Intracellular accumulations US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Intracellular accumulations. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Intracellular accumulations US Medical PG Question 1: A 45-year-old man comes to the physician for a routine health maintenance examination. He feels well. He has type 2 diabetes mellitus. There is no family history of serious illness. He works as an engineer at a local company. He does not smoke. He drinks one glass of red wine every other day. He does not use illicit drugs. His only medication is metformin. He is 180 cm (5 ft 11 in) tall and weighs 100 kg (220 lb); BMI is 31 kg/m2. His vital signs are within normal limits. Examination shows a soft, nontender abdomen. The liver is palpated 2 to 3 cm below the right costal margin. Laboratory studies show an aspartate aminotransferase concentration of 100 U/L and an alanine aminotransferase concentration of 130 U/L. Liver biopsy shows hepatocyte ballooning degeneration, as well as inflammatory infiltrates with scattered lymphocytes, neutrophils, and Kupffer cells. Which of the following is the most likely diagnosis?
- A. Nonalcoholic steatohepatitis (Correct Answer)
- B. Autoimmune hepatitis
- C. Viral hepatitis
- D. Primary biliary cholangitis
- E. Alcoholic fatty liver disease
Intracellular accumulations Explanation: ***Nonalcoholic steatohepatitis***
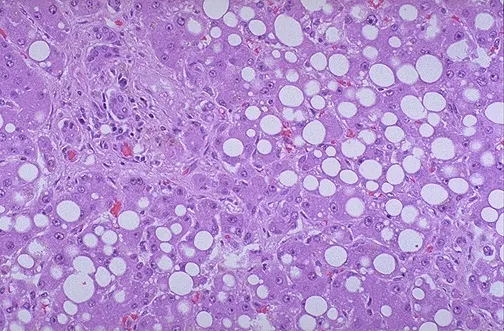
- The patient's **obesity (BMI 31)**, **type 2 diabetes mellitus**, and elevated liver enzymes (ALT > AST) in the absence of significant alcohol intake or other causes of liver disease are highly suggestive of **nonalcoholic fatty liver disease (NAFLD)**, with the biopsy findings of **hepatocyte ballooning degeneration** and **inflammatory infiltrates** confirming progression to **nonalcoholic steatohepatitis (NASH)**.
- **NASH** is a severe form of NAFLD characterized by **steatosis**, **inflammation**, and hepatocyte injury (ballooning degeneration), which can progress to cirrhosis and liver failure.
*Autoimmune hepatitis*
- This condition is typically characterized by high levels of **autoantibodies** (e.g., ANA, anti-smooth muscle antibodies), which are not mentioned and would be an important diagnostic clue.
- Although it can cause elevated transaminases and inflammatory infiltrates, the biopsy typically shows **interface hepatitis** and prominent plasma cell infiltrates, rather than significant steatosis and ballooning degeneration.
*Viral hepatitis*
- While viral hepatitis (e.g., hepatitis B or C) causes elevated transaminases and inflammatory changes, the biopsy findings of **hepatocyte ballooning** are not characteristic.
- The patient's presentation does not include risk factors or symptoms typically associated with acute or chronic viral hepatitis, and serological markers would be required for diagnosis.
*Primary biliary cholangitis*
- This is a chronic autoimmune cholestatic liver disease primarily affecting **interlobular bile ducts**, usually seen in middle-aged women.
- It is characterized by elevated **alkaline phosphatase** levels and positive **antimitochondrial antibodies (AMA)**, which are not described in this patient, and the biopsy would show granulomatous destruction of bile ducts.
*Alcoholic fatty liver disease*
- Although the biopsy findings of **steatosis**, **hepatocyte ballooning**, and **inflammation** can be seen in alcoholic liver disease, the patient's reported alcohol consumption of "one glass of red wine every other day" is well below the threshold for causing significant alcoholic liver damage.
- **Alcoholic hepatitis** typically involves an AST:ALT ratio of >2 and a history of heavy, prolonged alcohol use.
Intracellular accumulations US Medical PG Question 2: A 59-year-old woman with a history of chronic kidney disease comes to the physician for a 3-month history of easy fatiguability. Physical examination shows subconjunctival pallor. Her hemoglobin concentration is 8.9 g/dL, mean corpuscular volume is 86 μm3, and serum ferritin is 225 ng/mL. Treatment with erythropoietin is begun. A peripheral blood smear is obtained one week after treatment. A photomicrograph of the smear after specialized staining is shown. The prominent color of the intracellular structure in some of the cells is most likely the result of staining which of the following?
- A. Golgi apparatus
- B. Ribosomal RNA (Correct Answer)
- C. Remnants of the nucleus
- D. Denatured globin chains
- E. Mitochondria
Intracellular accumulations Explanation: ***Ribosomal RNA***
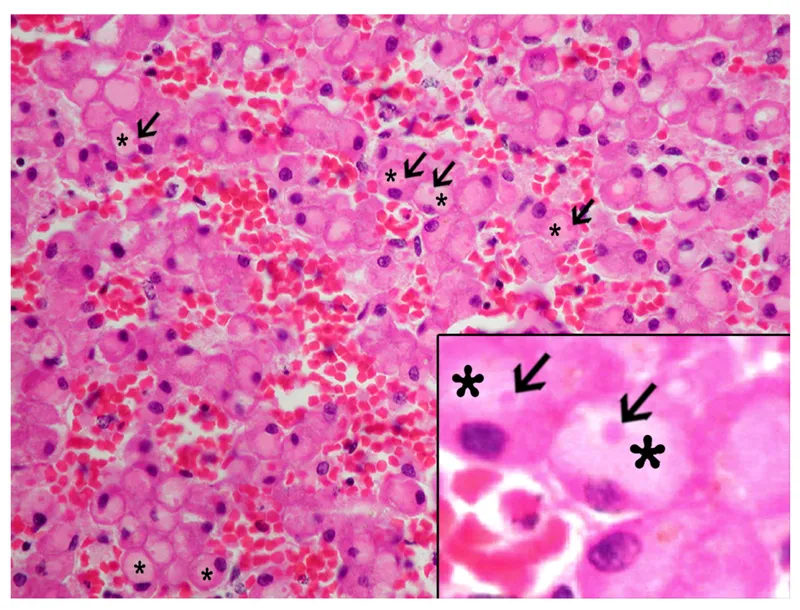
- The patient's presentation of **anemia** in the setting of chronic kidney disease and subsequent treatment with erythropoietin points to a likely increase in **reticulocytes** in the peripheral smear.
- The described prominent intracellular structures are characteristic of **reticulofilamentous material**, which is composed primarily of **RNA (ribosomal RNA)** that precipitates out with supravital stains like **new methylene blue**.
*Golgi apparatus*
- The **Golgi apparatus** is an organelle involved in modifying, sorting, and packaging proteins and lipids.
- It is not visible as prominent intracellular structures with **supravital stains** on a peripheral blood smear and does not contribute to reticulocyte staining.
*Remnants of the nucleus*
- While red blood cell precursors have a nucleus, mature erythrocytes and reticulocytes are **anucleated**.
- **Nuclear remnants** (e.g., Howell-Jolly bodies) are typically **DNA-containing fragments** appearing as dense, basophilic inclusions, which are distinctly different from the reticulofilamentous network.
*Denatured globin chains*
- **Denatured globin chains** (e.g., **Heinz bodies**) are associated with oxidative stress and appear as small, irregular inclusions that require **crystal violet stain** for visualization.
- These are not the prominent basophilic reticulations seen in reticulocytes.
*Mitochondria*
- **Mitochondria** are organelles responsible for cellular respiration and are present in many cell types, including immature red blood cells.
- However, they do not stain in the characteristic reticular pattern observed in reticulocytes using **supravital stains** for RNA.
Intracellular accumulations US Medical PG Question 3: A 43-year-old man presents to his primary care provider with concerns about general weakness and decreased concentration over the past several months. He reports constipation and unintentional weight loss of about 9.1 kg (20 lb). The past medical history is noncontributory. He works as a bank manager and occasionally drinks alcohol but does not smoke tobacco. Today, the vital signs include blood pressure 145/90 mm Hg, heart rate 60/min, respiratory rate 19/min, and temperature 36.6°C (97.9°F). On physical examination, the patient looks fatigued. His heart has a regular rate and rhythm, and his lungs are clear to auscultation bilaterally. Laboratory studies show:
Calcium 14.5 mg/dL
Phosphate 2.2 mg/dL
Parathyroid hormone (PTH) 18 pg/mL
Parathyroid hormone-related protein (PTHrP) 4 pmol/L Normal value: < 2 pmol/L
Calcitriol 46 pg/mL Normal value: 25–65 pg/mL
T3 120 ng/mL
T4 10.2 mcg/dL
Taking into account the clinical and laboratory findings, what is the most likely cause of this patient's hypercalcemia?
- A. Hyperparathyroidism
- B. Hypervitaminosis D
- C. Malignancy (Correct Answer)
- D. Thyrotoxicosis
- E. Chronic kidney disease
Intracellular accumulations Explanation: **Malignancy**
- The patient exhibits significant **hypercalcemia (14.5 mg/dL)**, **low normal PTH (18 pg/mL)**, elevated **PTHrP (4 pmol/L)**, and **unintentional weight loss**, all of which are highly suggestive of **humoral hypercalcemia of malignancy (HHM)**. PTHrP acts like PTH, leading to increased calcium reabsorption from bones and kidneys.
- The constellation of **weakness, decreased concentration, constipation**, and especially the **unexplained weight loss**, are classic paraneoplastic symptoms often associated with underlying malignancy, as opposed to primary endocrine disorders.
*Hyperparathyroidism*
- This condition is characterized by **elevated PTH levels** (typically > 65 pg/mL) in the presence of hypercalcemia, which is not seen here as the PTH is low normal.
- While it causes hypercalcemia, it typically does **not present with elevated PTHrP** or significant unexplained weight loss.
*Hypervitaminosis D*
- This would present with **elevated calcitriol (1,25-dihydroxyvitamin D)** levels, but in this patient, calcitriol is within the normal range.
- PTH levels would be suppressed, but **PTHrP would not be elevated**, which is a key differentiator in this case.
*Thyrotoxicosis*
- While hypercalcemia can sometimes be a feature of hyperthyroidism (thyrotoxicosis) due to increased bone turnover, it is usually **mild** and less severe than observed here (14.5 mg/dL).
- The patient's **T3 and T4 levels are within the normal range**, ruling out hyperthyroidism as the cause of hypercalcemia.
*Chronic kidney disease*
- In chronic kidney disease, hypercalcemia is less common; **hypocalcemia is more typical** due to impaired vitamin D activation and phosphate retention.
- While PTH can be elevated in secondary hyperparathyroidism of CKD, it would be in response to hypocalcemia, and **PTHrP would not be elevated**.
Intracellular accumulations US Medical PG Question 4: A 49-year-old man comes to the physician because of a 6-month history of increasing fatigue and reduced libido. He also complains of joint pain in both of his hands. His vital signs are within normal limits. Physical examination shows tanned skin and small testes. The second and third metacarpophalangeal joints of both hands are tender to palpation and range of motion is limited. The liver is palpated 2 to 3 cm below the right costal margin. Histopathologic examination of a liver biopsy specimen shows intracellular material that stains with Prussian blue. This patient is at greatest risk for developing which of the following complications?
- A. Rheumatoid arthritis
- B. Restrictive cardiomyopathy (Correct Answer)
- C. Non-Hodgkin lymphoma
- D. Colorectal carcinoma
- E. Pancreatic adenocarcinoma
Intracellular accumulations Explanation: ***Restrictive cardiomyopathy***
- The patient's symptoms (fatigue, reduced libido, tanned skin, small testes, joint pain, hepatomegaly) and **Prussian blue-positive intracellular material** in the liver biopsy are classic for **hemochromatosis**.
- **Cardiac iron deposition** is a serious and common complication leading to cardiomyopathy with symptoms like **fatigue** and heart failure.
- While hemochromatosis most commonly causes **dilated cardiomyopathy** or a mixed pattern, **restrictive features** can occur, and cardiac involvement is the **leading cause of death** in untreated patients.
*Rheumatoid arthritis*
- While joint pain is present, the specific involvement of the **second and third MCP joints** and the overall clinical picture are more consistent with **hemochromatosis-associated arthropathy**, not rheumatoid arthritis.
- Absence of typical RA features like **symmetric polyarthritis**, **morning stiffness lasting over 30 minutes**, and positive RF/anti-CCP antibodies make RA less likely.
*Non-Hodgkin lymphoma*
- **Non-Hodgkin lymphoma** is not a complication of hemochromatosis.
- While chronic immune stimulation in some conditions can increase lymphoma risk, there is no established association with **iron overload**.
*Colorectal carcinoma*
- There is no established increased risk of **colorectal carcinoma** due to hemochromatosis.
- **Hereditary hemochromatosis** primarily increases the risk of **hepatocellular carcinoma** (up to 200-fold increased risk in cirrhotic patients).
*Pancreatic adenocarcinoma*
- While **hemochromatosis** can lead to iron deposition in the pancreas, causing **diabetes mellitus** (bronze diabetes), it does not significantly increase the risk of **pancreatic adenocarcinoma**.
- Pancreatic involvement typically manifests as endocrine dysfunction, specifically **insulin deficiency** from beta-cell damage.
Intracellular accumulations US Medical PG Question 5: A 42-year-old man with systolic heart failure secondary to amyloidosis undergoes heart transplantation. The donor heart is obtained from a 17-year-old boy who died in a motor vehicle collision. Examination of the donor heart during the procedure shows a flat, yellow-white discoloration with an irregular border on the luminal surface of the aorta. A biopsy of this lesion is most likely to show which of the following?
- A. Apoptotic smooth muscle cells
- B. Necrotic cell debris
- C. Proteoglycan accumulation
- D. Collagen deposition
- E. Lipoprotein-laden macrophages (Correct Answer)
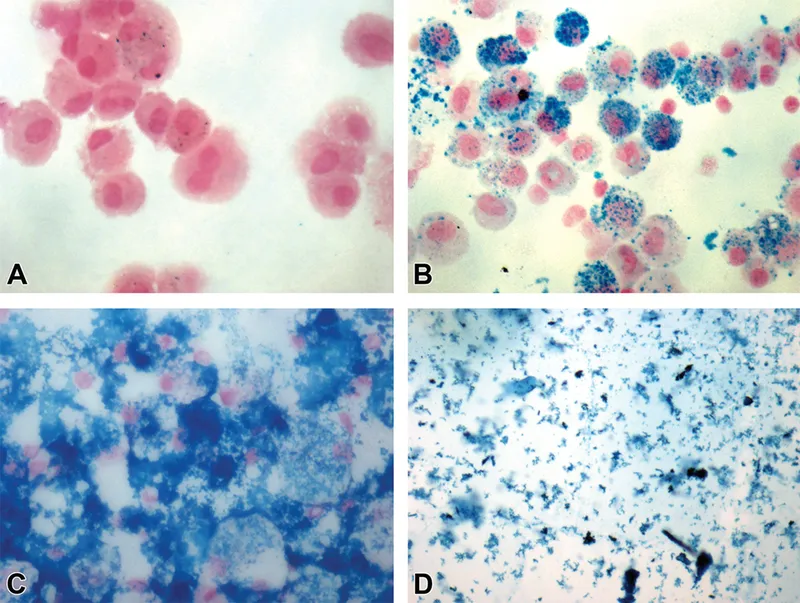
Intracellular accumulations Explanation: ***Lipoprotein-laden macrophages***
- The description of a flat, yellow-white discolored lesion with an irregular border on the luminal surface of the aorta in a 17-year-old is classic for a **fatty streak**, the earliest lesion of **atherosclerosis**.
- Fatty streaks are histologically characterized by the accumulation of **macrophages that have ingested oxidized lipoproteins**, appearing as foam cells within the intima.
*Apoptotic smooth muscle cells*
- While apoptosis of various cell types, including smooth muscle cells, can occur in advanced atherosclerotic lesions, it is not the primary or defining feature of an early **fatty streak**.
- **Apoptosis** contributes to the necrotic core formation in later stages of plaque development, not the initial yellow-white discoloration of a fatty streak.
*Necrotic cell debris*
- **Necrotic cell debris** is a prominent feature of more advanced, **complicated atherosclerotic plaques**, forming the necrotic core.
- In a **fatty streak**, the cells are primarily viable foam cells, and significant necrosis is not yet present.
*Proteoglycan accumulation*
- **Proteoglycan accumulation** occurs in the arterial intima and is involved in the retention of lipoproteins, contributing to the development of atherosclerosis.
- However, the immediate and most characteristic histological finding of the **yellow-white discoloration** in a fatty streak is the lipid-laden macrophage.
*Collagen deposition*
- **Collagen deposition** is a key feature of the fibrous cap in **advanced atherosclerotic plaques**, laid down by migrating smooth muscle cells.
- It is not the primary histological characteristic of an early, flat, yellow-white **fatty streak**.
Intracellular accumulations US Medical PG Question 6: A 45-year-old man comes to the physician for his routine health maintenance examination. He was diagnosed with diabetes mellitus 4 years ago. His medical history is otherwise unremarkable. He takes no medications other than daily metformin. He has consumed a can of beer every night for the past 10 years. His blood pressure is 145/90 mm Hg. His body mass index is 31 kg/m2. Physical examination shows no abnormalities. Laboratory studies show:
Partial thromboplastin time (activated) 30 seconds (N=25-40 seconds)
Prothrombin time 13 seconds (N=11-15 seconds)
International normalized ratio 1.2
Serum albumin 4 g/dL
Bilirubin, total 0.9 mg/dL
Direct 0.2 mg/dL
Alkaline phosphatase 45 U/L
Aspartate aminotransferase (AST, GOT) 43 U/L
Alanine aminotransferase (ALT, GPT) 56 U/L
γ-Glutamyltransferase (GGT) 43 U/L (N=5-50 U/L)
Hepatitis A antibody Negative
Hepatitis B surface antigen Negative
Hepatitis C antibody Negative
Liver biopsy shows excessive intracellular fat accumulation, hepatocyte ballooning, and perivenular infiltration of lymphocytes and neutrophils without significant fibrosis. Which of the following best describes these findings?
- A. Alcoholic hepatitis
- B. Nonalcoholic steatohepatitis (Correct Answer)
- C. Alcoholic cirrhosis
- D. Nonalcoholic-fatty-liver-disease-induced cirrhosis
- E. Alcoholic fatty liver
Intracellular accumulations Explanation: ***Nonalcoholic steatohepatitis***
- The patient has several risk factors for **nonalcoholic fatty liver disease (NAFLD)**, including **diabetes mellitus**, **obesity (BMI 31)**, and **hypertension**. The biopsy findings of **excessive intracellular fat accumulation**, **hepatocyte ballooning**, and **perivenular infiltration of lymphocytes and neutrophils without significant fibrosis** are characteristic of nonalcoholic steatohepatitis (NASH).
- The patient's modest alcohol intake of one can of beer per night for 10 years, while consistent, is generally not considered sufficient to cause alcoholic liver disease in the absence of other specific markers or severe presentation typically associated with alcoholic hepatitis or cirrhosis.
*Alcoholic hepatitis*
- **Alcoholic hepatitis** typically presents with a more significant history of **heavy alcohol consumption**, often leading to jaundice, fever, and a markedly elevated AST:ALT ratio (usually >2:1).
- While there is some alcohol intake, it is relatively modest (one can of beer daily), and the AST:ALT ratio is 43:56 (less than 1:1), which makes alcoholic hepatitis less likely.
*Alcoholic cirrhosis*
- **Alcoholic cirrhosis** requires a prolonged history of **heavy alcohol abuse**, which is not present here. It would also show significant **fibrosis** and architectural distortion on liver biopsy.
- The biopsy explicitly states **"without significant fibrosis,"** ruling out cirrhosis.
*Nonalcoholic-fatty-liver-disease-induced cirrhosis*
- While the patient has NAFLD, the biopsy specifically states **"without significant fibrosis"**.
- **Cirrhosis** by definition involves advanced fibrosis and architectural distortion, which are absent in this biopsy.
*Alcoholic fatty liver*
- **Alcoholic fatty liver (steatosis)** would primarily show **fat accumulation** without significant inflammation or hepatocyte ballooning.
- The presence of **hepatocyte ballooning** and **perivenular infiltration of lymphocytes and neutrophils** indicates inflammation and injury beyond simple steatosis, consistent with steatohepatitis.
Intracellular accumulations US Medical PG Question 7: Parkinson’s disease is a progressive neurodegenerative disease. It is characterized by a loss of dopaminergic neurons in the substantia nigra pars compacta and the formation of cellular inclusions called Lewy bodies. These are composed of α-synuclein that has been bound to ubiquitin. In healthy individuals, α-synuclein bound to ubiquitin would be degraded by which of the following?
- A. Peroxisome
- B. Lysosome
- C. Proteasome (Correct Answer)
- D. Ribosome
- E. Vesicle
Intracellular accumulations Explanation: ***Proteasome***
- The **ubiquitin-proteasome system** is the primary pathway for degrading misfolded or damaged proteins, such as **α-synuclein** bound to **ubiquitin**, within the cell.
- The proteasome specifically recognizes and breaks down proteins that have been tagged with multiple copies of the small protein **ubiquitin**.
*Peroxisome*
- Peroxisomes are involved in **fatty acid metabolism**, detoxification of reactive oxygen species, and other metabolic processes.
- They do not play a primary role in the degradation of ubiquitinated proteins.
*Lysosome*
- Lysosomes contain hydrolytic enzymes and are primarily responsible for the degradation of **extracellular material**, organelles, and certain intracellular proteins through **autophagy**.
- While they can degrade some ubiquitinated proteins, the proteasome is the dominant pathway for the specific degradation of misfolded cytoplasmic proteins.
*Ribosome*
- Ribosomes are responsible for **protein synthesis** (translation) based on mRNA templates.
- They are not involved in the degradation of proteins.
*Vesicle*
- Vesicles are small, membrane-bound sacs involved in transporting substances within the cell or releasing them outside the cell.
- They are primarily involved in storage and transport, not the enzymatic degradation of ubiquitinated proteins.
Intracellular accumulations US Medical PG Question 8: Two weeks after returning from vacation in Mexico, a 21-year-old man comes to the emergency department because of malaise, nausea, vomiting, fever, and abdominal pain. He has no history of serious illness and takes no medications. Physical examination shows scleral icterus and right upper quadrant tenderness. The liver is palpated 1.5 cm below the right costal margin. A biopsy specimen of this patient's liver would most likely show which of the following findings?
- A. Piecemeal necrosis and fatty changes
- B. Lymphocytic infiltration and progressive ductopenia
- C. Ballooning degeneration and bridging necrosis (Correct Answer)
- D. Ground glass hepatocytes and apoptotic bodies
- E. Dysplastic hepatocytes with intracellular bile
Intracellular accumulations Explanation: ***Ballooning degeneration and bridging necrosis***
- The patient presents with symptoms and signs of **acute viral hepatitis**, characterized by malaise, nausea, vomiting, fever, abdominal pain, scleral icterus, and right upper quadrant tenderness following travel to an endemic area (Mexico). **Ballooning degeneration** of hepatocytes and **bridging necrosis** (necrosis extending between portal tracts and central veins) are classic histological features of severe acute viral hepatitis.
- These findings reflect the **cytopathic effect of the virus** and the host's immune response, leading to hepatocyte injury and extensive liver damage.
*Piecemeal necrosis and fatty changes*
- **Piecemeal necrosis** (also known as interface hepatitis) is characteristic of **chronic hepatitis**, where inflammation at the portal-parenchymal interface leads to destruction of periportal hepatocytes, not typical for acute resolving hepatitis.
- **Fatty changes** (steatosis) are commonly seen in conditions like **alcoholic liver disease** or **non-alcoholic fatty liver disease (NAFLD)**, and are not primary features of acute viral hepatitis.
*Lymphocytic infiltration and progressive ductopenia*
- **Lymphocytic infiltration** is a general feature of many forms of hepatitis, but **progressive ductopenia** (loss of bile ducts) is highly suggestive of **primary biliary cholangitis (PBC)**, an autoimmune condition, or **primary sclerosing cholangitis (PSC)**, which does not fit the acute presentation or travel history.
- These conditions are typically chronic and have different clinical manifestations.
*Ground glass hepatocytes and apoptotic bodies*
- **Ground-glass hepatocytes** are a hallmark feature of **chronic hepatitis B infection**, indicating the accumulation of HBsAg in the endoplasmic reticulum. This is not typical for acute viral hepatitis where the virus may still be replicating rapidly.
- While **apoptotic bodies** (Councilman bodies) can be seen in acute hepatitis, they are not the predominant or most specific finding to describe the widespread damage seen with ballooning degeneration and necrosis.
*Dysplastic hepatocytes with intracellular bile*
- **Dysplastic hepatocytes** are indicative of **precancerous changes** or **hepatocellular carcinoma (HCC)**, usually occurring in the context of chronic liver disease, not acute self-limiting hepatitis.
- While **intracellular bile** might be seen in cholestatic conditions, the combination of dysplastic hepatocytes points away from acute viral hepatitis.
Intracellular accumulations US Medical PG Question 9: A 75-year-old man comes to the physician because of abdominal pain and nausea over the past 2 weeks and a 1-month history of pain in his knees and hips. He has smoked one pack of cigarettes daily for 30 years. Physical examination shows decreased muscle strength. Laboratory studies show:
Hemoglobin 11.0 mg/dL
Serum
Creatinine 1.5 mg/dL
Calcium 12.2 mg/dL
Parathyroid hormone 115 pg/mL
Parathyroid hormone-related peptide elevated
Urine
Blood 2+
Ultrasonography of his abdomen shows a 6-cm mass in his right kidney. Nephrectomy is performed. A photograph of the resected specimen is shown. The patient's tumor most likely originated from which of the following locations?
- A. Collecting tubules
- B. Proximal convoluted tubules (Correct Answer)
- C. Glomerulus
- D. Renal pelvis
- E. Distal convoluted tubules
Intracellular accumulations Explanation: ***Proximal convoluted tubules***
- The patient's symptoms (abdominal pain, nausea, bone pain, hypercalcemia, elevated PTHrP, renal mass, anemia, hematuria) are classic for **renal cell carcinoma (RCC)**, which typically arises from the **proximal convoluted tubules**.
- RCC often secretes **parathyroid hormone-related peptide (PTHrP)**, leading to **hypercalcemia** through paraneoplastic mechanisms.
- Note: In typical malignancy-associated hypercalcemia, PTHrP causes hypercalcemia which should **suppress** endogenous PTH via negative feedback; the elevated PTH shown here may represent concurrent primary hyperparathyroidism or laboratory timing issues.
*Collecting tubules*
- Tumors originating from the collecting tubules are rare and are known as **collecting duct carcinoma (Bellini duct carcinoma)**.
- These aggressive tumors typically present with **hematuria** and flank pain but are less commonly associated with paraneoplastic syndromes like PTHrP-induced hypercalcemia.
*Glomerulus*
- Tumors originating directly from the glomerulus, such as primary glomerular cancers, are exceedingly rare.
- Most glomerular pathologies are inflammatory or degenerative rather than primary neoplasms.
*Renal pelvis*
- Tumors in the renal pelvis are typically **urothelial carcinomas (transitional cell carcinomas)**, which arise from the urothelial lining.
- While they can present with hematuria and flank pain, they are less commonly associated with the paraneoplastic syndrome of hypercalcemia due to PTHrP secretion compared to RCC.
*Distal convoluted tubules*
- Tumors originating from the distal convoluted tubules are uncommon.
- **Oncocytomas**, a benign renal tumor, are thought to arise from the distal nephron or collecting ducts, but they do not typically cause paraneoplastic syndromes like hypercalcemia.
Intracellular accumulations US Medical PG Question 10: A 32-year-old woman presents to her primary care physician for an annual checkup. She reports that she has been feeling well and has no medical concerns. Her past medical history is significant for childhood asthma but she has not experienced any symptoms since she was a teenager. Physical exam reveals a 1-centimeter hard mobile mass in the left upper outer quadrant of her breast. A mammogram was performed and demonstrated calcifications within the mass so a biopsy was obtained. The biopsy shows acinar proliferation with intralobular fibrosis. Which of the following conditions is most likely affecting this patient?
- A. Sclerosing adenosis (Correct Answer)
- B. Fibroadenoma
- C. Cystic hyperplasia
- D. Invasive lobular carcinoma
- E. Infiltrating ductal carcinoma
Intracellular accumulations Explanation: ***Sclerosing adenosis***
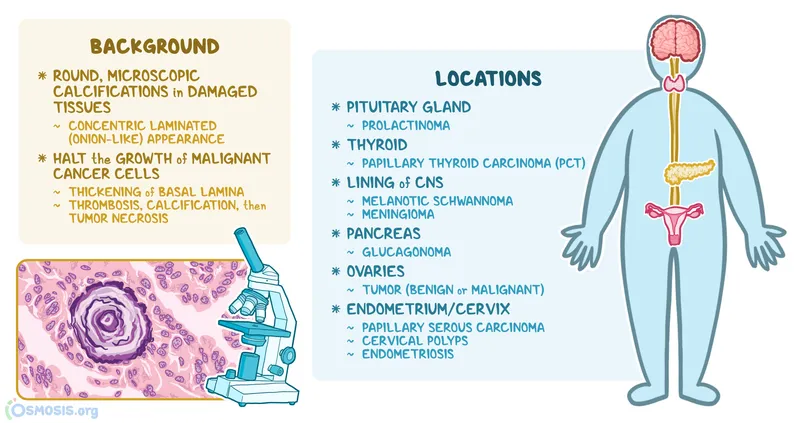
- This condition is characterized by **acinar proliferation with intralobular fibrosis**, which exactly matches the biopsy findings mentioned in the vignette.
- Sclerosing adenosis can present as a palpable mass with **calcifications on mammography**, mimicking carcinoma, necessitating biopsy for definitive diagnosis.
*Fibroadenoma*
- Characterized by proliferation of both **stromal and epithelial elements**, often forming well-circumscribed, mobile masses.
- While it can present as a mobile mass, the specific histological finding of "acinar proliferation with intralobular fibrosis" is not the primary descriptive characteristic of a fibroadenoma.
*Cystic hyperplasia*
- This term, often used interchangeably with **fibrocystic changes**, involves the formation of cysts and an increase in fibrous tissue.
- While it can involve hyperplasia, it doesn't typically describe the distinct pattern of "acinar proliferation with intralobular fibrosis" as seen in sclerosing adenosis.
*Invasive lobular carcinoma*
- This carcinoma is characterized by its **infiltrative growth pattern** often in single file lines, and typically does not form a well-defined mass.
- While it can present with calcifications, the absence of overt malignant features and the specific benign histological description rule out this diagnosis.
*Infiltrating ductal carcinoma*
- The most common type of breast cancer, characterized by **malignant epithelial cells infiltrating the stroma**.
- The biopsy findings described ("acinar proliferation with intralobular fibrosis") are features of a benign process, not a malignant one.
More Intracellular accumulations US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.