Disorders of pigmentation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Disorders of pigmentation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Disorders of pigmentation US Medical PG Question 1: A 52-year-old Caucasian man presents to the clinic for evaluation of a mole on his back that he finds concerning. He states that his wife noticed the lesion and believes that it has been getting larger. On inspection, the lesion is 10 mm in diameter with irregular borders. A biopsy is performed. Pathology reveals abnormal melanocytes forming nests at the dermo-epidermal junction and discohesive cell growth into the epidermis. What is the most likely diagnosis?
- A. Desmoplastic melanoma
- B. Lentigo maligna melanoma
- C. Superficial spreading melanoma (Correct Answer)
- D. Nodular melanoma
- E. Acral lentiginous melanoma
Disorders of pigmentation Explanation: ***Superficial spreading melanoma***
- This is the **most common type of melanoma**, accounting for 70% of cases, and typically presents with a **radial growth phase** showing irregular borders and enlarging size.
- Histopathology revealing **nests of abnormal melanocytes at the dermo-epidermal junction** and **discohesive cell growth into the epidermis** (pagetoid spread) is characteristic of superficial spreading melanoma.
*Desmoplastic melanoma*
- Characterized by **fibrous stroma** and often **neural invasion**, with a less pigmented appearance, which is not described.
- Typically presents as a firm, often amelanotic nodule, and can be more aggressive.
*Lentigo maligna melanoma*
- Primarily found in **chronically sun-damaged areas** of the elderly, often on the face, and begins as a flat, tan-brown macule that slowly enlarges.
- Histologically, it shows **atypical melanocytes along the basal layer** of a thinned epidermis, not necessarily forming nests or extensive discohesive growth into the epidermis early on.
*Nodular melanoma*
- This type of melanoma has a **vertical growth phase from the outset**, appearing as a rapidly growing, dark, elevated lesion without a significant preceding radial growth phase.
- Histologically, it involves a substantial dermal component with **minimal or absent intraepidermal radial growth**.
*Acral lentiginous melanoma*
- Occurs on the **palms, soles, or under the nails (subungual)**, and is less associated with sun exposure, often presenting as a dark, spreading lesion.
- Its histological features involve **lentiginous proliferation of atypical melanocytes** along the dermo-epidermal junction with spread into the rete ridges in an acral distribution.
Disorders of pigmentation US Medical PG Question 2: A 19-year-old man presents to his primary care physician for evaluation before going off to college. Specifically, he wants to know how to stay healthy while living outside his home. Since childhood he has suffered severe sunburns even when he goes outside for a small period of time. He has also developed many freckles and rough-surfaced growths starting at the same age. Finally, his eyes are very sensitive and become irritated, bloodshot, and painful after being outside. A defect in a protein with which of the following functions is most likely responsible for this patient's symptoms?
- A. Distinguishing methylated from unmethylated strands
- B. Recognition of chemically dimerized bases (Correct Answer)
- C. Endonucleolytic removal of bases from backbone
- D. Recognition of mismatched bases
- E. Sister chromatid binding and recombination
Disorders of pigmentation Explanation: ***Recognition of chemically dimerized bases***
- The patient's symptoms (severe sunburns, numerous freckles, rough growths, and ocular irritation) are highly suggestive of **Xeroderma Pigmentosum (XP)**, a genetic disorder characterized by extreme sensitivity to UV light.
- XP is caused by a defect in **nucleotide excision repair (NER)**, specifically the proteins involved in **recognizing and excising DNA damage** like thymine dimers formed by UV radiation.
*Distinguishing methylated from unmethylated strands*
- This function is crucial for **DNA mismatch repair**, which corrects errors incorporated during DNA replication.
- Defects in mismatch repair are associated with conditions like **Hereditary Nonpolyposis Colorectal Cancer (HNPCC)**, which presents differently from the patient's symptoms.
*Endonucleolytic removal of bases from backbone*
- This describes a step in **base excision repair (BER)**, which primarily handles small, non-helix-distorting base lesions.
- While important for DNA repair, defects in BER would not typically lead to the severe UV sensitivity and skin manifestations seen in this patient.
*Recognition of mismatched bases*
- This is a key step in **DNA mismatch repair**, where enzymes identify incorrectly paired bases after DNA replication.
- Deficiencies in this pathway lead to increased mutation rates and specific cancer syndromes, but not the severe UV sensitivity of Xeroderma Pigmentosum.
*Sister chromatid binding and recombination*
- This function is essential for proper chromosome segregation during cell division and for DNA repair via **homologous recombination**.
- Defects here can lead to disorders with chromosomal instability but do not directly explain the extreme UV sensitivity and skin cancers characteristic of Xeroderma Pigmentosum.
Disorders of pigmentation US Medical PG Question 3: A 53-year-old farmer presents to the clinic for evaluation of a pigmented lesion on his arm. He states that he first noticed the lesion last year, but he believes that it has been slowly growing in size. He otherwise does not have any complaints and is generally healthy. Which of the following findings on physical exam would suggest a malignant diagnosis?
- A. Symmetrical ovoid lesion
- B. Flat lesion with symmetric hyperpigmentation
- C. Tenderness to palpation
- D. Hyperpigmented lesion with smooth borders
- E. Different pigmentation throughout the lesion (Correct Answer)
Disorders of pigmentation Explanation: ***Different pigmentation throughout the lesion***
- **Malignant melanoma** often presents with **multicolor variegation** or areas of differing pigmentation within the same lesion, which is a key indicator for malignancy (the "C" in ABCDE).
- This **uneven coloration** reflects the uncontrolled proliferation of melanocytes producing melanin in varying amounts and patterns, a hallmark of dysplastic changes.
*Symmetrical ovoid lesion*
- **Benign nevi** (moles) typically maintain **symmetry** in their shape and border, meaning that if you were to draw a line through the middle of the lesion, both halves would largely match.
- While some melanomas can be ovoid, **asymmetry** is a more concerning feature for malignancy, unlike the description provided here.
*Flat lesion with symmetric hyperpigmentation*
- A **benign lesion** often has **symmetric pigmentation** and a uniform color distribution, with a flat appearance.
- **Irregular pigmentation** (color variegation) within the lesion is a more concerning sign for **melanoma**, falling under the "C" (color) criteria of the ABCDEs.
*Tenderness to palpation*
- **Tenderness** is not a typical characteristic of early or even advanced **melanoma**; pain or tenderness is often associated with inflammation, infection, or trauma rather than primary skin cancer.
- While ulcerated or infected tumors can be painful, tenderness alone without other suspicious features is **not a primary diagnostic criterion** for melanoma.
*Hyperpigmented lesion with smooth borders*
- **Benign moles** typically have **smooth, regular, and well-defined borders**, making them appear round or oval.
- In contrast, **malignant melanoma** often presents with **irregular, notched, or poorly defined borders (the "B" in ABCDE),** which would be more indicative of malignancy.
Disorders of pigmentation US Medical PG Question 4: A 27-year-old Caucasian female presents complaining of recent weight loss and weakness. She reports that she feels dizzy and lightheaded every morning when she gets out of bed, and often at work whenever she must rise from her desk. Physical exam reveals several areas of her skin including her elbows and knees are more pigmented than other areas. Which of the following would be consistent with the patient's disease?
- A. Pretibial myxedema
- B. Hyperkalemia (Correct Answer)
- C. Hypernatremia
- D. Central obesity
- E. Hyperglycemia
Disorders of pigmentation Explanation: ***Hyperkalemia***
- The patient's symptoms (weight loss, weakness, **orthostatic hypotension**, and **hyperpigmentation**) are classic for **primary adrenal insufficiency (Addison's disease)**.
- In primary adrenal insufficiency, decreased **aldosterone** production leads to **impaired renal sodium reabsorption** and **potassium excretion**, resulting in **hyperkalemia**.
*Pretibial myxedema*
- This condition is characteristic of **Graves' disease**, which involves hyperthyroidism, not adrenal insufficiency.
- It presents as localized thickening and induration of the skin, typically on the shins.
*Hypernatremia*
- **Hyponatremia** (low sodium) is a common finding in primary adrenal insufficiency due to impaired aldosterone action and increased ADH secretion.
- **Hypernatremia** (high sodium) would be inconsistent with this diagnosis.
*Central obesity*
- **Central obesity** and **moon facies** are characteristic features of **Cushing's syndrome**, which is caused by *excess* glucocorticoids, the opposite of adrenal insufficiency.
- Patients with Addison's disease often experience **weight loss** rather than weight gain.
*Hyperglycemia*
- **Hypoglycemia** is commonly seen in primary adrenal insufficiency due to the lack of **cortisol**, which plays a crucial role in maintaining blood glucose levels.
- **Hyperglycemia** would suggest conditions like diabetes or Cushing's syndrome, not adrenal insufficiency.
Disorders of pigmentation US Medical PG Question 5: A 52-year-old woman sees you in your office with a complaint of new-onset headaches over the past few weeks. On exam, you find a 2 x 2 cm dark, irregularly shaped, pigmented lesion on her back. She is concerned because her father recently passed away from skin cancer. What tissue type most directly gives rise to the lesion this patient is experiencing?
- A. Neural crest cells (Correct Answer)
- B. Endoderm
- C. Mesoderm
- D. Ectoderm
- E. Neuroectoderm
Disorders of pigmentation Explanation: ***Neural crest cells***
- The suspected lesion, given its description and the patient's family history of skin cancer, is likely a **melanoma**.
- Melanoma originates from **melanocytes**, which are derived from **neural crest cells** during embryonic development.
*Endoderm*
- The endoderm gives rise to the **lining of the gastrointestinal and respiratory tracts**, as well as organs such as the liver and pancreas.
- It is not involved in the formation of melanocytes or skin lesions like melanoma.
*Mesoderm*
- The mesoderm forms tissues such as **muscle, bone, cartilage, connective tissue**, and the circulatory system.
- It does not directly give rise to melanocytes, which are the cells of origin for melanoma.
*Ectoderm*
- The ectoderm gives rise to the **epidermis, nervous system**, and sensory organs.
- While melanocytes are found in the epidermis, they are specifically derived from the **neural crest (a sub-population of ectoderm)**, not the general ectoderm.
*Neuroectoderm*
- Neuroectoderm specifically refers to the ectoderm that develops into the **nervous system**.
- While neural crest cells originate from the neuroectoderm, "neural crest cells" is a more precise answer for the origin of melanocytes.
Disorders of pigmentation US Medical PG Question 6: A 17-year-old Latin American woman with no significant past medical history or family history presents to her pediatrician with concerns about several long-standing skin lesions. She notes that she has had a light-colored rash on her chest and abdomen that has been present for the last 2 years. The blood pressure is 111/81 mm Hg, pulse is 82/min, respiratory rate is 16/min, and temperature is 37.3°C (99.1°F). Physical examination reveals numerous hypopigmented macules over her chest and abdomen. No lesions are seen on her palms or soles. When questioned, she states that these lesions do not tan like the rest of her skin when exposed to the sun. The remainder of her review of systems is negative. What is the most likely cause of these lesions?
- A. Cutaneous T cell lymphoma
- B. Post-viral immunologic reaction
- C. Malassezia yeast (Correct Answer)
- D. Treponema pallidum infection
- E. TYR gene dysfunction in melanocytes
Disorders of pigmentation Explanation: ***Malassezia yeast***
- The presence of **long-standing hypopigmented macules** on the trunk that **do not tan with sun exposure** is highly characteristic of **tinea versicolor**, caused by *Malassezia* yeast.
- *Malassezia* produces **azelaic acid**, which inhibits melanin synthesis in melanocytes, leading to the characteristic hypopigmentation.
*Cutaneous T cell lymphoma*
- This typically presents as **erythematous patches or plaques** (mycosis fungoides) and would not primarily cause uniform hypopigmented macules that are exacerbated by sun exposure in this manner.
- While hypopigmented mycosis fungoides exists, it is rare and usually associated with other skin and systemic symptoms not described here.
*Post-viral immunologic reaction*
- A post-viral reaction might cause a rash, but it is unlikely to result in **chronic, localized hypopigmented macules** that specifically fail to tan.
- Such reactions are usually more generalized, self-limiting, or present with other characteristic features like pityriasis rosea.
*Treponema pallidum infection*
- **Syphilis** can cause a wide variety of skin manifestations, but hypopigmented macules on the trunk are not a typical presentation, especially without other signs of primary or secondary syphilis, and lesions would also appear on palms and soles.
- **Hyperpigmented macules** (syphilitic leukoderma) can rarely occur, but typically appear on the neck ("collar of Venus").
*TYR gene dysfunction in melanocytes*
- **TYR gene dysfunction** refers to mutations affecting **tyrosinase**, an enzyme crucial for melanin production. This is the underlying cause for **oculocutaneous albinism**, a condition characterized by widespread *congenital* hypopigmentation or amelanosis affecting skin, hair, and eyes.
- This patient's rash is described as "light-colored," "present for 2 years," and a late-onset issue, not a generalized congenital lack of pigmentation, making albinism unlikely.
Disorders of pigmentation US Medical PG Question 7: A 28-year-old woman presents with progressive darkening of her face that started during pregnancy. The pigmentation is symmetrical and primarily affects her cheeks and forehead. It became more prominent with sun exposure. Examination reveals bilateral, symmetrical brown patches on her face. Which of the following is the most appropriate initial management?
- A. Topical steroids
- B. Oral isotretinoin
- C. Broad-spectrum sunscreen and sun avoidance (Correct Answer)
- D. Phototherapy
Disorders of pigmentation Explanation: ***Broad-spectrum sunscreen and sun avoidance***
- The patient's presentation of **symmetrical facial hyperpigmentation** during pregnancy that worsens with sun exposure is characteristic of **melasma**.
- **Photoprotection** with broad-spectrum sunscreen and strict sun avoidance is the cornerstone of initial management and prevention of melasma exacerbation.
*Topical steroids*
- Topical steroids are **anti-inflammatory agents** and are **not indicated** as primary treatment for melasma.
- Their prolonged use on the face can lead to side effects such as **skin atrophy**, telangiectasias, and acne.
*Oral isotretinoin*
- Oral isotretinoin is primarily used for **severe acne** and is a potent teratogen, making it **contraindicated in pregnancy**.
- It is **not effective** for the treatment of melasma.
*Phototherapy*
- Phototherapy, such as **UVB or UVA light therapy**, is used for conditions like psoriasis or eczema.
- It would be **counterproductive** for melasma, as UV exposure actually worsens the condition.
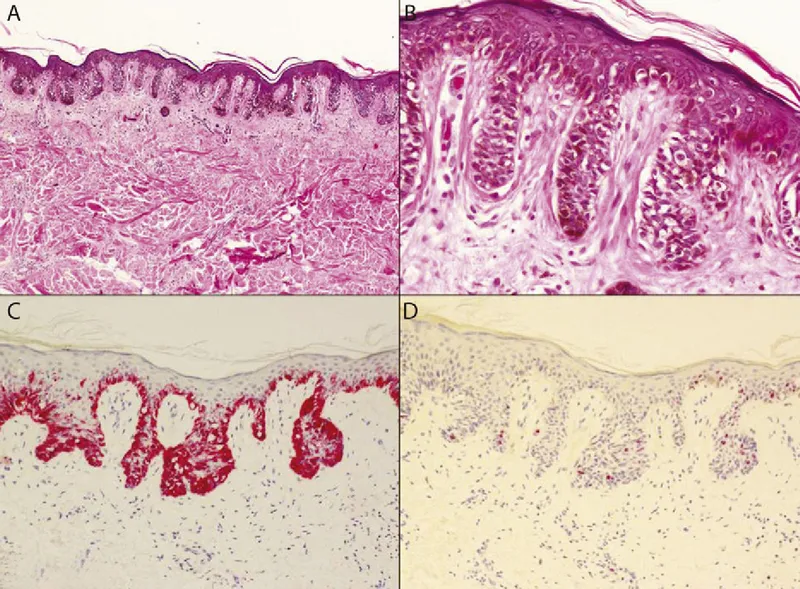
Disorders of pigmentation US Medical PG Question 8: An otherwise healthy 17-year-old girl comes to the physician because of multiple patches on her face, hands, abdomen, and feet that are lighter than the rest of her skin. The patches began to appear 3 years ago and have been gradually increasing in size since. There is no associated itchiness, redness, numbness, or pain. She emigrated from India 2 years ago. An image of the lesions on her face is shown. Which of the following is most likely involved in the pathogenesis of this patient's skin findings?
- A. Defective tuberin protein
- B. Infection with Malassezia globosa
- C. Infection with Mycobacterium leprae
- D. Absence of tyrosinase activity
- E. Autoimmune destruction of melanocytes (Correct Answer)
Disorders of pigmentation Explanation: ***Autoimmune destruction of melanocytes***
- The presentation of **multiple, gradually enlarging hypopigmented patches** on various body areas, particularly in an otherwise healthy individual, is highly suggestive of **vitiligo**.
- **Vitiligo** is an acquired depigmentation disorder resulting from the **autoimmune destruction of melanocytes**, leading to a complete absence of melanin in the affected areas.
*Defective tuberin protein*
- **Defective tuberin protein** is associated with **tuberous sclerosis**, a neurocutaneous syndrome.
- Skin manifestations of tuberous sclerosis include **ash-leaf spots** (hypopigmented macules), **facial angiofibromas**, and **Shagreen patches**, which are typically present from birth or early childhood and often associated with neurological symptoms.
*Infection with Malassezia globosa*
- **Malassezia globosa** causes **tinea versicolor** (pityriasis versicolor), a superficial fungal infection characterized by **hypopigmented or hyperpigmented patches** with fine scale.
- These lesions often occur on the trunk and proximal extremities and typically **fluoresce yellow-green** under Wood's lamp, which is not mentioned here.
*Infection with Mycobacterium leprae*
- **Mycobacterium leprae** causes **leprosy**, which can present with **hypopigmented macules** that are typically **anesthetic** (loss of sensation).
- While the patient is from an endemic area (India), the lack of **anesthesia**, associated neuropathic symptoms, or active inflammation makes leprosy less likely.
*Absence of tyrosinase activity*
- **Absence of tyrosinase activity** is characteristic of **oculocutaneous albinism**, a *genetic* condition leading to a *generalized lack of pigmentation* in the skin, hair, and eyes.
- This patient presents with *localized patches* of depigmentation that appeared at 14 years old, which is inconsistent with congenital albinism.
Disorders of pigmentation US Medical PG Question 9: A 50-year-old woman with rheumatoid arthritis on methotrexate develops rapidly progressive painful ulcers on her legs with violaceous undermined borders. Biopsy shows neutrophilic dermal infiltrate with areas of necrosis, but no vasculitis or infection. Wound cultures are negative. Despite debridement, the ulcers worsen. C-ANCA and P-ANCA are negative. Evaluate the diagnosis and determine the management that addresses both the cutaneous condition and systemic disease.
- A. Discontinue all immunosuppression to allow wound healing
- B. Increase methotrexate dose and add wound care
- C. Discontinue methotrexate, start cyclosporine and prednisone
- D. Start broad-spectrum antibiotics and surgical debridement
- E. Continue methotrexate, add TNF-alpha inhibitor and systemic corticosteroids (Correct Answer)
Disorders of pigmentation Explanation: ***Continue methotrexate, add TNF-alpha inhibitor and systemic corticosteroids***
- This patient presents with **Pyoderma Gangrenosum (PG)**, a neutrophilic dermatosis characterized by **violaceous undermined borders** and **pathergy**, where surgical debridement cause lesion expansion.
- **TNF-alpha inhibitors** (e.g., adalimumab, infliximab) are first-line for recalcitrant PG and simultaneously provide excellent control for the underlying **Rheumatoid Arthritis**.
*Discontinue all immunosuppression to allow wound healing*
- Since PG is an **autoimmune inflammatory condition**, withdrawing immunosuppression would result in rapid progression of the ulcers rather than healing.
- Wound healing in PG requires **suppressing the inflammatory response** rather than the typical wound care approach for infected ulcers.
*Increase methotrexate dose and add wound care*
- While **methotrexate** treats RA, it is often insufficient as a monotherapy for the acute, rapidly progressive phase of **Pyoderma Gangrenosum**.
- Standard wound care alone is ineffective because the primary driver is **neutrophilic infilatration**, which requires targeted biologic or corticosteroid therapy.
*Discontinue methotrexate, start cyclosporine and prednisone*
- While **cyclosporine** and **prednisone** are used for PG, discontinuing methotrexate may lead to a flare of the patient’s **Rheumatoid Arthritis**.
- Maintaining a coordinated regimen that addresses both the skin and the joints, such as adding a **TNF-alpha inhibitor**, is preferred over switching all medications.
*Start broad-spectrum antibiotics and surgical debridement*
- **Surgical debridement** is contraindicated in PG due to **pathergy**, a phenomenon where trauma to the skin induces new or worsening lesions.
- **Antibiotics** are unnecessary as the biopsy and cultures confirmed a **sterile neutrophilic infiltrate** rather than an infectious process.
Disorders of pigmentation US Medical PG Question 10: A 25-year-old woman presents with painful oral ulcers and a pustular rash at venipuncture sites. She has genital ulcers and a history of recurrent uveitis. Skin biopsy from a pustule shows neutrophilic infiltrate in the dermis without vasculitis or infection. HLA-B51 testing is positive. She is planning pregnancy. Evaluate the management strategy considering disease control and pregnancy planning.
- A. Start methotrexate for disease control
- B. Start colchicine monotherapy and proceed with pregnancy
- C. Start high-dose corticosteroids and azathioprine, delay pregnancy
- D. Start infliximab, use contraception, then transition to low-risk therapy before conception (Correct Answer)
- E. Avoid all immunosuppression and manage symptoms only
Disorders of pigmentation Explanation: ***Start infliximab, use contraception, then transition to low-risk therapy before conception***
- This patient has **Beh'et's disease** with **recurrent uveitis**, which is **sight-threatening** and requires aggressive biological therapy like **infliximab** or **TNF-inhibitors** for rapid remission.
- Achievng **remission** before pregnancy is vital; while TNF-inhibitors are often continued, transitioning to pregnancy-compatible agents like **azathioprine** or **colchicine** ensures long-term safety.
*Start methotrexate for disease control*
- **Methotrexate** is strictly **teratogenic** and must be avoided in patients planning pregnancy or discontinued months before conception.
- While it can treat some aspects of systemic inflammation, it is not the first-line gold standard for **acute ocular Beh'et's** compared to biologics.
*Start colchicine monotherapy and proceed with pregnancy*
- **Colchicine** is excellent for **mucocutaneous** symptoms (oral and genital ulcers) but is insufficient as monotherapy to prevent blindness from **recurrent uveitis**.
- Relying on monotherapy in a patient with active ocular disease risks **permanent vision loss** during the pregnancy period.
*Start high-dose corticosteroids and azathioprine, delay pregnancy*
- While **azathioprine** is used for maintenance, **high-dose corticosteroids** carry significant side effects and are usually a bridge, not a comprehensive plan for ocular stabilization.
- This strategy lacks the rapid, potent **TNF-alpha inhibition** needed to quickly arrest the neutrophilic inflammation seen in severe Beh'et's flare-ups.
*Avoid all immunosuppression and manage symptoms only*
- **Beh'et's disease** is a multi-system inflammatory disorder; leaving **uveitis** and systemic vasculitis untreated leads to irreversible organ damage and **blindness**.
- Symptomatic management alone ignores the **neutrophilic infiltrate** and underlying autoimmune process, which could also lead to pregnancy complications due to active maternal disease.
More Disorders of pigmentation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.