Adrenal cortical diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Adrenal cortical diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Adrenal cortical diseases US Medical PG Question 1: A 33-year-old woman presents to the physician because of abdominal discomfort, weakness, and fever. She has had a significant weight loss of 15 kg (33.1 lb) over the past 2 months. She has no history of medical illness and is not on any medications. Her pulse is 96/min, the blood pressure is 167/92 mm Hg, the respiratory rate is 20/min, and the temperature is 37.7°C (99.8°F). Her weight is 67 kg (147.71 lb), height is 160 cm (5 ft 3 in), and BMI is 26.17 kg/m2. Abdominal examination shows purple striae and a vaguely palpable mass in the left upper quadrant of the abdomen, which does not move with respirations. She has coarse facial hair and a buffalo hump along with central obesity. Her extremities have poor muscle bulk, and muscle weakness is noted on examination. An ultrasound of the abdomen demonstrates an adrenal mass with para-aortic lymphadenopathy. Which of the following is the most likely laboratory profile in this patient?
- A. Impaired glucose tolerance, elevated serum cortisol, elevated 24-h urinary free cortisol, and high plasma ACTH
- B. Normal glucose tolerance, elevated serum cortisol, normal 24-h urinary free cortisol, and normal plasma adrenocorticotropic hormone (ACTH)
- C. Impaired glucose tolerance, elevated serum cortisol, elevated 24-h urinary free cortisol, and low plasma ACTH (Correct Answer)
- D. Impaired glucose tolerance, reduced serum cortisol, normal 24-h urinary free cortisol, and low plasma ACTH
- E. Impaired glucose tolerance, elevated serum cortisol, normal 24-h urinary free cortisol, and normal plasma ACTH
Adrenal cortical diseases Explanation: ***Impaired glucose tolerance, elevated serum cortisol, elevated 24-h urinary free cortisol, and low plasma ACTH***
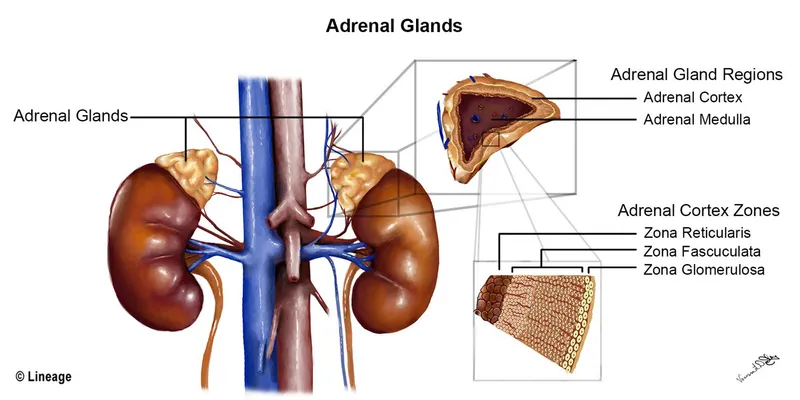
- The clinical picture of **Cushing's syndrome** is evident from purple striae, coarse facial hair, buffalo hump, central obesity, muscle weakness, hypertension, and abdominal mass. The adrenal mass with para-aortic lymphadenopathy points to an **adrenocortical carcinoma**, which independently produces cortisol.
- In cases of **adrenal tumors** producing cortisol, the **exogenous cortisol suppresses ACTH production** from the pituitary, leading to low plasma ACTH levels. Elevated cortisol leads to **insulin resistance** and impaired glucose tolerance.
*Impaired glucose tolerance, elevated serum cortisol, elevated 24-h urinary free cortisol, and high plasma ACTH*
- While significant **hypercortisolism** would cause impaired glucose tolerance, elevated serum and urinary free cortisol, **high plasma ACTH** is characteristic of **Cushing's disease** (pituitary ACTH overproduction), not an adrenal tumor.
- An adrenal tumor directly secretes cortisol, thereby **suppressing ACTH** via negative feedback.
*Normal glucose tolerance, elevated serum cortisol, normal 24-h urinary free cortisol, and normal plasma adrenocorticotropic hormone (ACTH)*
- With the strong clinical signs of Cushing's syndrome and an adrenal mass, **elevated serum cortisol** and **elevated 24-h urinary free cortisol** are highly expected, making "normal" results for these parameters incorrect.
- **Impaired glucose tolerance** is a common consequence of chronic hypercortisolism, so normal glucose tolerance would be unlikely.
*Impaired glucose tolerance, reduced serum cortisol, normal 24-h urinary free cortisol, and low plasma ACTH*
- The clinical presentation clearly indicates **hypercortisolism** (Cushing's syndrome), making **reduced serum cortisol** and normal 24-h urinary free cortisol inconsistent with the diagnosis.
- Low plasma ACTH would be appropriate for an adrenal tumor, but the cortisol levels contradict the clinical picture.
*Impaired glucose tolerance, elevated serum cortisol, normal 24-h urinary free cortisol, and normal plasma ACTH*
- While **impaired glucose tolerance** and **elevated serum cortisol** are consistent with Cushing's syndrome, a **normal 24-h urinary free cortisol** would be highly unlikely given the other clinical signs and the presence of an adrenal mass secreting cortisol.
- **Normal plasma ACTH** is also incorrect; it should be suppressed in cases of primary adrenal hypercortisolism.
Adrenal cortical diseases US Medical PG Question 2: A 15-year-old female is brought to the emergency room with high fever and confusion. She complains of chills and myalgias, and physical examination reveals a petechial rash. Petechial biopsy reveals a Gram-negative diplococcus. The patient is at greatest risk for which of the following?
- A. Pelvic inflammatory disease
- B. Septic arthritis
- C. Bilateral adrenal destruction (Correct Answer)
- D. Osteomyelitis
- E. Acute endocarditis
Adrenal cortical diseases Explanation: ***Bilateral adrenal destruction***
- The clinical presentation with **high fever, confusion, myalgias, and a petechial rash**, along with the finding of **Gram-negative diplococci** from a petechial biopsy, strongly indicates **meningococcemia** (*Neisseria meningitidis* infection).
- **Waterhouse-Friderichsen syndrome**, a severe complication of meningococcemia, involves **massive bilateral adrenal hemorrhage** leading to acute adrenal insufficiency.
*Pelvic inflammatory disease*
- This is an infection of the female reproductive organs, often caused by *Chlamydia trachomatis* or *Neisseria gonorrhoeae*, and typically presents with lower abdominal pain, vaginal discharge, and fever, not usually with a widespread petechial rash and confusion.
- While *Neisseria gonorrhoeae* is a Gram-negative diplococcus, the systemic symptoms and petechial rash point to a disseminated infection like meningococcemia, not localized PID.
*Septic arthritis*
- Septic arthritis involves bacterial infection of a joint, leading to pain, swelling, and reduced range of motion in that specific joint.
- Although disseminated gonococcal infection can cause septic arthritis, the primary presentation with confusion and a rapidly progressive petechial rash points to a more severe systemic infection like meningococcemia.
*Osteomyelitis*
- Osteomyelitis is an infection of the bone, characterized by localized pain, tenderness, swelling, and fever, often without the rapid onset of confusion and widespread petechial rash.
- While it can be caused by various bacteria, including some Gram-negative organisms, it's not the most likely acute complication of the described systemic infection.
*Acute endocarditis*
- Acute endocarditis is an infection of the heart's inner lining or valves, often caused by bacteria like *Staphylococcus aureus*, leading to symptoms such as fever, new heart murmurs, and embolic phenomena.
- While systemic symptoms and petechiae can occur, confusion and a rapidly spreading rash, coupled with the specific Gram-negative diplococcus finding, more strongly suggest meningococcal sepsis over acute endocarditis.
Adrenal cortical diseases US Medical PG Question 3: A 32-year-old man presents with hypertension that has been difficult to control with medications. His symptoms include fatigue, frequent waking at night for voiding, and pins and needles in the legs. His symptoms started 2 years ago. Family history is positive for hypertension in his mother. His blood pressure is 160/100 mm Hg in the right arm and 165/107 mm Hg in the left arm, pulse is 85/min, and temperature is 36.5°C (97.7°F). Physical examination reveals global hyporeflexia and muscular weakness. Lab studies are shown:
Serum sodium 147 mEq/L
Serum creatinine 0.7 mg/dL
Serum potassium 2.3 mEq/L
Serum bicarbonate 34 mEq/L
Plasma renin activity low
Which of the following is the most likely diagnosis?
- A. Renal artery stenosis
- B. Coarctation of aorta
- C. Cushing syndrome
- D. Primary aldosteronism (Correct Answer)
- E. Essential hypertension
Adrenal cortical diseases Explanation: ***Primary aldosteronism***
- The patient presents with **resistant hypertension**, **hypokalemia** (2.3 mEq/L), **metabolic alkalosis** (bicarbonate 34 mEq/L), and **low plasma renin activity**, which are classic features of primary aldosteronism.
- Symptoms like **fatigue**, **nocturia**, and **paresthesias** (pins and needles) in the legs are consistent with severe hypokalemia, directly resulting from excessive aldosterone secretion.
*Renal artery stenosis*
- This condition typically causes **secondary hypertension** with **elevated renin levels** due to decreased renal perfusion, which contradicts the low plasma renin activity seen in this patient.
- While it can cause hypokalemia because of increased renin-angiotensin-aldosterone system activation, the **primary driver** in this case, based on low renin, points away from renal artery stenosis.
*Coarctation of aorta*
- Characterized by **differential blood pressures** between the upper and lower extremities and sometimes between the arms, and a **systolic murmur** that is often present.
- It does not typically present with severe **hypokalemia** or metabolic alkalosis or the low plasma renin activity observed in this patient.
*Cushing syndrome*
- This syndrome is caused by **excessive cortisol** and can lead to hypertension and hypokalemia, but it is also associated with distinct clinical features like **central obesity**, buffalo hump, moon facies, and proximal muscle weakness, which are not described.
- While it can cause similar electrolyte imbalances, the lack of classic Cushingoid features makes it less likely, and the specific **low plasma renin** points more strongly to aldosterone excess.
*Essential hypertension*
- This is a diagnosis of exclusion, typically presenting without a clear secondary cause and with **normal electrolyte levels**.
- The presence of severe **hypokalemia**, **metabolic alkalosis**, and **low plasma renin activity** indicates a secondary cause, ruling out essential hypertension.
Adrenal cortical diseases US Medical PG Question 4: A 27-year-old Caucasian female presents complaining of recent weight loss and weakness. She reports that she feels dizzy and lightheaded every morning when she gets out of bed, and often at work whenever she must rise from her desk. Physical exam reveals several areas of her skin including her elbows and knees are more pigmented than other areas. Which of the following would be consistent with the patient's disease?
- A. Pretibial myxedema
- B. Hyperkalemia (Correct Answer)
- C. Hypernatremia
- D. Central obesity
- E. Hyperglycemia
Adrenal cortical diseases Explanation: ***Hyperkalemia***
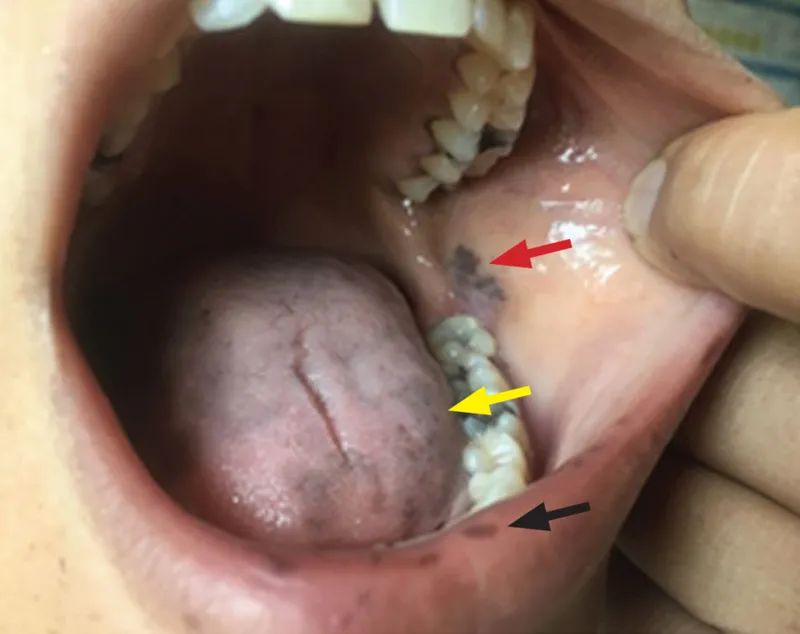
- The patient's symptoms (weight loss, weakness, **orthostatic hypotension**, and **hyperpigmentation**) are classic for **primary adrenal insufficiency (Addison's disease)**.
- In primary adrenal insufficiency, decreased **aldosterone** production leads to **impaired renal sodium reabsorption** and **potassium excretion**, resulting in **hyperkalemia**.
*Pretibial myxedema*
- This condition is characteristic of **Graves' disease**, which involves hyperthyroidism, not adrenal insufficiency.
- It presents as localized thickening and induration of the skin, typically on the shins.
*Hypernatremia*
- **Hyponatremia** (low sodium) is a common finding in primary adrenal insufficiency due to impaired aldosterone action and increased ADH secretion.
- **Hypernatremia** (high sodium) would be inconsistent with this diagnosis.
*Central obesity*
- **Central obesity** and **moon facies** are characteristic features of **Cushing's syndrome**, which is caused by *excess* glucocorticoids, the opposite of adrenal insufficiency.
- Patients with Addison's disease often experience **weight loss** rather than weight gain.
*Hyperglycemia*
- **Hypoglycemia** is commonly seen in primary adrenal insufficiency due to the lack of **cortisol**, which plays a crucial role in maintaining blood glucose levels.
- **Hyperglycemia** would suggest conditions like diabetes or Cushing's syndrome, not adrenal insufficiency.
Adrenal cortical diseases US Medical PG Question 5: A 55-year-old man presents to his primary care physician for a new patient appointment. The patient states that he feels well and has no concerns at this time. The patient has a past medical history of hypertension, an elevated fasting blood glucose, and is not currently taking any medications. His blood pressure is 177/118 mmHg, pulse is 90/min, respirations are 16/min, and oxygen saturation is 97% on room air. Physical exam is notable for an obese man with atrophy of his limbs and striae on his abdomen. Laboratory values are notable for a blood glucose of 175 mg/dL. Which of the following is the best next step in evaluation?
- A. Hydrochlorothiazide
- B. MRI of the head
- C. Metformin
- D. Weight loss
- E. Dexamethasone suppression test (Correct Answer)
Adrenal cortical diseases Explanation: ***Dexamethasone suppression test***
- The patient presents with **atrophy of the limbs** with concurrent **striae on the abdomen**, uncontrolled hypertension, and elevated blood glucose, which are all classic signs of **Cushing's syndrome**.
- A **dexamethasone suppression test** is the best initial diagnostic step to confirm Cushing's syndrome by assessing the body's cortisol regulation.
*Hydrochlorothiazide*
- While the patient has **hypertension**, treating the symptom without addressing the underlying cause (Cushing's syndrome) would be insufficient and potentially delay proper diagnosis.
- **Hydrochlorothiazide** is an antihypertensive, but without addressing the likely cortisol excess, blood pressure control will be challenging.
*MRI of the head*
- An **MRI of the head** (specifically the pituitary) would be considered after biochemical confirmation of Cushing's syndrome to localize a potential tumor, but it is not the initial diagnostic step.
- Imaging is performed *after* biochemical tests indicate cortisol excess, to differentiate between pituitary, adrenal, or ectopic causes.
*Metformin*
- The patient has **elevated blood glucose**, but initiating an antidiabetic medication like **metformin** before evaluating for Cushing's syndrome would be treating a symptom without identifying the root cause.
- Diabetes in this context is likely secondary to excess cortisol, so managing it effectively requires addressing the underlying endocrine disorder.
*Weight loss*
- While **weight loss** is generally beneficial for hypertension and diabetes, in the context of Cushing's syndrome with **limb atrophy** and **central obesity**, focusing solely on weight loss without addressing the hormonal imbalance would be ineffective.
- The characteristic fat redistribution in Cushing's syndrome makes simple weight loss difficult and less impactful until cortisol levels are managed.
Adrenal cortical diseases US Medical PG Question 6: A 69-year-old woman is brought to the emergency department because of fatigue and lethargy for 5 days. She has also had weakness and nausea for the last 3 days. She has sarcoidosis, major depressive disorder, and hypertension. She had a stroke 5 years ago. Current medications include aspirin, nifedipine, prednisolone, fluoxetine, and rosuvastatin, but she has not taken any of her medications for 7 days due to international travel. Her temperature is 36.1°C (96.9°F), pulse is 95/min, and blood pressure is 85/65 mm Hg. She is lethargic but oriented. Examination shows no other abnormalities. Her hemoglobin concentration is 13.4 g/dL and leukocyte count is 9,600/mm3. Both serum cortisol and ACTH levels are decreased. This patient is most likely to have which of the following additional laboratory abnormalities?
- A. Hyperglycemia
- B. Hyperkalemia
- C. Hyponatremia (Correct Answer)
- D. Hypokalemia
- E. Normal anion gap metabolic acidosis
Adrenal cortical diseases Explanation: ***Hyponatremia***
- This patient has **secondary adrenal insufficiency** due to **HPA axis suppression** from chronic prednisolone use, precipitated by abrupt withdrawal after 7 days without medication.
- **Both decreased cortisol and ACTH** confirm secondary (central) adrenal insufficiency, distinguishing it from primary adrenal insufficiency where ACTH would be elevated.
- **Hyponatremia** develops due to **cortisol deficiency** impairing free water excretion, leading to dilutional hyponatremia—a hallmark laboratory finding in adrenal insufficiency.
- Clinical features include **fatigue, lethargy, hypotension, nausea, and weakness**, consistent with adrenal crisis.
*Hyperglycemia*
- While **glucocorticoids** cause hyperglycemia, **cortisol deficiency** in adrenal insufficiency leads to **impaired gluconeogenesis** and a tendency toward **hypoglycemia**, not hyperglycemia.
- The patient's presentation with hypotension and weakness is consistent with adrenal crisis, not hyperglycemia.
*Hyperkalemia*
- **Hyperkalemia** is characteristic of **primary adrenal insufficiency** (Addison's disease) due to **aldosterone deficiency** affecting the renin-angiotensin-aldosterone system.
- In **secondary adrenal insufficiency**, the hypothalamic-pituitary axis is suppressed but the **renin-angiotensin-aldosterone system remains intact**, so aldosterone secretion is preserved and significant hyperkalemia does not occur.
*Hypokalemia*
- **Hypokalemia** is not a typical feature of adrenal insufficiency and is more commonly associated with diuretic use, primary hyperaldosteronism, or other conditions not present in this case.
- The patient's condition reflects cortisol deficiency with preserved aldosterone function.
*Normal anion gap metabolic acidosis*
- **Normal anion gap metabolic acidosis** occurs in conditions like **renal tubular acidosis** or **diarrhea**, but is not a direct or common consequence of secondary adrenal insufficiency.
- The acute presentation with hypotension and electrolyte disturbance (hyponatremia) is the primary metabolic derangement in this case.
Adrenal cortical diseases US Medical PG Question 7: A 27-year-old woman presents to her primary care physician because of headaches that she has had over the last three weeks. She has not had any significant past medical history though she does recall that various types of cancer run in her family. She has also noticed that she has been gaining some weight, and her feet no longer fit into her favorite shoes. On presentation, her temperature is 98.6°F (37°C), blood pressure is 159/92 mmHg, pulse is 75/min, and respirations are 16/min. Physical exam reveals 1+ edema in her lower extremities bilaterally. She is placed on captopril and presents to the emergency department two weeks later after a minor motor vehicle accident. She is cleared of any serious injuries, and as part of her workup, labs are drawn with the following results:
BUN: 47 mg/dL
Creatinine: 1.4 mg/dL
Which of the following findings would most likely also be seen in this patient?
- A. Mass present in adrenal cortex
- B. Atherosclerotic plaques blocking blood flow
- C. Mass present in adrenal medulla
- D. No lesions present
- E. String-of-beads appearance on angiography (Correct Answer)
Adrenal cortical diseases Explanation: ***String-of-beads appearance on angiography***
- The patient's symptoms of **headaches**, **weight gain**, **bilateral lower extremity edema**, and **hypertension** (159/92 mmHg) in a young woman, especially with the presentation of acute kidney injury after beginning an ACE inhibitor (captopril), are highly suggestive of **renovascular hypertension** due to **fibromuscular dysplasia (FMD)**.
- FMD characteristically presents as a **"string-of-beads"** appearance on renal angiography due to areas of stenosis alternating with aneurysmal dilations in the renal arteries.
*Mass present in adrenal cortex*
- A mass in the adrenal cortex typically causes **hyperaldosteronism (Conn syndrome)** or **Cushing's syndrome**. While hyperaldosteronism can cause hypertension and hypokalemia, it does not explain the acute kidney injury with ACE inhibitor treatment.
- Cushing's syndrome involves **central obesity**, **moon facies**, and **striae**, which are not described.
*Atherosclerotic plaques blocking blood flow*
- **Atherosclerotic renovascular disease** typically affects older individuals with a history of cardiovascular risk factors (diabetes, hyperlipidemia, smoking). This patient is young and has no such history.
- While it can cause renal artery stenosis and acute kidney injury with ACE inhibitors, the demographic profile does not fit.
*Mass present in adrenal medulla*
- A mass in the adrenal medulla suggests a **pheochromocytoma**, which causes **episodic hypertension**, **palpitations**, **sweating**, and **anxiety**.
- The patient's hypertension is sustained, and she does not present with classic symptoms of a pheochromocytoma.
*No lesions present*
- The patient's clinical presentation, including the development of acute kidney injury after starting captopril, strongly indicates an underlying renovascular pathology.
- The absence of lesions would not explain the severe, sustained hypertension and the adverse reaction to captopril.
Adrenal cortical diseases US Medical PG Question 8: A 45-year-old woman presents to her physician with a four-month history of headache. Her headache is nonfocal but persistent throughout the day without any obvious trigger. She was told that it was a migraine but has never responded to sumatriptan, oxygen, or antiemetics. She takes amlodipine for hypertension. She does not smoke. She denies any recent weight loss or constitutional symptoms. Her temperature is 98°F (36.7°C), blood pressure is 180/100 mmHg, pulse is 70/min, and respirations are 15/min. She is obese with posterior cervical fat pads and central abdominal girth. Her neurological exam is unremarkable. In her initial laboratory workup, her fasting blood glucose level is 200 mg/dL. The following additional lab work is obtained and is as follows:
Serum:
Na+: 142 mEq/L
Cl-: 102 mEq/L
K+: 4.1 mEq/L
HCO3-: 24 mEq/L
BUN: 20 mg/dL
Glucose: 135 mg/dL
Creatinine: 1.3 mg/dL
Ca2+: 10.0 mg/dL
AST: 8 U/L
ALT: 8 U/L
24-hour urinary cortisol: 500 µg (reference range < 300 µg)
Serum cortisol: 25 µg/mL (reference range 5-23 µg/dL)
24-hour low dose dexamethasone suppression test: Not responsive
High dose dexamethasone suppression test: Responsive
Adrenocorticotropin-releasing hormone (ACTH): 20 pg/mL (5-15 pg/mL)
Imaging reveals a 0.5 cm calcified pulmonary nodule in the right middle lobe that has been present for 5 years but an otherwise unremarkable pituitary gland, mediastinum, and adrenal glands. What is the best next step in management?
- A. Pituitary resection
- B. CT-guided biopsy of the pulmonary nodule
- C. Inferior petrosal sinus sampling (Correct Answer)
- D. Pulmonary nodule resection
- E. Repeat high dose dexamethasone suppression test
Adrenal cortical diseases Explanation: ***Inferior petrosal sinus sampling***
- The patient exhibits clear signs of **Cushing's syndrome** (hypertension, obesity with central fat distribution, hyperglycemia, elevated cortisol, lack of suppression with low-dose dexamethasone).
- The elevated ACTH and suppression with high-dose dexamethasone point towards **Cushing's disease** (pituitary ACTH overproduction). However, with an unremarkable pituitary MRI, **inferior petrosal sinus sampling (IPSS)** is crucial to differentiate ectopic ACTH production (e.g., from a bronchial carcinoid, lung nodule) from pituitary disease.
*Pituitary resection*
- This is a treatment for **Cushing's disease** (pituitary adenoma), but it should only be performed after definitive localization of the ACTH-producing tumor.
- Since the pituitary gland appears unremarkable on imaging and the patient has a lung nodule, **IPSS** is needed to confirm the source of ACTH overexpression before surgery.
*CT-guided biopsy of the pulmonary nodule*
- While the patient has a calcified pulmonary nodule, it has been stable for 5 years and calcified, suggesting it is likely **benign**.
- Without evidence that this nodule is the source of **ectopic ACTH production** (which IPSS would help determine), a biopsy is premature and may not yield a definitive answer for the Cushing's presentation.
*Pulmonary nodule resection*
- Resection is a treatment for **ectopic ACTH-producing tumors**, typically **carcinoid tumors** in the lung.
- However, the nodule is calcified and stable, making it unlikely to be the cause of Cushing's syndrome, and further, the diagnosis of ectopic ACTH needs to be confirmed with **IPSS** before considering such an invasive procedure.
*Repeat high dose dexamethasone suppression test*
- The results already indicate responsiveness to the high-dose dexamethasone suppression test, suggesting a **pituitary source** of ACTH.
- Repeating the test would not add more diagnostic value and would only delay the necessary localization studies like **IPSS** or imaging.
Adrenal cortical diseases US Medical PG Question 9: A 63-year-old woman presents to your outpatient clinic complaining of headaches, blurred vision, and fatigue. She has a blood pressure of 171/91 mm Hg and heart rate of 84/min. Physical examination is unremarkable. Her lab results include K+ of 3.1mEq/L and a serum pH of 7.51. Of the following, which is the most likely diagnosis for this patient?
- A. Pheochromocytoma
- B. Renal artery stenosis
- C. Cushing’s syndrome
- D. Primary hyperaldosteronism (Conn’s syndrome) (Correct Answer)
- E. Addison’s disease
Adrenal cortical diseases Explanation: ***Primary hyperaldosteronism (Conn’s syndrome)***
- The combination of **hypertension**, **hypokalemia (K+ 3.1 mEq/L)**, and **metabolic alkalosis (pH 7.51)** is highly characteristic of primary hyperaldosteronism.
- Excess aldosterone leads to increased sodium reabsorption and potassium/hydrogen ion excretion, causing these electrolyte imbalances.
*Pheochromocytoma*
- This condition involves episodic **hypertension**, palpitations, sweating, and anxiety due to catecholamine excess.
- While hypertension is present, the absence of paroxysmal symptoms and the specific electrolyte abnormalities (hypokalemia, alkalosis) make it less likely.
*Renal artery stenosis*
- This can cause **secondary hypertension** and occasionally hypokalemia, but it typically presents with **renal bruits**, and the metabolic alkalosis is not a direct or prominent feature.
- The elevated renin-angiotensin-aldosterone axis would lead to secondary hyperaldosteronism, but primary hyperaldosteronism is suggested by the overall clinical picture.
*Cushing’s syndrome*
- Cushing's syndrome is characterized by **central obesity**, striae, moon facies, and **hyperglycemia**, among other symptoms.
- While hypertension and hypokalemia can occur in severe cases, the predominant clinical features are not aligned with this patient's presentation.
*Addison’s disease*
- This condition is characterized by **adrenal insufficiency**, leading to hypoglycemia, **hyponatremia**, **hyperkalemia**, and **hypotension**.
- The patient's hypertension and hypokalemia directly contradict the typical presentation of Addison’s disease.
Adrenal cortical diseases US Medical PG Question 10: A 42-year-old man with systolic heart failure secondary to amyloidosis undergoes heart transplantation. The donor heart is obtained from a 17-year-old boy who died in a motor vehicle collision. Examination of the donor heart during the procedure shows a flat, yellow-white discoloration with an irregular border on the luminal surface of the aorta. A biopsy of this lesion is most likely to show which of the following?
- A. Apoptotic smooth muscle cells
- B. Necrotic cell debris
- C. Proteoglycan accumulation
- D. Collagen deposition
- E. Lipoprotein-laden macrophages (Correct Answer)
Adrenal cortical diseases Explanation: ***Lipoprotein-laden macrophages***
- The description of a flat, yellow-white discolored lesion with an irregular border on the luminal surface of the aorta in a 17-year-old is classic for a **fatty streak**, the earliest lesion of **atherosclerosis**.
- Fatty streaks are histologically characterized by the accumulation of **macrophages that have ingested oxidized lipoproteins**, appearing as foam cells within the intima.
*Apoptotic smooth muscle cells*
- While apoptosis of various cell types, including smooth muscle cells, can occur in advanced atherosclerotic lesions, it is not the primary or defining feature of an early **fatty streak**.
- **Apoptosis** contributes to the necrotic core formation in later stages of plaque development, not the initial yellow-white discoloration of a fatty streak.
*Necrotic cell debris*
- **Necrotic cell debris** is a prominent feature of more advanced, **complicated atherosclerotic plaques**, forming the necrotic core.
- In a **fatty streak**, the cells are primarily viable foam cells, and significant necrosis is not yet present.
*Proteoglycan accumulation*
- **Proteoglycan accumulation** occurs in the arterial intima and is involved in the retention of lipoproteins, contributing to the development of atherosclerosis.
- However, the immediate and most characteristic histological finding of the **yellow-white discoloration** in a fatty streak is the lipid-laden macrophage.
*Collagen deposition*
- **Collagen deposition** is a key feature of the fibrous cap in **advanced atherosclerotic plaques**, laid down by migrating smooth muscle cells.
- It is not the primary histological characteristic of an early, flat, yellow-white **fatty streak**.
More Adrenal cortical diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.