Adnexal tumors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Adnexal tumors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Adnexal tumors US Medical PG Question 1: A 7-year-old girl comes in to the emergency department with her mother for swelling of her left periorbital region. Yesterday morning she woke up with a painful, warm, soft lump on her left eyelid. Eye movement does not worsen the pain. Physical examination shows redness and swelling of the upper left eyelid, involving the hair follicles. Upon palpation, the swelling drains purulent fluid. Which of the following is the most likely diagnosis?
- A. Xanthelasma
- B. Chalazion
- C. Dacryocystitis
- D. Blepharitis
- E. Hordeolum (Correct Answer)
Adnexal tumors Explanation: ***Hordeolum***
- A hordeolum (stye) is an **acute bacterial infection** of the sebaceous glands of the eyelid, often involving a hair follicle, presenting as a **painful, warm, soft lump with purulent drainage**.
- The swelling of the eyelid **involving hair follicles** and the presence of **purulent fluid** are classic signs of a hordeolum.
*Xanthelasma*
- **Xanthelasma** consists of **yellowish plaques** on the eyelids, typically caused by cholesterol deposits, and is painless and not inflammatory.
- It is a **chronic condition** and does not present with acute pain, warmth, or purulent discharge.
*Chalazion*
- A **chalazion** is a **painless, firm, non-tender nodule** resulting from a blocked meibomian gland, which is usually not painful or associated with acute inflammation and purulence.
- Unlike a hordeolum, it is a **granulomatous reaction** and typically presents as a non-infectious, chronic lesion.
*Dacryocystitis*
- **Dacryocystitis** is an infection of the **lacrimal sac**, located at the inner corner of the eye, presenting with swelling, redness, and pain in that specific area.
- This condition would not typically involve the eyelid's hair follicles or present with general eyelid purulence.
*Blepharitis*
- **Blepharitis** is a **chronic inflammation of the eyelid margins**, characterized by redness, flaking, and crusting of the eyelashes, often with itching or burning.
- It causes **generalized eyelid discomfort and irritation**, but not a localized warm, painful, purulent lump like described in the scenario.
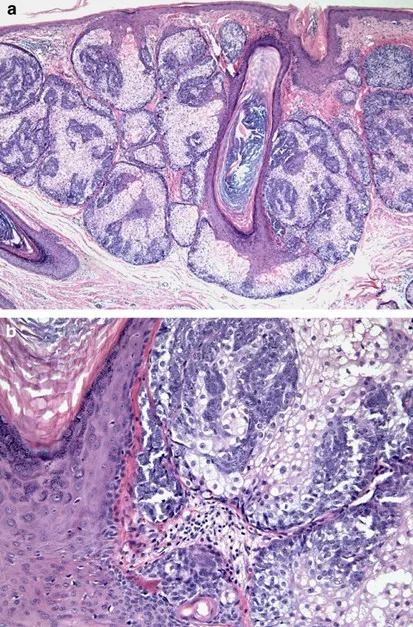
Adnexal tumors US Medical PG Question 2: A 14-year-old boy presents as a new patient to your practice. While conducting your physical exam, you observe the findings depicted in Figures A and B. Which of the following additional findings would most likely be found in this patient?
- A. Multiple café-au-lait macules (Correct Answer)
- B. A white tuft of scalp hair since birth
- C. The presence of ash-leaf spots
- D. Facial angiofibromas
- E. A family history of seizures and intellectual disability
Adnexal tumors Explanation: ***Multiple café-au-lait macules***
- The images show **Lisch nodules** (iris hamartomas), which are pathognomonic for **Neurofibromatosis type 1 (NF1)**.
- **Café-au-lait macules** are the most common and often earliest manifestation of NF1, present in **>99% of patients**.
- Diagnostic criteria require **≥6 café-au-lait macules** (>5mm in diameter prepubertal, >15mm postpubertal).
- This is the **most likely additional finding** in a patient with Lisch nodules.
*A family history of seizures and intellectual disability*
- While **learning disabilities** occur in ~50% of NF1 patients and **seizures** can occur, this is not the most specific or common finding.
- **Café-au-lait macules** and **cutaneous neurofibromas** are far more consistent and diagnostically significant.
*A white tuft of scalp hair since birth*
- A **white tuft of scalp hair** (poliosis) is characteristic of **Waardenburg syndrome**, not NF1.
- Waardenburg syndrome presents with **hearing loss**, **heterochromia iridis**, and **dystopia canthorum**.
*The presence of ash-leaf spots*
- **Ash-leaf spots** (hypopigmented macules) are a hallmark of **Tuberous Sclerosis Complex (TSC)**.
- TSC has different ocular findings like **retinal hamartomas**, not Lisch nodules.
*Facial angiofibromas*
- **Facial angiofibromas** (adenoma sebaceum) are a classic manifestation of **Tuberous Sclerosis Complex (TSC)**, not NF1.
- NF1 typically presents with **cutaneous and plexiform neurofibromas**, not angiofibromas.
Adnexal tumors US Medical PG Question 3: A 16-year-old girl is brought to the physician by her mother because she has not had her menstrual period yet. At birth, she was found to have partial labial fusion and clitoromegaly. The mother reports that during the pregnancy she had noticed abnormal hair growth on her chin. The girl has severe acne. Three years ago, she broke her wrist after a minor trauma. Last year, she sustained a spinal compression fracture after lifting a box during a move. She currently takes oral isotretinoin and an oral contraceptive. The patient is at the 97th percentile for height and 50th percentile for weight. Physical examination shows numerous inflamed pustules on her face and upper back. Breast development is at Tanner stage I. The patient refuses to have a pelvic examination. A pelvic ultrasound shows ovaries with multiple cysts and a normal uterus. Which of the following is the most likely diagnosis?
- A. Polycystic ovary syndrome
- B. Turner syndrome
- C. Congenital adrenal hyperplasia
- D. Aromatase deficiency (Correct Answer)
- E. Hyperprolactinemia
Adnexal tumors Explanation: ***Aromatase deficiency***
- Aromatase deficiency presents with **undervirilized female external genitalia** at birth due to impaired estrogen synthesis, leading to **ambiguous genitalia** (partial labial fusion and clitoromegaly) in 46,XX individuals, which describes the patient's birth findings.
- The patient's **primary amenorrhea**, **acne**, advanced bone age (suggested by fractures from minor trauma), **high height percentile**, and **low or absent breast development (Tanner stage I)** are all consistent with a lack of estrogenization and excess androgen effects due to impaired conversion of androgens to estrogens.
*Polycystic ovary syndrome*
- While **PCOS** can cause hirsutism, acne, and menstrual irregularities, it typically presents after puberty with **normal external genitalia at birth** and often **obesity**, which contrasts with this patient's birth findings and current high height percentile with only average weight.
- PCOS is associated with **insulin resistance** and usually presents with secondary amenorrhea or oligomenorrhea, not primary amenorrhea in a patient with severe virilization signs from birth.
*Turner syndrome*
- **Turner syndrome** (45,XO) is characterized by **gonadal dysgenesis**, leading to **primary amenorrhea** and **lack of breast development**, but it presents with a distinctive phenotype including short stature, webbed neck, and **normal female external genitalia** at birth, and does not involve virilization or clitoromegaly.
- Patients with Turner syndrome typically have **short stature** and a lack of secondary sexual characteristics, which is inconsistent with this patient's 97th percentile for height and signs of androgen excess.
*Congenital adrenal hyperplasia*
- **CAH**, particularly 21-hydroxylase deficiency, causes **virilization** in 46,XX individuals with **clitoromegaly** and labial fusion at birth, and pubertal development issues. However, untreated CAH typically results in **short stature** due to premature epiphyseal fusion from excessive androgens and often presents with salt-wasting crises, neither of which are described here.
- The patient's **tall stature** (97th percentile for height) makes CAH less likely, as CAH typically leads to advanced bone age and short adult stature.
*Hyperprolactinemia*
- **Hyperprolactinemia** causes **amenorrhea** and can lead to absent or delayed puberty, but it does **not cause virilization** (clitoromegaly, acne) or ambiguous genitalia at birth.
- It is often associated with galactorrhea, which is not mentioned in this case, and does not explain the patient's birth findings.
Adnexal tumors US Medical PG Question 4: A 27-year-old school teacher visits her doctor because of disfiguring skin lesions that started to appear in the past few days. The lesions are mostly located on her chest, shoulders, and back. They are 2–5 mm in diameter, droplike, erythematous papules with fine silver scales. Besides a sore throat and laryngitis requiring amoxicillin several weeks ago, she has no significant medical history. What is the most likely diagnosis?
- A. Bullous pemphigoid
- B. Plaque psoriasis
- C. Pemphigus vulgaris
- D. Guttate psoriasis (Correct Answer)
- E. Inverse psoriasis
Adnexal tumors Explanation: ***Guttate psoriasis***
- This condition is characterized by **acute onset** of **small (2–5 mm)**, **droplike**, erythematous papules with **fine silver scales**, predominantly on the trunk.
- It often follows an **upper respiratory tract infection**, particularly with *Streptococcus pyogenes*, as indicated by the recent **sore throat and laryngitis** requiring amoxicillin.
*Bullous pemphigoid*
- This autoimmune blistering disease primarily affects the **elderly** and presents with large, **tense bullae** on an erythematous or urticarial base.
- It does not typically present with small, scaly papules or have a direct association with recent streptococcal infections.
*Plaque psoriasis*
- The most common type of psoriasis, presenting with **well-demarcated**, erythematous plaques covered by **thick, silvery scales**, usually larger than 5 mm.
- While it can be found on the trunk, its lesions are typically larger and chronologically more stable than the acute, droplike lesions described.
*Pemphigus vulgaris*
- This is a severe autoimmune blistering disease characterized by **flaccid bullae** and erosions on the skin and **mucous membranes**.
- It involves intraepidermal blistering due to acantholysis and is not associated with recent sore throat or small, scaly papules.
*Inverse psoriasis*
- This form of psoriasis affects **skin folds** (e.g., axillae, groin, inframammary regions) and presents as **smooth, erythematous plaques** without significant scaling due to moisture.
- Its location and lack of typical scaling differ from the described lesions on the chest, shoulders, and back.
Adnexal tumors US Medical PG Question 5: A 9-year-old boy is brought to the physician for evaluation of 2 months of progressive clumsiness, falls, and increased urinary frequency. Physical examination shows bilateral temporal visual field loss. An MRI of the head shows a small calcified suprasellar mass. The patient undergoes surgery with complete removal of the mass. Pathological examination of the specimen shows a lobular tumor composed of cysts filled with oily, brownish-yellow fluid. This mass is most likely derived from which of the following structures?
- A. Arachnoid cells
- B. Ventricular ependyma
- C. Lactotroph cells
- D. Rathke pouch (Correct Answer)
- E. Astroglial cells
Adnexal tumors Explanation: ***Rathke pouch***
- The combination of **suprasellar mass**, visual field deficits (bitemporal hemianopsia due to optic chiasm compression), **calcification**, and cystic components filled with **oily, brownish-yellow fluid** in a child points strongly to a **craniopharyngioma**.
- **Craniopharyngiomas** are benign tumors derived from remnants of **Rathke's pouch**, which is an embryonic evagination of the stomodeum that gives rise to the anterior pituitary.
*Arachnoid cells*
- Tumors arising from **arachnoid cells** are typically **meningiomas**, which are more common in adults and usually present as dural-based masses, often without significant cystic components.
- While meningiomas can calcify, their characteristic histology (whorled patterns, psammoma bodies) and typical presentation differ from craniopharyngiomas.
*Ventricular ependyma*
- Tumors derived from **ependyma** are **ependymomas**, which typically arise within the ventricles of the brain or spinal cord.
- They are less common in the suprasellar region and their characteristic cystic or fluid content is usually not described as oily and brownish-yellow.
*Lactotroph cells*
- **Lactotroph cells** are found in the **anterior pituitary gland**, and tumors arising from them are **prolactinomas**.
- While prolactinomas can present with visual field defects due to suprasellar extension, they are typically solid pituitary adenomas, rarely calcified, and do not contain oily, brownish-yellow fluid.
*Astroglial cells*
- Tumors originating from **astroglial cells** include **astrocytomas** and **glioblastomas**, which are highly variable in presentation but are typically solid or have pseudocystic areas, not an oily, brownish-yellow fluid-filled cyst.
- While some astrocytomas can calcify, their microscopic appearance and characteristic fluid content are different from what is described.
Adnexal tumors US Medical PG Question 6: A 55-year-old man with a history of sun exposure presents with a slowly growing, pearly nodule with telangiectasias on his nose. The lesion occasionally bleeds when traumatized. Biopsy shows basaloid cells arranged in palisading patterns. Which of the following mutations is most likely involved in the pathogenesis?
- A. P53 mutation
- B. PTCH1 gene mutation (Correct Answer)
- C. EGFR mutation
- D. KIT mutation
Adnexal tumors Explanation: **PTCH1 gene mutation**
- The clinical presentation of a **pearly nodule with telangiectasias** on the **nose**, history of **sun exposure**, and **basaloid cells arranged in palisading patterns** on biopsy are classic for **basal cell carcinoma (BCC)** [1].
- Mutations in the **PTCH1 gene**, a tumor suppressor gene involved in the **Hedgehog signaling pathway**, are found in the majority of sporadic BCCs and are central to its pathogenesis [2,3].
*P53 mutation*
- While **P53 mutations** are common in many cancers, including **squamous cell carcinoma** [3], they are not the primary driver mutation for basal cell carcinoma in the way PTCH1 mutations are.
- Loss of P53 function typically leads to uncontrolled cell growth and reduced apoptosis, but it's a general cancer mechanism rather than a specific one for BCC.
*EGFR mutation*
- **EGFR mutations** are primarily associated with certain types of **lung adenocarcinoma** and **glioblastoma**, not basal cell carcinoma.
- These mutations lead to constitutive activation of the **epidermal growth factor receptor** signaling pathway, promoting cell proliferation and survival in those specific cancers.
*KIT mutation*
- **KIT mutations** are most commonly found in **gastrointestinal stromal tumors (GIST)** and certain types of **melanoma**.
- The KIT receptor tyrosine kinase plays a role in cell growth and differentiation in specific cell lineages, distinct from the epidermal cells involved in BCC.
**References:**
[1] Kumar V, Abbas AK, et al.. Robbins and Cotran Pathologic Basis of Disease. 9th ed. The Skin, pp. 1158-1162.
[2] Kumar V, Abbas AK, et al.. Robbins and Cotran Pathologic Basis of Disease. 9th ed. Neoplasia, pp. 306-307.
[3] Cross SS. Underwood's Pathology: A Clinical Approach. 6th ed. Disorders Involving Inflammatory And Haemopoietic Cells, pp. 643-644.
Adnexal tumors US Medical PG Question 7: A 51-year-old woman presents to the dermatologist with concern for a new skin lesion (Image A). You note two similar lesions on her back. Which of the following is a true statement about these lesions?
- A. They must be followed closely for concern of malignancy.
- B. They will likely regress spontaneously.
- C. They may be associated with von Hippel-Lindau disease.
- D. They will likely grow rapidly.
- E. They will likely increase in number over time. (Correct Answer)
Adnexal tumors Explanation: ***They will likely increase in number over time.***
- The image likely displays **cherry angiomas**, which are common benign vascular lesions that typically increase in number with age.
- While individual lesions may remain stable, their overall prevalence on the skin tends to rise as a person ages, especially after the age of 30.
*They must be followed closely for concern of malignancy.*
- **Cherry angiomas** are **benign vascular proliferations** and do not carry a risk of malignant transformation.
- They are typically diagnosed clinically and do not require ongoing surveillance for malignancy.
*They will likely regress spontaneously.*
- **Cherry angiomas** are **permanent lesions** and do not typically regress spontaneously.
- Once they appear, they usually persist and often grow slightly in size over time.
*They may be associated with von Hippel-Lindau disease.*
- **Von Hippel-Lindau (VHL) disease** is associated with **hemangioblastomas** (in the CNS and retina), **pheochromocytomas**, and **renal cell carcinoma**, but not typically cherry angiomas.
- The characteristic skin lesions in VHL are often **cutaneous cavernous hemangiomas** or **capillary malformations**, not the common cherry angioma.
*They will likely grow rapidly.*
- While cherry angiomas can slowly increase in size over many years, they do **not typically grow rapidly**.
- Rapid growth of a cutaneous lesion would be a more concerning feature for other conditions, such as **malignant melanoma** or a **rapidly growing cyst**, not cherry angiomas.
Adnexal tumors US Medical PG Question 8: A 50-year-old woman with rheumatoid arthritis on methotrexate develops rapidly progressive painful ulcers on her legs with violaceous undermined borders. Biopsy shows neutrophilic dermal infiltrate with areas of necrosis, but no vasculitis or infection. Wound cultures are negative. Despite debridement, the ulcers worsen. C-ANCA and P-ANCA are negative. Evaluate the diagnosis and determine the management that addresses both the cutaneous condition and systemic disease.
- A. Discontinue all immunosuppression to allow wound healing
- B. Increase methotrexate dose and add wound care
- C. Discontinue methotrexate, start cyclosporine and prednisone
- D. Start broad-spectrum antibiotics and surgical debridement
- E. Continue methotrexate, add TNF-alpha inhibitor and systemic corticosteroids (Correct Answer)
Adnexal tumors Explanation: ***Continue methotrexate, add TNF-alpha inhibitor and systemic corticosteroids***
- This patient presents with **Pyoderma Gangrenosum (PG)**, a neutrophilic dermatosis characterized by **violaceous undermined borders** and **pathergy**, where surgical debridement cause lesion expansion.
- **TNF-alpha inhibitors** (e.g., adalimumab, infliximab) are first-line for recalcitrant PG and simultaneously provide excellent control for the underlying **Rheumatoid Arthritis**.
*Discontinue all immunosuppression to allow wound healing*
- Since PG is an **autoimmune inflammatory condition**, withdrawing immunosuppression would result in rapid progression of the ulcers rather than healing.
- Wound healing in PG requires **suppressing the inflammatory response** rather than the typical wound care approach for infected ulcers.
*Increase methotrexate dose and add wound care*
- While **methotrexate** treats RA, it is often insufficient as a monotherapy for the acute, rapidly progressive phase of **Pyoderma Gangrenosum**.
- Standard wound care alone is ineffective because the primary driver is **neutrophilic infilatration**, which requires targeted biologic or corticosteroid therapy.
*Discontinue methotrexate, start cyclosporine and prednisone*
- While **cyclosporine** and **prednisone** are used for PG, discontinuing methotrexate may lead to a flare of the patient’s **Rheumatoid Arthritis**.
- Maintaining a coordinated regimen that addresses both the skin and the joints, such as adding a **TNF-alpha inhibitor**, is preferred over switching all medications.
*Start broad-spectrum antibiotics and surgical debridement*
- **Surgical debridement** is contraindicated in PG due to **pathergy**, a phenomenon where trauma to the skin induces new or worsening lesions.
- **Antibiotics** are unnecessary as the biopsy and cultures confirmed a **sterile neutrophilic infiltrate** rather than an infectious process.
Adnexal tumors US Medical PG Question 9: A 25-year-old woman presents with painful oral ulcers and a pustular rash at venipuncture sites. She has genital ulcers and a history of recurrent uveitis. Skin biopsy from a pustule shows neutrophilic infiltrate in the dermis without vasculitis or infection. HLA-B51 testing is positive. She is planning pregnancy. Evaluate the management strategy considering disease control and pregnancy planning.
- A. Start methotrexate for disease control
- B. Start colchicine monotherapy and proceed with pregnancy
- C. Start high-dose corticosteroids and azathioprine, delay pregnancy
- D. Start infliximab, use contraception, then transition to low-risk therapy before conception (Correct Answer)
- E. Avoid all immunosuppression and manage symptoms only
Adnexal tumors Explanation: ***Start infliximab, use contraception, then transition to low-risk therapy before conception***
- This patient has **Beh'et's disease** with **recurrent uveitis**, which is **sight-threatening** and requires aggressive biological therapy like **infliximab** or **TNF-inhibitors** for rapid remission.
- Achievng **remission** before pregnancy is vital; while TNF-inhibitors are often continued, transitioning to pregnancy-compatible agents like **azathioprine** or **colchicine** ensures long-term safety.
*Start methotrexate for disease control*
- **Methotrexate** is strictly **teratogenic** and must be avoided in patients planning pregnancy or discontinued months before conception.
- While it can treat some aspects of systemic inflammation, it is not the first-line gold standard for **acute ocular Beh'et's** compared to biologics.
*Start colchicine monotherapy and proceed with pregnancy*
- **Colchicine** is excellent for **mucocutaneous** symptoms (oral and genital ulcers) but is insufficient as monotherapy to prevent blindness from **recurrent uveitis**.
- Relying on monotherapy in a patient with active ocular disease risks **permanent vision loss** during the pregnancy period.
*Start high-dose corticosteroids and azathioprine, delay pregnancy*
- While **azathioprine** is used for maintenance, **high-dose corticosteroids** carry significant side effects and are usually a bridge, not a comprehensive plan for ocular stabilization.
- This strategy lacks the rapid, potent **TNF-alpha inhibition** needed to quickly arrest the neutrophilic inflammation seen in severe Beh'et's flare-ups.
*Avoid all immunosuppression and manage symptoms only*
- **Beh'et's disease** is a multi-system inflammatory disorder; leaving **uveitis** and systemic vasculitis untreated leads to irreversible organ damage and **blindness**.
- Symptomatic management alone ignores the **neutrophilic infiltrate** and underlying autoimmune process, which could also lead to pregnancy complications due to active maternal disease.
Adnexal tumors US Medical PG Question 10: A 70-year-old man on chronic warfarin therapy presents with sudden onset of painful purpura on his thighs and buttocks three days after starting warfarin for atrial fibrillation. He has a history of multiple DVTs. Skin biopsy shows thrombosis of dermal blood vessels with minimal inflammation. Laboratory studies show an INR of 3.5. Evaluate the pathophysiology and determine the most appropriate immediate management.
- A. Reduce warfarin dose and add compression therapy
- B. Discontinue all anticoagulation and monitor
- C. Continue warfarin and add aspirin for antiplatelet effect
- D. Discontinue warfarin, give vitamin K and fresh frozen plasma, start heparin bridge
- E. Discontinue warfarin, give protein C concentrate and alternative anticoagulation (Correct Answer)
Adnexal tumors Explanation: ***Discontinue warfarin, give protein C concentrate and alternative anticoagulation***
- This patient presents with **warfarin-induced skin necrosis**, likely caused by an underlying **Protein C deficiency** accentuated by the rapid drop in Protein C levels during initial warfarin therapy.
- Management requires immediate **discontinuation of warfarin**, replacement of the missing anticoagulant via **Protein C concentrate**, and switching to an **alternative anticoagulant** (like heparin).
*Reduce warfarin dose and add compression therapy*
- Reducing the dose is insufficient because the patient is in a **hypercoagulable state** that requires the complete removal of the offending agent.
- **Compression therapy** is used for venous insufficiency and does not address the underlying **microvascular thrombosis** seen in this condition.
*Discontinue all anticoagulation and monitor*
- Discontinuing all anticoagulation is dangerous as the patient is currently **hypercoagulable** and has a high risk for further **thromboembolic events**.
- Monitoring alone does not address the **dermal vessel thrombosis** already causing tissue necrosis.
*Continue warfarin and add aspirin for antiplatelet effect*
- Continuing warfarin would worsen the condition by further suppressing **Protein C** and **Protein S** levels while procoagulant factors like **Prothrombin** are still present.
- **Aspirin** targets platelets but does not reverse the **clotting factor imbalance** responsible for skin necrosis.
*Discontinue warfarin, give vitamin K and fresh frozen plasma, start heparin bridge*
- While **vitamin K** and **FFP** help reverse warfarin effects, FFP may not contain enough **Protein C** to rapidly stabilize this specific critical deficiency.
- Management must prioritize **specific protein replacement** or therapeutic dose heparin rather than a standard bridge protocol which may be too slow to stop the necrosis.
More Adnexal tumors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.