Panniculitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Panniculitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Panniculitis US Medical PG Question 1: A previously healthy 46-year-old woman comes to her physician because of an itchy rash on her legs. She denies any recent trauma, insect bites, or travel. Her vital signs are within normal limits. Examination of the oral cavity shows white lace-like lines on the buccal mucosa. A photograph of the rash is shown. A biopsy specimen of the skin lesion is most likely to show which of the following?
- A. Inflammation of subcutaneous adipose tissue
- B. Proliferation of vascular endothelium
- C. Lymphocytes at the dermoepidermal junction (Correct Answer)
- D. Decreased thickness of the stratum granulosum
- E. Deposition of antibodies around epidermal cells
Panniculitis Explanation: ***Lymphocytes at the dermoepidermal junction***
- The patient's symptoms (itchy rash on legs, white lace-like lines on buccal mucosa) are classic for **lichen planus**.
- Skin biopsy in lichen planus typically shows a **dense band-like lymphocytic infiltrate** at the dermoepidermal junction, often obscuring the basal layer.
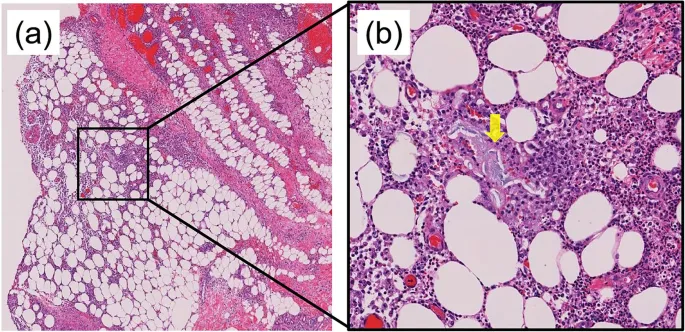
*Inflammation of subcutaneous adipose tissue*
- This finding, often called **panniculitis**, is seen in conditions like **erythema nodosum** or **lupus panniculitis**, which present differently.
- The rash described, particularly with oral involvement, does not suggest a primary inflammatory process in the subcutaneous fat.
*Proliferation of vascular endothelium*
- This is characteristic of **vascular tumors** or **vasculitis**, where there is an overgrowth or inflammation of blood vessel lining cells.
- The patient's presentation with an itchy rash and oral lesions is not consistent with these vascular conditions.
*Decreased thickness of the stratum granulosum*
- A **decreased or absent stratum granulosum** along with **parakeratosis** is a hallmark of **psoriasis**.
- The clinical features of psoriasis (silvery scales, extensor surface involvement) differ from those described for this patient.
*Deposition of antibodies around epidermal cells*
- This finding, particularly **intercellular antibody deposition**, is characteristic of pemphigus group diseases.
- While these can cause oral lesions, they typically present with **flaccid blisters** and erosions, not the lace-like pattern seen in lichen planus.
Panniculitis US Medical PG Question 2: A 55-year-old man is brought to the emergency room by his roommate due to an abdominal pain that started 2 hours ago. His pain is dull, aching, and radiates to the back. He admits to binge drinking alcohol for the past 2 days. Past medical history is significant for multiple admissions to the hospital for similar abdominal pain events, hypertension, and hyperlipidemia. He takes chlorthalidone and atorvastatin. He admits to heavy alcohol consumption over the past 10 years. He has smoked a pack of cigarettes a day for the last 20 years. In the emergency department, his temperature is 38.9℃ (102.0℉), pulse rate is 100/min, and respiratory rate is 28/min. On physical examination, he looks generally unwell and diaphoretic. Auscultation of his heart and lungs reveals an elevated heart rate with a regular rhythm. His lungs are clear to auscultation bilaterally. His abdomen is tympanitic with generalized tenderness. Evaluation of lab values reveals a leukocyte count of 28,000/mm3 with 89% of neutrophils. His amylase level is 255 U/L. A CT scan of the abdomen shows the diffuse enlargement of the pancreas. Which pathological process is most likely occurring in this patient’s peripancreatic tissue?
- A. Fat necrosis (Correct Answer)
- B. Caseous necrosis
- C. Fibrinoid necrosis
- D. Coagulative necrosis
- E. Liquefactive necrosis
Panniculitis Explanation: ***Fat necrosis***
- This patient presents with **acute pancreatitis**, characterized by severe epigastric pain radiating to the back, elevated amylase, and diffuse pancreatic enlargement on CT, all exacerbated by **binge drinking**.
- In acute pancreatitis, activated pancreatic enzymes, particularly **lipases**, leak into the peripancreatic fat, causing enzymatic breakdown of fat into fatty acids, which then combine with calcium to form **calcium soaps** (saponification), clinically recognizable as fat necrosis.
*Caseous necrosis*
- This type of necrosis is typically associated with **tuberculosis** and fungal infections, forming a cheesy, crumbly appearance.
- It involves a granulomatous inflammatory response and does not align with the enzyme-driven fat breakdown seen in pancreatitis.
*Fibrinoid necrosis*
- This is a vascular injury characterized by the deposition of **fibrin-like material** in arterial walls, often seen in immune-mediated vasculitis or severe hypertension.
- It is not a primary pathological process in the peripancreatic tissue during acute pancreatitis.
*Coagulative necrosis*
- This form of necrosis is characteristic of **ischemic injury** in most solid organs (e.g., heart, kidney) where the cellular architecture is preserved for some time.
- While pancreatic necrosis can occur, the specific breakdown of peripancreatic fat by lipases leads to fat necrosis, not coagulative necrosis of the fat itself.
*Liquefactive necrosis*
- This type of necrosis occurs in tissues rich in hydrolytic enzymes and low in structural proteins, such as the **brain after ischemia** or in **abscesses**.
- While pancreatic tissue undergoing severe necrosis can exhibit liquefaction, the specific process affecting the surrounding fat in pancreatitis is fat necrosis due to lipase activity.
Panniculitis US Medical PG Question 3: A 50-year-old Caucasian man is admitted to the ER with an 8-hour history of intense abdominal pain that radiates to the back, nausea, and multiple episodes of vomiting. Past medical history is insignificant. His blood pressure is 90/60 mm Hg, pulse is 120/min, respirations are 20/min, and body temperature is 37.8°C (100°F). Upon examination, he has significant epigastric tenderness, and hypoactive bowel sounds. Serum lipase and amylase are elevated and the patient rapidly deteriorates, requiring transfer to the intensive care unit for a month. After being stabilized, he is transferred to the general medicine floor with an abdominal computed tomography (CT) reporting a well-circumscribed collection of fluid of homogeneous density. Which of the following best describes the condition this patient has developed?
- A. Acute necrotic collection
- B. Fistula formation
- C. Walled-off necrosis
- D. Pancreatic pseudocyst (Correct Answer)
- E. Pancreatic cancer
Panniculitis Explanation: ***Pancreatic pseudocyst***
- The patient experienced an episode of **severe acute pancreatitis**, followed by the development of a well-circumscribed collection of fluid with homogeneous density, which is characteristic of a **pancreatic pseudocyst**.
- **Pseudocysts** are collections of pancreatic fluid and inflammatory exudates that become encapsulated by a fibrous wall, typically appearing around 4 weeks after an episode of acute pancreatitis.
*Acute necrotic collection*
- An **acute necrotic collection** is an early phase (within 4 weeks) of peripancreatic fluid collection that contains both fluid and non-viable pancreatic or peripancreatic tissue, which is not described as homogeneous in density.
- This term usually refers to the initial, unorganized collection of necrotic material, prior to the development of a well-defined wall.
*Fistula formation*
- **Fistula formation** involves an abnormal connection between two epithelialized organs or between an organ and the skin, which is not described by a well-circumscribed fluid collection.
- While it can be a complication of pancreatitis, the CT finding of a homogeneous fluid collection does not directly indicate a fistula.
*Walled-off necrosis*
- **Walled-off necrosis (WON)** is a mature collection (typically >4 weeks) of pancreatic and/or peripancreatic necrotic tissue that has developed a well-defined inflammatory wall but contains a significant solid/necrotic component.
- The CT description of a "homogeneous density" fluid collection does not align with WON, which would typically show heterogeneous density due to solid necrotic debris.
*Pancreatic cancer*
- **Pancreatic cancer** is an abnormal growth of cells within the pancreas and would typically present as a mass lesion, often with tissue invasion.
- While a pseudocyst can sometimes mimic a cystic tumor, the history of acute pancreatitis and the specific CT description of a homogeneous fluid collection make pancreatic cancer less likely in this context.
Panniculitis US Medical PG Question 4: A 27-year-old school teacher visits her doctor because of disfiguring skin lesions that started to appear in the past few days. The lesions are mostly located on her chest, shoulders, and back. They are 2–5 mm in diameter, droplike, erythematous papules with fine silver scales. Besides a sore throat and laryngitis requiring amoxicillin several weeks ago, she has no significant medical history. What is the most likely diagnosis?
- A. Bullous pemphigoid
- B. Plaque psoriasis
- C. Pemphigus vulgaris
- D. Guttate psoriasis (Correct Answer)
- E. Inverse psoriasis
Panniculitis Explanation: ***Guttate psoriasis***
- This condition is characterized by **acute onset** of **small (2–5 mm)**, **droplike**, erythematous papules with **fine silver scales**, predominantly on the trunk.
- It often follows an **upper respiratory tract infection**, particularly with *Streptococcus pyogenes*, as indicated by the recent **sore throat and laryngitis** requiring amoxicillin.
*Bullous pemphigoid*
- This autoimmune blistering disease primarily affects the **elderly** and presents with large, **tense bullae** on an erythematous or urticarial base.
- It does not typically present with small, scaly papules or have a direct association with recent streptococcal infections.
*Plaque psoriasis*
- The most common type of psoriasis, presenting with **well-demarcated**, erythematous plaques covered by **thick, silvery scales**, usually larger than 5 mm.
- While it can be found on the trunk, its lesions are typically larger and chronologically more stable than the acute, droplike lesions described.
*Pemphigus vulgaris*
- This is a severe autoimmune blistering disease characterized by **flaccid bullae** and erosions on the skin and **mucous membranes**.
- It involves intraepidermal blistering due to acantholysis and is not associated with recent sore throat or small, scaly papules.
*Inverse psoriasis*
- This form of psoriasis affects **skin folds** (e.g., axillae, groin, inframammary regions) and presents as **smooth, erythematous plaques** without significant scaling due to moisture.
- Its location and lack of typical scaling differ from the described lesions on the chest, shoulders, and back.
Panniculitis US Medical PG Question 5: A 29-year-old man presents to the clinic complaining of fatigue and loss of sensation in his lower legs. The patient notes no history of trauma or chronic disease but states that he spends a lot of time outside and often encounters wild animals. On examination, the patient has multiple dark lesions over the skin of his face and back, as well as a decreased sensation of fine touch and vibration bilaterally in the lower extremities. What is the morphology of the etiologic agent causing this patient’s symptoms?
- A. An acid-fast, intracellular bacillus (Correct Answer)
- B. Reactivation of latent viral infection
- C. Maltose-fermenting gram-negative diplococci
- D. A spirochete transmitted via tick
- E. Gram-positive, branching anaerobe
Panniculitis Explanation: ***An acid-fast, intracellular bacillus***
- The patient's symptoms (fatigue, loss of sensation in lower legs, dark skin lesions, exposure to wild animals, and decreased fine touch/vibration) are highly suggestive of **leprosy** (Hansen's disease).
- Leprosy is caused by **_Mycobacterium leprae_**, which is an **acid-fast, obligate intracellular bacillus** that preferentially infects macrophages and Schwann cells, leading to nerve damage and skin lesions.
*Reactivation of latent viral infection*
- While viral infections can cause neurological symptoms, the presentation with specific **dark skin lesions** and the history of exposure to **wild animals** (potentially armadillos, a reservoir for _M. leprae_) point away from a common latent viral reactivation.
- **Herpes zoster** (shingles) is a common reactivation of a latent viral infection (varicella-zoster virus), but it typically presents with a dermatomal rash and neuropathic pain rather than widespread dark lesions and bilateral sensory loss in the lower extremities.
*Maltose-fermenting gram-negative diplococci*
- **Maltose-fermenting gram-negative diplococci** describe **_Neisseria meningitidis_**, which causes meningitis.
- This organism primarily causes symptoms related to meningitis (fever, headache, neck stiffness), and does not typically present with the chronic sensory loss or characteristic skin lesions seen in this patient.
*A spirochete transmitted via tick*
- A **spirochete transmitted via a tick** refers to **_Borrelia burgdorferi_**, the causative agent of **Lyme disease**.
- Lyme disease presents with an **erythema migrans rash** (bull's-eye rash), joint pain, and neurological symptoms, but the skin lesions described here (multiple dark lesions) and the progressive sensory loss are not typical for Lyme disease.
*Gram-positive, branching anaerobe*
- A **gram-positive, branching anaerobe** describes **_Actinomyces_ species**, which cause **actinomycosis**.
- Actinomycosis typically presents with chronic abscesses and sinus tracts, often affecting the head and neck, thorax, or abdomen, and does not cause the diffuse sensory loss or skin lesions described in this case.
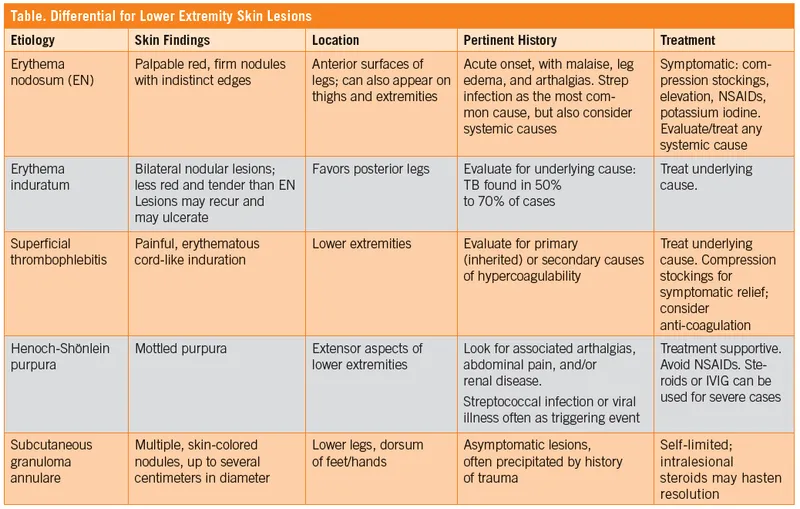
Panniculitis US Medical PG Question 6: A 22-year-old woman presents with multiple tender, erythematous nodules on her shins that developed over the past week. She reports having a sore throat 2 weeks ago. She also complains of joint pain and fatigue. Physical examination reveals raised, red, tender nodules on the anterior surface of both legs. Her temperature is 38.2°C. Which of the following is the most likely diagnosis?
- A. Cellulitis
- B. Erythema nodosum (Correct Answer)
- C. Sweet syndrome
- D. Superficial thrombophlebitis
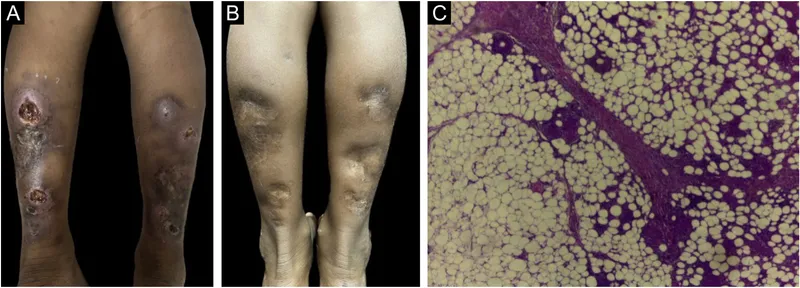
Panniculitis Explanation: ***Erythema nodosum***
- The presentation of **tender, erythematous nodules on the shins**, following a preceding **sore throat**, with associated **joint pain and fatigue**, is highly characteristic of **erythema nodosum**.
- It is a form of **panniculitis** typically triggered by infections (e.g., streptococcal pharyngitis), medications, or systemic diseases.
*Cellulitis*
- Characterized by a **warm, erythematous, swollen area** with poorly defined borders, often accompanied by pain and fever, but typically presents as a diffuse skin infection rather than distinct nodules.
- While fever is present, the **nodular nature** of the lesions and their bilateral, symmetrical distribution are less consistent with cellulitis.
*Sweet syndrome*
- Also known as acute febrile neutrophilic dermatosis, it presents with **tender erythematous plaques or nodules** and **fever**, but typically has a more prominent **neutrophilic infiltrate** histologically.
- Lesions of Sweet syndrome often appear on the **upper extremities, face, or neck**, and while it can affect the shins, the clinical picture here is more classic for erythema nodosum, especially given the history of sore throat.
*Superficial thrombophlebitis*
- Presents as a **palpable, tender, erythematous cord** along the course of a superficial vein, often with localized swelling and warmth.
- The lesions are typically **linear or cord-like**, not discrete nodules scattered over the shins, and are directly related to a thrombosed vein.
Panniculitis US Medical PG Question 7: A 50-year-old female presents to her physician with vesicles and tense blisters across her chest, arms, and the back of her shoulders. Physical examination reveals that blistering is not present in her oral mucosa, and the epidermis does not separate upon light stroking of the skin. The patient most likely suffers from a hypersensitivity reaction located:
- A. Linearly along the epidermal basement membrane (Correct Answer)
- B. In fat cells beneath the skin
- C. In nuclei within epidermal cells
- D. In net-like patterns around epidermal cells
- E. In granular deposits at the tips of dermal papillae
Panniculitis Explanation: ***Linearly along the epidermal basement membrane***
- The description of **tense blisters** and the absence of **Nikolsky's sign** (no epidermal separation with light stroking) are characteristic features of **bullous pemphigoid**.
- **Bullous pemphigoid** is an autoimmune disease where autoantibodies target components of the **hemidesmosomes** located along the **epidermal basement membrane**, leading to subepidermal blistering.
*In fat cells beneath the skin*
- This description is not consistent with any common blistering disorder, and **fat cells** (adipocytes) are not primary targets for blistering in autoimmune diseases.
- Blistering disorders typically involve the epidermis or the dermal-epidermal junction, not the subcutaneous fat.
*In nuclei within epidermal cells*
- Autoantibodies targeting **nuclear antigens** are associated with conditions like **lupus erythematosus**, but this generally leads to characteristic skin rashes, not tense blistering.
- Blistering from nuclear involvement is uncommon and does not match the clinical presentation of bullous pemphigoid or pemphigus.
*In net-like patterns around epidermal cells*
- This pattern of antibody deposition is characteristic of **pemphigus vulgaris**, where autoantibodies target **desmogleins** in the intercellular spaces of the epidermis.
- Pemphigus vulgaris typically presents with **flaccid blisters** that are easily rupturable, and often involves the **oral mucosa**, in contrast to the patient's presentation.
*In granular deposits at the tips of dermal papillae*
- This pattern of IgA deposition, particularly in a granular fashion at the **dermal papillae tips**, is characteristic of **dermatitis herpetiformis**.
- Dermatitis herpetiformis typically presents with **pruritic papules and vesicles**, often on extensor surfaces, and is commonly associated with **celiac disease**, which is not indicated here.
Panniculitis US Medical PG Question 8: An otherwise healthy 28-year-old woman comes to the physician because of a 14-day history of painful red nodules on her legs associated with malaise and mild joint pains. She reports that the nodules were initially smaller and distinct but some have fused together over the past 3–4 days and now appear like bruises. There is no preceding history of fever, trauma, or insect bites. Her vital signs are within normal limits. A photograph of the tender lesions on her shins is shown. The remainder of the examination shows no abnormalities. Complete blood count and antistreptolysin O (ASO) titers are within the reference range. Erythrocyte sedimentation rate is 30 mm/h. Which of the following is the most appropriate next step in management ?
- A. X-ray of the chest (Correct Answer)
- B. Skin biopsy
- C. Oral amoxicillin
- D. Stool culture
- E. Oral isoniazid
Panniculitis Explanation: ***X-ray of the chest***
- The patient's symptoms (painful red nodules on legs, malaise, mild joint pains, nodules fusing and appearing like bruises) are highly suggestive of **erythema nodosum**.
- Erythema nodosum is often associated with systemic conditions, and a chest X-ray is crucial to rule out **sarcoidosis** or **tuberculosis**, common underlying causes.
*Skin biopsy*
- While a skin biopsy could confirm the diagnosis of erythema nodosum, it is **not the most appropriate *next step* in management** as the clinical presentation is highly characteristic.
- The primary goal after suspecting erythema nodosum is to **identify and address the underlying cause**, which would then guide specific treatment.
*Oral amoxicillin*
- **Elevated ASO titers** would suggest an association with streptococcal infection, indicating antibiotic treatment; however, the patient's ASO titers are within the reference range.
- Erythema nodosum has **multiple potential causes**, and empiric antibiotic therapy without evidence of bacterial infection is not indicated.
*Stool culture*
- Stool culture would be relevant if there were clinical signs of a **gastrointestinal infection** (e.g., diarrhea) associated with infectious causes like *Salmonella*, *Yersinia*, or *Campylobacter*.
- The patient has no gastrointestinal symptoms, making a stool culture a **less likely initial investigation** in the absence of other clues.
*Oral isoniazid*
- Isoniazid is an **antibiotic used to treat tuberculosis**. While tuberculosis can cause erythema nodosum, there is currently no direct evidence (e.g., positive PPD, night sweats, persistent cough) to warrant tuberculosis treatment without further investigation.
- A **chest X-ray is a necessary first step** to screen for pulmonary tuberculosis before initiating antitubercular therapy.
Panniculitis US Medical PG Question 9: A 54-year-old man comes to the physician because of a cough with blood-tinged sputum for 1 week. He also reports fever and a 5-kg (11 lb) weight loss during the past 2 months. Over the past year, he has had 4 episodes of sinusitis. Physical examination shows palpable nonblanching skin lesions over the hands and feet. Examination of the nasal cavity shows ulceration of the nasopharyngeal mucosa and a depressed nasal bridge. Oral examination shows a painful erythematous gingival enlargement that bleeds easily on contact. Which of the following is the most likely cause of the patient's symptoms?
- A. Metalloprotease enzyme deficiency
- B. Malignant myeloid cell proliferation
- C. Arteriovenous malformation
- D. Immune complex deposition
- E. Neutrophil-mediated damage (Correct Answer)
Panniculitis Explanation: ***Neutrophil-mediated damage***
- The constellation of **sinusitis**, **pulmonary symptoms** (cough with blood-tinged sputum), **renal involvement** (indicated by systemic symptoms and often associated with microhematuria in this condition), and **skin lesions (palpable purpura)**, along with **nasal ulceration**, a **depressed nasal bridge**, and **gingival enlargement**, is highly characteristic of **Granulomatosis with Polyangiitis (GPA)**.
- GPA is an **ANCA-associated vasculitis** characterized by **necrotizing granulomatous inflammation** and **vasculitis** of small to medium-sized vessels, primarily driven by **neutrophil activation** and subsequent tissue damage.
*Metalloprotease enzyme deficiency*
- This description commonly refers to conditions like **alpha-1 antitrypsin deficiency**, which primarily causes **emphysema** and liver disease, not the widespread vasculitic manifestations seen here.
- It does not explain the diverse multi-organ involvement including skin, ENT, and likely renal symptoms.
*Malignant myeloid cell proliferation*
- This would suggest conditions like **leukemia** or **myelodysplastic syndromes**, which present with altered blood counts, fatigue, infections, and bleeding, but typically not this specific pattern of vasculitis and granulomatous inflammation.
- While constitutional symptoms like weight loss can occur, the localized findings like depressed nasal bridge and gingival enlargement are not characteristic.
*Arteriovenous malformation*
- An **arteriovenous malformation (AVM)** is an abnormal connection between arteries and veins; depending on its location, it can cause bleeding (e.g., hemoptysis if pulmonary) or neurological symptoms if cerebral.
- However, AVMs do not explain the systemic inflammatory symptoms, skin lesions, sinusitis, depressed nasal bridge, or gingival changes.
*Immune complex deposition*
- **Immune complex vasculitis** (e.g., IgA vasculitis, cryoglobulinemic vasculitis) often presents with palpable purpura and can affect kidneys and GI tract.
- However, the prominent **granulomatous inflammation** causing **nasal ulceration** and **depressed nasal bridge**, and the specific type of **pulmonary-renal syndrome** seen in GPA, are more indicative of **ANCA-mediated neutrophil damage** rather than immune complex deposition.
Panniculitis US Medical PG Question 10: A 37-year-old woman presents to the occupational health clinic for a new employee health screening. She has limited medical records prior to her immigration to the United States several years ago. She denies any current illness or significant medical history. Purified protein derivative (PPD) is injected on the inside of her left forearm for tuberculosis (TB) screening. Approximately 36 hours later, the patient comes back to the occupational health clinic and has an indurated lesion with bordering erythema measuring 15 mm in diameter at the site of PPD injection. Of the following options, which is the mechanism of her reaction?
- A. Type III and IV–mixed immune complex and cell-mediated hypersensitivity reactions
- B. Type III–immune complex-mediated hypersensitivity reaction
- C. Type I–anaphylactic hypersensitivity reaction
- D. Type II–cytotoxic hypersensitivity reaction
- E. Type IV–cell-mediated (delayed) hypersensitivity reaction (Correct Answer)
Panniculitis Explanation: ***Type IV–cell-mediated (delayed) hypersensitivity reaction***
- The **PPD test** for tuberculosis is a classic example of a **Type IV hypersensitivity reaction**, also known as **delayed-type hypersensitivity (DTH)**. This reaction is orchestrated by **T lymphocytes** (specifically CD4+ T cells) that recognize antigens presented by antigen-presenting cells
- The **induration** at 36 hours is a hallmark of this type of reaction, as it typically peaks between **24 to 72 hours** after antigen exposure, reflecting the time required for T cells to migrate to the site and initiate an inflammatory response. The immune response involves the release of **cytokines** leading to macrophage accumulation and localized tissue damage.
*Type III and IV–mixed immune complex and cell-mediated hypersensitivity reactions*
- While immune complexes (Type III) and cell-mediated reactions (Type IV) can both lead to tissue damage, a PPD test is primarily a **cell-mediated response** and is not characterized by significant immune complex deposition.
- Mixed reactions are less common and usually involve a sustained presence of antigen leading to both types of responses, which is not the typical mechanism for an acute PPD skin test.
*Type III–immune complex-mediated hypersensitivity reaction*
- **Type III hypersensitivity** is characterized by the formation of **antigen-antibody immune complexes** that deposit in tissues, leading to inflammation and tissue damage, often seen in conditions like serum sickness or lupus nephritis.
- The PPD reaction is based on T-cell recognition of mycobacterial antigens, not the deposition of soluble antigen-antibody complexes.
*Type I–anaphylactic hypersensitivity reaction*
- **Type I hypersensitivity** is an **immediate allergic reaction** mediated by **IgE antibodies** binding to mast cells and basophils, leading to histamine release upon re-exposure to an allergen.
- This type of reaction typically occurs within minutes of exposure, not 36 hours later, and presents with symptoms like hives, angioedema, or anaphylaxis.
*Type II–cytotoxic hypersensitivity reaction*
- **Type II hypersensitivity** involves **antibodies (IgG or IgM)** binding to antigens on the surface of **host cells**, leading to cell lysis or dysfunction, often seen in transfusion reactions or autoimmune hemolytic anemia.
- The PPD test does not involve direct antibody-mediated destruction of host cells.
More Panniculitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.