Reversible cell injury mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Reversible cell injury mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Reversible cell injury mechanisms US Medical PG Question 1: A scientist is studying the anatomy and function of bone growth. He is able to create a cell line of osteocytes with a mutation that prevents the osteocytes from exchanging nutrients and waste products within neighboring lamellae. This mutation most likely affected which of the following cell structures?
- A. Dynein
- B. Gap junctions (Correct Answer)
- C. Endoplasmic reticulum
- D. Plasma membrane
- E. Kinesin
Reversible cell injury mechanisms Explanation: ***Gap junctions***
- **Gap junctions** are specialized intercellular connections that permit direct communication and exchange of small molecules and ions between adjacent cells.
- In osteocytes, **gap junctions** located in the **canaliculi** are crucial for the exchange of nutrients, waste, and signaling molecules within and between lamellae, allowing for synchronous activity and maintaining bone health.
- These connexin-based channels physically connect the cytoplasm of neighboring osteocytes embedded in bone matrix.
*Dynein*
- **Dynein** is a motor protein involved in intracellular transport towards the minus end of **microtubules**, playing a role in moving organelles and vesicles.
- It is not directly responsible for the intercellular exchange of nutrients and waste products between cells.
*Endoplasmic reticulum*
- The **endoplasmic reticulum** is an organelle involved in protein synthesis and lipid metabolism, playing a critical role in cellular function.
- It does not directly mediate the exchange of nutrients and waste products between adjacent cells.
*Plasma membrane*
- While **gap junctions** are embedded within the **plasma membrane**, the membrane itself does not facilitate direct cytoplasmic continuity between cells.
- The question specifically refers to structures that enable direct cell-to-cell exchange; the mutation affects the gap junction channels themselves (connexins), not the general plasma membrane structure.
- Without functional gap junctions, the plasma membrane alone cannot support the intercellular communication required for osteocyte networks.
*Kinesin*
- **Kinesin** is a motor protein that moves cargo along **microtubules** towards the plus end, involved in fundamental cellular processes like cell division and organelle transport.
- It is not involved in direct intercellular communication for nutrient and waste exchange but rather internal cellular trafficking.
Reversible cell injury mechanisms US Medical PG Question 2: A healthy 34-year-old woman comes to the physician for advice on UV protection. She works as an archaeologist and is required to work outside for extended periods of time. She is concerned about premature skin aging. The physician recommends sun-protective clothing and sunscreen. In order to protect effectively against photoaging, the sunscreen should contain which of the following active ingredients?
- A. Zinc oxide (Correct Answer)
- B. Vitamin E
- C. Para-aminobenzoic acid
- D. Trimethoprim/sulfamethoxazole
- E. Trolamine salicylate
Reversible cell injury mechanisms Explanation: **Zinc oxide**
- **Zinc oxide** is a physical sunscreen that provides broad-spectrum protection by **blocking both UVA and UVB rays**.
- **UVA rays** are primarily responsible for **photoaging**, and physical blockers like zinc oxide are highly effective against them.
*Vitamin E*
- **Vitamin E** is an antioxidant that helps prevent cellular damage from free radicals, but it does **not provide direct protection against UV radiation** as a primary sunscreen ingredient.
- While commonly used in skincare for its **antioxidant properties**, it is not an active UV-blocking agent.
*Para-aminobenzoic acid*
- **Para-aminobenzoic acid (PABA)** is an older chemical sunscreen ingredient that primarily **blocks UVB rays**.
- It is often **associated with allergic reactions** and photosensitivity, and does not offer sufficient UVA protection for broad-spectrum coverage.
*Trimethoprim/sulfamethoxazole*
- **Trimethoprim/sulfamethoxazole** is an antibiotic combination used to treat various infections and has **no role in UV protection**.
- It is a medication and not an ingredient found in sunscreens for UV blocking.
*Trolamine salicylate*
- **Trolamine salicylate** is a topical analgesic ingredient often found in pain-relief creams and is **not an active sunscreen agent**.
- It has **no UV filtering properties** and does not protect against sun damage or photoaging.
Reversible cell injury mechanisms US Medical PG Question 3: A 52-year-old man is brought to the emergency department by ambulance after a motor vehicle accident. He was an unrestrained passenger who was ejected from the vehicle. On presentation, he is found to be actively bleeding from numerous wounds. His blood pressure is 76/42 mmHg and pulse is 152/min. Attempts at resuscitation fail, and he dies 25 minutes later. Autopsy shows blood in the peritoneal cavity, and histology of the kidney reveals swelling of the proximal convoluted tubule epithelial cells. Which of the following is most likely the mechanism underlying the renal cell findings?
- A. Decreased activity of caspase 7
- B. Increased activity of caspase 9
- C. Increased function of the Na+/K+-ATPase
- D. Increased activity of caspase 8
- E. Decreased function of the Na+/K+-ATPase (Correct Answer)
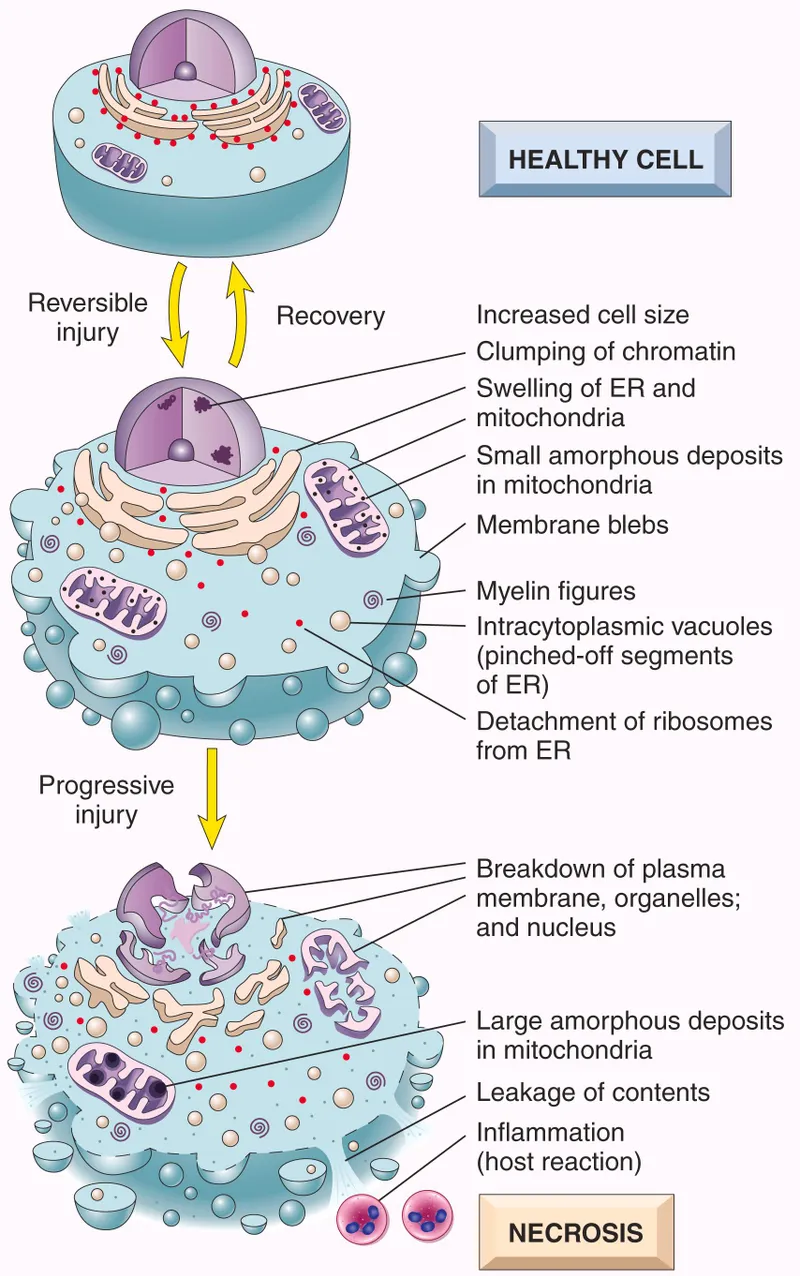
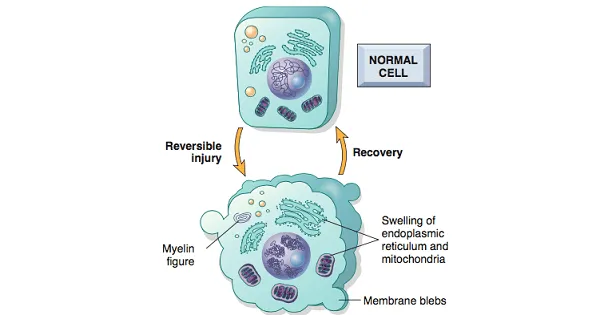
Reversible cell injury mechanisms Explanation: ***Decreased function of the Na+/K+-ATPase***
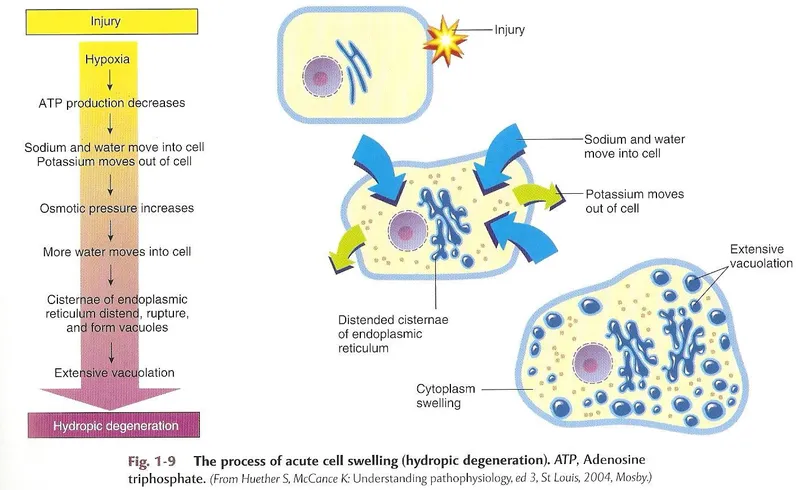
- The patient experienced **hypovolemic shock** due to severe blood loss, leading to a significant drop in blood pressure and organ perfusion. This results in **ischemia** of the renal cells.
- **Ischemic injury** impairs ATP production, which is essential for the function of the **Na+/K+-ATPase pump**. Failure of this pump leads to intracellular accumulation of sodium and water, causing **cellular swelling**, particularly noticeable in the proximal convoluted tubules.
*Decreased activity of caspase 7*
- **Caspases**, including caspase 7, are involved in **apoptosis** (programmed cell death), which involves cell shrinkage and fragmentation, not the swelling observed here.
- Decreased caspase activity would generally *reduce* apoptosis, which is not the primary mechanism of acute cell injury in shock.
*Increased activity of caspase 9*
- Increased activity of **caspase 9** is indicative of the **intrinsic apoptotic pathway**, typically initiated by mitochondrial damage.
- While prolonged ischemia can eventually lead to apoptotic changes, the acute finding of **cellular swelling** points more directly to immediate membrane pump dysfunction due to ATP depletion.
*Increased function of the Na+/K+-ATPase*
- **Increased function** of the Na+/K+-ATPase would actively pump sodium out of the cell and potassium in, *preventing* intracellular swelling.
- This option contradicts the observed finding of proximal convoluted tubule epithelial cell swelling, which is characteristic of acute cellular injury due to pump failure.
*Increased activity of caspase 8*
- **Caspase 8** is a key initiator caspase in the **extrinsic apoptotic pathway**, often triggered by death receptor signaling.
- Similar to caspase 9, increased caspase 8 activity would lead to apoptosis, characterized by cell shrinkage, not the **cellular swelling** seen in acute ischemic injury.
Reversible cell injury mechanisms US Medical PG Question 4: An investigator is studying the interaction between epithelial cells and calcium ion concentration. When the calcium ion concentration available to a sample of epithelial tissue is decreased, an increased gap between adjacent epithelial cells is seen on electron microscopy. This observed decrease in cell adhesion is most likely due to an effect on which of the following proteins?
- A. Actin
- B. Integrin
- C. Cadherin (Correct Answer)
- D. Claudin
- E. Cytokeratin
Reversible cell injury mechanisms Explanation: ***Cadherin***
- **Cadherins** are calcium-dependent adhesion proteins that mediate cell-to-cell adhesion, particularly in epithelial tissues.
- A decrease in calcium concentration would directly impair cadherin function, leading to reduced cell adhesion and increased intercellular gaps.
*Actin*
- **Actin** is a component of the cell's cytoskeleton, involved in cell shape, motility, and intracellular transport, but not directly responsible for calcium-dependent cell adhesion between epithelial cells.
- While actin filaments interact with adhesion junctions, their primary role is structural and dynamic rather than adhesive.
*Integrin*
- **Integrins** are primarily involved in cell-to-extracellular matrix adhesion, connecting the cell to the surrounding matrix, not directly mediating calcium-dependent cell-to-cell adhesion between epithelial cells.
- They can be affected by intracellular calcium signaling but do not directly bind calcium to mediate their adhesive function in the same way cadherins do.
*Claudin*
- **Claudins** are key components of **tight junctions**, which regulate paracellular permeability and form a barrier between cells, but they are not directly responsible for calcium-dependent cell-to-cell adhesion, which is characteristic of adherens junctions.
- While tight junctions contribute to overall cell-cell contact, the observation of an *increased gap* suggests an issue with adhesive complexes like adherens junctions, where cadherins are prominent.
*Cytokeratin*
- **Cytokeratins** are intermediate filaments found in epithelial cells, providing structural support and mechanical strength.
- They are linked to desmosomes and hemidesmosomes but are not directly involved in calcium-dependent cell-to-cell adhesion.
Reversible cell injury mechanisms US Medical PG Question 5: An investigator is studying muscle tissue in high-performance athletes. He obtains blood samples from athletes before and after a workout session consisting of short, fast sprints. Which of the following findings is most likely upon evaluation of blood obtained after the workout session?
- A. Decreased concentration of NADH
- B. Increased concentration of H+ (Correct Answer)
- C. Decreased concentration of lactate
- D. Increased concentration of insulin
- E. Increased concentration of ATP
Reversible cell injury mechanisms Explanation: ***Increased concentration of H+***
- During **anaerobic metabolism** in high-intensity exercise like sprints, pyruvate is converted to **lactate** by **lactate dehydrogenase** to regenerate NAD+. This process produces H+, leading to a decrease in pH and an increase in H+ concentration in the blood.
- The accumulation of **hydrogen ions (H+)** contributes to metabolic acidosis, muscle fatigue, and the burning sensation experienced during intense exertion.
- Blood gas analysis would show **decreased pH** and **increased H+ concentration**.
*Decreased concentration of NADH*
- NADH is primarily an **intracellular metabolite** and is not typically measured in blood samples as it does not circulate freely in significant concentrations.
- Within muscle cells during anaerobic glycolysis, NADH is consumed by lactate dehydrogenase to convert pyruvate to lactate, regenerating NAD+ for continued glycolysis.
- This option is not a realistic blood finding from a clinical laboratory perspective.
*Decreased concentration of lactate*
- **High-intensity sprints** primarily rely on **anaerobic metabolism**, which rapidly produces **lactate** from pyruvate.
- Therefore, the concentration of lactate in the blood would significantly **increase** after such a workout, not decrease.
- Elevated blood lactate is a hallmark finding after intense anaerobic exercise.
*Increased concentration of insulin*
- **Insulin** levels typically **decrease** during exercise, especially high-intensity exercise, due to **sympathetic nervous system activation** and the body's need to mobilize glucose from liver glycogen and fatty acids.
- Exercise promotes glucose uptake through **insulin-independent mechanisms** (GLUT4 translocation via AMP-activated protein kinase).
- Increased insulin would be counterproductive during intense exercise when glucose mobilization is needed.
*Increased concentration of ATP*
- ATP does not circulate in blood in measurable concentrations as a typical laboratory finding.
- Within muscle cells, ATP is rapidly **consumed** during intense exercise to fuel muscle contraction.
- While cells work to maintain ATP levels through anaerobic glycolysis and the creatine phosphate system, net ATP does not accumulate in the blood.
Reversible cell injury mechanisms US Medical PG Question 6: A 3-year-old female is found to have unusual susceptibility to infections by catalase-producing organisms. This patient likely has a problem with the function of which of the following cell types?
- A. Natural killer cells
- B. Eosinophils
- C. B cells
- D. T cells
- E. Neutrophils (Correct Answer)
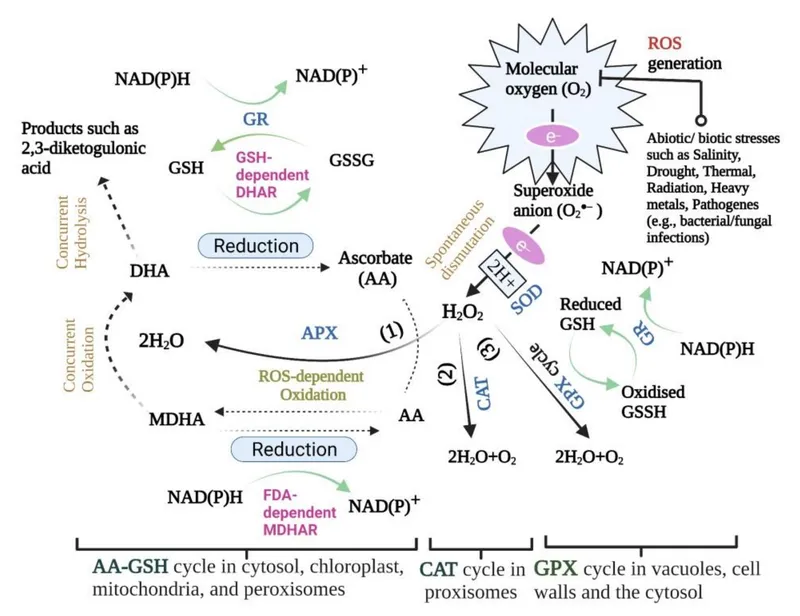
Reversible cell injury mechanisms Explanation: ***Neutrophils***
- Catalase-producing organisms, such as *Staphylococcus aureus* or *Aspergillus*, are typically cleared by **phagocytic cells**, specifically **neutrophils**, which use the **respiratory burst** to produce reactive oxygen species.
- A defect in neutrophil function, particularly in the **NADPH oxidase enzyme complex** responsible for the respiratory burst, leads to **chronic granulomatous disease (CGD)**, characterized by increased susceptibility to infections by these specific pathogens.
*Natural killer cells*
- **Natural killer (NK) cells** are primarily involved in the anti-viral and anti-tumor immune responses, recognizing and **killing infected or malignant cells**.
- They do not play a primary role in clearing bacterial or fungal infections, especially those caused by catalase-producing organisms.
*Eosinophils*
- **Eosinophils** are primarily involved in defense against **parasitic infections** and in mediating **allergic reactions**.
- Their role in clearing common bacterial or fungal infections is limited.
*B cells*
- **B cells** are responsible for **humoral immunity**, producing **antibodies** that neutralize pathogens and toxins or opsonize them for phagocytosis.
- While antibodies can aid in the clearance of many pathogens, a primary deficiency in B cell function (e.g., agammaglobulinemia) would lead to broad susceptibility to encapsulated bacteria, not specifically catalase-positive organisms.
*T cells*
- **T cells** are central to **cell-mediated immunity**, recognizing and eliminating intracellular pathogens or directly killing infected cells.
- Deficiencies in T cell function (e.g., SCID) lead to severe immunodeficiency with susceptibility to opportunistic infections, but do not specifically point to problems with catalase-producing organisms as the hallmark.
Reversible cell injury mechanisms US Medical PG Question 7: A neurophysiology expert is teaching his students the physiology of the neuromuscular junction. While describing the sequence of events that takes place at the neuromuscular junction, he mentions that as the action potential travels down the motor neuron, it causes depolarization of the presynaptic membrane. This results in the opening of voltage-gated calcium channels, which leads to an influx of calcium into the synapse of the motor neuron. Consequently, the cytosolic concentration of Ca2+ ions increases. Which of the following occurs at the neuromuscular junction as a result of this increase in cytosolic Ca2+?
- A. Generation of an end plate potential
- B. Exocytosis of acetylcholine from the synaptic vesicles (Correct Answer)
- C. Increased Na+ and K+ conductance of the motor end plate
- D. Binding of Ca2+ ions to NM receptors
- E. Release of Ca2+ ions into the synaptic cleft
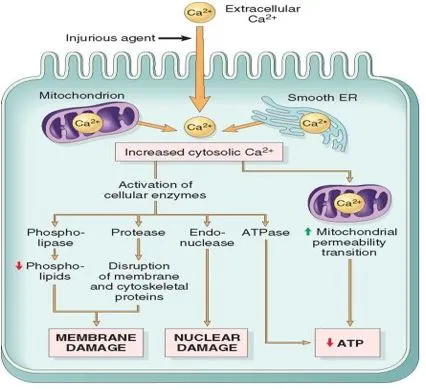
Reversible cell injury mechanisms Explanation: ***Exocytosis of acetylcholine from the synaptic vesicles***
- The increase in **cytosolic Ca2+** within the presynaptic terminal is the primary trigger for the fusion of **synaptic vesicles** filled with **acetylcholine (ACh)** with the presynaptic membrane.
- This fusion process, known as **exocytosis**, releases ACh into the **synaptic cleft**, initiating synaptic transmission.
*Generation of an end plate potential*
- The **end plate potential (EPP)** is generated *after* acetylcholine (ACh) is released into the synaptic cleft and binds to receptors on the motor end plate.
- This event occurs *following* the Ca2+-induced release of neurotransmitter, not as a direct result of the Ca2+ increase itself.
*Increased Na+ and K+ conductance of the motor end plate*
- Increased **Na+ and K+ conductance** across the motor end plate membrane is a direct consequence of acetylcholine binding to its receptors, which are **ligand-gated ion channels**.
- This change in conductance *generates the end plate potential*, occurring after ACh release.
*Binding of Ca2+ ions to NM receptors*
- **NM receptors** (nicotinic muscle receptors) are located on the **postsynaptic membrane** (motor end plate) and bind to **acetylcholine (ACh)**, not Ca2+ ions.
- Calcium's primary role in this context is presynaptic: triggering ACh release.
*Release of Ca2+ ions into the synaptic cleft*
- Calcium ions enter the **presynaptic terminal** from the synaptic cleft, and their increased cytosolic concentration within the presynaptic terminal drives neurotransmitter release.
- Calcium itself is not released *into* the synaptic cleft in this process; rather, it enters the presynaptic neuron from the cleft.
Reversible cell injury mechanisms US Medical PG Question 8: An 87-year-old woman is admitted to the intensive care unit after a neighbor found her lying on the floor at her home. Her respirations are 13/min and shallow. Despite appropriate therapy, the patient dies. Gross examination of the brain at autopsy shows neovascularization and liquefactive necrosis without cavitation in the distribution of the left middle cerebral artery. Histological examination of a brain tissue sample from the left temporal lobe shows proliferation of neural cells that stain positive for glial fibrillary acidic protein. Based on these findings, approximately how much time has most likely passed since the initial injury in this patient?
- A. 2 days
- B. 2 hours
- C. 10 days (Correct Answer)
- D. 25 days
- E. 12 hours
Reversible cell injury mechanisms Explanation: ***10 days***
- **Neovascularization** and the absence of cavitation with **liquefactive necrosis** are indicative of a subacute phase of ischemic injury, typically seen around 1-3 weeks.
- The proliferation of **glial fibrillary acidic protein (GFAP)** positive neural cells (astrocytes) signifies **astrogliosis**, a repair response common after approximately one week, peaking around 2-3 weeks post-injury.
*2 days*
- At 2 days, the primary histological findings would be **neutrophilic infiltration** and initial stages of neuronal necrosis.
- **Neovascularization** and significant astrogliosis are generally not prominent until later in the recovery phase.
*2 hours*
- Within 2 hours, there would be minimal to no gross changes, and microscopic examination might show only **red neurons** (eosinophilic neurons with pyknotic nuclei) reflecting early irreversible neuronal damage.
- There would be no signs of inflammation, tissue breakdown, or repair processes like neovascularization or astrogliosis.
*25 days*
- By 25 days (approximately 3-4 weeks), **cavitation** with a **cystic astrocytic glial scar** would likely be prominent at the site of liquefactive necrosis, which is explicitly stated as absent in the question.
- While astrogliosis would still be present, the lack of cavitation points to an earlier stage of repair.
*12 hours*
- At 12 hours, gross changes are typically still absent or subtle, and microscopic findings would primarily involve **edema** and early signs of neuronal injury (e.g., changes in Nissl bodies, mild eosinophilia).
- Inflammatory cell infiltration and reparative processes like neovascularization or astrogliosis would not yet be significant.
Reversible cell injury mechanisms US Medical PG Question 9: A 21-year-old medical student is studying different types of necrosis and tissue injuries. In the pathology laboratory, he observes different dead tissues under the microscope and notices the changes that are occurring as a function of time. After serial observations, he deduced that coagulation necrosis is...?
- A. The result of denaturation of glucose
- B. Characterized by the preservation of cellular shape (Correct Answer)
- C. Characteristic of brain ischemia
- D. Commonly associated with acute pancreatic necrosis
- E. The result of hydrolytic enzymes
Reversible cell injury mechanisms Explanation: ***Characterized by the preservation of cellular shape***
* **Coagulation necrosis** results from **protein denaturation**, which prevents the breakdown of the cell's structural proteins and enzymes.
* This preserves the **outline of the cell** and tissue architecture for a period of time, even after cell death, giving it a ghost-like appearance.
*The result of denaturation of glucose*
* **Glucose** is a simple sugar and does not undergo denaturation in the context of necrosis; rather, **proteins** are denatured.
* Denaturation refers to the disruption of the three-dimensional structure of proteins, not carbohydrates.
*Characteristic of brain ischemia*
* **Brain ischemia** typically results in **liquefactive necrosis**, not coagulation necrosis.
* This is due to the brain's high lipid content and the abundance of hydrolytic enzymes that rapidly digest the tissue.
*Commonly associated with acute pancreatic necrosis*
* **Acute pancreatitis** is primarily associated with **fat necrosis** (due to lipase activity) and **hemorrhagic necrosis**, not classic coagulation necrosis.
* The release of activated pancreatic enzymes leads to the digestion of local adipose tissue and blood vessels.
*The result of hydrolytic enzymes*
* While hydrolytic enzymes are involved in various forms of necrosis, **coagulation necrosis** is characterized by the **denaturation of structural proteins and enzymes**, which initially inhibits their proteolytic activity.
* **Liquefactive necrosis**, conversely, is largely driven by the release of powerful hydrolytic enzymes.
Reversible cell injury mechanisms US Medical PG Question 10: An 84-year-old man is brought to the physician by the staff of a group home where he resides because of worsening confusion and decreased urinary output. His nurse reports that the patient has not been drinking much for the last 3 days. Examination shows a decreased skin turgor and dry oral mucosa. His pulse is 105/min and blood pressure is 100/65 mm Hg. His serum creatinine is 3.1 mg/dL and a urea nitrogen is 42 mg/dL. Urine studies show multiple brownish granular casts. Which of the following processes is most likely involved in the pathogenesis of this patient's condition?
- A. Immune complex deposition in mesangium
- B. Leukocytic infiltration of renal interstitium
- C. Necrosis of renal papillae
- D. Necrosis of tubular epithelial cells (Correct Answer)
- E. Disruption of glomerular podocytes
Reversible cell injury mechanisms Explanation: ***Necrosis of tubular epithelial cells***
- The patient presents with classic signs of **acute kidney injury (AKI)**, including confusion, decreased urinary output, decreased skin turgor, dry oral mucosa, tachycardia, hypotension, elevated creatinine (3.1 mg/dL), and urea nitrogen (42 mg/dL).
- The presence of **brownish granular casts** in the urine is highly suggestive of **acute tubular necrosis (ATN)**, secondary to ischemia caused by severe dehydration and hypoperfusion.
*Immune complex deposition in mesangium*
- This typically points to a **glomerular pathology**, such as IgA nephropathy or post-infectious glomerulonephritis.
- These conditions would usually present with **hematuria** and **proteinuria**, not necessarily brownish granular casts or the acute dehydration found here.
*Leukocytic infiltration of renal interstitium*
- This finding is characteristic of **acute interstitial nephritis**, which is often caused by drug hypersensitivity or infection.
- The clinical presentation with dehydration and granular casts is not typical for acute interstitial nephritis.
*Necrosis of renal papillae*
- **Renal papillary necrosis** is often associated with analgesic abuse, sickle cell disease, diabetes, or obstruction.
- While it can cause AKI, it typically presents with **flank pain** and **hematuria**, and the urine sediment would show ghost cells or fragments of necrotic papillae, not specifically brownish granular casts.
*Disruption of glomerular podocytes*
- **Podocyte disruption** is seen in primary glomerular diseases like minimal change disease or focal segmental glomerulosclerosis.
- These conditions primarily cause **nephrotic syndrome** (heavy proteinuria, edema), which is not the main presentation here.
More Reversible cell injury mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.