Melanoma pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Melanoma pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Melanoma pathology US Medical PG Question 1: A research team develops a new monoclonal antibody checkpoint inhibitor for advanced melanoma that has shown promise in animal studies as well as high efficacy and low toxicity in early phase human clinical trials. The research team would now like to compare this drug to existing standard of care immunotherapy for advanced melanoma. The research team decides to conduct a non-randomized study where the novel drug will be offered to patients who are deemed to be at risk for toxicity with the current standard of care immunotherapy, while patients without such risk factors will receive the standard treatment. Which of the following best describes the level of evidence that this study can offer?
- A. Level 1
- B. Level 3 (Correct Answer)
- C. Level 5
- D. Level 4
- E. Level 2
Melanoma pathology Explanation: ***Level 3***
- A **non-randomized controlled trial** like the one described, where patient assignment to treatment groups is based on specific characteristics (risk of toxicity), falls into Level 3 evidence.
- This level typically includes **non-randomized controlled trials** and **well-designed cohort studies** with comparison groups, which are prone to selection bias and confounding.
- The study compares two treatments but lacks randomization, making it Level 3 evidence.
*Level 1*
- Level 1 evidence is the **highest level of evidence**, derived from **systematic reviews and meta-analyses** of multiple well-designed randomized controlled trials or large, high-quality randomized controlled trials.
- The described study is explicitly stated as non-randomized, ruling out Level 1.
*Level 2*
- Level 2 evidence involves at least one **well-designed randomized controlled trial** (RCT) or **systematic reviews** of randomized trials.
- The current study is *non-randomized*, which means it cannot be classified as Level 2 evidence, as randomization is a key criterion for this level.
*Level 4*
- Level 4 evidence includes **case series**, **case-control studies**, and **poorly designed cohort or case-control studies**.
- While the study is non-randomized, it is a controlled comparative trial rather than a case series or retrospective case-control study, placing it at Level 3.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, typically consisting of **expert opinion** without explicit critical appraisal, or based on physiology, bench research, or animal studies.
- While the drug was initially tested in animal studies, the current human comparative study offers a higher level of evidence than expert opinion or preclinical data.
Melanoma pathology US Medical PG Question 2: A 67-year-old woman presents to a surgeon with a painless, slowly growing ulcer in the periauricular region for the last 2 months. On physical examination, there is an irregular-shaped ulcer, 2 cm x 1 cm in its dimensions, with irregular margins and crusting over the surface. The woman is a fair-skinned individual who loves to go sunbathing. There is no family history of malignancy. After a complete physical examination, the surgeon performs a biopsy of the lesion under local anesthesia and sends the tissue for histopathological examination. The pathologist confirms the diagnosis of squamous cell carcinoma of the skin. When she asks about the cause, the surgeon explains that there are many possible causes, but it is likely that she has developed squamous cell carcinoma on her face due to repeated exposure to ultraviolet rays from the sun, especially ultraviolet B (UVB) rays. If the surgeon’s opinion is correct, which of the following mechanisms is most likely involved in the pathogenesis of the condition?
- A. Upregulation of expression of cyclin D2
- B. Loss-of-function mutations of TP53
- C. Activation of transcription factor NF-κB
- D. Intrastrand cross-linking of thymidine residues in DNA (Correct Answer)
- E. DNA damage caused by the formation of reactive oxygen species
Melanoma pathology Explanation: ***Intrastrand cross-linking of thymidine residues in DNA***
- **UVB radiation** primarily causes direct DNA damage, leading to the formation of **pyrimidine dimers**, particularly cyclobutane pyrimidine dimers (CPDs) and pyrimidine-pyrimidone (6-4) photoproducts.
- This **intrastrand cross-linking** between adjacent thymidine or cytosine bases on the same DNA strand disrupts the DNA structure and interferes with DNA replication and transcription, promoting mutations that can initiate carcinogenesis.
*Upregulation of expression of cyclin D2*
- While **cyclin D2** is involved in cell cycle progression, its upregulation is a downstream effect of various oncogenic pathways and not the *direct mechanism* of DNA damage by UVB.
- **UVB's primary action** is DNA damage, which then secondarily drives cellular responses potentially including altered cell cycle protein expression.
*Loss-of-function mutations of TP53*
- **TP53 mutations** are very common in skin cancers, especially squamous cell carcinoma, and greatly contribute to carcinogenesis by abolishing tumor suppressor functions.
- However, the *primary mechanism* by which **UVB** causes these mutations is through direct DNA damage, specifically the induction of pyrimidine dimers that are then misrepaired, leading to TP53 mutations as a *consequence* rather than the initial mechanism.
*Activation of transcription factor NF-κB*
- **NF-κB activation** is involved in inflammatory responses and cell survival pathways, which can contribute to tumor progression.
- While UVB can activate NF-κB, this is a **downstream signaling event** in response to cellular stress and damage, not the primary mechanism of **UVB-induced DNA damage**.
*DNA damage caused by the formation of reactive oxygen species*
- **Reactive oxygen species (ROS)** are a major cause of DNA damage, often associated with **UVA radiation** and oxidative stress.
- However, **UVB radiation** primarily causes *direct DNA damage* through the formation of pyrimidine dimers, rather than indirectly through ROS generation as its main carcinogenic effect.
Melanoma pathology US Medical PG Question 3: A 52-year-old Caucasian man presents to the clinic for evaluation of a mole on his back that he finds concerning. He states that his wife noticed the lesion and believes that it has been getting larger. On inspection, the lesion is 10 mm in diameter with irregular borders. A biopsy is performed. Pathology reveals abnormal melanocytes forming nests at the dermo-epidermal junction and discohesive cell growth into the epidermis. What is the most likely diagnosis?
- A. Desmoplastic melanoma
- B. Lentigo maligna melanoma
- C. Superficial spreading melanoma (Correct Answer)
- D. Nodular melanoma
- E. Acral lentiginous melanoma
Melanoma pathology Explanation: ***Superficial spreading melanoma***
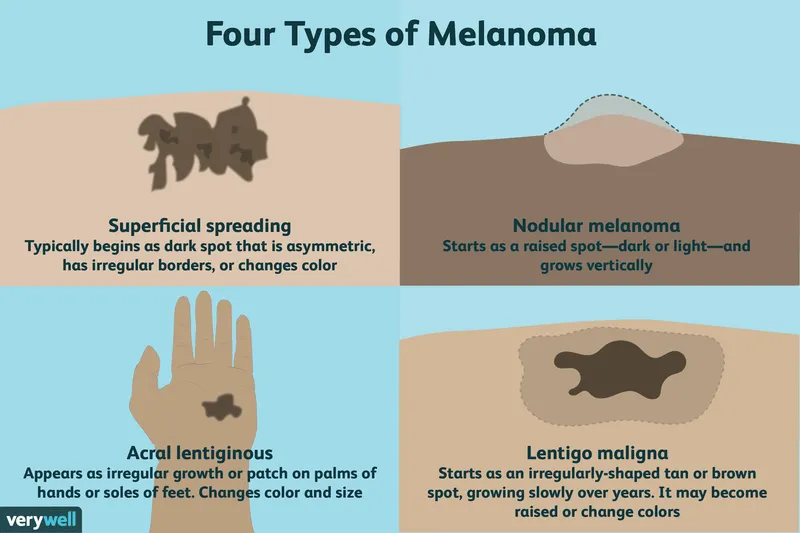
- This is the **most common type of melanoma**, accounting for 70% of cases, and typically presents with a **radial growth phase** showing irregular borders and enlarging size.
- Histopathology revealing **nests of abnormal melanocytes at the dermo-epidermal junction** and **discohesive cell growth into the epidermis** (pagetoid spread) is characteristic of superficial spreading melanoma.
*Desmoplastic melanoma*
- Characterized by **fibrous stroma** and often **neural invasion**, with a less pigmented appearance, which is not described.
- Typically presents as a firm, often amelanotic nodule, and can be more aggressive.
*Lentigo maligna melanoma*
- Primarily found in **chronically sun-damaged areas** of the elderly, often on the face, and begins as a flat, tan-brown macule that slowly enlarges.
- Histologically, it shows **atypical melanocytes along the basal layer** of a thinned epidermis, not necessarily forming nests or extensive discohesive growth into the epidermis early on.
*Nodular melanoma*
- This type of melanoma has a **vertical growth phase from the outset**, appearing as a rapidly growing, dark, elevated lesion without a significant preceding radial growth phase.
- Histologically, it involves a substantial dermal component with **minimal or absent intraepidermal radial growth**.
*Acral lentiginous melanoma*
- Occurs on the **palms, soles, or under the nails (subungual)**, and is less associated with sun exposure, often presenting as a dark, spreading lesion.
- Its histological features involve **lentiginous proliferation of atypical melanocytes** along the dermo-epidermal junction with spread into the rete ridges in an acral distribution.
Melanoma pathology US Medical PG Question 4: A 4-month-old boy is brought to the pediatrician for a wellness visit. Upon examination, the physician notes severe burns on the sun-exposed areas of the skin, including the face (especially the ears and nose), dorsal aspect of the hands, shoulders, and dorsal aspect of his feet. The child has very fair skin and blond hair. The parents insist that the child has not spent any extraordinary amount of time in the sun, but they admit that they rarely apply sunscreen. Which of the following physical factors is the most likely etiology for the burns?
- A. UV-B radiation (Correct Answer)
- B. Child abuse
- C. Gamma radiation
- D. Infrared radiation
- E. Ionizing radiation
Melanoma pathology Explanation: ***UV-B radiation***
- **UV-B radiation** is the primary cause of sunburn, especially in individuals with **fair skin** who lack sufficient melanin protection and do not use sunscreen.
- The distribution of burns on **sun-exposed areas** (face, ears, nose, hands, shoulders, feet) is highly consistent with typical sunburn patterns from direct sunlight exposure.
*Child abuse*
- While burns can be a sign of child abuse, the described pattern of burns on **regularly sun-exposed areas** in an infant with fair skin and reported lack of sunscreen use is more indicative of accidental sun exposure.
- Abusive burns often present with **distinct patterns**, such as immersion burns, contact burns with clear borders, or burns in protected areas, which are not described here.
*Gamma radiation*
- **Gamma radiation** exposure is typically associated with very severe, deep tissue damage, systemic illness, and often occurs due to accidents involving radioactive materials or during specific medical treatments.
- The presented scenario describes **skin burns** consistent with everyday environmental exposure, not high-energy gamma radiation.
*Infrared radiation*
- **Infrared radiation** primarily causes heat and thermal burns, often from direct contact with hot objects or intense heat sources.
- While heat can cause burns, this is distinct from the **sunburn** caused by ultraviolet light, which is more specifically linked to the sun's inflammatory effects on the skin.
*Ionizing radiation*
- **Ionizing radiation** (which includes gamma rays, X-rays, and alpha/beta particles) causes cell damage through ionization and can result in radiation burns, but these typically occur in highly controlled environments or after significant exposure to radioactive sources.
- Sunburn is specifically caused by the **non-ionizing UV spectrum** of radiation.
Melanoma pathology US Medical PG Question 5: A 52-year-old woman sees you in your office with a complaint of new-onset headaches over the past few weeks. On exam, you find a 2 x 2 cm dark, irregularly shaped, pigmented lesion on her back. She is concerned because her father recently passed away from skin cancer. What tissue type most directly gives rise to the lesion this patient is experiencing?
- A. Neural crest cells (Correct Answer)
- B. Endoderm
- C. Mesoderm
- D. Ectoderm
- E. Neuroectoderm
Melanoma pathology Explanation: ***Neural crest cells***
- The suspected lesion, given its description and the patient's family history of skin cancer, is likely a **melanoma**.
- Melanoma originates from **melanocytes**, which are derived from **neural crest cells** during embryonic development.
*Endoderm*
- The endoderm gives rise to the **lining of the gastrointestinal and respiratory tracts**, as well as organs such as the liver and pancreas.
- It is not involved in the formation of melanocytes or skin lesions like melanoma.
*Mesoderm*
- The mesoderm forms tissues such as **muscle, bone, cartilage, connective tissue**, and the circulatory system.
- It does not directly give rise to melanocytes, which are the cells of origin for melanoma.
*Ectoderm*
- The ectoderm gives rise to the **epidermis, nervous system**, and sensory organs.
- While melanocytes are found in the epidermis, they are specifically derived from the **neural crest (a sub-population of ectoderm)**, not the general ectoderm.
*Neuroectoderm*
- Neuroectoderm specifically refers to the ectoderm that develops into the **nervous system**.
- While neural crest cells originate from the neuroectoderm, "neural crest cells" is a more precise answer for the origin of melanocytes.
Melanoma pathology US Medical PG Question 6: A 63-year-old man comes to the physician for the evaluation of a skin lesion on his chest. He first noticed the lesion 2 months ago and thinks that it has increased in size since then. The lesion is not painful or pruritic. He has type 2 diabetes mellitus, hypercholesterolemia, and glaucoma. The patient has smoked 1 pack of cigarettes daily for the last 40 years and drinks two to three beers on the weekend. Current medications include metformin, atorvastatin, topical timolol, and a multivitamin. Vital signs are within normal limits. The lesion is partly elevated on palpation and does not change its form on pinching. A photograph of the lesion is shown. Which of the following is the most likely diagnosis?
- A. Seborrheic keratosis
- B. Malignant melanoma (Correct Answer)
- C. Keratoacanthoma
- D. Basal cell carcinoma
- E. Lentigo maligna
Melanoma pathology Explanation: ***Malignant melanoma***
- The lesion's **recent growth** and **elevated, irregular appearance** (as suggested by "partly elevated on palpation and does not change its form on pinching," implying a solid, infiltrative nature) in a patient with a history of **significant sun exposure** (implied by age and lesion location) are highly suspicious for melanoma.
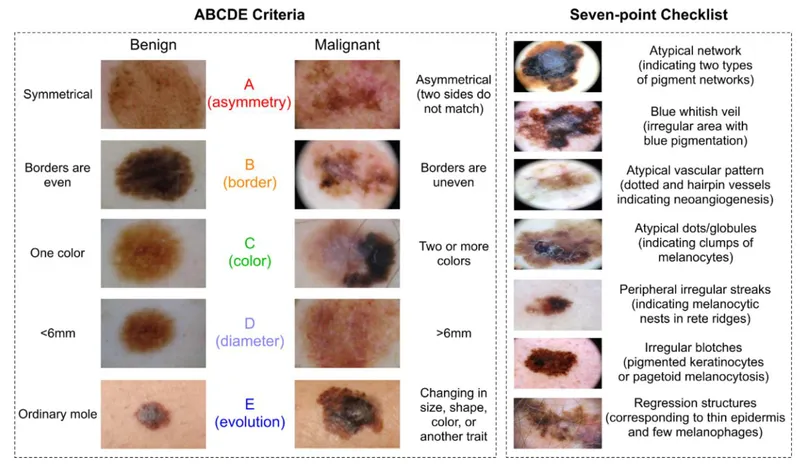
- While visual representation is key, this description aligns with a potentially advanced melanoma, characterized by **asymmetry, irregular borders, varied color, and a diameter greater than 6mm (ABCD rule)**, especially given the reported growth.
*Seborrheic keratosis*
- Typically presents as a **"stuck-on"** appearance, often described as velvety or warty, and is usually **benign** and grows slowly, if at all.
- The elevated, firm nature of the described lesion that does not change on pinching is less consistent with the soft, waxy texture often found in seborrheic keratosis.
*Keratoacanthoma*
- Characterized by rapid growth over weeks to months, often forming a **dome-shaped nodule with a central keratotic plug**.
- While it can grow quickly, the detailed description and the potential for a more variegated appearance (melanoma) are not fully captured by this option, and it often has spontaneous regression, which is not suggested here.
*Basal cell carcinoma*
- Most commonly presents as a **pearly nodule with telangiectasias**, or a **rolled border** with central ulceration.
- While it can be elevated and solid, the description of rapid growth and the implication of an irregular clinical appearance (without direct visualization) make melanoma a stronger consideration.
*Lentigo maligna*
- This is a form of melanoma in situ that typically appears as a **slowly enlarging, flat, irregularly shaped, and variegated brown-to-black patch** on chronically sun-damaged skin.
- Although the patient's age and lesion location fit, the description of "partly elevated on palpation" suggests a more invasive lesion, making **malignant melanoma** (which encompasses invasive forms) a more appropriate diagnosis.
Melanoma pathology US Medical PG Question 7: A 43-year-old woman presents to your clinic for the evaluation of an abnormal skin lesion on her forearm. The patient is worried because her mother passed away from melanoma. You believe that the lesion warrants biopsy for further evaluation for possible melanoma. Your patient is concerned about her risk for malignant disease. What is the most important prognostic factor of melanoma?
- A. Depth of invasion of atypical cells (Correct Answer)
- B. S-100 tumor marker present
- C. Evolution of lesion over time
- D. Age at presentation
- E. Level of irregularity of the borders
Melanoma pathology Explanation: ***Depth of invasion of atypical cells***
- The **Breslow depth**, which measures the vertical thickness of the melanoma from the granular layer of the epidermis to the deepest part of the tumor, is the **single most important prognostic factor** for localized melanoma.
- A greater depth of invasion correlates directly with a higher risk of **metastasis** and a poorer prognosis due to increased likelihood of reaching dermal lymphatics or blood vessels.
*S-100 tumor marker present*
- While **S-100 protein** is a marker expressed in melanoma cells and can be used to detect metastatic disease (e.g., in lymph nodes), its mere presence does not serve as the primary prognostic indicator for the primary lesion itself.
- S-100 reflects the presence of melanoma cells but does not provide information about the **depth or biological aggressiveness** of the initial tumor.
*Evolution of lesion over time*
- The **evolution or change** in a lesion (e.g., in size, shape, color, new symptoms) is a crucial diagnostic criterion for identifying suspicious lesions for biopsy.
- While important for diagnosis, it is not a direct prognostic factor once melanoma is confirmed; the **pathological features** after biopsy, particularly depth, determine prognosis.
*Age at presentation*
- **Age** can influence treatment decisions and overall health status, but it is not the most important independent prognostic factor for melanoma.
- Prognosis is primarily driven by tumor-specific characteristics rather than the patient's age.
*Level of irregularity of the borders*
- **Border irregularity** is one of the ABCDE criteria (Asymmetry, Border irregularity, Color variation, Diameter >6mm, Evolving) used to identify suspicious pigmented lesions.
- It is a diagnostic indicator that warrants further investigation but does not independently determine **prognosis** as definitively as the Breslow depth after biopsy.
Melanoma pathology US Medical PG Question 8: A 65-year-old man comes to the physician because he is worried about a mole on his right forearm. He has had the mole for several years, but it has grown in size in the past 3 months. Physical examination shows a hyperpigmented plaque with irregular borders and small area of ulceration. Histopathologic analysis of a full-thickness excisional biopsy confirms the diagnosis of malignant melanoma. Invasion of which of the following layers of skin carries the highest risk of mortality for this patient?
- A. Reticular dermis
- B. Papillary dermis
- C. Stratum basale
- D. Stratum corneum
- E. Hypodermis (Correct Answer)
Melanoma pathology Explanation: ***Hypodermis***
- Invasion into the **hypodermis (subcutaneous tissue)** indicates the deepest penetration of the melanoma, correlated with the **greatest tumor thickness** (Breslow depth).
- Deeper invasion significantly increases the likelihood of **lymphatic and hematogenous spread**, leading to the highest risk of **metastasis** and mortality.
- This represents the **worst prognosis** among the layers listed.
*Stratum corneum*
- The **stratum corneum** is the outermost, dead keratinized layer of the epidermis.
- Melanoma cells limited to this layer would indicate **melanoma in situ** or a very superficial lesion.
- This represents the most superficial involvement, carrying the **lowest risk of mortality** and metastasis.
*Stratum basale*
- The **stratum basale** is the deepest layer of the epidermis at the dermal-epidermal junction.
- Melanoma confined to or near this level represents early invasion just beyond the basement membrane.
- This level of invasion is still relatively superficial and is associated with a **better prognosis** than deeper dermal or subcutaneous invasion.
*Papillary dermis*
- Invasion into the **papillary dermis** signifies invasive melanoma but represents an early stage of dermal invasion.
- The risk of distant metastasis and mortality is present but lower compared to invasion into deeper dermal layers or the hypodermis.
*Reticular dermis*
- Invasion into the **reticular dermis** indicates deeper penetration and a more advanced tumor with greater Breslow depth.
- Metastatic risk is significantly increased compared to papillary dermis invasion but is still lower than invasion into the subcutaneous tissue (hypodermis).
Melanoma pathology US Medical PG Question 9: A 50-year-old woman with rheumatoid arthritis on methotrexate develops rapidly progressive painful ulcers on her legs with violaceous undermined borders. Biopsy shows neutrophilic dermal infiltrate with areas of necrosis, but no vasculitis or infection. Wound cultures are negative. Despite debridement, the ulcers worsen. C-ANCA and P-ANCA are negative. Evaluate the diagnosis and determine the management that addresses both the cutaneous condition and systemic disease.
- A. Discontinue all immunosuppression to allow wound healing
- B. Increase methotrexate dose and add wound care
- C. Discontinue methotrexate, start cyclosporine and prednisone
- D. Start broad-spectrum antibiotics and surgical debridement
- E. Continue methotrexate, add TNF-alpha inhibitor and systemic corticosteroids (Correct Answer)
Melanoma pathology Explanation: ***Continue methotrexate, add TNF-alpha inhibitor and systemic corticosteroids***
- This patient presents with **Pyoderma Gangrenosum (PG)**, a neutrophilic dermatosis characterized by **violaceous undermined borders** and **pathergy**, where surgical debridement cause lesion expansion.
- **TNF-alpha inhibitors** (e.g., adalimumab, infliximab) are first-line for recalcitrant PG and simultaneously provide excellent control for the underlying **Rheumatoid Arthritis**.
*Discontinue all immunosuppression to allow wound healing*
- Since PG is an **autoimmune inflammatory condition**, withdrawing immunosuppression would result in rapid progression of the ulcers rather than healing.
- Wound healing in PG requires **suppressing the inflammatory response** rather than the typical wound care approach for infected ulcers.
*Increase methotrexate dose and add wound care*
- While **methotrexate** treats RA, it is often insufficient as a monotherapy for the acute, rapidly progressive phase of **Pyoderma Gangrenosum**.
- Standard wound care alone is ineffective because the primary driver is **neutrophilic infilatration**, which requires targeted biologic or corticosteroid therapy.
*Discontinue methotrexate, start cyclosporine and prednisone*
- While **cyclosporine** and **prednisone** are used for PG, discontinuing methotrexate may lead to a flare of the patient’s **Rheumatoid Arthritis**.
- Maintaining a coordinated regimen that addresses both the skin and the joints, such as adding a **TNF-alpha inhibitor**, is preferred over switching all medications.
*Start broad-spectrum antibiotics and surgical debridement*
- **Surgical debridement** is contraindicated in PG due to **pathergy**, a phenomenon where trauma to the skin induces new or worsening lesions.
- **Antibiotics** are unnecessary as the biopsy and cultures confirmed a **sterile neutrophilic infiltrate** rather than an infectious process.
Melanoma pathology US Medical PG Question 10: A 25-year-old woman presents with painful oral ulcers and a pustular rash at venipuncture sites. She has genital ulcers and a history of recurrent uveitis. Skin biopsy from a pustule shows neutrophilic infiltrate in the dermis without vasculitis or infection. HLA-B51 testing is positive. She is planning pregnancy. Evaluate the management strategy considering disease control and pregnancy planning.
- A. Start methotrexate for disease control
- B. Start colchicine monotherapy and proceed with pregnancy
- C. Start high-dose corticosteroids and azathioprine, delay pregnancy
- D. Start infliximab, use contraception, then transition to low-risk therapy before conception (Correct Answer)
- E. Avoid all immunosuppression and manage symptoms only
Melanoma pathology Explanation: ***Start infliximab, use contraception, then transition to low-risk therapy before conception***
- This patient has **Beh'et's disease** with **recurrent uveitis**, which is **sight-threatening** and requires aggressive biological therapy like **infliximab** or **TNF-inhibitors** for rapid remission.
- Achievng **remission** before pregnancy is vital; while TNF-inhibitors are often continued, transitioning to pregnancy-compatible agents like **azathioprine** or **colchicine** ensures long-term safety.
*Start methotrexate for disease control*
- **Methotrexate** is strictly **teratogenic** and must be avoided in patients planning pregnancy or discontinued months before conception.
- While it can treat some aspects of systemic inflammation, it is not the first-line gold standard for **acute ocular Beh'et's** compared to biologics.
*Start colchicine monotherapy and proceed with pregnancy*
- **Colchicine** is excellent for **mucocutaneous** symptoms (oral and genital ulcers) but is insufficient as monotherapy to prevent blindness from **recurrent uveitis**.
- Relying on monotherapy in a patient with active ocular disease risks **permanent vision loss** during the pregnancy period.
*Start high-dose corticosteroids and azathioprine, delay pregnancy*
- While **azathioprine** is used for maintenance, **high-dose corticosteroids** carry significant side effects and are usually a bridge, not a comprehensive plan for ocular stabilization.
- This strategy lacks the rapid, potent **TNF-alpha inhibition** needed to quickly arrest the neutrophilic inflammation seen in severe Beh'et's flare-ups.
*Avoid all immunosuppression and manage symptoms only*
- **Beh'et's disease** is a multi-system inflammatory disorder; leaving **uveitis** and systemic vasculitis untreated leads to irreversible organ damage and **blindness**.
- Symptomatic management alone ignores the **neutrophilic infiltrate** and underlying autoimmune process, which could also lead to pregnancy complications due to active maternal disease.
More Melanoma pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.