Pathologic calcification US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pathologic calcification. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pathologic calcification US Medical PG Question 1: A 57-year-old man comes to the emergency department for the evaluation of worsening fatigue, urinary frequency, and constipation over the past 5 days. He was recently diagnosed with metastatic bladder cancer and is currently awaiting treatment. He has smoked 1 pack of cigarettes daily for 35 years. Physical examination shows dry mucous membranes and diffuse abdominal tenderness. An ECG shows a shortened QT interval. Which of the following sets of serum findings is most likely in this patient?
$$$ Calcium %%% Phosphorus %%% Parathyroid hormone %%% 1,25-dihydroxyvitamin D $$$
- A. ↑ ↓ ↓ ↓ (Correct Answer)
- B. ↑ ↑ ↓ ↑
- C. ↑ ↑ ↑ ↓
- D. ↑ ↓ ↑ ↑
- E. ↓ ↑ ↑ ↓
Pathologic calcification Explanation: ***↑ ↓ ↓ ↓***
- This pattern of **elevated calcium**, **low phosphorus**, **low parathyroid hormone (PTH)**, and **low 1,25-dihydroxyvitamin D** is characteristic of **humoral hypercalcemia of malignancy (HHM)**. Malignant cells, particularly those from bladder cancer, can secrete **parathyroid hormone-related peptide (PTHrP)**, mimicking PTH, leading to increased bone resorption and renal calcium reabsorption, while suppressing endogenous PTH and indirectly leading to low 1,25-dihydroxyvitamin D synthesis.
- The patient's symptoms of fatigue, constipation, urinary frequency, and signs like dry mucous membranes and a shortened QT interval on ECG are all consistent with **hypercalcemia**.
*↑ ↑ ↓ ↑*
- This pattern suggests **hypercalcemia** with **elevated phosphorus** and **elevated 1,25-dihydroxyvitamin D**, which is inconsistent with HHM. Elevated phosphorus is more commonly seen in conditions like **renal failure** or **tumor lysis syndrome**, neither of which are indicated here.
- Elevated 1,25-dihydroxyvitamin D is typically seen in **granulomatous diseases** (e.g., sarcoidosis) or **lymphomas** causing hypercalcemia, not bladder carcinoma.
*↑ ↑ ↑ ↓*
- This profile indicates **hypercalcemia**, **elevated phosphorus**, and **elevated PTH**, which is consistent with **primary hyperparathyroidism**. However, primary hyperparathyroidism typically presents with inappropriately elevated PTH for the level of hypercalcemia, and it's less likely to develop acute, severe hypercalcemia with malignancy unless concurrent.
- The patient's presentation with advanced bladder cancer makes HHM a more likely cause of hypercalcemia than primary hyperparathyroidism.
*↑ ↓ ↑ ↑*
- This constellation, with **elevated calcium**, **low phosphorus**, and **elevated PTH**, is classic for **primary hyperparathyroidism**. In this condition, inappropriately high PTH levels cause increased bone resorption, renal calcium reabsorption, and renal phosphate excretion, leading to hypophosphatemia.
- While primary hyperparathyroidism causes hypercalcemia, the clinical context of advanced metastatic bladder cancer makes HHM a much more probable diagnosis in this patient, and PTH would be suppressed in HHM due to PTHrP mimicking its effects.
*↓ ↑ ↑ ↓*
- This pattern describes **hypocalcemia** (low calcium) with **elevated phosphorus** and **elevated PTH**. This is the hallmark of **secondary hyperparathyroidism**, often seen in **chronic kidney disease**, where low calcium and high phosphorus stimulate PTH release.
- The patient in the vignette presents with symptoms of hypercalcemia, not hypocalcemia, making this option inconsistent with the clinical picture.
Pathologic calcification US Medical PG Question 2: A 17-year-old boy comes to the physician for a follow-up examination. Two months ago, he suffered a spinal fracture after a fall from the roof. He feels well. His father has multiple endocrine neoplasia type 1. Vital signs are within normal limits. Examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.7 g/dL
Serum
Creatinine 0.7 mg/dL
Proteins
Total 7.0 g/dL
Albumin 4.1 g/dL
Calcium 11.4 mg/dL
Phosphorus 5.3 mg/dL
Alkaline phosphatase 100 U/L
Which of the following is the most likely cause of these findings?
- A. Immobilization (Correct Answer)
- B. Parathyroid adenoma
- C. Paraneoplastic syndrome
- D. Sarcoidosis
- E. Pseudohypercalcemia
Pathologic calcification Explanation: ***Immobilization***
- Prolonged **immobilization**, especially after a spinal fracture, leads to **bone resorption**, releasing calcium and phosphorus into the bloodstream, causing **hypercalcemia** and **hyperphosphatemia**.
- Though calcium and phosphorus are elevated, the **alkaline phosphatase** is normal, which is consistent with immobilization-induced bone resorption rather than primary bone disease.
*Parathyroid adenoma*
- A **parathyroid adenoma** causes primary **hyperparathyroidism**, characterized by **hypercalcemia** and **hypophosphatemia** (due to increased renal phosphate excretion), which contradicts the elevated phosphorus level seen here.
- Although the father has MEN1, a personal history of parathyroid adenoma is not indicated by the lab results.
*Paraneoplastic syndrome*
- **Paraneoplastic syndrome** causing hypercalcemia is typically due to ectopic production of **parathyroid hormone-related peptide (PTHrP)**, leading to **hypercalcemia** with **low PTH** and generally **low phosphorus** levels.
- This condition most commonly occurs with malignancies, such as squamous cell carcinoma, which is not indicated in this healthy-appearing young man with a recent fracture.
*Sarcoidosis*
- **Sarcoidosis** causes hypercalcemia due to increased synthesis of **1,25-dihydroxyvitamin D** by activated macrophages, leading to increased intestinal calcium absorption.
- This typically results in **hypercalcemia** with **normal or low PTH** and **normal or low phosphorus** levels; it is not associated with elevated phosphorus.
*Pseudohypercalcemia*
- **Pseudohypercalcemia** is an artifactual elevation of total calcium, usually due to **severe dehydration** or **elevated protein** levels, particularly **albumin** or **immunoglobulins**.
- In this case, the albumin and total protein levels are within the normal range, making pseudohypercalcemia unlikely.
Pathologic calcification US Medical PG Question 3: A 37-year-old female presents to her primary care physician with constipation and abdominal pain. She notes that the pain has been present for several days and is not related to food. She also reports increased urinary frequency without incontinence, as well as increased thirst. She takes no medications, but notes taking vitamin supplements daily. Her vital signs are: BP 130/72 mmHg, HR 82 bpm, T 97.0 degrees F, and RR 12 bpm. Lab studies reveal: Na 139, K 4.1, Cl 104, HCO3 25, Cr 0.9, and Ca 12.4. Further studies show an increased ionized calcium, decreased PTH, and normal phosphate. What is the most likely cause of this patient's symptoms?
- A. Vitamin overdose (Correct Answer)
- B. Vitamin deficiency
- C. Inherited disorder
- D. Plasma cell neoplasm
- E. Primary endocrine dysfunction
Pathologic calcification Explanation: ***Vitamin overdose***
- The patient's symptoms of **constipation**, **abdominal pain**, **increased urinary frequency**, and **thirst** are classic signs of **hypercalcemia**.
- The lab findings of **hypercalcemia (Ca 12.4)**, **increased ionized calcium**, **decreased PTH**, and increased phosphate, coupled with a history of daily vitamin supplements, strongly suggest **Vitamin D toxicity** from overdose, which leads to increased calcium absorption and bone resorption.
*Vitamin deficiency*
- Vitamin deficiencies typically do not cause **hypercalcemia**; in fact, severe **Vitamin D deficiency** can lead to **hypocalcemia** and **secondary hyperparathyroidism**.
- Symptoms associated with common vitamin deficiencies (e.g., scurvy, rickets) are not consistent with this patient's presentation.
*Inherited disorder*
- While some **inherited disorders** (e.g., **Familial Hypocalciuric Hypercalcemia**) can cause hypercalcemia, the distinguishing feature is typically a **normal or mildly elevated PTH** and **low urinary calcium excretion**, which is not entirely aligned with the presented PTH and phosphate levels and the acute onset suggested by symptoms.
- The patient's history of **vitamin supplement** use provides a more direct and likely explanation for acute hypercalcemia.
*Plasma cell neoplasm*
- **Plasma cell neoplasms** like **multiple myeloma** can cause **hypercalcemia** due to increased bone resorption from osteoclast-activating factors.
- However, hypercalcemia from these conditions is often accompanied by other signs of malignancy such as **renal failure**, **anemia**, or **bone lesions**, which are not reported in this case, and the **decreased PTH** points away from malignancy-associated humorally mediated hypercalcemia.
*Primary endocrine dysfunction*
- **Primary hyperparathyroidism** is a common cause of **hypercalcemia**, but it is characterized by **elevated or inappropriately normal PTH levels** in the presence of hypercalcemia, which contradicts the **decreased PTH** found in this patient.
- Other endocrine causes of hypercalcemia, such as **thyrotoxicosis** or **adrenal insufficiency**, present with distinct clinical features not described here.
Pathologic calcification US Medical PG Question 4: A 28-year-old African American woman presents to her primary care physician with two weeks of nausea, abdominal pain, and increased urination. She states she has had kidney stones in the past and is concerned because her current pain is different in character from what she had experienced then. In addition she reports increasing weakness and fatigue over the past several months as well as mild shortness of breath. Chest radiography shows bilateral hilar adenopathy. Which of the following processes is most likely responsible for her current symptoms?
- A. Osteoclast-driven bone resorption
- B. Increased intestinal absorption of calcium (Correct Answer)
- C. Ectopic parathyroid hormone release
- D. Increased production of parathyroid hormone
- E. Increased renal calcium reabsorption
Pathologic calcification Explanation: ***Increased intestinal absorption of calcium***
- The constellation of symptoms including **bilateral hilar adenopathy**, chronic fatigue, weakness, and hypercalcemia symptoms (nausea, abdominal pain, increased urination) in an African American woman is highly suggestive of **sarcoidosis**.
- In sarcoidosis, activated macrophages within granulomas produce **1α-hydroxylase**, which converts **25-hydroxyvitamin D to 1,25-dihydroxyvitamin D (calcitriol)**, leading to increased intestinal absorption of calcium and subsequent hypercalcemia.
*Osteoclast-driven bone resorption*
- While hypercalcemia can result from increased osteoclast activity (e.g., in **malignancy** or **primary hyperparathyroidism**), sarcoidosis-associated hypercalcemia is primarily due to increased gut absorption of calcium.
- The patient's history does not strongly point to significant bone destructive processes that would be the primary cause of her hypercalcemia.
*Ectopic parathyroid hormone release*
- **Ectopic PTH release** is characteristic of certain malignancies, such as squamous cell carcinoma, leading to **hypercalcemia of malignancy**.
- This syndrome is typically associated with very high calcium levels and PTHrP (parathyroid hormone-related peptide) production, not the clinical picture of sarcoidosis.
*Increased production of parathyroid hormone*
- **Increased PTH production** (primary hyperparathyroidism) causes hypercalcemia by increasing bone resorption, renal calcium reabsorption, and renal production of calcitriol.
- Although some symptoms overlap, the presence of **bilateral hilar adenopathy** and the absence of clear evidence for a parathyroid adenoma makes this less likely than sarcoidosis.
*Increased renal calcium reabsorption*
- While increased renal calcium reabsorption contributes to hypercalcemia, in the context of sarcoidosis, it is a secondary effect due to the overall calcium imbalance, not the primary mechanism.
- The principal driver of hypercalcemia in this patient's likely condition is the **overproduction of active vitamin D** leading to increased intestinal absorption.
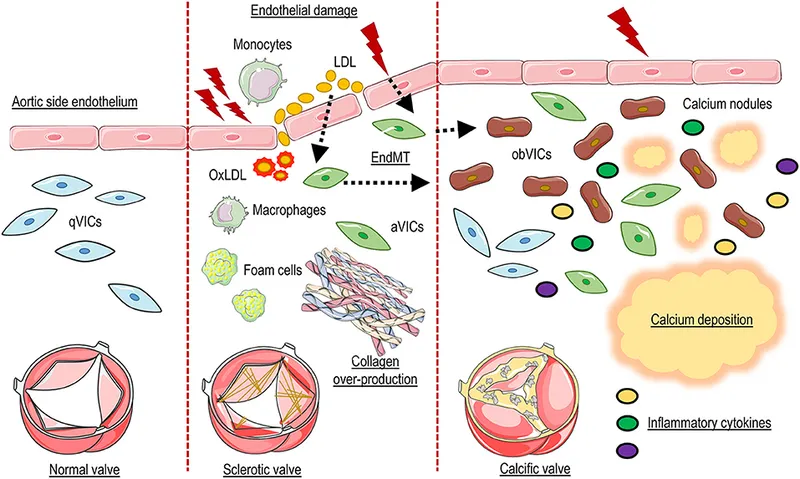
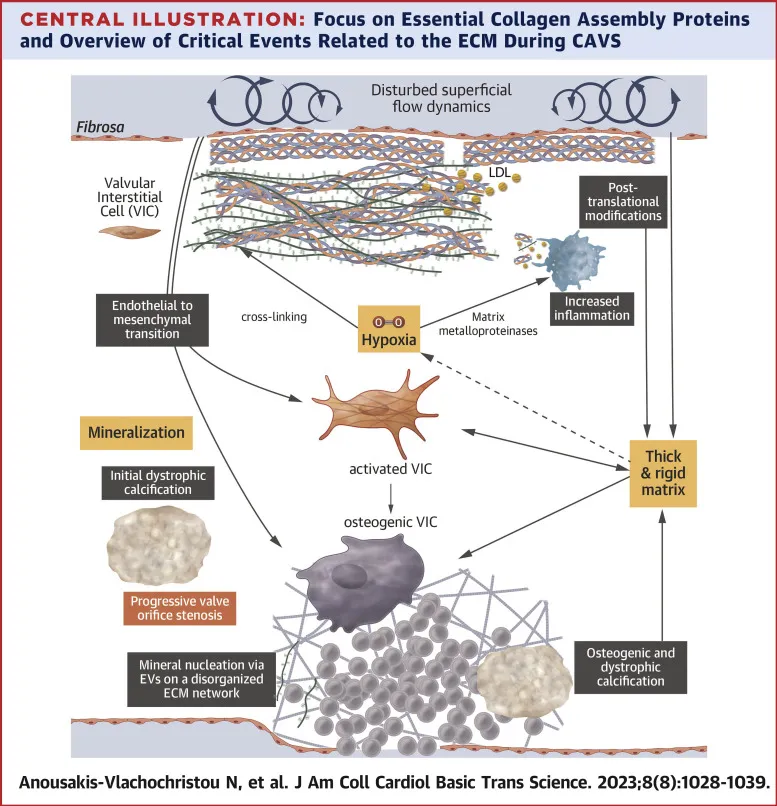
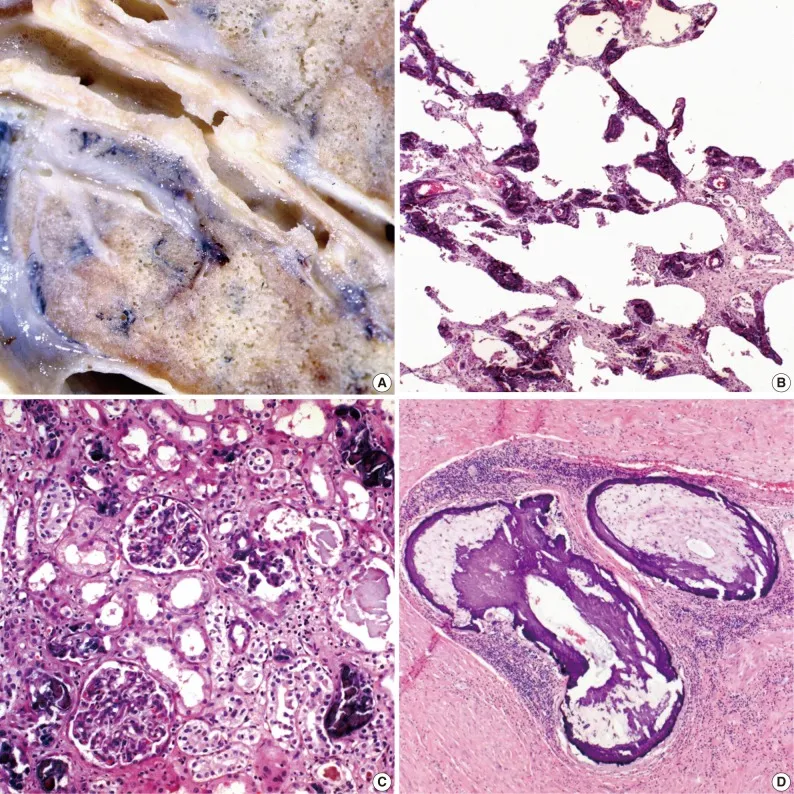
Pathologic calcification US Medical PG Question 5: A 72-year-old man who was involved in a traffic collision is brought to the emergency room by the ambulance service. He was in shock and comatose at the time of presentation. On examination, the heart rate is 60/min, and the blood pressure is 70/40 mm Hg. The patient dies, despite resuscitative efforts. Autopsy reveals multiple internal hemorrhages and other evidence of ischemic damage affecting the lungs, kidneys, and brain. The patient’s heart shows evidence of gross anomaly similar to the picture. While acute hypovolemia is the likely cause of the ischemic changes seen in the lungs, kidneys, and brain, which of the following best explains the gross anomaly of his heart?
- A. Senile calcific aortic stenosis (Correct Answer)
- B. Accumulation of amyloid in the myocardium
- C. Mitral valve stenosis
- D. Hypertrophic cardiomyopathy
- E. Aortic valve regurgitation
Pathologic calcification Explanation: ***Senile calcific aortic stenosis***
- The patient's age (72 years) makes **senile calcific aortic stenosis** a very likely finding, as it is a degenerative condition common in the elderly leading to stiffening and calcification of the aortic valve.
- While the immediate cause of death was **hypovolemic shock**, the presence of an underlying **cardiac anomaly** could worsen the patient's ability to compensate for significant blood loss, contributing to the rapid decompensation observed.
- Gross pathology typically shows **calcified, thickened aortic valve leaflets** that are stenotic.
*Accumulation of amyloid in the myocardium*
- While **cardiac amyloidosis** can occur in the elderly and cause restrictive cardiomyopathy, it typically presents with **heart failure symptoms** and often results in thickened ventricular walls, which is not specifically indicated as the "gross anomaly" in this context.
- The sudden, acute decompensation due to trauma does not align as strongly with the chronic progression of amyloidosis as it does with a structural valvular issue exacerbated by shock.
*Mitral valve stenosis*
- **Mitral valve stenosis** is more often associated with **rheumatic heart disease** or congenital anomalies, which are less common in this age group as a primary, sudden anomaly.
- While it can lead to heart failure, the description of a "gross anomaly" in the context of acute decompensation and the patient's age points more towards a common degenerative valvular condition like aortic stenosis.
*Hypertrophic cardiomyopathy*
- **Hypertrophic cardiomyopathy (HCM)** is a genetic condition that typically presents earlier in life with symptoms of outflow obstruction or sudden cardiac death in young athletes.
- While HCM can present in older adults, the gross pathology shows **asymmetric septal hypertrophy** rather than valvular pathology.
- In a 72-year-old, age-related degenerative valve disease is more common than first presentation of genetic cardiomyopathy.
*Aortic valve regurgitation*
- Although **aortic regurgitation** can lead to cardiac remodeling and failure, it is less likely to be referred to simply as a "gross anomaly" in this context without more specific valvular description.
- **Senile calcific aortic stenosis** is a more common degenerative anomaly in this age group, and the question implies a common, age-related finding.
Pathologic calcification US Medical PG Question 6: A 65-year-old man comes to the physician for evaluation of a neck mass and weight loss. He first noticed the growing mass 2 months ago. The mass is not painful. He also has decreased appetite and intermittent abdominal pain. He has lost 10 kg (22 lb) of weight over the past 3 months. Sometimes, he wakes up in the morning drenched in sweat. He takes daily over-the-counter multivitamins. He appears pale. His pulse is 65/min, blood pressure is 110/70 mm Hg, and temperature is 38.1°C (100.6°F). Physical exam shows a painless, golf ball-sized mass in the anterior triangle of the neck. A biopsy shows large cells with a bilobed nucleus that are CD15-positive and CD30-positive. Laboratory analysis of serum shows a calcium level of 14.5 mg/dL and a parathyroid hormone level of 40 pg/mL. Which of the following is the most likely explanation of this patient's laboratory findings?
- A. Ectopic vitamin D production
- B. Osteolytic metastasis
- C. Ectopic PTH-related protein production (Correct Answer)
- D. Multivitamin overdose
- E. Osteoblastic metastasis
Pathologic calcification Explanation: ***Ectopic PTH-related protein production***
- The patient's symptoms (neck mass, weight loss, night sweats, fever) and biopsy findings (CD15+ and CD30+ large cells with bilobed nucleus) are highly suggestive of **Hodgkin lymphoma** with classic Reed-Sternberg cells.
- **Hypercalcemia (14.5 mg/dL)** with **inappropriately normal PTH (40 pg/mL)** in the context of malignancy points to **humoral hypercalcemia of malignancy (HHM)**, mediated by **PTH-related protein (PTHrP)** produced ectopically by tumor cells.
- PTH should be suppressed (<20 pg/mL) in the setting of hypercalcemia, so a level of 40 pg/mL indicates autonomous calcium elevation from a non-PTH source.
*Ectopic vitamin D production*
- While some lymphomas can produce **1,25-dihydroxyvitamin D** (through activated macrophages), leading to hypercalcemia, this would also cause **suppressed PTH**.
- This mechanism occurs in Hodgkin lymphoma but is less common than PTHrP-mediated hypercalcemia in most cases of malignancy-associated hypercalcemia.
*Osteolytic metastasis*
- **Osteolytic metastases** (e.g., from multiple myeloma or breast cancer) can cause hypercalcemia by directly destroying bone and releasing calcium.
- The biopsy is consistent with Hodgkin lymphoma, not a solid tumor that typically produces purely lytic bone metastases.
- While Hodgkin lymphoma can involve bone, systemic hypercalcemia due to direct bone destruction is less common than HHM through PTHrP.
*Multivitamin overdose*
- Overdosing on multivitamins could potentially lead to **vitamin D toxicity** and hypercalcemia if the supplements contained extremely high doses of vitamin D.
- However, the patient's symptoms, neck mass, fever, and biopsy findings clearly indicate a malignancy (Hodgkin lymphoma), making multivitamin overdose an unlikely cause of his profound hypercalcemia.
*Osteoblastic metastasis*
- **Osteoblastic metastases** (e.g., from prostate cancer) stimulate new bone formation and typically cause **elevated alkaline phosphatase** with normal or slightly elevated calcium, not profound hypercalcemia.
- Furthermore, the biopsy findings (Reed-Sternberg cells) are not consistent with a tumor type that causes osteoblastic metastases.
Pathologic calcification US Medical PG Question 7: An 11-year-old male is brought in by ambulance to the emergency department after being a restrained passenger in a motor vehicle accident. His father was driving him to soccer practice when they were hit by a wrong way driver. On presentation, his temperature is 101°F (38.3°C), blood pressure is 100/62 mmHg, pulse is 108/min, and respirations are 21/min. He is found to be agitated and complains of nausea, severe epigastric pain, and lower extremity pain. Physical exam reveals lacerations and ecchymosis on his left forehead, right flank, and lower extremities. Radiographs demonstrate an open book fracture of the pelvis as well as bilateral femur fractures. Despite multiple interventions, his condition deteriorates and he passes away from his injuries. Post-mortem pathologic examination of abdominal tissues reveals white deposits containing calcium. Abnormal activity of which of the following proteins is most likely responsible for these deposits?
- A. Proteases
- B. Plasmin
- C. Thrombin
- D. Lipases (Correct Answer)
- E. Immunoglobulin
Pathologic calcification Explanation: ***Lipases***
- The patient's presentation with **severe epigastric pain**, **agitation**, and **fever** following massive trauma suggests **acute pancreatitis**, which can result from blunt abdominal injury.
- In acute pancreatitis, activated **lipases** degrade adipocytes, leading to the release of fatty acids that combine with calcium to form **calcium soaps**, appearing as white, chalky deposits in the abdominal tissues.
*Proteases*
- While proteases are also involved in the pathogenesis of acute pancreatitis, their primary role is the **breakdown of proteins** and cell membranes, contributing to tissue destruction.
- They do not directly cause the characteristic **white, calcium-containing deposits** observed in fat necrosis.
*Plasmin*
- **Plasmin** is a key enzyme in the **fibrinolytic system**, responsible for dissolving blood clots.
- While trauma can activate coagulation and fibrinolysis, plasmin's activity is not directly linked to the formation of **calcium deposits** in fat necrosis.
*Thrombin*
- **Thrombin** is a central enzyme in the **coagulation cascade**, converting fibrinogen to fibrin, leading to clot formation.
- Its primary role is in **hemostasis**, and it is not directly responsible for the development of **calcium soaps** in adipose tissue necrosis.
*Immunoglobulin*
- **Immunoglobulins** (antibodies) are part of the immune system, involved in recognizing and neutralizing pathogens or foreign substances.
- They are not directly involved in the enzymatic processes that lead to **fat necrosis** and **calcium deposition** in the context of acute pancreatitis.
Pathologic calcification US Medical PG Question 8: A 13-year-old girl is brought to the outpatient clinic by her parents with a complaint of episodic spasm in her fingers for the past few months. Upon further questioning, her mother notes that the girl has not been doing well at school. She also believes that the girl is shorter than the other children in her class. On examination, her pulse is 72/min, temperature 37.6°C (99.7°F), respiratory rate 16/min, and blood pressure 120/88 mm Hg. The girl has short 4th and 5th fingers on both hands, a round face, and discolored teeth. Her height is 135 cm (4 ft 5 in) and she weighs 60 kg (132 lb). Investigation reports show the following values:
Hemoglobin (Hb%) 12.5 g/dL
White blood cell total count 10,000/mm3
Platelets 260,000/mm3
Calcium, serum (Ca2+) 4.0 mg/dL
Serum albumin 4.0 g/dL
Alanine aminotransferase (ALT), serum 15 U/L
Aspartate aminotransferase (AST), serum 8 U/L
Serum creatinine 0.5 mg/dL
Urea 27 mg/dL
Sodium 137 mEq/L
Potassium 4.5 mEq/L
Magnesium 2.5 mEq/L
Parathyroid hormone, serum, N-terminal 930 pg/mL (normal: 230-630 pg/mL)
Serum vitamin D 45 ng/dL
Which of the following is the mode of inheritance of the disease this patient has?
- A. X-linked recessive
- B. Mitochondrial inheritance
- C. X linked dominant
- D. Autosomal recessive
- E. Autosomal dominant (Correct Answer)
Pathologic calcification Explanation: ***Autosomal dominant***
- The clinical presentation with **short 4th and 5th fingers**, **round face**, **short stature** (height 135 cm, which is below average for a 13-year-old girl), **hypocalcemia** (4.0 mg/dL), and **elevated PTH** (930 pg/mL) is characteristic of **pseudohypoparathyroidism (PHP)**, specifically **Albright hereditary osteodystrophy (AHO)**.
- PHP type 1A (AHO) is typically inherited in an **autosomal dominant** pattern, often due to mutations in the **GNAS gene**.
*X-linked recessive*
- This mode of inheritance primarily affects males, with females usually being asymptomatic carriers. The patient is a female, making X-linked recessive less likely for a symptomatic presentation like this.
- Conditions like **Duchenne muscular dystrophy** or **fragile X syndrome** are X-linked recessive and have different clinical features.
*Mitochondrial inheritance*
- This inheritance pattern involves genes located in the mitochondria and is passed down from the mother to all her children; however, the clinical picture here does not align with typical mitochondrial disorders such as **MELAS syndrome** or **Leber's hereditary optic neuropathy**.
- Mitochondrial disorders often present with neurological or muscular symptoms that are progressive and distinct from the endocrine and skeletal features seen in this patient.
*X linked dominant*
- X-linked dominant inheritance would typically cause affected fathers to pass the trait to all their daughters, but not to their sons. Affected mothers have a 50% chance of passing it to each child. While females can be affected, the specific constellation of symptoms (PHP type 1A with AHO features) does not primarily follow an X-linked dominant pattern.
- Examples include **Rett syndrome** and **vitamin D-resistant rickets**, which have different clinical manifestations.
*Autosomal recessive*
- Autosomal recessive conditions require two copies of a mutated gene for the disease to manifest, meaning both parents are usually carriers. This mode of inheritance is seen in conditions like **cystic fibrosis** or **sickle cell anemia**, which have distinct presentations and are not consistent with the patient's symptoms of AHO and PHP.
- While some forms of hypoparathyroidism can be autosomal recessive, the classic features of AHO with brachydactyly and osteodystrophy strongly point away from autosomal recessive inheritance for this specific syndrome.
Pathologic calcification US Medical PG Question 9: A 32-year-old woman presents to her primary care physician for an annual checkup. She reports that she has been feeling well and has no medical concerns. Her past medical history is significant for childhood asthma but she has not experienced any symptoms since she was a teenager. Physical exam reveals a 1-centimeter hard mobile mass in the left upper outer quadrant of her breast. A mammogram was performed and demonstrated calcifications within the mass so a biopsy was obtained. The biopsy shows acinar proliferation with intralobular fibrosis. Which of the following conditions is most likely affecting this patient?
- A. Sclerosing adenosis (Correct Answer)
- B. Fibroadenoma
- C. Cystic hyperplasia
- D. Invasive lobular carcinoma
- E. Infiltrating ductal carcinoma
Pathologic calcification Explanation: ***Sclerosing adenosis***
- This condition is characterized by **acinar proliferation with intralobular fibrosis**, which exactly matches the biopsy findings mentioned in the vignette.
- Sclerosing adenosis can present as a palpable mass with **calcifications on mammography**, mimicking carcinoma, necessitating biopsy for definitive diagnosis.
*Fibroadenoma*
- Characterized by proliferation of both **stromal and epithelial elements**, often forming well-circumscribed, mobile masses.
- While it can present as a mobile mass, the specific histological finding of "acinar proliferation with intralobular fibrosis" is not the primary descriptive characteristic of a fibroadenoma.
*Cystic hyperplasia*
- This term, often used interchangeably with **fibrocystic changes**, involves the formation of cysts and an increase in fibrous tissue.
- While it can involve hyperplasia, it doesn't typically describe the distinct pattern of "acinar proliferation with intralobular fibrosis" as seen in sclerosing adenosis.
*Invasive lobular carcinoma*
- This carcinoma is characterized by its **infiltrative growth pattern** often in single file lines, and typically does not form a well-defined mass.
- While it can present with calcifications, the absence of overt malignant features and the specific benign histological description rule out this diagnosis.
*Infiltrating ductal carcinoma*
- The most common type of breast cancer, characterized by **malignant epithelial cells infiltrating the stroma**.
- The biopsy findings described ("acinar proliferation with intralobular fibrosis") are features of a benign process, not a malignant one.
Pathologic calcification US Medical PG Question 10: A 36-year-old man is admitted to the hospital because of a 1-day history of epigastric pain and vomiting. He has had similar episodes of epigastric pain in the past. He drinks 8 oz of vodka daily. Five days after admission, the patient develops aspiration pneumonia and sepsis. Despite appropriate therapy, the patient dies. At autopsy, the pancreas appears gray, enlarged, and nodular. Microscopic examination of the pancreas shows localized deposits of calcium. This finding is most similar to an adaptive change that can occur in which of the following conditions?
- A. Primary hyperparathyroidism
- B. Sarcoidosis
- C. Multiple myeloma
- D. Congenital CMV infection
- E. Chronic kidney disease (Correct Answer)
Pathologic calcification Explanation: ***Chronic kidney disease***
- The pancreatic finding represents **dystrophic calcification** (calcium deposition in damaged tissue with normal serum calcium levels), a consequence of chronic pancreatitis.
- **Chronic kidney disease** is the most similar condition because it also involves pathologic calcification as an adaptive/pathologic change, though through a different mechanism called **metastatic calcification**.
- In CKD, **hyperphosphatemia** and secondary **hyperparathyroidism** elevate the serum calcium-phosphate product, leading to calcium deposition in **normal tissues** (blood vessels, kidneys, lungs, gastric mucosa).
- Both conditions demonstrate **pathologic calcification as a tissue response** to metabolic derangement, making CKD the best answer among the options provided.
*Primary hyperparathyroidism*
- Causes **hypercalcemia** and **hypophosphatemia** due to excess PTH secretion.
- Can lead to **metastatic calcification** in normal tissues, but is less commonly associated with widespread tissue calcification compared to CKD.
- The mineral imbalance pattern differs from CKD (high calcium, low phosphate vs. high phosphate, variable calcium).
*Sarcoidosis*
- Causes **hypercalcemia** due to increased 1,25-dihydroxyvitamin D production by activated macrophages in granulomas.
- Can result in **metastatic calcification**, particularly nephrocalcinosis.
- However, this is less common and less extensive than the calcification seen in CKD.
*Multiple myeloma*
- Produces **hypercalcemia** through osteolytic bone destruction and cytokine-mediated bone resorption.
- Can theoretically cause **metastatic calcification**, but this is not a typical or prominent feature of the disease.
- The hypercalcemia is usually addressed before significant tissue calcification occurs.
*Congenital CMV infection*
- Causes **dystrophic calcification** in damaged tissues, typically **periventricular intracranial calcifications**.
- While this involves the same type of calcification (dystrophic), CMV infection is not characterized by systemic or progressive calcification as an adaptive metabolic response.
- The calcifications are focal sequelae of viral tissue damage, not a widespread metabolic derangement.
More Pathologic calcification US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.