Vesiculobullous diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Vesiculobullous diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Vesiculobullous diseases US Medical PG Question 1: A 64-year-old man presents to his primary care provider after noticing the development of a blistering rash. The patient states that his symptoms began 1 week ago after he noticed a blister develop on the inside of his mouth that eventually ruptured. Over the past several days, he has noticed several more blisters on his torso. The patient denies a fever or any other symptoms. He has a history of high blood pressure, for which he takes hydrochlorothiazide. He is otherwise healthy and denies any recent changes to his medication. Today, the patient’s temperature is 99.0°F (37.2°C), blood pressure is 124/84 mmHg, pulse is 66/min, and respirations are 12/min. On exam, the patient’s mouth is notable for a previously ruptured blister on his left buccal mucosa. On his left flank and anterior abdomen are scattered 10-15-cm bullae that appear flaccid and filled with serous fluid. The lesions are erythematous but there is no surrounding erythema. On manual rubbing of the skin near the lesions, new blisters form within minutes. Which of the following is involved in the pathogenesis of this disease?
- A. IgA antibodies depositing in the dermal papillae
- B. Autoantibodies against hemidesmosomes
- C. Exotoxin destroying keratinocyte attachments
- D. Viral infection of skin
- E. IgG against transmembrane proteins between cells (Correct Answer)
Vesiculobullous diseases Explanation: ***IgG against transmembrane proteins between cells***
- This clinical presentation, including flaccid bullae, Nikolsky sign (new blisters with manual rubbing), and oral involvement, is characteristic of **pemphigus vulgaris**.
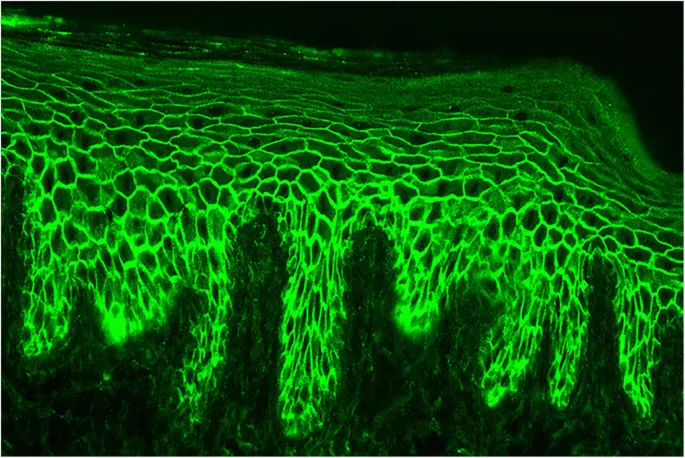
- Pemphigus vulgaris is caused by **IgG autoantibodies** targeting **desmoglein 1** and **desmoglein 3**, which are transmembrane proteins forming desmosomes that connect keratinocytes.
*IgA antibodies depositing in the dermal papillae*
- This describes the pathogenesis of **dermatitis herpetiformis**, which presents with intensely pruritic papulovesicular lesions, typically on extensor surfaces.
- The lesions in dermatitis herpetiformis are small, grouped vesicles, not the large, flaccid bullae seen in this patient.
*Autoantibodies against hemidesmosomes*
- This mechanism is characteristic of **bullous pemphigoid**, which typically presents with tense bullae that do not rupture easily and are often associated with pruritus.
- Unlike pemphigus vulgaris, bullous pemphigoid usually spares the oral mucosa, and the Nikolsky sign is typically absent.
*Exotoxin destroying keratinocyte attachments*
- This mechanism is seen in conditions like **staphylococcal scalded skin syndrome (SSSS)**, caused by exfoliating toxins that cleave **desmoglein 1**.
- SSSS typically presents with diffuse erythema and superficial epidermal peeling, often in children, and the patient's history does not suggest an acute infection.
*Viral infection of skin*
- Viral infections leading to blistering rashes, such as **herpes simplex** or **varicella-zoster virus**, typically cause painful, grouped vesicles on an erythematous base.
- The extensive, flaccid bullae and lack of fever or prodromal symptoms are inconsistent with a primary viral blistering eruption.
Vesiculobullous diseases US Medical PG Question 2: A 50-year-old woman comes to the physician because of blisters on her forearm that appeared 3 days ago. She also reports pain in her left cheek when eating and pain during sexual intercourse for the past week. She has not been sick for the past 6 months. She has started hiking in the woods on the weekends with her son a couple months ago but has been careful to avoid poison ivy. She has a history of hypertension and osteoarthritis. She recently started taking captopril and stopped taking meloxicam 2 weeks ago. She has a family history of pernicious anemia and Graves' disease. The patient's vital signs are within normal limits. Examination reveals multiple, flaccid blisters on the volar surface of the forearm and ulcers on the buccal, gingival, and vulvar mucosa. The epidermis on the forearm separates when the skin is lightly stroked. The total body surface area involvement of the blisters is estimated to be 10%. The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Bullous pemphigoid
- B. Toxic epidermal necrolysis
- C. Dermatitis herpetiformis
- D. Pemphigus vulgaris (Correct Answer)
- E. Lichen planus
Vesiculobullous diseases Explanation: ***Pemphigus vulgaris***
- The presence of **flaccid blisters** on the forearm, along with **oral and vulvar mucosal ulcers**, is highly characteristic of pemphigus vulgaris. Oral lesions often precede skin lesions, and the **Nikolsky sign** (epidermal separation with light stroking) is positive.
- This autoimmune blistering disease is caused by antibodies against **desmoglein 1 and 3**, leading to acantholysis (loss of cohesion between keratinocytes) in the epidermis. The Captopril use is notable as ACE inhibitors can rarely trigger pemphigus.
*Bullous pemphigoid*
- Bullous pemphigoid typically presents with **tense bullae** that do not rupture easily and are often accompanied by **pruritus**, which is not described here, and a negative Nikolsky sign.
- Mucosal involvement is less common and usually less severe than in pemphigus vulgaris, often sparing the oral cavity.
*Toxic epidermal necrolysis*
- This condition is characterized by widespread **erythema and epidermal detachment** (often >30% body surface area), usually triggered by medications, with prominent systemic symptoms (e.g., fever, malaise). The patient's 10% BSA involvement and lack of systemic illness makes this less likely.
- The lesions in TEN are typically diffuse and rapidly progressing, resembling a severe burn, unlike the more localized flaccid blisters seen here.
*Dermatitis herpetiformis*
- Dermatitis herpetiformis presents as intensely **pruritic vesicles and papules**, primarily on extensor surfaces, and is strongly associated with **celiac disease**.
- The blisters are typically firm and grouped, and mucosal lesions are uncommon, differentiating it from the flaccid blisters and mucosal ulcers described.
*Lichen planus*
- Lichen planus manifests as **pruritic, polygonal, planar, purple papules and plaques**, often with **Wickham's striae**.
- While it can cause oral mucosal lesions (reticular white patches) and erosions, it does not typically present with the widespread flaccid blisters or positive Nikolsky sign seen in this patient.
Vesiculobullous diseases US Medical PG Question 3: A 22-year-old woman presents to the emergency department with a 2-day history of severe blistering. She says that she woke up 2 days ago with a number of painful blisters in her mouth and has since been continuing to develop blisters of her cutaneous skin all over her body and the mucosa of her mouth. She has no past medical history and has never experienced these symptoms before. Physical exam reveals a diffuse vesicular rash with painful, flaccid blisters that separate easily with gentle rubbing. The function of which of the following proteins is most likely disrupted in this patient?
- A. T-cell receptor
- B. Cadherin (Correct Answer)
- C. Keratin
- D. Collagen
- E. Integrin
Vesiculobullous diseases Explanation: ***Cadherin***
- The patient's presentation with **diffuse flaccid blisters** that separate easily with gentle rubbing (a positive **Nikolsky sign**) and **oral mucosal involvement** is highly suggestive of **pemphigus vulgaris**.
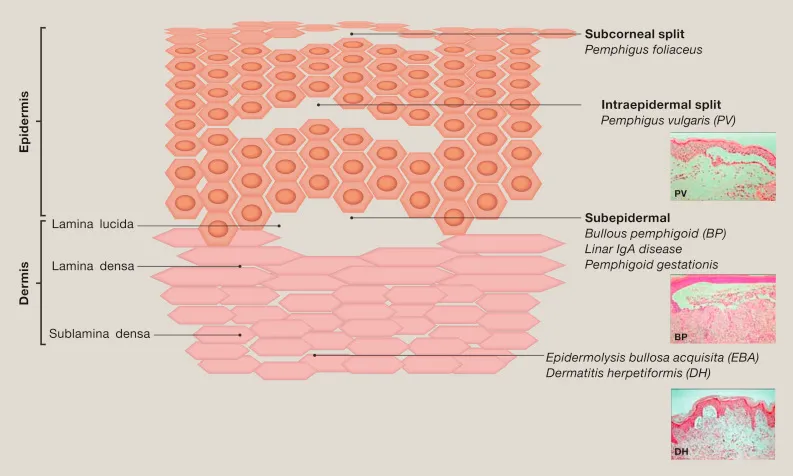
- **Pemphigus vulgaris** is an autoimmune blistering disease where autoantibodies target **desmoglein 1 and 3**, which are types of **cadherin cell adhesion proteins** responsible for cell-to-cell adhesion in the epidermis. Their disruption leads to **intraepidermal blistering**.
*T-cell receptor*
- **T-cell receptors** are involved in immune recognition and T-cell activation, but their primary disruption is not directly responsible for the blistering seen in pemphigus vulgaris, which is mediated by **autoantibodies against desmogleins**.
- Conditions involving T-cell receptor dysfunction typically manifest as **immunodeficiencies**, **autoimmune responses** directed at self-antigens via cellular immunity, or **lymphomas**, not primary blistering diseases of this type.
*Keratin*
- **Keratin** is an intermediate filament protein that provides structural integrity to epithelial cells. While disruptions in keratin can lead to blistering disorders (e.g., **epidermolysis bullosa simplex**), these often present with **intact, tense blisters** (due to basal cell layer separation) or mechanical fragility, unlike the flaccid blisters of pemphigus vulgaris.
- **Genetic defects in keratin** would typically present earlier in life and are not usually associated with an autoimmune mechanism causing acute onset flaccid blistering.
*Collagen*
- **Collagen** is a primary component of the extracellular matrix and is crucial for skin strength and integrity. Disorders involving collagen, such as **epidermolysis bullosa acquisita** or certain types of **dystrophic epidermolysis bullosa**, typically disrupt the **dermal-epidermal junction**, leading to **subepidermal blistering** and often **scarring**.
- The flaccid, intraepidermal blisters and positive Nikolsky sign described are not characteristic of collagen-related blistering disorders.
*Integrin*
- **Integrins** are cell surface receptors involved in cell-to-extracellular matrix adhesion, particularly in forming **hemidesmosomes** that anchor basal keratinocytes to the basement membrane.
- Disruption of integrins or other hemidesmosomal components (e.g., in **bullous pemphigoid**) leads to **subepidermal blistering**, where blisters are typically tense and do not easily rupture with gentle pressure, which is distinct from the flaccid blisters of pemphigus vulgaris.
Vesiculobullous diseases US Medical PG Question 4: A 45-year-old man visits the office with complaints of severe pain with urination for 5 days. In addition, he reports having burning discomfort and itchiness at the tip of his penis. He is also concerned regarding a yellow-colored urethral discharge that started a week ago. Before his symptoms began, he states that he had sexual intercourse with multiple partners at different parties organized by the hotel he was staying at. Physical examination shows edema and erythema concentrated around the urethral meatus accompanied by a mucopurulent discharge. Which of the following diagnostic tools will best aid in the identification of the causative agent for his symptoms?
- A. Nucleic acid amplification tests (NAATs) (Correct Answer)
- B. Urethral biopsy
- C. Tzanck smear
- D. Leukocyte esterase dipstick test
- E. Gram stain
Vesiculobullous diseases Explanation: ***Nucleic acid amplification tests (NAATs)***
- NAATs are the **most sensitive and specific diagnostic tools** for detecting common sexually transmitted infections (STIs) like **gonorrhea** and **chlamydia**, which present with urethral discharge, dysuria, and itching.
- They can identify the **genetic material** of the causative organisms directly from urine samples or urethral swabs, making them highly effective even with low bacterial loads.
*Urethral biopsy*
- A urethral biopsy is an **invasive procedure** generally reserved for investigating conditions like **strictures, tumors, or chronic inflammatory diseases** when other diagnostic methods are inconclusive.
- It is not a primary diagnostic tool for acute urethritis suspected to be an STI, as it carries risks and is unnecessary given the availability of less invasive options.
*Tzanck smear*
- The Tzanck smear is primarily used for diagnosing **herpes simplex virus (HSV) infections** by looking for multinucleated giant cells and intranuclear inclusions.
- While HSV can cause genital lesions, it typically does not present as a primary symptom of mucopurulent urethral discharge and dysuria without visible vesicles or ulcers, making it less likely in this scenario.
*Leukocyte esterase dipstick test*
- A leukocyte esterase dipstick test detects the presence of **white blood cells** in urine, indicating inflammation or infection in the urinary tract.
- While it can suggest urethritis, it is **not specific for the causative agent** and merely indicates inflammation, requiring further specific testing to identify the pathogen.
*Gram stain*
- A Gram stain of urethral discharge can rapidly identify Gram-negative intracellular diplococci suggestive of **gonorrhea** (Neisseria gonorrhoeae).
- However, its sensitivity for gonorrhea is lower than NAATs, especially in asymptomatic cases or for detecting other common causes of urethritis like **Chlamydia trachomatis**, which are not visible on Gram stain.
Vesiculobullous diseases US Medical PG Question 5: A 58-year-old woman presents with tense bullae on an erythematous base, primarily affecting her trunk and extremities. The lesions developed over the past 3 weeks. Nikolsky sign is negative. Skin biopsy shows subepidermal bullae with eosinophilic infiltrate. Direct immunofluorescence shows linear deposits of IgG and C3 at the basement membrane zone. Which of the following is the target antigen in this condition?
- A. Type IV collagen
- B. BP180/BP230 (Correct Answer)
- C. Type VII collagen
- D. Desmoglein-3
Vesiculobullous diseases Explanation: ***BP180/BP230***
- The clinical presentation of **tense bullae**, negative **Nikolsky sign**, subepidermal bullae with **eosinophilic infiltrate**, and **linear IgG and C3 deposition at the basement membrane zone** are classic features of **bullous pemphigoid**.
- **BP180** (also known as type XVII collagen) and **BP230** are hemidesmosomal proteins that serve as the primary target antigens in bullous pemphigoid.
*Type IV collagen*
- **Type IV collagen** is a major component of the **basement membrane**, but it is not the target antigen in bullous pemphigoid.
- Antibodies against type IV collagen may be involved in **Goodpasture syndrome**, which affects the kidneys and lungs, not primarily the skin in this manner.
*Type VII collagen*
- **Type VII collagen** is found in the **anchoring fibrils** beneath the basement membrane.
- Antibodies against **type VII collagen** are characteristic of **epidermolysis bullosa acquisita**, which typically presents with **fragile skin, trauma-induced blistering**, and scarring, differentiating it from this case.
*Desmoglein-3*
- **Desmoglein-3** is a **desmosomal protein** that is a primary target antigen in **pemphigus vulgaris**, especially the **mucosal dominant form**.
- **Pemphigus vulgaris** is characterized by **flaccid bullae, painful erosions**, and a **positive Nikolsky sign**, which are not consistent with the patient's presentation.
Vesiculobullous diseases US Medical PG Question 6: A 53-year-old woman seeks medical care for superficial erosions and blisters over the skin of her head and trunk. She also has significant involvement of her buccal mucosa, which has made eating difficult. A year earlier, she developed tender sores on the oral mucosa and soft palate of her mouth, which was initially treated as herpes simplex stomatitis. Her condition worsened despite treatment, resulting in the development of eroded areas over her trunk and extremities, with a 10 kg weight loss. Upon further questioning, she denies itching, but she notes that the top layer of her skin could be easily removed when firm horizontal pressure was applied. What is the most likely diagnosis for this patient’s condition?
- A. Dermatitis herpetiformis
- B. Toxic epidermal necrolysis
- C. Pemphigus vulgaris (Correct Answer)
- D. Bullous pemphigoid
- E. Behcet’s disease
Vesiculobullous diseases Explanation: ***Pemphigus vulgaris***
- This condition is characterized by **superficial erosions and blisters**, significant **mucosal involvement** (especially oral), and a **positive Nikolsky sign** (skin easily removed with pressure), all classic features of pemphigus vulgaris.
- The initial presentation often includes painful **oral lesions** that precede cutaneous involvement and can lead to **weight loss** due to difficult eating.
*Dermatitis herpetiformis*
- Typically presents with intensely **pruritic (itchy) urticarial papules and vesicles**, primarily on extensor surfaces, which is contrary to the patient's denial of itching.
- Strongly associated with **celiac disease** and presents with distinct IgA deposits on direct immunofluorescence, unlike the IgG deposits seen in pemphigus vulgaris.
*Toxic epidermal necrolysis*
- Characterized by widespread **epidermal detachment**, often triggered by drugs, with fever and severe systemic symptoms, which are not detailed here.
- The onset is usually acute and rapid, leading to extensive "sheet-like" skin loss, rather than the more gradual progression described.
*Bullous pemphigoid*
- Presents with **tense bullae** on an erythematous or urticarial base, and while oral involvement can occur, it is less common and less severe than in pemphigus vulgaris.
- The **Nikolsky sign is typically negative** in bullous pemphigoid, and the blisters are subepidermal, remaining intact longer.
*Behcet’s disease*
- Characterized by **recurrent oral and genital aphthous ulcers**, along with ocular and skin lesions, but typically does not present with widespread blistering and positive Nikolsky sign.
- It is a multisystem inflammatory disorder, and the skin lesions are usually **erythema nodosum-like** or papulopustular, not extensive superficial erosions and blisters.
Vesiculobullous diseases US Medical PG Question 7: A 54-year-old man comes to the physician because of a cough with blood-tinged sputum for 1 week. He also reports fever and a 5-kg (11 lb) weight loss during the past 2 months. Over the past year, he has had 4 episodes of sinusitis. Physical examination shows palpable nonblanching skin lesions over the hands and feet. Examination of the nasal cavity shows ulceration of the nasopharyngeal mucosa and a depressed nasal bridge. Oral examination shows a painful erythematous gingival enlargement that bleeds easily on contact. Which of the following is the most likely cause of the patient's symptoms?
- A. Metalloprotease enzyme deficiency
- B. Malignant myeloid cell proliferation
- C. Arteriovenous malformation
- D. Immune complex deposition
- E. Neutrophil-mediated damage (Correct Answer)
Vesiculobullous diseases Explanation: ***Neutrophil-mediated damage***
- The constellation of **sinusitis**, **pulmonary symptoms** (cough with blood-tinged sputum), **renal involvement** (indicated by systemic symptoms and often associated with microhematuria in this condition), and **skin lesions (palpable purpura)**, along with **nasal ulceration**, a **depressed nasal bridge**, and **gingival enlargement**, is highly characteristic of **Granulomatosis with Polyangiitis (GPA)**.
- GPA is an **ANCA-associated vasculitis** characterized by **necrotizing granulomatous inflammation** and **vasculitis** of small to medium-sized vessels, primarily driven by **neutrophil activation** and subsequent tissue damage.
*Metalloprotease enzyme deficiency*
- This description commonly refers to conditions like **alpha-1 antitrypsin deficiency**, which primarily causes **emphysema** and liver disease, not the widespread vasculitic manifestations seen here.
- It does not explain the diverse multi-organ involvement including skin, ENT, and likely renal symptoms.
*Malignant myeloid cell proliferation*
- This would suggest conditions like **leukemia** or **myelodysplastic syndromes**, which present with altered blood counts, fatigue, infections, and bleeding, but typically not this specific pattern of vasculitis and granulomatous inflammation.
- While constitutional symptoms like weight loss can occur, the localized findings like depressed nasal bridge and gingival enlargement are not characteristic.
*Arteriovenous malformation*
- An **arteriovenous malformation (AVM)** is an abnormal connection between arteries and veins; depending on its location, it can cause bleeding (e.g., hemoptysis if pulmonary) or neurological symptoms if cerebral.
- However, AVMs do not explain the systemic inflammatory symptoms, skin lesions, sinusitis, depressed nasal bridge, or gingival changes.
*Immune complex deposition*
- **Immune complex vasculitis** (e.g., IgA vasculitis, cryoglobulinemic vasculitis) often presents with palpable purpura and can affect kidneys and GI tract.
- However, the prominent **granulomatous inflammation** causing **nasal ulceration** and **depressed nasal bridge**, and the specific type of **pulmonary-renal syndrome** seen in GPA, are more indicative of **ANCA-mediated neutrophil damage** rather than immune complex deposition.
Vesiculobullous diseases US Medical PG Question 8: A 72-year-old nursing home resident is complaining of pruritis. She is noted to have multiple, tense blisters on her trunk as well as the flexor surfaces of her extremities. The blisters have an erythematous base. You are unable to extend the blisters when you apply lateral traction. You suspect an autoimmune bullous dermatosis. Which of the following is the cause of the likely condition?
- A. Antibodies to epidermal transglutaminase
- B. Epidermal necrolysis
- C. Antibodies to hemidesmosomes (Correct Answer)
- D. Antibodies to desmoglein
- E. Antibodies to desmosomes
Vesiculobullous diseases Explanation: **Antibodies to hemidesmosomes**
- The patient's presentation with **tense blisters** that do not extend with lateral traction (negative Nikolsky sign) is classic for **bullous pemphigoid**.
- **Bullous pemphigoid** is an autoimmune disease caused by antibodies targeting components of the **hemidesmosomes** (specifically BP180 and BP230) at the dermal-epidermal junction.
*Antibodies to epidermal transglutaminase*
- Antibodies against **epidermal transglutaminase** are characteristic of **dermatitis herpetiformis**, which presents with intensely pruritic, grouped vesicles and papules, often on extensor surfaces.
- This condition is also associated with **celiac disease**, and its classic lesions are small and vesicular, not the large, tense bullae described.
*Epidermal necrolysis*
- **Epidermal necrolysis**, including Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN), is characterized by widespread epidermal detachment and necrosis, often triggered by medications.
- It presents with diffuse painful erythema and sheet-like skin loss, which is distinctly different from the described tense blisters of bullous pemphigoid.
*Antibodies to desmoglein*
- Antibodies to **desmoglein 1 and/or 3** (components of desmosomes) are the hallmark of **pemphigus vulgaris** and **pemphigus foliaceus**.
- These conditions cause **flaccid blisters** that are easily ruptured and often exhibit a positive Nikolsky sign, contrary to the tense blisters in this case.
*Antibodies to desmosomes*
- Antibodies to **desmosomes** (specifically desmogleins) lead to **pemphigus**, which is characterized by intraepidermal blistering and a positive Nikolsky sign.
- The described **tense blisters** and negative Nikolsky sign rule out pemphigus, where the defect is in keratinocyte adhesion within the epidermis.
Vesiculobullous diseases US Medical PG Question 9: You are seeing an otherwise healthy 66-year-old male in clinic who is complaining of localized back pain and a new rash. On physical exam, his vital signs are within normal limits. You note a vesicular rash restricted to the upper left side of his back. In order to confirm your suspected diagnosis, you perform a diagnostic test. What would you expect to find on the diagnostic test that was performed?
- A. Gram negative bacilli
- B. Branching pseudohyphae
- C. Pear shaped motile cells
- D. Multinucleated giant cells (Correct Answer)
- E. Gram positive cocci
Vesiculobullous diseases Explanation: ***Multinucleated giant cells***
- The patient's presentation of a **unilateral, vesicular rash** in an older adult, along with localized back pain, is highly suggestive of **herpes zoster (shingles)**.
- A Tzanck smear, a common diagnostic test for vesicular lesions, would reveal **multinucleated giant cells** and **intranuclear inclusions**, characteristic cytopathic effects of herpesviruses like VZV.
*Gram negative bacilli*
- This finding would suggest a **bacterial infection**, typically not associated with vesicular rashes like shingles.
- Gram-negative bacilli are often implicated in conditions such as **urinary tract infections** or **sepsis**, not dermatological viral infections.
*Branching pseudohyphae*
- This microscopic feature is characteristic of **fungal infections**, specifically **Candida species**, which present as a candidiasis rash, not a dermatomal vesicular rash.
- Fungal rashes are typically erythematous and can be pruritic but do not usually form discrete vesicles in a dermatomal distribution.
*Pear shaped motile cells*
- This describes **Trichomonas vaginalis**, a parasite causing sexually transmitted infections, primarily **vaginitis** or **urethritis**.
- This finding would be completely unrelated to a vesicular skin rash or the suspected diagnosis of shingles.
*Gram positive cocci*
- This finding is indicative of a **bacterial infection**, such as those caused by **Staphylococcus aureus** or **Streptococcus pyogenes**.
- While these bacteria can cause skin infections (e.g., impetigo, cellulitis), they do not produce the classic unilateral vesicular rash of shingles and would not involve multinucleated giant cells on microscopy.
Vesiculobullous diseases US Medical PG Question 10: A 50-year-old woman with rheumatoid arthritis on methotrexate develops rapidly progressive painful ulcers on her legs with violaceous undermined borders. Biopsy shows neutrophilic dermal infiltrate with areas of necrosis, but no vasculitis or infection. Wound cultures are negative. Despite debridement, the ulcers worsen. C-ANCA and P-ANCA are negative. Evaluate the diagnosis and determine the management that addresses both the cutaneous condition and systemic disease.
- A. Discontinue all immunosuppression to allow wound healing
- B. Increase methotrexate dose and add wound care
- C. Discontinue methotrexate, start cyclosporine and prednisone
- D. Start broad-spectrum antibiotics and surgical debridement
- E. Continue methotrexate, add TNF-alpha inhibitor and systemic corticosteroids (Correct Answer)
Vesiculobullous diseases Explanation: ***Continue methotrexate, add TNF-alpha inhibitor and systemic corticosteroids***
- This patient presents with **Pyoderma Gangrenosum (PG)**, a neutrophilic dermatosis characterized by **violaceous undermined borders** and **pathergy**, where surgical debridement cause lesion expansion.
- **TNF-alpha inhibitors** (e.g., adalimumab, infliximab) are first-line for recalcitrant PG and simultaneously provide excellent control for the underlying **Rheumatoid Arthritis**.
*Discontinue all immunosuppression to allow wound healing*
- Since PG is an **autoimmune inflammatory condition**, withdrawing immunosuppression would result in rapid progression of the ulcers rather than healing.
- Wound healing in PG requires **suppressing the inflammatory response** rather than the typical wound care approach for infected ulcers.
*Increase methotrexate dose and add wound care*
- While **methotrexate** treats RA, it is often insufficient as a monotherapy for the acute, rapidly progressive phase of **Pyoderma Gangrenosum**.
- Standard wound care alone is ineffective because the primary driver is **neutrophilic infilatration**, which requires targeted biologic or corticosteroid therapy.
*Discontinue methotrexate, start cyclosporine and prednisone*
- While **cyclosporine** and **prednisone** are used for PG, discontinuing methotrexate may lead to a flare of the patient’s **Rheumatoid Arthritis**.
- Maintaining a coordinated regimen that addresses both the skin and the joints, such as adding a **TNF-alpha inhibitor**, is preferred over switching all medications.
*Start broad-spectrum antibiotics and surgical debridement*
- **Surgical debridement** is contraindicated in PG due to **pathergy**, a phenomenon where trauma to the skin induces new or worsening lesions.
- **Antibiotics** are unnecessary as the biopsy and cultures confirmed a **sterile neutrophilic infiltrate** rather than an infectious process.
More Vesiculobullous diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.