Inflammatory dermatoses US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Inflammatory dermatoses. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Inflammatory dermatoses US Medical PG Question 1: A 72-year-old nursing home resident is complaining of pruritis. She is noted to have multiple, tense blisters on her trunk as well as the flexor surfaces of her extremities. The blisters have an erythematous base. You are unable to extend the blisters when you apply lateral traction. You suspect an autoimmune bullous dermatosis. Which of the following is the cause of the likely condition?
- A. Antibodies to epidermal transglutaminase
- B. Epidermal necrolysis
- C. Antibodies to hemidesmosomes (Correct Answer)
- D. Antibodies to desmoglein
- E. Antibodies to desmosomes
Inflammatory dermatoses Explanation: **Antibodies to hemidesmosomes**
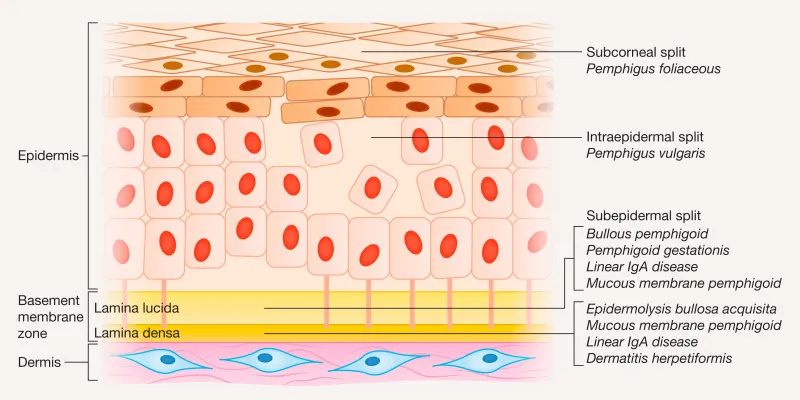
- The patient's presentation with **tense blisters** that do not extend with lateral traction (negative Nikolsky sign) is classic for **bullous pemphigoid**.
- **Bullous pemphigoid** is an autoimmune disease caused by antibodies targeting components of the **hemidesmosomes** (specifically BP180 and BP230) at the dermal-epidermal junction.
*Antibodies to epidermal transglutaminase*
- Antibodies against **epidermal transglutaminase** are characteristic of **dermatitis herpetiformis**, which presents with intensely pruritic, grouped vesicles and papules, often on extensor surfaces.
- This condition is also associated with **celiac disease**, and its classic lesions are small and vesicular, not the large, tense bullae described.
*Epidermal necrolysis*
- **Epidermal necrolysis**, including Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN), is characterized by widespread epidermal detachment and necrosis, often triggered by medications.
- It presents with diffuse painful erythema and sheet-like skin loss, which is distinctly different from the described tense blisters of bullous pemphigoid.
*Antibodies to desmoglein*
- Antibodies to **desmoglein 1 and/or 3** (components of desmosomes) are the hallmark of **pemphigus vulgaris** and **pemphigus foliaceus**.
- These conditions cause **flaccid blisters** that are easily ruptured and often exhibit a positive Nikolsky sign, contrary to the tense blisters in this case.
*Antibodies to desmosomes*
- Antibodies to **desmosomes** (specifically desmogleins) lead to **pemphigus**, which is characterized by intraepidermal blistering and a positive Nikolsky sign.
- The described **tense blisters** and negative Nikolsky sign rule out pemphigus, where the defect is in keratinocyte adhesion within the epidermis.
Inflammatory dermatoses US Medical PG Question 2: A 23-year-old woman comes to the physician because of a 5-month history of a pruritic rash on the bilateral upper extremities. She has no history of serious illness and takes no medications. A skin biopsy of the rash shows intraepidermal accumulation of edematous fluid and widening of intercellular spaces between keratinocytes. Which of the following is the most likely diagnosis?
- A. Dermatitis herpetiformis
- B. Eczematous dermatitis (Correct Answer)
- C. Acanthosis nigricans
- D. Lichen planus
- E. Psoriasis vulgaris
Inflammatory dermatoses Explanation: ***Eczematous dermatitis***
- The biopsy findings of **intraepidermal edema** and **widening of intercellular spaces between keratinocytes (spongiosis)** are classic histopathologic features of eczematous dermatitis.
- The clinical presentation of a **pruritic rash** on the upper extremities further supports this diagnosis, as eczema is characterized by itching and inflammation.
*Dermatitis herpetiformis*
- This condition is characterized by **subepidermal vesicles** and **neutrophilic infiltrates** in the dermal papillae, with IgA deposition, which differs from the findings described.
- It is strongly associated with **celiac disease** and presents with intensely pruritic, grouped papules and vesicles, predominantly on extensor surfaces.
*Acanthosis nigricans*
- Histologically, acanthosis nigricans shows **papillomatosis** and **hyperkeratosis**, with epidermal thickening, rather than intraepidermal edema or spongiosis.
- Clinically, it presents as **hyperpigmented, velvety plaques** in intertriginous areas, not a generalized pruritic rash.
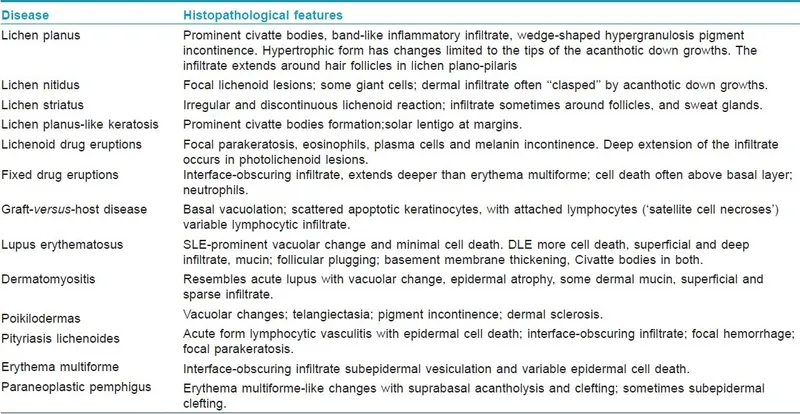
*Lichen planus*
- Biopsy of lichen planus would reveal a **band-like lymphocytic infiltrate** at the dermoepidermal junction, **sawtooth rete ridges**, and **Civatte bodies**.
- Clinically, it often presents with **pruritic, polygonal, purple, planar papules and plaques** (the 6 Ps), which is not consistent with the described rash.
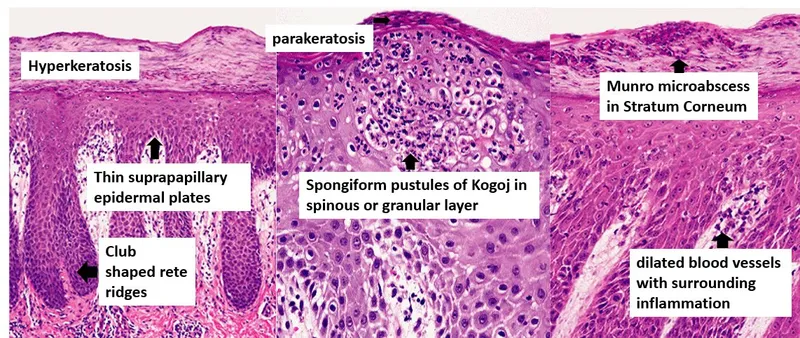
*Psoriasis vulgaris*
- Histopathologically, psoriasis is characterized by **acanthosis**, **parakeratosis**, **Munro microabscesses**, and **dilated blood vessels** in the dermal papillae.
- Clinically, it manifests as **erythematous plaques with silvery scales**, typically on extensor surfaces, distinguishing it from a generalized pruritic rash with spongiosis.
Inflammatory dermatoses US Medical PG Question 3: A 29-year-old woman presents with skin lesions on her elbows and forearms. She notes that they first started appearing 2 months ago and have not improved. She describes the lesions as painless and rarely itchy. She denies any similar symptoms in the past, and has no other significant past medical history. Review of systems is significant for recent joint pain, conjunctivitis, and corneal dryness. The patient is afebrile and vital signs are within normal limits. Non-tender, raised, inflamed, white-silver maculopapular lesions are present. Which of the following are the most likely histopathologic findings in this patient's skin biopsy?
- A. Intercellular edema with detachment at basal level
- B. Acanthosis, hyperkeratosis with parakeratosis, and dermal papillary capillary proliferation (Correct Answer)
- C. Cytoplasmic vacuolation
- D. Nuclear atypia, cellular pleomorphism, and a disorganized structure of cells from basal to apical layers of the tissue
- E. Subepidermal blister with detachment at dermal-epidermal junction
Inflammatory dermatoses Explanation: ***Acanthosis, hyperkeratosis with parakeratosis, and dermal papillary capillary proliferation***
- The patient's presentation with **raised, inflamed, white-silver maculopapular lesions** on elbows and forearms, along with joint pain and conjunctivitis, is highly suggestive of **psoriasis**.
- **Acanthosis** (epidermal hyperplasia), **hyperkeratosis with parakeratosis** (retained nuclei in the stratum corneum), and **dermal papillary capillary proliferation** (elongated dermal papillae with dilated blood vessels) are classic histopathological findings in psoriasis.
*Intercellular edema with detachment at basal level*
- This description is more consistent with conditions causing **spongiosis** (intercellular edema in the epidermis) or **dermatitis**, which typically present with different clinical features (e.g., vesicles, oozing).
- Basal layer detachment can be seen in **bullous pemphigoid** or other blistering disorders, which are characterized by large tense blisters, unlike the described lesions.
*Cytoplasmic vacuolation*
- **Cytoplasmic vacuolation** is a non-specific finding that can be observed in various conditions, including **viral infections** (e.g., HPV), certain **drug reactions**, or **degenerative changes**.
- It does not specifically describe the characteristic changes seen in psoriasis.
*Subepidermal blister with detachment at dermal-epidermal junction*
- A **subepidermal blister** (detachment of the epidermis from the dermis at the dermal-epidermal junction) is characteristic of conditions like **bullous pemphigoid**.
- The patient's lesions are described as maculopapular, not blistering, making this diagnosis unlikely.
*Nuclear atypia, cellular pleomorphism, and a disorganized structure of cells from basal to apical layers of the tissue*
- These findings (**nuclear atypia**, **cellular pleomorphism**, **disorganized cell structure**) are hallmarks of **dysplasia** or **carcinoma in situ**.
- The patient's symptoms are recent onset, widespread, and associated with joint pain, which are not typical of a malignant skin lesion.
Inflammatory dermatoses US Medical PG Question 4: A 24-year-old man comes to the physician for the evaluation of a severely pruritic skin rash. Physical examination shows a symmetrical rash over the knees and elbows with tense, grouped vesicles, and several excoriation marks. Microabscesses in the papillary dermis are seen on light microscopy. Immunofluorescence shows deposits of immunoglobulin A at the tips of dermal papillae. This patient's skin findings are most likely associated with which of the following?
- A. Mite eggs and fecal pellets
- B. Positive Nikolsky sign
- C. Gliadin-dependent hypersensitivity (Correct Answer)
- D. Multinucleated giant cells
- E. Nail pitting
Inflammatory dermatoses Explanation: ***Gliadin-dependent hypersensitivity***
- The description of a severely **pruritic rash** with **grouped vesicles** on extensor surfaces (knees and elbows), along with **IgA deposits** at the tips of dermal papillae and **microabscesses**, is classic for **dermatitis herpetiformis**.
- Dermatitis herpetiformis is strongly associated with **celiac disease**, which is caused by a **hypersensitivity reaction to gliadin**, a protein found in gluten.
*Mite eggs and fecal pellets*
- This finding is characteristic of **scabies**, which presents with burrows, intense pruritus, and a rash that primarily affects the web spaces of fingers, wrists, and other areas where mites burrow.
- The clinical presentation and microscopic findings (IgA deposits, microabscesses) do not align with scabies.
*Positive Nikolsky sign*
- A positive Nikolsky sign (skin sloughing with gentle lateral pressure) is typically seen in **pemphigus vulgaris** or **toxic epidermal necrolysis (TEN)**.
- These conditions involve blistering but have distinct histological features and different immune pathologies (e.g., IgG antibodies against desmoglein in pemphigus vulgaris).
*Multinucleated giant cells*
- The presence of **multinucleated giant cells** is a histological hallmark of **viral infections**, such as **herpes simplex virus (HSV)** or **varicella-zoster virus (VZV)**.
- While these can cause vesicular rashes, the characteristic IgA deposition and microabscesses are not typical of viral infections.
*Nail pitting*
- **Nail pitting** is a common finding in **psoriasis** and **psoriatic arthritis**.
- Psoriasis typically presents with erythematous plaques with silvery scales, which is different from the vesicular rash seen in this patient.
Inflammatory dermatoses US Medical PG Question 5: A 47-year-old man presents to his primary care physician complaining of pain and stiffness in his right index finger and left knee. The past medical history is remarkable for severe dandruff and an episode of apparent gout in the left 1st toe 6 months ago, which never resolved. The physical examination confirms dactylitis of the right index finger and several toes, as well as synovitis of the left knee. He is also noted to have pitting of his fingernails. Plain X-rays of his hand reveal erosions in the distal interphalangeal (DIP) joint and periarticular new bone formation. Which of the following is most consistent with these findings?
- A. Psoriatic arthritis (Correct Answer)
- B. Pseudogout
- C. Osteoarthritis
- D. Reactive arthritis
- E. Rheumatoid arthritis
Inflammatory dermatoses Explanation: ***Psoriatic arthritis***
- The constellation of **dactylitis**, **nail pitting**, involvement of both **DIP joints** with erosions, and a history of **psoriasis** (severe dandruff) is highly characteristic of psoriatic arthritis.
- The previous episode resembling gout and synovitis of the knee are also consistent, as psoriatic arthritis can mimic other arthropathies and affect various joints.
*Pseudogout*
- This condition is caused by **calcium pyrophosphate dihydrate crystal deposition** and typically presents as acute, severe joint pain, often in larger joints like the knee or wrist, but without dermatological or nail changes.
- While it can cause synovitis, it does not typically involve dactylitis, DIP erosions, nail pitting, or a history of psoriasis.
*Osteoarthritis*
- Characterized by **cartilage degeneration** and **new bone formation** (osteophytes), often in weight-bearing joints or DIP/PIP joints, but typically without the marked inflammatory signs like dactylitis or nail changes.
- While X-rays can show new bone formation, the presence of dactylitis, nail pitting, and psoriasis history rule out uncomplicated osteoarthritis.
*Reactive arthritis*
- This is an **acute, inflammatory arthropathy** that typically develops after a genitourinary or gastrointestinal infection.
- While it can present with dactylitis and oligoarthritis, it does not involve nail pitting or a history of psoriasis, and the initial trigger infection is usually identifiable.
*Rheumatoid arthritis*
- This is a **chronic autoimmune disease** primarily affecting smaller joints symmetrically, particularly the MCP and PIP joints, but typically sparing the DIP joints.
- It is not associated with psoriasis, nail pitting, and usually presents with periarticular osteopenia rather than significant new bone formation on X-ray.
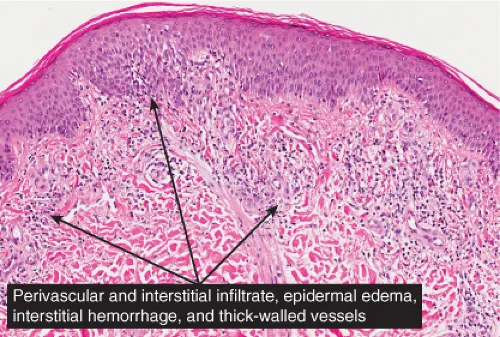
Inflammatory dermatoses US Medical PG Question 6: A 40-year-old man presents with a rash, oral lesions, and vision problems for 5 days. He says the rash started as a burning feeling on his face and the upper part of his torso, but soon red spots appeared in that same distribution. The spots grew in size and spread to his upper extremities. The patient says the spots are painful but denies any associated pruritus. He says the painful oral lesions appeared about the same time as the rash. For the past 3 days, he also says he has been having double vision and dry, itchy eyes. He reports that he had a mild upper respiratory infection for a few days that preceded his current symptoms. The patient denies any chills, hematuria, abdominal or chest pain, or similar symptoms in the past. Past medical history is significant for a severe urinary tract infection diagnosed 3 weeks ago for which he has been taking trimethoprim-sulfamethoxazole. The vital signs include: temperature 38.3℃ (101.0℉), blood pressure 110/60 mm Hg, respiratory rate 20/min, and pulse 108/min. On physical examination, the patient has severe painful erosions of the oral mucosa. There are multiple fluid-filled vesicles and bullae averaging 3 mm in diameter with a surrounding erythematous ring that involve only the upper torso and extensor surfaces of upper extremities. Several of the lesions have ruptured, resulting in sloughing off of the epidermal layer. There is a prominent conjunctival injection present. Ophthalmic examination reveals mild bilateral corneal abrasions without any evidence of frank ulceration. Laboratory findings are significant for the following:
White blood cell (WBC) count 8,500/mm3
Red blood cell (RBC) count 4.20 x 106/mm3
Hematocrit 41.5%
Hemoglobin 14.0 g/dL
Platelet count 215,000/mm3
C-reactive protein (CRP) 86 mg/L
Urine and blood cultures are pending. Which of the following would confirm the most likely diagnosis in this patient?
- A. Gram stain and culture of skin sample
- B. Urine collection (24-hour)
- C. Biopsy and histopathologic analysis of skin lesions (Correct Answer)
- D. Direct immunofluorescence analysis of perilesional skin biopsy
- E. Flow cytometry
Inflammatory dermatoses Explanation: ***Biopsy and histopathologic analysis of skin lesions***
- This patient's presentation of **vesiculobullous rash**, **oral erosions**, and **conjunctivitis** following recent trimethoprim-sulfamethoxazole use is highly suggestive of **Stevens-Johnson Syndrome (SJS)** or **Toxic Epidermal Necrolysis (TEN)**.
- **Skin biopsy with histopathologic analysis** is the **gold standard** for **confirming** SJS/TEN, showing characteristic findings of **full-thickness epidermal necrosis**, **keratinocyte apoptosis**, and **subepidermal blistering** with minimal dermal inflammation.
- These histologic features definitively establish the diagnosis and differentiate SJS/TEN from other vesiculobullous disorders.
*Direct immunofluorescence analysis of perilesional skin biopsy*
- While **direct immunofluorescence (DIF)** can be helpful in the workup, it typically shows **negative or sparse staining** in SJS/TEN, as this is not an autoimmune bullous disease.
- DIF is primarily used to **rule out** conditions like **pemphigus vulgaris** (which shows intercellular IgG/C3) or **bullous pemphigoid** (which shows linear basement membrane IgG/C3).
- A negative DIF supports but does not **confirm** SJS/TEN; it merely excludes autoimmune causes.
*Gram stain and culture of skin sample*
- While secondary bacterial infection can complicate SJS/TEN, a **Gram stain and culture** would only identify superimposed infection, not the underlying etiology.
- The clinical picture points to a severe **drug-induced hypersensitivity reaction**, not a primary bacterial skin infection.
*Flow cytometry*
- **Flow cytometry** analyzes **cell surface markers** and is used for hematologic malignancies, immunodeficiencies, and cell population analysis.
- It has no role in diagnosing **vesiculobullous skin disorders** or drug hypersensitivity reactions.
*Urine collection (24-hour)*
- A **24-hour urine collection** measures urinary excretion of various substances and is used for metabolic or renal assessments.
- It has no diagnostic value for **mucocutaneous drug reactions** like SJS/TEN.
Inflammatory dermatoses US Medical PG Question 7: A 50-year-old female presents to her physician with vesicles and tense blisters across her chest, arms, and the back of her shoulders. Physical examination reveals that blistering is not present in her oral mucosa, and the epidermis does not separate upon light stroking of the skin. The patient most likely suffers from a hypersensitivity reaction located:
- A. Linearly along the epidermal basement membrane (Correct Answer)
- B. In fat cells beneath the skin
- C. In nuclei within epidermal cells
- D. In net-like patterns around epidermal cells
- E. In granular deposits at the tips of dermal papillae
Inflammatory dermatoses Explanation: ***Linearly along the epidermal basement membrane***
- The description of **tense blisters** and the absence of **Nikolsky's sign** (no epidermal separation with light stroking) are characteristic features of **bullous pemphigoid**.
- **Bullous pemphigoid** is an autoimmune disease where autoantibodies target components of the **hemidesmosomes** located along the **epidermal basement membrane**, leading to subepidermal blistering.
*In fat cells beneath the skin*
- This description is not consistent with any common blistering disorder, and **fat cells** (adipocytes) are not primary targets for blistering in autoimmune diseases.
- Blistering disorders typically involve the epidermis or the dermal-epidermal junction, not the subcutaneous fat.
*In nuclei within epidermal cells*
- Autoantibodies targeting **nuclear antigens** are associated with conditions like **lupus erythematosus**, but this generally leads to characteristic skin rashes, not tense blistering.
- Blistering from nuclear involvement is uncommon and does not match the clinical presentation of bullous pemphigoid or pemphigus.
*In net-like patterns around epidermal cells*
- This pattern of antibody deposition is characteristic of **pemphigus vulgaris**, where autoantibodies target **desmogleins** in the intercellular spaces of the epidermis.
- Pemphigus vulgaris typically presents with **flaccid blisters** that are easily rupturable, and often involves the **oral mucosa**, in contrast to the patient's presentation.
*In granular deposits at the tips of dermal papillae*
- This pattern of IgA deposition, particularly in a granular fashion at the **dermal papillae tips**, is characteristic of **dermatitis herpetiformis**.
- Dermatitis herpetiformis typically presents with **pruritic papules and vesicles**, often on extensor surfaces, and is commonly associated with **celiac disease**, which is not indicated here.
Inflammatory dermatoses US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Inflammatory dermatoses Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Inflammatory dermatoses US Medical PG Question 9: A 53-year-old woman seeks medical care for superficial erosions and blisters over the skin of her head and trunk. She also has significant involvement of her buccal mucosa, which has made eating difficult. A year earlier, she developed tender sores on the oral mucosa and soft palate of her mouth, which was initially treated as herpes simplex stomatitis. Her condition worsened despite treatment, resulting in the development of eroded areas over her trunk and extremities, with a 10 kg weight loss. Upon further questioning, she denies itching, but she notes that the top layer of her skin could be easily removed when firm horizontal pressure was applied. What is the most likely diagnosis for this patient’s condition?
- A. Dermatitis herpetiformis
- B. Toxic epidermal necrolysis
- C. Pemphigus vulgaris (Correct Answer)
- D. Bullous pemphigoid
- E. Behcet’s disease
Inflammatory dermatoses Explanation: ***Pemphigus vulgaris***
- This condition is characterized by **superficial erosions and blisters**, significant **mucosal involvement** (especially oral), and a **positive Nikolsky sign** (skin easily removed with pressure), all classic features of pemphigus vulgaris.
- The initial presentation often includes painful **oral lesions** that precede cutaneous involvement and can lead to **weight loss** due to difficult eating.
*Dermatitis herpetiformis*
- Typically presents with intensely **pruritic (itchy) urticarial papules and vesicles**, primarily on extensor surfaces, which is contrary to the patient's denial of itching.
- Strongly associated with **celiac disease** and presents with distinct IgA deposits on direct immunofluorescence, unlike the IgG deposits seen in pemphigus vulgaris.
*Toxic epidermal necrolysis*
- Characterized by widespread **epidermal detachment**, often triggered by drugs, with fever and severe systemic symptoms, which are not detailed here.
- The onset is usually acute and rapid, leading to extensive "sheet-like" skin loss, rather than the more gradual progression described.
*Bullous pemphigoid*
- Presents with **tense bullae** on an erythematous or urticarial base, and while oral involvement can occur, it is less common and less severe than in pemphigus vulgaris.
- The **Nikolsky sign is typically negative** in bullous pemphigoid, and the blisters are subepidermal, remaining intact longer.
*Behcet’s disease*
- Characterized by **recurrent oral and genital aphthous ulcers**, along with ocular and skin lesions, but typically does not present with widespread blistering and positive Nikolsky sign.
- It is a multisystem inflammatory disorder, and the skin lesions are usually **erythema nodosum-like** or papulopustular, not extensive superficial erosions and blisters.
Inflammatory dermatoses US Medical PG Question 10: A 54-year-old man comes to the physician because of a cough with blood-tinged sputum for 1 week. He also reports fever and a 5-kg (11 lb) weight loss during the past 2 months. Over the past year, he has had 4 episodes of sinusitis. Physical examination shows palpable nonblanching skin lesions over the hands and feet. Examination of the nasal cavity shows ulceration of the nasopharyngeal mucosa and a depressed nasal bridge. Oral examination shows a painful erythematous gingival enlargement that bleeds easily on contact. Which of the following is the most likely cause of the patient's symptoms?
- A. Metalloprotease enzyme deficiency
- B. Malignant myeloid cell proliferation
- C. Arteriovenous malformation
- D. Immune complex deposition
- E. Neutrophil-mediated damage (Correct Answer)
Inflammatory dermatoses Explanation: ***Neutrophil-mediated damage***
- The constellation of **sinusitis**, **pulmonary symptoms** (cough with blood-tinged sputum), **renal involvement** (indicated by systemic symptoms and often associated with microhematuria in this condition), and **skin lesions (palpable purpura)**, along with **nasal ulceration**, a **depressed nasal bridge**, and **gingival enlargement**, is highly characteristic of **Granulomatosis with Polyangiitis (GPA)**.
- GPA is an **ANCA-associated vasculitis** characterized by **necrotizing granulomatous inflammation** and **vasculitis** of small to medium-sized vessels, primarily driven by **neutrophil activation** and subsequent tissue damage.
*Metalloprotease enzyme deficiency*
- This description commonly refers to conditions like **alpha-1 antitrypsin deficiency**, which primarily causes **emphysema** and liver disease, not the widespread vasculitic manifestations seen here.
- It does not explain the diverse multi-organ involvement including skin, ENT, and likely renal symptoms.
*Malignant myeloid cell proliferation*
- This would suggest conditions like **leukemia** or **myelodysplastic syndromes**, which present with altered blood counts, fatigue, infections, and bleeding, but typically not this specific pattern of vasculitis and granulomatous inflammation.
- While constitutional symptoms like weight loss can occur, the localized findings like depressed nasal bridge and gingival enlargement are not characteristic.
*Arteriovenous malformation*
- An **arteriovenous malformation (AVM)** is an abnormal connection between arteries and veins; depending on its location, it can cause bleeding (e.g., hemoptysis if pulmonary) or neurological symptoms if cerebral.
- However, AVMs do not explain the systemic inflammatory symptoms, skin lesions, sinusitis, depressed nasal bridge, or gingival changes.
*Immune complex deposition*
- **Immune complex vasculitis** (e.g., IgA vasculitis, cryoglobulinemic vasculitis) often presents with palpable purpura and can affect kidneys and GI tract.
- However, the prominent **granulomatous inflammation** causing **nasal ulceration** and **depressed nasal bridge**, and the specific type of **pulmonary-renal syndrome** seen in GPA, are more indicative of **ANCA-mediated neutrophil damage** rather than immune complex deposition.
More Inflammatory dermatoses US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.