuse mesangial sclerosis (nephropathy), and male pseudohermaphroditism, but typically *not aniridia*.
* The constellation of symptoms including aniridia and undescended testes together with a Wilms tumor is more characteristic of a larger deletion encompassing *PAX6* (responsible for aniridia) and *WT1*.
*Duplication of 11-p-15*
* A **duplication of 11p15** is associated with **Beckwith-Wiedemann syndrome**, which includes macrosomia, macroglossia, omphalocele, and an increased risk of Wilms tumor.
* However, Beckwith-Wiedemann syndrome does *not* typically present with aniridia or undescended testes as core features.
*Amplification of MYCN (N-myc) proto-oncogene*
* **MYCN amplification** is a significant genetic alteration found in neuroblastoma, a common extracranial solid tumor of childhood, originating from neural crest cells.
* **Neuroblastoma** is distinct from Wilms tumor (which is intra-renal) and does not typically present with the specific features of aniridia or undescended testes as co-occurring symptoms.
*Trisomy 18*
* **Trisomy 18 (Edwards syndrome)** is characterized by severe developmental delays, distinctive facial features, rocker-bottom feet, and various congenital anomalies affecting multiple organ systems (e.g., heart defects, kidney abnormalities, omphalocele).
* While kidney abnormalities can occur, **aniridia** and **isolated undescended testes combined with a Wilms tumor** are not classic features of Trisomy 18.
Adrenal medullary disorders US Medical PG Question 5: A 49-year-old male presents with a primary complaint of several recent episodes of severe headache, sudden anxiety, and a "racing heart". The patient originally attributed these symptoms to stress at work; however, these episodes are becoming more frequent and severe. Laboratory evaluation during such an episode reveals elevated plasma free metanephrines. Which of the following additional findings in this patient is most likely?
- A. Anhidrosis
- B. Diarrhea
- C. Episodic hypertension (Correct Answer)
- D. Hypoglycemia
- E. Decreased 24 hour urine vanillylmandelic acid (VMA) levels
Adrenal medullary disorders Explanation: ***Episodic hypertension***
- The patient's symptoms of severe headache, sudden anxiety, a "racing heart," and **elevated plasma free metanephrines** are classic presentations of a **pheochromocytoma**, a tumor that produces catecholamines. These catecholamines cause **paroxysmal (episodic) hypertension**.
- **Hypertensive episodes** are a hallmark symptom of pheochromocytoma, often triggered by stress, exercise, or changes in body position.
*Anhidrosis*
- **Anhidrosis** (lack of sweating) is not a typical manifestation of pheochromocytoma; rather, patients often experience **diaphoresis (excessive sweating)** due to overstimulation of adrenergic receptors.
- Anhidrosis can be a feature of certain neuropathies or autonomic dysfunction, but it does not align with the hyperadrenergic state described.
*Diarrhea*
- While pheochromocytoma can cause gastrointestinal symptoms due to altered autonomic tone, **diarrhea** is uncommon; **constipation** is more frequently reported because of catecholamine effects on gut motility.
- Diarrhea is more commonly associated with conditions like carcinoid syndrome or irritable bowel syndrome.
*Hypoglycemia*
- **Hypoglycemia** is generally not associated with pheochromocytoma; the excess catecholamines typically promote **glycogenolysis and gluconeogenesis**, leading to **hyperglycemia**.
- Hypoglycemia could be caused by an insulinoma or certain endocrine deficiencies.
*Decreased 24 hour urine vanillylmandelic acid (VMA) levels*
- **Elevated plasma free metanephrines** indicate excessive catecholamine production, which would lead to **elevated 24-hour urine VMA** (a catecholamine metabolite), not decreased levels.
- Decreased VMA levels would suggest conditions with reduced catecholamine production, which contradicts the clinical picture of hyperadrenergic symptoms.
Adrenal medullary disorders US Medical PG Question 6: A 30-year-old man comes to the physician after receiving a high blood pressure reading of 160/90 mm Hg at an annual employee health check-up. During the past few months, the patient has had occasional headaches and mild abdominal pain, both of which were relieved with ibuprofen. He has also had several episodes of heart palpitations. He has no history of serious illness. His mother and father both have hypertension. He has smoked one pack of cigarettes daily for the past 10 years and drinks one glass of wine daily. He occasionally smokes marijuana. He appears pale. His temperature is 36.8°C (98.2°F), pulse is 103/min, and blood pressure is 164/102 mm Hg. Physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 15.3 g/dL
Leukocyte count 7,900/mm3
Platelet count 223,000/mm3
Serum
Na+ 138 mEq/L
K+ 4.6 mEq/L
Cl- 103 mEq/L
Urea nitrogen 14 mg/dL
Glucose 90 mg/dL
Creatinine 0.9 mg/dL
Plasma metanephrines 1.2 nmol/L (N < 0.5 nmol/L)
Urine toxicology screening is positive for tetrahydrocannabinol (THC). Renal doppler shows no abnormalities. A CT scan of the abdomen shows a mass in the left adrenal gland. Which of the following is the most appropriate next step in management of this patient?
- A. Resection of adrenal mass
- B. Phenoxybenzamine (Correct Answer)
- C. Propranolol
- D. Metoprolol
- E. MIBG therapy
Adrenal medullary disorders Explanation: ***Phenoxybenzamine***
- The patient's presentation with **hypertension**, **palpitations**, and significantly elevated **plasma metanephrines** (1.2 nmol/L vs. normal < 0.5 nmol/L), along with an **adrenal mass**, strongly suggests a **pheochromocytoma**.
- **Alpha-blockade** with phenoxybenzamine is the crucial first step to control blood pressure and prevent a **hypertensive crisis** during subsequent surgical resection.
*Resection of adrenal mass*
- While surgical resection is the **definitive treatment** for pheochromocytoma, it should **not be performed before adequate alpha-blockade**.
- **Unprepared surgery** can lead to a fatal hypertensive crisis due to uncontrolled catecholamine release during manipulation of the tumor.
*Propranolol*
- Propranolol is a **non-selective beta-blocker** and should **not be initiated before alpha-blockade** in pheochromocytoma.
- Blocking beta-adrenergic receptors can lead to **unopposed alpha-adrenergic vasoconstriction**, potentially worsening hypertension and causing a crisis.
*Metoprolol*
- Metoprolol is a **selective beta-1 blocker** and, like other beta-blockers, should **not be used before alpha-blockade** in pheochromocytoma.
- While it may have fewer peripheral vasoconstrictive effects than non-selective beta-blockers, the risk of unopposed alpha-stimulation remains significant.
*MIBG therapy*
- **Metaiodobenzylguanidine (MIBG) therapy** is a form of **radiotherapy** used for metastatic or inoperable pheochromocytoma/paraganglioma.
- It is **not the initial management** for a resectable adrenal mass in a patient with a newly diagnosed pheochromocytoma.
Adrenal medullary disorders US Medical PG Question 7: A 43-year-old male with a history of thyroid cancer status post total thyroidectomy presents to his primary care physician after repeated bouts of headaches. His headaches are preceded by periods of anxiety, palpitations, and sweating. The patient says he is unable to pinpoint any precipitating factors and instead says the events occur without warning. Of note, the patient's father and uncle also have a history of thyroid cancer. On exam his vitals are: T 36.8 HR 87, BP 135/93, RR 14, and O2 Sat 100% on room air. The patient's TSH is within normal limits, and he reports taking his levothyroxine as prescribed. What is the next best step in diagnosing this patient's chief complaint?
- A. 24-hour urine free cortisol
- B. Plasma aldosterone/renin ratio
- C. Abdominal CT scan with and without IV contrast
- D. Plasma fractionated metanephrines (Correct Answer)
- E. High dose dexamethasone suppression test
Adrenal medullary disorders Explanation: ***Plasma fractionated metanephrines***
- The patient's symptoms of **anxiety, palpitations, sweating, and headaches** occurring in discrete "attacks" are classic for a **pheochromocytoma**, a tumor that secretes catecholamines.
- Given the patient's and his family's history of **thyroid cancer**, specifically likely **medullary thyroid cancer** due to the familial link, there is a high suspicion for **Multiple Endocrine Neoplasia type 2 (MEN2)**, which commonly includes pheochromocytoma. **Plasma fractionated metanephrines** are the most sensitive screening test for pheochromocytoma.
*24-hour urine free cortisol*
- This test is used to detect **Cushing's syndrome**, which involves excessive cortisol production.
- Although Cushing's can cause **hypertension**, the paroxysmal symptoms of anxiety, palpitations, and sweating are not typical of Cushing's syndrome.
*Plasma aldosterone/renin ratio*
- This ratio is used to screen for **primary hyperaldosteronism**, a cause of secondary hypertension.
- While the patient has **hypertension (135/93 mm Hg)**, his symptom complex of episodic anxiety, palpitations, and sweating is not characteristic of primary hyperaldosteronism.
*Abdominal CT scan with and without IV contrast*
- An abdominal CT scan can visualize adrenal masses, but it is typically performed *after* biochemical confirmation of a pheochromocytoma to localize the tumor.
- Performing imaging before biochemical testing risks incidentalomas or missing a biochemically active but small tumor, and it is not the most appropriate *next step* in diagnosis given the strong clinical suspicion.
*High dose dexamethasone suppression test*
- This test is specifically used to differentiate between **Cushing's disease** (pituitary ACTH excess) and other causes of Cushing's syndrome.
- The patient's symptoms are not consistent with excessive cortisol production, making this test inappropriate for his chief complaint.
Adrenal medullary disorders US Medical PG Question 8: A 51-year-old African American man with a history of poorly controlled hypertension presents to the emergency room with blurry vision and dyspnea. He reports rapid-onset blurred vision and difficulty breathing 4 hours prior to presentation. He takes lisinopril, hydrochlorothiazide, and spironolactone but has a history of poor medication compliance. He has a 50 pack-year smoking history and drinks 4-6 shots of vodka per day. His temperature is 99.2°F (37.3°C), blood pressure is 195/115 mmHg, pulse is 85/min, and respirations are 20/min. On exam, he is ill-appearing and pale. He is intermittently responsive and oriented to person but not place or time. Fundoscopic examination reveals swelling of the optic disc with blurred margins. A biopsy of this patient’s kidney would most likely reveal which of the following?
- A. Concentrically thickened arteriolar tunica media with abundant nuclei (Correct Answer)
- B. Calcific deposits in the arterial media without luminal narrowing
- C. Fibrous atheromatous plaques in the arterial intima
- D. Anuclear arteriolar thickening
- E. Endothelial proliferation and luminal narrowing with a chronic inflammatory infiltrate
Adrenal medullary disorders Explanation: ***Concentrically thickened arteriolar tunica media with abundant nuclei***
- This describes **hyperplastic arteriolosclerosis**, a hallmark of **malignant hypertension**, characterized by severe, rapid-onset blood pressure elevation leading to acute organ damage.
- The patient's **blood pressure of 195/115 mmHg**, **blurry vision** (due to optic disc swelling), and **dyspnea** (suggesting pulmonary edema or cardiac involvement) are classic symptoms of malignant hypertension, which causes "onion-skinning" of arterioles.
*Calcific deposits in the arterial media without luminal narrowing*
- This describes **Mönckeberg arteriolosclerosis**, or medial calcific sclerosis, which involves calcification of the tunica media in muscular arteries.
- It typically occurs in older individuals and is usually **clinically silent** unless complicated by atherosclerosis, and does not cause malignant hypertension.
*Fibrous atheromatous plaques in the arteriolar intima*
- This describes **atherosclerosis**, which involves the formation of plaques in larger arteries, not typically in arterioles, and is a chronic process.
- While the patient has risk factors for atherosclerosis (smoking, hypertension), the acute severe presentation points to a microvascular pathology.
*Anuclear arteriolar thickening*
- This describes **hyaline arteriolosclerosis**, associated with benign (non-malignant) hypertension or diabetes, where plasma proteins leak into the vessel walls, causing uniform, acellular thickening.
- The patient's severe symptoms and optic disc swelling indicate a more aggressive and acute form of vascular damage, not benign hyaline changes.
*Endothelial proliferation and luminal narrowing with a chronic inflammatory infiltrate*
- This pattern is characteristic of **vasculitis** or conditions like **thrombotic microangiopathy**, which can cause luminal narrowing and kidney damage.
- While some features of vasculitis might overlap, the specific context of poorly controlled severe hypertension points more directly to malignant hypertension-induced changes.
Adrenal medullary disorders US Medical PG Question 9: A 60-year-old woman comes to the physician because of lower back pain, generalized weakness, and weight loss that has occurred over the past 6 weeks. She also says that her urine has appeared foamy recently. Physical examination shows focal midline tenderness of the lumbar spine and conjunctival pallor. Her temperature is 100.5°F (38°C). A photomicrograph of a bone marrow biopsy specimen is shown. Further evaluation of this patient is most likely to show which of the following findings?
- A. Myeloblasts with needle-shaped cytoplasmic inclusions
- B. Erythrocytes with cytoplasmic hemoglobin inclusions
- C. Neutrophils with hypersegmented nuclear lobes
- D. Grouped erythrocytes with stacked-coin appearance (Correct Answer)
- E. B-lymphocytes with radial cytoplasmic projections
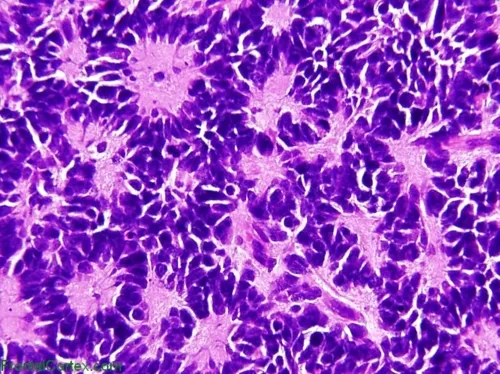
Adrenal medullary disorders Explanation: ***Grouped erythrocytes with stacked-coin appearance***
- The patient's presentation of **lower back pain** (lytic bone lesions), **foamy urine** (proteinuria from Bence Jones proteins), **weight loss**, and **fever** strongly suggests **multiple myeloma**.
- Bone marrow biopsy would show **increased plasma cells**, and further evaluation with **peripheral blood smear** would reveal **rouleaux formation** (stacked-coin appearance of RBCs).
- Rouleaux formation occurs due to **increased serum proteins** (M-protein/paraprotein) that decrease the negative charge between erythrocytes, causing them to stack.
- This finding, combined with **anemia** (conjunctival pallor) and **hypercalcemia** symptoms, is characteristic of multiple myeloma.
*Myeloblasts with needle-shaped cytoplasmic inclusions*
- This describes **Auer rods**, which are pathognomonic for **acute myeloid leukemia (AML)**.
- AML typically presents with **bleeding**, **infections**, and **pancytopenia**, rather than bone pain and foamy urine.
- The patient's clinical picture points to a **plasma cell dyscrasia**, not myeloid leukemia.
*Erythrocytes with cytoplasmic hemoglobin inclusions*
- This finding (Howell-Jolly bodies, Heinz bodies, or other inclusions) suggests **hemolytic anemia**, **thalassemia**, or **asplenia**.
- These conditions do not explain the **bone pain**, **proteinuria**, or **plasma cell proliferation** seen in this case.
- The patient's symptoms are better explained by **multiple myeloma**, not hemoglobinopathy.
*Neutrophils with hypersegmented nuclear lobes*
- Hypersegmented neutrophils (≥5 lobes) are characteristic of **megaloblastic anemia** due to **vitamin B12** or **folate deficiency**.
- While this could cause weakness and anemia, it does not explain the **bone pain**, **fever**, **foamy urine**, or **lumbar spine tenderness**.
- The complete clinical picture is consistent with **multiple myeloma**, not nutritional deficiency.
*B-lymphocytes with radial cytoplasmic projections*
- This describes **hairy cell leukemia**, a rare B-cell neoplasm with characteristic "hairy" projections.
- Hairy cell leukemia presents with **splenomegaly** and **pancytopenia**, not the bone lesions and proteinuria seen here.
- The patient's presentation aligns with **plasma cell myeloma**, not B-cell lymphoproliferative disorder.
Adrenal medullary disorders US Medical PG Question 10: A 38-year-old woman with type 1 diabetes for 20 years presents with diabetic ketoacidosis. She is treated and recovers. Six months later, she develops progressive fatigue, nausea, and hyperpigmentation. Laboratory studies show morning cortisol 3 μg/dL, ACTH 180 pg/mL, TSH 8.2 mIU/L, free T4 0.6 ng/dL, and positive anti-thyroid peroxidase antibodies. She also has positive 21-hydroxylase antibodies. Her 12-year-old daughter was recently diagnosed with type 1 diabetes. Evaluate the pathologic process and most critical monitoring recommendation for the daughter.
- A. Multiple endocrine neoplasia syndrome; screen for pheochromocytoma and medullary thyroid cancer
- B. Autoimmune polyglandular syndrome type 2; screen daughter for adrenal antibodies and thyroid function annually (Correct Answer)
- C. Schmidt syndrome with isolated sporatic occurrence; routine diabetes management only for daughter
- D. Autoimmune polyglandular syndrome type 1; screen for mucocutaneous candidiasis and hypoparathyroidism
- E. Secondary endocrine failure from diabetes complications; optimize glycemic control in daughter
Adrenal medullary disorders Explanation: ***Autoimmune polyglandular syndrome type 2; screen daughter for adrenal antibodies and thyroid function annually***
- The patient presents with **Schmidt syndrome (APS type 2)**, defined by the triad of **Addison's disease** (low cortisol, high ACTH, 21-hydroxylase antibodies), **type 1 diabetes**, and **autoimmune thyroid disease** (Hashimoto's).
- Because APS-2 is **polygenic** and associated with **HLA-DR3/DR4**, first-degree relatives with one component (like the daughter) require screening for other silent autoimmune conditions to prevent **adrenal crisis**.
*Multiple endocrine neoplasia syndrome; screen for pheochromocytoma and medullary thyroid cancer*
- **MEN syndromes** are characterized by **neoplastic** growths (like medullary thyroid cancer or parathyroid adenomas) rather than the **autoimmune destruction** of glands seen here.
- The absence of hypertension or neck masses and the presence of **autoantibodies** directly contradict a diagnosis of MEN.
*Schmidt syndrome with isolated sporatic occurrence; routine diabetes management only for daughter*
- While the patient does have **Schmidt syndrome**, it is incorrect to label it as purely sporadic because it has a strong **familial clustering** component.
- Managing only diabetes in the daughter is insufficient and dangerous, as it ignores her increased risk for life-threatening **primary adrenal insufficiency**.
*Autoimmune polyglandular syndrome type 1; screen for mucocutaneous candidiasis and hypoparathyroidism*
- **APS-1** typically presents in childhood with the triad of **chronic mucocutaneous candidiasis**, **hypoparathyroidism**, and adrenal failure, which does not match this adult patient’s profile.
- APS-1 is caused by a single gene mutation in **AIRE**, whereas this patient's presentation and family history are classic for the polygenic **APS-2**.
*Secondary endocrine failure from diabetes complications; optimize glycemic control in daughter*
- Diabetic complications lead to **microvascular** or **macrovascular** damage, not the **primary gland failure** (indicated by high ACTH and TSH) seen in this patient.
- **Hyperpigmentation** and the presence of **organ-specific antibodies** (21-hydroxylase) confirm an **autoimmune primary failure**, not a secondary metabolic complication.
More Adrenal medullary disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.