Non-melanoma skin cancers US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Non-melanoma skin cancers. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Non-melanoma skin cancers US Medical PG Question 1: A 72-year-old man presents to the clinic for the evaluation of a lesion on his nose that has been slowly getting larger for the past 2 months. The patient notes no history of trauma, pruritus, or pain, but states that the size of the lesion is making his nose feel uncomfortable. On exam, the nodule is pink with rolled borders. Telangiectasias are also present within the lesion, with central ulceration. What is the characteristic histologic appearance of this lesion?
- A. Palisading nuclei (Correct Answer)
- B. Keratin pearls
- C. Sawtooth lymphocytic infiltrate
- D. Epidermal hyperplasia with cutaneous darkening
- E. Atypical melanocytes
Non-melanoma skin cancers Explanation: ***Palisading nuclei***
- The clinical presentation of a **slowly enlarging, pink nodule with rolled borders**, **telangiectasias**, and **central ulceration** on the nose is highly suggestive of **basal cell carcinoma (BCC)**.
- Histologically, BCC is characterized by nests of **basaloid cells** with **palisading nuclei** at the periphery of the tumor nests.
*Keratin pearls*
- **Keratin pearls**, or **dyskeratosis**, are characteristic histologic features of **squamous cell carcinoma (SCC)**, which typically presents with a more scaly or ulcerating lesion, often firmer and redder.
- While SCC can ulcerate, the **rolled borders** and **telangiectasias** are less common than in BCC.
*Sawtooth lymphocytic infiltrate*
- A **sawtooth lymphocytic infiltrate** at the dermo-epidermal junction is a classic histological finding in **lichen planus**, a pruritic, papular rash.
- This condition does not match the description of a solitary, enlarging nodule on the nose.
*Epidermal hyperplasia with cutaneous darkening*
- **Epidermal hyperplasia with cutaneous darkening** (acanthosis nigricans) is a velvety, hyperpigmented thickening of the skin, often associated with insulin resistance or malignancy.
- This is a diffuse skin change and does not resemble the localized, nodular lesion described.
*Atypical melanocytes*
- The presence of **atypical melanocytes** in the epidermis and/or dermis is characteristic of **melanoma** or precursor lesions like dysplastic nevi.
- Melanoma lesions typically show irregular borders, varied pigmentation, and rapid growth, which differ from the described lesion.
Non-melanoma skin cancers US Medical PG Question 2: A 34-year-old man presents to the office for evaluation of a lesion on his upper arm that appeared a few months ago and has not healed. The patient appears healthful but has a history of cardiovascular disease. He states that his friend at the industrial ammunition factory where he works told him he should "get it looked at." The patient admits to some nausea, vomiting, and diarrhea over the past year, but he states that he "feels fine now." On physical examination, the lesion is an erythematous, scaly, ulcerated plaque on the flexor surface of his upper arm. The rest of the exam is within normal limits. What is the most likely diagnosis?
- A. Squamous cell carcinoma (SCC) (Correct Answer)
- B. Erythema multiforme
- C. Actinic keratosis
- D. Erysipelas
- E. Contact dermatitis
Non-melanoma skin cancers Explanation: ***Squamous cell carcinoma (SCC)***
- The patient's occupational exposure to chemicals at an **ammunition factory**, along with chronic non-healing, **ulcerated, scaly plaque**, raises suspicion for SCC, particularly **arsenic-induced SCC**.
- His history of vague **gastrointestinal symptoms** (nausea, vomiting, diarrhea) over the past year is also consistent with **chronic arsenic exposure**, which is a known carcinogen.
*Erythema multiforme*
- This is an **acute, self-limiting hypersensitivity reaction** to medications or infections, characterized by target lesions, not a chronic, non-healing ulcerated plaque.
- It would not typically present with a history of chronic GI symptoms related to occupational exposure.
*Actinic keratosis*
- This is a **precancerous lesion** caused by chronic sun exposure, typically presenting as a rough, scaly patch on sun-exposed areas.
- While it has malignant potential to transform into SCC, the description of an **ulcerated, non-healing lesion** with a history of probable chemical exposure makes SCC a more likely *current* diagnosis.
*Erysipelas*
- Erysipelas is a **superficial bacterial infection** of the skin characterized by a rapidly spreading, bright red, well-demarcated, and painful rash, often accompanied by fever and systemic symptoms.
- It would not manifest as a chronic, non-healing ulcerated plaque over several months.
*Contact dermatitis*
- This is an **inflammatory skin reaction** due to direct contact with an allergen or irritant, typically presenting as an itchy, erythematous rash with vesicles or papules.
- It would not typically result in a chronic, ulcerated, non-healing plaque and is not associated with the systemic symptoms or occupational exposure history presented.
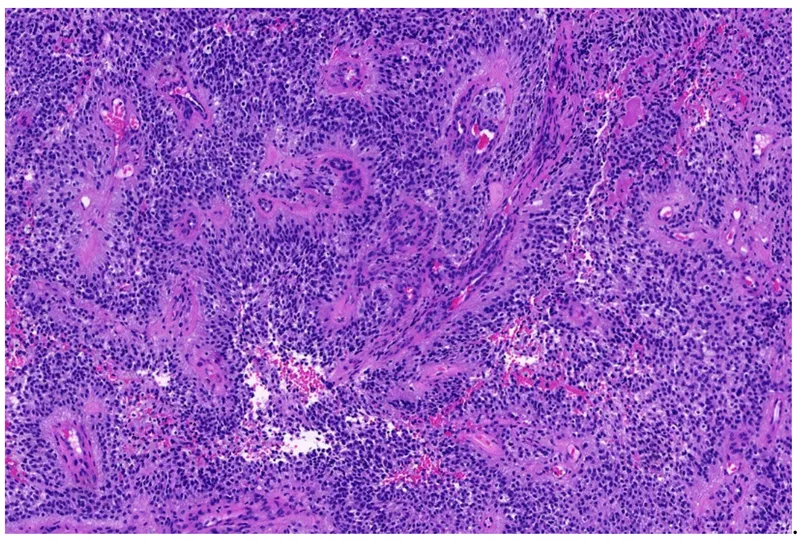
Non-melanoma skin cancers US Medical PG Question 3: A 67-year-old man is referred to a dermatologist after a reddish mole appears on his nose. The mole’s size has changed over the last 2 years, and occasional bleeding is noted. The man’s medical history is unremarkable, and he does not take any medications. He retired from his construction job 15 years ago. Physical examination of his nose reveals a 2-cm pink papule with a pearly appearance and overlying telangiectasia on the ala of the nose (see image). Which of the following would be the best treatment modality if surgery is not an option?
- A. Radiation therapy (Correct Answer)
- B. Imiquimod
- C. Interferon
- D. 5-fluorouracil
- E. Photodynamic therapy
Non-melanoma skin cancers Explanation: ***Radiation therapy***
- This patient's presentation is highly suggestive of **basal cell carcinoma (BCC)**, given the reddish, pearly papule with telangiectasias on a sun-exposed area, a history of growth over two years, bleeding, and his prior occupation as a construction worker. **Radiation therapy** is an excellent option for **localized BCC** when surgery is contraindicated or not feasible due to patient preferences, tumor location (e.g., cosmetic areas), or medical comorbidities.
- **Definitive radiation therapy** can achieve high cure rates for BCC, comparable to Mohs surgery for appropriately selected superficial and nodular types, and is particularly useful in older patients.
*Imiquimod*
- **Imiquimod** is an **immune-response modifier** used topically for superficial BCCs, actinic keratoses, and external genital warts.
- While effective for **superficial BCCs**, its efficacy is lower for nodular or infiltrative BCCs, which appears more likely given the size (2 cm) and depth implied by chronic bleeding and growth over 2 years.
*Interferon*
- **Interferon** has been explored as an intralesional treatment for BCC, but it is **not a first-line or standard treatment option** due to variable response rates and the availability of more effective and reliable modalities.
- Its use is generally reserved for more advanced or difficult-to-treat cases, typically as part of clinical trials or for very specific indications, not as a primary treatment for a localized BCC where surgery or radiation is an option.
*5-fluorouracil*
- **5-fluorouracil (5-FU)** is a **topical chemotherapeutic agent** used primarily for **actinic keratoses** and **superficial BCCs**.
- Similar to imiquimod, its efficacy is limited to **superficial lesions** and is less effective for nodular, infiltrative, or larger BCCs due to insufficient penetration and risk of recurrence.
*Photodynamic therapy*
- **Photodynamic therapy (PDT)** involves applying a photosensitizing agent followed by exposure to specific wavelengths of light, primarily used for **actinic keratoses** and **superficial BCCs**.
- While effective for superficial lesions, its efficacy significantly decreases for **nodular BCCs** or those with deeper invasion, making it less suitable for a 2 cm lesion that has been growing and bleeding.
Non-melanoma skin cancers US Medical PG Question 4: A 39-year-old woman comes to the physician for a follow-up examination after a colonoscopy showed 42 hamartomatous polyps. The physical examination findings are shown in the photograph. Which of the following conditions is most likely to develop in this patient?
- A. Mandibular osteoma
- B. Malignant melanoma
- C. Hepatocellular carcinoma
- D. Medulloblastoma
- E. Pancreatic carcinoma (Correct Answer)
Non-melanoma skin cancers Explanation: ***Pancreatic carcinoma***
- The image shows **perioral hyperpigmentation** (melanin spots on the lips and oral mucosa) and hamartomatous polyps in the colon, which are classic features of **Peutz-Jeghers syndrome**.
- Peutz-Jeghers syndrome is an autosomal dominant disorder that significantly increases the risk of various cancers, most notably **pancreatic carcinoma**, as well as gastric, small bowel, lung, breast, and gynecological cancers.
*Mandibular osteoma*
- **Mandibular osteomas** are characteristic of **Gardner syndrome**, a variant of Familial Adenomatous Polyposis, which involves hundreds of adenomatous polyps, not hamartomatous polyps as described in the case.
- Gardner syndrome also presents with other extra-colonic manifestations like epidermoid cysts and desmoid tumors, which are not suggested by the provided information.
*Malignant melanoma*
- While Peutz-Jeghers syndrome involves **mucocutaneous pigmentation**, these are typically benign melanin macules and do not progress to **malignant melanoma**.
- Malignant melanoma is a skin cancer linked to UV exposure and certain genetic predispositions, but not a primary manifestation or increased risk in Peutz-Jeghers syndrome beyond general population risk.
*Hepatocellular carcinoma*
- **Hepatocellular carcinoma** is strongly associated with chronic liver diseases such as **hepatitis B and C infections**, alcoholism, and non-alcoholic fatty liver disease.
- There is no direct significant increased risk of hepatocellular carcinoma specifically linked to Peutz-Jeghers syndrome.
*Medulloblastoma*
- **Medulloblastoma** is a common malignant brain tumor in children, often associated with syndromes like **Gorlin syndrome** (Nevoid Basal Cell Carcinoma Syndrome) or Turcot syndrome, but not Peutz-Jeghers syndrome.
- The patient's age and presenting features do not align with known risk factors for medulloblastoma.
Non-melanoma skin cancers US Medical PG Question 5: A 63-year-old man comes to the physician for the evaluation of a skin lesion on his chest. He first noticed the lesion 2 months ago and thinks that it has increased in size since then. The lesion is not painful or pruritic. He has type 2 diabetes mellitus, hypercholesterolemia, and glaucoma. The patient has smoked 1 pack of cigarettes daily for the last 40 years and drinks two to three beers on the weekend. Current medications include metformin, atorvastatin, topical timolol, and a multivitamin. Vital signs are within normal limits. The lesion is partly elevated on palpation and does not change its form on pinching. A photograph of the lesion is shown. Which of the following is the most likely diagnosis?
- A. Seborrheic keratosis
- B. Malignant melanoma (Correct Answer)
- C. Keratoacanthoma
- D. Basal cell carcinoma
- E. Lentigo maligna
Non-melanoma skin cancers Explanation: ***Malignant melanoma***
- The lesion's **recent growth** and **elevated, irregular appearance** (as suggested by "partly elevated on palpation and does not change its form on pinching," implying a solid, infiltrative nature) in a patient with a history of **significant sun exposure** (implied by age and lesion location) are highly suspicious for melanoma.
- While visual representation is key, this description aligns with a potentially advanced melanoma, characterized by **asymmetry, irregular borders, varied color, and a diameter greater than 6mm (ABCD rule)**, especially given the reported growth.
*Seborrheic keratosis*
- Typically presents as a **"stuck-on"** appearance, often described as velvety or warty, and is usually **benign** and grows slowly, if at all.
- The elevated, firm nature of the described lesion that does not change on pinching is less consistent with the soft, waxy texture often found in seborrheic keratosis.
*Keratoacanthoma*
- Characterized by rapid growth over weeks to months, often forming a **dome-shaped nodule with a central keratotic plug**.
- While it can grow quickly, the detailed description and the potential for a more variegated appearance (melanoma) are not fully captured by this option, and it often has spontaneous regression, which is not suggested here.
*Basal cell carcinoma*
- Most commonly presents as a **pearly nodule with telangiectasias**, or a **rolled border** with central ulceration.
- While it can be elevated and solid, the description of rapid growth and the implication of an irregular clinical appearance (without direct visualization) make melanoma a stronger consideration.
*Lentigo maligna*
- This is a form of melanoma in situ that typically appears as a **slowly enlarging, flat, irregularly shaped, and variegated brown-to-black patch** on chronically sun-damaged skin.
- Although the patient's age and lesion location fit, the description of "partly elevated on palpation" suggests a more invasive lesion, making **malignant melanoma** (which encompasses invasive forms) a more appropriate diagnosis.
Non-melanoma skin cancers US Medical PG Question 6: A 51-year-old woman presents to the dermatologist with concern for a new skin lesion (Image A). You note two similar lesions on her back. Which of the following is a true statement about these lesions?
- A. They must be followed closely for concern of malignancy.
- B. They will likely regress spontaneously.
- C. They may be associated with von Hippel-Lindau disease.
- D. They will likely grow rapidly.
- E. They will likely increase in number over time. (Correct Answer)
Non-melanoma skin cancers Explanation: ***They will likely increase in number over time.***
- The image likely displays **cherry angiomas**, which are common benign vascular lesions that typically increase in number with age.
- While individual lesions may remain stable, their overall prevalence on the skin tends to rise as a person ages, especially after the age of 30.
*They must be followed closely for concern of malignancy.*
- **Cherry angiomas** are **benign vascular proliferations** and do not carry a risk of malignant transformation.
- They are typically diagnosed clinically and do not require ongoing surveillance for malignancy.
*They will likely regress spontaneously.*
- **Cherry angiomas** are **permanent lesions** and do not typically regress spontaneously.
- Once they appear, they usually persist and often grow slightly in size over time.
*They may be associated with von Hippel-Lindau disease.*
- **Von Hippel-Lindau (VHL) disease** is associated with **hemangioblastomas** (in the CNS and retina), **pheochromocytomas**, and **renal cell carcinoma**, but not typically cherry angiomas.
- The characteristic skin lesions in VHL are often **cutaneous cavernous hemangiomas** or **capillary malformations**, not the common cherry angioma.
*They will likely grow rapidly.*
- While cherry angiomas can slowly increase in size over many years, they do **not typically grow rapidly**.
- Rapid growth of a cutaneous lesion would be a more concerning feature for other conditions, such as **malignant melanoma** or a **rapidly growing cyst**, not cherry angiomas.
Non-melanoma skin cancers US Medical PG Question 7: A 62-year-old man seeks evaluation at an outpatient clinic for a single, red, crusty lesion on the shaft of his penis and a similar lesion on the middle finger of his left hand. He recently immigrated to the US from Africa. The lesions are painless and the physicians in his country treated him for syphilis and eczema, with no improvement. He lives with his 4th wife. He smokes 2 packs of cigarette per day and has been doing so for the last 30 years. He is not aware of any family members with malignancies or hereditary diseases. The physical examination is remarkable for an erythematous plaque, with areas of crusting, oozing, and irregular borders on the dorsal surface of the penile shaft and a similar lesion on his left middle finger (shown in the picture). The regional lymph nodes are not affected. A biopsy is obtained and the pathologic evaluation reveals cells with nuclear hyperchromasia, multinucleation, and increased mitotic figures within the epidermis. What is the most likely diagnosis?
- A. Bowen's disease (Correct Answer)
- B. Bowenoid papulosis
- C. Erythroplasia of Queyrat
- D. Lichen sclerosus
- E. Condyloma acuminata
Non-melanoma skin cancers Explanation: ***Bowen's disease***
- The patient presents with **solitary, erythematous, crusty lesions on the penile shaft and finger**, which are characteristic of Bowen's disease, an in situ squamous cell carcinoma. The histological findings of **nuclear hyperchromasia, multinucleation, and increased mitotic figures within the epidermis** further confirm this diagnosis.
- The **lack of improvement with syphilis and eczema treatments** and the patient's **smoking history** (a risk factor for SCC) support this diagnosis over benign conditions.
*Bowenoid papulosis*
- This condition typically presents as **multiple, small, reddish-brown to violaceous papules**, often in the genital area of younger individuals.
- Unlike Bowen's disease, it is generally considered a **benign or low-grade intraepithelial neoplasia** with a lower risk of progression to invasive cancer.
*Erythroplasia of Queyrat*
- This is a form of **squamous cell carcinoma in situ** that specifically affects the **glans penis or prepuce**, presenting as a well-demarcated, velvety, erythematous patch.
- While histologically similar to Bowen's disease, the patient's lesion is on the **penile shaft and finger**, making Bowen's disease a more encompassing diagnosis for both sites.
*Lichen sclerosus*
- This is a **chronic inflammatory skin condition** characterized by **atrophic, white, sclerotic plaques**, often on the genitals.
- It does not present with the **crusting, oozing, and irregular borders** described, nor the specific histological features of squamous cell carcinoma in situ.
*Condyloma acuminata*
- These are **genital warts caused by HPV**, appearing as soft, flesh-colored, verrucous papules or plaques.
- They typically lack the **crusting, oozing, and histological features of severe atypia and increased mitotic figures** seen in this patient's biopsy.
Non-melanoma skin cancers US Medical PG Question 8: A 61-year-old Caucasian male presents to your office complaining of morning headaches of 6 weeks duration. A head MRI reveals a likely metastasis of unknown origin in the supratentorial region of the brain. On biopsy, the neoplastic mass is shown to have a mutation in BRAF, a protein kinase, in which a glutamic acid is substituted for valine at position 600 of the protein. Where did this metastasis most likely originate?
- A. Stomach
- B. Skin (Correct Answer)
- C. Breast
- D. Brain
- E. Bone
Non-melanoma skin cancers Explanation: ***Skin***
- A brain metastasis with a **V600E BRAF mutation** is highly suggestive of **melanoma**, a type of skin cancer.
- Melanoma frequently metastasizes to the **brain**, and the BRAF V600E mutation is a common and actionable target in advanced melanoma.
*Stomach*
- Stomach cancers (gastric adenocarcinomas) less commonly metastasize to the brain compared to melanoma.
- While BRAF mutations can occur in gastric cancer, the **V600E mutation** is not typically a defining feature of gastric cancer metastases to the brain.
*Breast*
- Breast cancer can metastasize to the brain, but the presence of a **BRAF V600E mutation** is not a characteristic genetic alteration for breast cancer.
- Common mutations in breast cancer include those in **ER, PR, and HER2** receptors or **PIK3CA**, not BRAF V600E.
*Brain*
- The question states the mass is a **metastasis of unknown origin**, implying it did not originate in the brain itself.
- Primary brain tumors like **gliomas** would not be described as metastases and have a different mutational spectrum.
*Bone*
- Bone cancers (sarcomas) or metastases to the bone usually do not present with a **BRAF V600E mutation** as their primary driver for brain metastasis.
- While various cancers can metastasize to bone, the specific mutation points away from a bone origin.
Non-melanoma skin cancers US Medical PG Question 9: A 72-year-old man comes to the physician because of a lesion on his eyelid for 6 months. The lesion is not painful or pruritic. He initially dismissed it as a 'skin tag' but the lesion has increased in size over the past 3 months. He has type 2 diabetes mellitus, coronary artery disease, and left hemiplegia from a stroke 3 years ago. Current medications include sitagliptin, metformin, aspirin, and simvastatin. He used to work as a construction contractor and retired 3 years ago. Examination shows a 1-cm (0.4-in) flesh-colored, nodular, nontender lesion with rolled borders. There is no lymphadenopathy. Cardiopulmonary examination shows no abnormalities. Muscle strength is reduced in the left upper and lower extremities. Visual acuity is 20/20. The pupils are equal and reactive to light. A shave biopsy confirms the diagnosis of basal cell carcinoma. Which of the following is the most appropriate next step in management?
- A. Laser ablation
- B. Cryotherapy
- C. Topical chemotherapy
- D. Wide local excision
- E. Mohs micrographic surgery (Correct Answer)
Non-melanoma skin cancers Explanation: ***Mohs micrographic surgery***
- The lesion's location on the **eyelid** (a cosmetically and functionally sensitive area), its **nodular appearance** with **rolled borders**, and the likely diagnosis of **basal cell carcinoma (BCC)** make Mohs surgery the most appropriate treatment.
- Mohs surgery offers the highest cure rates for BCCs and preserves the maximum amount of healthy tissue, which is crucial for lesions on the face and eyelids.
*Wide local excision*
- While effective for many skin cancers, **wide local excision** might lead to significant cosmetic or functional defects on the eyelid due to the need for a wider margin of healthy tissue removal.
- Its cure rates are generally lower than Mohs surgery for high-risk BCCs, especially in sensitive areas.
*Laser ablation*
- **Laser ablation** is typically used for superficial or precancerous lesions, not for nodular, invasive basal cell carcinoma.
- It does not allow for histological margin control, which is essential to ensure complete tumor removal and reduce recurrence.
*Cryotherapy*
- **Cryotherapy** is suitable for small, superficial, or pre-malignant lesions, but not for a nodular lesion on the eyelid where tissue preservation and precise margin control are critical.
- It does not offer histological confirmation of clear margins, increasing the risk of recurrence.
*Topical chemotherapy*
- **Topical chemotherapy** (e.g., imiquimod, 5-fluorouracil) is generally reserved for superficial basal cell carcinomas distant from critical structures.
- It is not effective for nodular BCCs and lacks the ability to confirm complete tumor removal via microscopic margin assessment.
Non-melanoma skin cancers US Medical PG Question 10: A 62-year-old woman comes to the physician for evaluation of a mole on her forearm that has increased in size over the last several months. Physical examination shows a 9-mm skin lesion on the right forearm with irregular borders. An excisional biopsy is performed, and genetic analysis shows a mutation in the gene that encodes B-Raf. Which of the following cellular events most likely predisposed this patient to developing this skin lesion?
- A. Deamination of cytosine, guanine, and adenine nucleotides
- B. Relocation of a chromosomal segment onto a nonhomologous chromosome
- C. Formation of covalent bonds between adjacent pyrimidine bases (Correct Answer)
- D. Insufficient phosphorylation of p53
- E. Double-strand breaks in DNA molecules
Non-melanoma skin cancers Explanation: ***Formation of covalent bonds between adjacent pyrimidine bases***
- This describes **pyrimidine dimers**, typically **thymine dimers**, which are formed due to **UV radiation exposure**.
- UV radiation is the primary environmental risk factor for **melanoma**, and the **B-Raf mutation** (common in melanoma) is often linked to these UV-induced DNA lesions.
*Deamination of cytosine, guanine, and adenine nucleotides*
- **Deamination** is a chemical alteration of DNA bases that can lead to mutations, but it is not the most direct or common mechanism for UV-induced melanoma.
- While deamination can occur spontaneously or be induced by certain chemicals, it is not the primary event linked to **UV radiation** and **B-Raf mutations** in melanoma.
*Relocation of a chromosomal segment onto a nonhomologous chromosome*
- This describes a **translocation**, a type of chromosomal rearrangement.
- While translocations can be associated with some cancers (e.g., leukemias, sarcomas), they are not the typical mechanism for initiating **melanoma** or directly causing **B-Raf mutations**.
*Insufficient phosphorylation of p53*
- **p53 phosphorylation** is crucial for its activation as a tumor suppressor protein, and insufficient phosphorylation would impair its function.
- However, the direct cause of this specific melanoma with a **B-Raf mutation** is usually DNA damage (like pyrimidine dimers) rather than a primary defect in p53 phosphorylation.
*Double-strand breaks in DNA molecules*
- **Double-strand breaks (DSBs)** are highly deleterious DNA lesions that can lead to chromosomal rearrangements or cell death if not repaired.
- While DSBs can be caused by various factors, including high-energy radiation, they are not the most common or characteristic DNA lesion specifically implicated in the initiation of **melanoma** due to UV exposure and subsequent **B-Raf mutation**.
More Non-melanoma skin cancers US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.