Hyperplasia and metaplasia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hyperplasia and metaplasia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hyperplasia and metaplasia US Medical PG Question 1: A 52-year-old Caucasian male presents to your office complaining of black, tarry stool. Which of the following possible causes of this patient's presentation is LEAST associated with the development of carcinoma?
- A. Adenomatous polyp
- B. H. pylori infection
- C. Gastric ulcer
- D. Barrett's esophagus
- E. Duodenal ulcer (Correct Answer)
Hyperplasia and metaplasia Explanation: ***Duodenal ulcer***
- While duodenal ulcers can cause **melena** due to upper GI bleeding, they are **rarely associated with an increased risk of carcinoma**.
- They typically result from **H. pylori infection** or NSAID use, and the duodenal mucosa has a very low propensity for malignant transformation.
*Adenomatous polyp*
- **Adenomatous polyps** are considered **premalignant lesions** and are strongly associated with the development of colorectal carcinoma.
- The risk of malignancy increases with polyp size, villous histology, and degree of dysplasia.
*H. pylori infection*
- **Chronic H. pylori infection** is a major risk factor for several gastric malignancies, including **gastric adenocarcinoma** and **MALT lymphoma**.
- It causes chronic inflammation, leading to atrophy, intestinal metaplasia, and dysplasia, which are precursors to cancer.
*Gastric ulcer*
- While most gastric ulcers are benign, a significant proportion (especially those not resolving with treatment) can be **malignant (gastric adenocarcinoma)**.
- H. pylori infection and NSAID use are common causes for both benign and malignant gastric ulcers, and all gastric ulcers require follow-up to rule out malignancy.
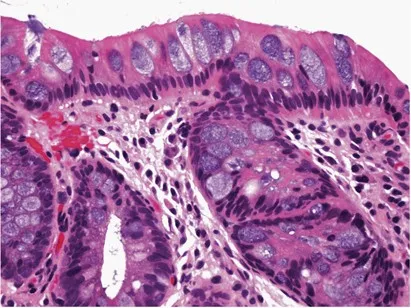
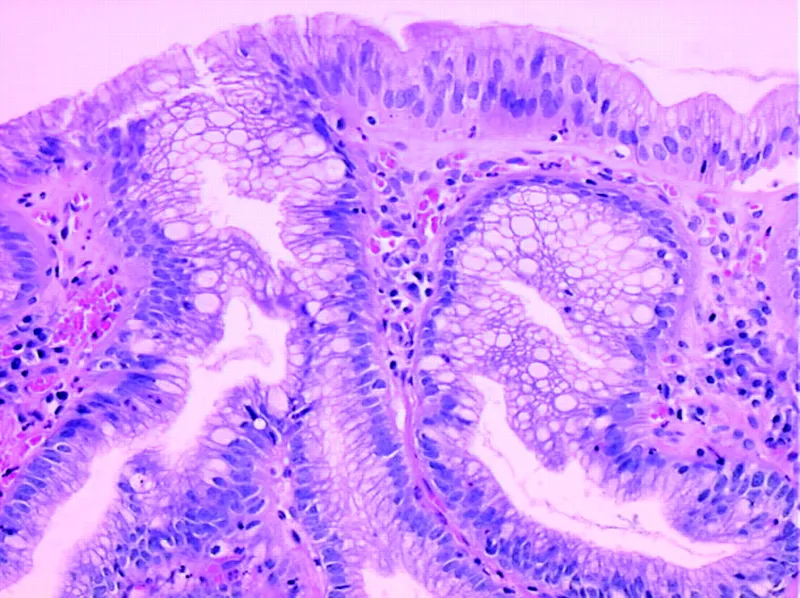
*Barrett's esophagus*
- **Barrett's esophagus** is a premalignant condition where the normal stratified squamous epithelium of the esophagus is replaced by intestinal columnar epithelium.
- It is a major risk factor for the development of **esophageal adenocarcinoma**, with the risk increasing with the degree of dysplasia.
Hyperplasia and metaplasia US Medical PG Question 2: A 34-year-old man with worsening refractory epigastric pain secondary to long-standing gastroesophageal reflux disease presents for endoscopic evaluation. Past medical history is also significant for type 2 diabetes mellitus that was diagnosed 3 years ago, managed medically. Current medications are metformin, metoclopramide, and omeprazole. Which of the following best describes this patient’s most likely endoscopic findings?
- A. Esophageal smooth muscle atrophy
- B. Metaplasia of the esophageal mucosa (Correct Answer)
- C. A malignant proliferation of squamous cells
- D. Hypertrophy of the esophageal mucosa protruding into the lumen of the lower esophagus
- E. Longitudinal lacerations of the esophageal mucosa
Hyperplasia and metaplasia Explanation: ***Metaplasia of the esophageal mucosa***
- Long-standing **gastroesophageal reflux disease (GERD)** can lead to **Barrett's esophagus**, a condition where the normal **squamous epithelium** of the esophagus is replaced by **columnar epithelium** (intestinal metaplasia) due to chronic acid exposure.
- This endoscopic finding is significant as **Barrett's esophagus** is a well-known **premalignant condition** for esophageal adenocarcinoma.
*Esophageal smooth muscle atrophy*
- This is commonly seen in conditions like **scleroderma** or other **motility disorders**, where the smooth muscle of the esophagus degenerates, leading to impaired peristalsis.
- While GERD can be a complication of such disorders, **smooth muscle atrophy** is not the primary endoscopic finding directly related to long-standing refractory GERD itself.
*A malignant proliferation of squamous cells*
- This describes **squamous cell carcinoma** of the esophagus, which is typically associated with risk factors like **smoking** and **alcohol consumption**.
- While Barrett's esophagus can progress to adenocarcinoma, direct squamous cell carcinoma is not the *most likely* initial finding after chronic reflux.
*Hypertrophy of the esophageal mucosa protruding into the lumen of the lower esophagus*
- **Hypertrophy** (enlargement) of the esophageal mucosa is not a typical finding in chronic GERD; rather, the mucosa undergoes changes like **inflammation**, **erosion**, or **metaplasia**.
- Protrusions into the lumen in this context would more likely suggest a **polyp** or **tumor**, which are less common primary findings than metaplasia in long-standing GERD.
*Longitudinal lacerations of the esophageal mucosa*
- **Longitudinal lacerations** of the esophageal mucosa, often near the gastroesophageal junction, are characteristic of **Mallory-Weiss tears**, which result from forceful vomiting or retching.
- These are acute injuries and not directly indicative of the chronic changes expected in long-standing refractory GERD.
Hyperplasia and metaplasia US Medical PG Question 3: A 35-year-old man comes to the physician for evaluation of a neck mass and hoarseness. He has no history of major medical illness. Physical examination shows a 2.5-cm fixed, irregular thyroid nodule. His serum calcitonin concentration is elevated. The nodule is most likely comprised of cells that are embryologically derived from which of the following structures?
- A. Second branchial pouch
- B. Fourth branchial arch
- C. Surface ectoderm
- D. Third branchial pouch
- E. Neural crest cells (Correct Answer)
Hyperplasia and metaplasia Explanation: ***Neural crest cells***
- The elevated **serum calcitonin** in the presence of a thyroid nodule is highly suggestive of **medullary thyroid carcinoma (MTC)**.
- **MTC** originates from the **parafollicular C cells** of the thyroid, which are embryologically derived from **neural crest cells** that migrate to the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) during development and subsequently integrate into the thyroid gland.
- This is the definitive embryological origin of calcitonin-producing C cells.
*Second branchial pouch*
- The second branchial pouch typically gives rise to the **palatine tonsil crypts** and **tonsillar fossa**.
- It is not associated with the development of the **parafollicular C cells** or thyroid malignancies.
*Fourth branchial arch*
- The fourth branchial arch gives rise to the **superior laryngeal nerve** and associated laryngeal cartilages.
- While the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) does contribute C cells to the thyroid, these cells themselves are derived from **neural crest cells** that migrate to this structure, not from the pouch itself.
- Therefore, the embryological origin is neural crest, not the branchial arch/pouch.
*Surface ectoderm*
- Surface ectoderm forms structures such as the **epidermis of the skin**, **hair**, **nails**, and **lens of the eye**.
- It does not contribute to the development of the **C cells** or the thyroid gland.
*Third branchial pouch*
- The third branchial pouch gives rise to the **inferior parathyroid glands** and the majority of the **thymus**.
- While it contributes to endocrine tissues, it does not form the **parafollicular C cells** of the thyroid.
Hyperplasia and metaplasia US Medical PG Question 4: A gastroenterology fellow is interested in the relationship between smoking and incidence of Barrett esophagus. At a departmental grand rounds she recently attended, one of the presenters claimed that smokers are only at increased risk for Barrett esophagus in the presence of acid reflux. She decides to design a retrospective cohort study to investigate the association between smoking and Barrett esophagus. After comparing 400 smokers to 400 non-smokers identified via chart review, she finds that smokers were at increased risk of Barrett esophagus at the end of a 10-year follow-up period (RR = 1.82, p < 0.001). Among patients with a history of acid reflux, there was no relationship between smoking and Barrett esophagus (p = 0.52). Likewise, no relationship was found between smoking and Barrett esophagus among patients without a history of acid reflux (p = 0.48). The results of this study are best explained by which of the following?
- A. Random error
- B. Matching
- C. Effect modification
- D. Stratification
- E. Confounding (Correct Answer)
Hyperplasia and metaplasia Explanation: ***Confounding***
- The initial finding of an increased risk (RR = 1.82) between smoking and Barrett esophagus disappears when the population is **stratified by acid reflux**. This suggests that acid reflux was **confounding** the observed association.
- A confounder is an **extraneous variable** that is related to both the exposure (smoking) and the outcome (Barrett esophagus) but is not part of the causal pathway, thereby distorting the true association.
*Random error*
- Random error leads to **imprecise results** due to natural variability and is unlikely to fully explain the disappearance of a statistically significant association (p < 0.001) after stratification.
- While it can affect the p-values, it typically wouldn't completely nullify a strong original finding across all stratified groups.
*Matching*
- Matching is a technique used in study design (e.g., case-control studies) to **control for confounding** by ensuring similar distribution of confounding variables between groups.
- The problem describes a **retrospective cohort study** where stratification was performed *after* data collection, not matching during the design phase.
*Effect modification*
- Effect modification occurs when the **effect of an exposure on an outcome differs across strata** of another variable. If there were effect modification, we would expect to see varying relationships (e.g., a strong association in one stratum and a weak/absent one in another).
- In this scenario, the association between smoking and Barrett esophagus becomes **non-significant in *both*** reflux and non-reflux strata (p=0.52 and p=0.48), indicating no differential effect but rather the removal of a spurious association.
*Stratification*
- Stratification is a **method of analysis** used to assess for confounding or effect modification by examining the association within subgroups (strata) based on a third variable.
- While stratification was *performed* in the study, it is the *result* (the disappearance of the association) that best explains the phenomenon, indicating **confounding** by acid reflux.
Hyperplasia and metaplasia US Medical PG Question 5: A 48-year-old man has smoked approximately 3 packs of cigarettes per day for the past 12 years. Which of the following pathologic changes is most likely to occur in his bronchial epithelium?
- A. Metaplasia (Correct Answer)
- B. Hyperplasia
- C. Hypertrophy
- D. Dysplasia
- E. Atrophy
Hyperplasia and metaplasia Explanation: ***Metaplasia***
- Chronic irritation from **cigarette smoking** can cause the **bronchial epithelium** to change from ciliated columnar to stratified squamous, a process known as **metaplasia**.
- This adaptation makes the tissue more resistant to injury but results in the loss of important protective functions like **mucociliary clearance**.
*Hyperplasia*
- **Hyperplasia** involves an increase in the number of cells in a tissue or organ, often in response to increased demand or chronic stimulation.
- While smoking can cause hyperplasia of goblet cells and mucous glands in the bronchi, the direct epithelial change in response to chronic irritation is more specifically **metaplasia**.
*Hypertrophy*
- **Hypertrophy** is an increase in the size of individual cells, leading to an increase in the size of the organ or tissue.
- This is not the primary adaptive change seen in the bronchial epithelium in response to chronic smoking; instead, cells change their type.
*Dysplasia*
- **Dysplasia** refers to disorderly cell growth, often characterized by variations in cell size, shape, and organization; it is considered a precursor to cancer.
- While chronic smoking can eventually lead to dysplasia and then carcinoma, the initial and most common adaptive change in the bronchial epithelium is **metaplasia**.
*Atrophy*
- **Atrophy** is a decrease in cell size or number, leading to a reduction in the size of an organ or tissue, usually due to decreased workload, nutrition, or blood supply.
- This is not a typical response of the bronchial epithelium to chronic irritation from smoking, which tends to induce proliferative or adaptive changes.
Hyperplasia and metaplasia US Medical PG Question 6: A 45-year-old African American male presents to his primary care physician complaining of difficulty swallowing that was initially limited to solids but has now progressed to liquids. Biopsy of the esophagus reveals dysplastic cells, but does not show evidence of glands or increased mucin. Which of the following most contributed to his condition?
- A. Gastroesophageal reflux disease
- B. Obesity
- C. Drinking extremely hot beverages
- D. Radiation exposure in the past 6 months
- E. Smoking (Correct Answer)
Hyperplasia and metaplasia Explanation: ***Smoking***
- **Smoking** is the most significant risk factor for **squamous cell carcinoma** of the esophagus, which is strongly suggested by the biopsy findings of **dysplastic cells without glands or mucin**.
- The combination of **progressive dysphagia** (solids to liquids) and smoking history in an **African American male** fits the classic demographic and presentation pattern for esophageal squamous cell carcinoma.
*Gastroesophageal reflux disease*
- **GERD** primarily leads to **esophageal adenocarcinoma** through **Barrett's esophagus**, which would show **glandular metaplasia** and **increased mucin production** on biopsy.
- The biopsy explicitly states **absence of glands and mucin**, making GERD-related adenocarcinoma unlikely as the primary pathologic process.
*Obesity*
- **Obesity** increases risk of **esophageal adenocarcinoma** by worsening **GERD** and promoting **Barrett's esophagus** development.
- Since the biopsy findings suggest **squamous cell carcinoma** rather than adenocarcinoma, obesity is not the most direct contributing factor in this case.
*Drinking extremely hot beverages*
- **Hot beverage consumption** is indeed a risk factor for **squamous cell carcinoma** of the esophagus, particularly in certain geographic regions.
- However, **smoking** remains the more prevalent and significant risk factor globally, especially when combined with **alcohol use**, making it the primary contributor.
*Radiation exposure in the past 6 months*
- **Radiation exposure** can increase risk of esophageal cancer, including **squamous cell carcinoma**, but typically requires a **longer latency period** (years to decades).
- A **6-month timeframe** is insufficient for radiation-induced carcinogenesis to manifest as advanced cancer with dysphagia and dysplastic changes.
Hyperplasia and metaplasia US Medical PG Question 7: As part of a clinical research study, microscopic analysis of tissues obtained from surgical specimens is performed. Some of these tissues have microscopic findings of an increase in the size of numerous cells within the tissue with an increase in the amount of cytoplasm, but the nuclei are uniform in size. Which of the following processes shows such microscopic findings?
- A. Liver following partial resection
- B. Female breasts at puberty
- C. Ovaries following menopause
- D. Uterine myometrium in pregnancy (Correct Answer)
- E. Cervix with chronic inflammation
Hyperplasia and metaplasia Explanation: ***Uterine myometrium in pregnancy***
- During pregnancy, the uterine myometrial cells undergo significant **hypertrophy** (increase in cell size) in response to hormonal stimulation, primarily *estrogen* and *progesterone*.
- This leads to a marked increase in the amount of **cytoplasm** and overall cell size, while maintaining relatively **uniform nuclei**, which precisely matches the microscopic findings described.
- The smooth muscle cells can increase **10-40 fold** in size, making this the classic example of physiologic hypertrophy.
- Note: Hyperplasia (increased cell number) also occurs but is less prominent; the microscopic findings described emphasize the hypertrophic changes.
*Liver following partial resection*
- The liver primarily undergoes **hyperplasia** (increase in cell number) to regenerate following partial resection.
- While some hypertrophy occurs, the dominant microscopic finding is an increase in hepatocyte **number** through proliferation rather than a marked increase in individual cell size and cytoplasm as the primary feature.
*Female breasts at puberty*
- Breast development at puberty involves both **hyperplasia** of the glandular epithelium and ductal structures and **adipose tissue deposition**, driven by *estrogen* and *progesterone*.
- The findings described (marked increase in cell size and cytoplasm with uniform nuclei) are more characteristic of the extreme cell hypertrophy seen in the gravid uterus rather than the mixed growth and differentiation patterns of pubertal breast development.
*Ovaries following menopause*
- Following menopause, the ovaries undergo **atrophy**, meaning a decrease in size and cellular activity due to declining hormonal production.
- This process involves a **decrease in cell size** and number, which is the opposite of the microscopic findings described in the question.
*Cervix with chronic inflammation*
- Chronic inflammation in the cervix can cause various changes, including **squamous metaplasia** (transformation of columnar epithelium to squamous epithelium) or an influx of inflammatory cells.
- While there might be some reactive cellular changes, it does not typically involve a widespread, uniform increase in cell size and cytoplasm within existing cells as described, but rather a change in cell type or infiltration by inflammatory cells.
Hyperplasia and metaplasia US Medical PG Question 8: An 83-year-old woman with a history of atrial fibrillation, multiple ischemic strokes, and early dementia is found unresponsive in her apartment at her retirement community. She is believed to have not refilled any of her medications for a month, and it is determined that she passed away from a stroke nearly 2 weeks ago. The family is adamant that she receive an autopsy. Which of the following findings are most likely on brain histology?
- A. Cellular debris and lymphocytes
- B. Cystic cavitation (Correct Answer)
- C. Fat saponification
- D. Cellular debris and neutrophils
- E. Increased binding of acidophilic dyes
Hyperplasia and metaplasia Explanation: **Cystic cavitation**
- A **stroke** that occurred two weeks prior would most likely show **cystic cavitation** as the brain tissue attempts to repair itself after the damage.
- Over time, the necrotic tissue is removed, and a fluid-filled cavity forms, which is the final stage of **infarction resolution**.
*Cellular debris and lymphocytes*
- While **cellular debris** would be present, **lymphocytes** are typically later responders in inflammation, and at two weeks, the most prominent feature would be cavitation.
- **Microglia** and **macrophages** would be the primary cells involved in clearing debris, leading to cavitation.
*Fat saponification*
- **Fat saponification** is a type of **fat necrosis** seen in areas like the pancreas or breast, not typically in the brain after an ischemic stroke.
- This process involves the hydrolysis of triglycerides into fatty acids that combine with calcium, forming a chalky substance.
*Cellular debris and neutrophils*
- **Neutrophils** are characteristic of the very **early stages of acute inflammation**, typically within the first 24-48 hours after an ischemic stroke.
- By two weeks, most neutrophils would have resolved, and mononuclear cells and macrophages would predominate.
*Increased binding of acidophilic dyes*
- **Increased binding of acidophilic dyes** (like eosin) is seen in **early ischemic changes** (e.g., within hours to days), indicating **cell necrosis** like **red neurons**.
- At two weeks, the tissue has progressed beyond this immediate necrotic stage to active removal and cavitation.
Hyperplasia and metaplasia US Medical PG Question 9: A 64-year-old woman is brought to the emergency department 30 minutes after the onset of right-sided weakness and impaired speech. On admission, she is diagnosed with thrombotic stroke and treatment with alteplase is begun. Neurologic examination four weeks later shows residual right hemiparesis. A CT scan of the head shows hypoattenuation in the territory of the left middle cerebral artery. Which of the following processes best explains this finding?
- A. Liquefactive necrosis (Correct Answer)
- B. Caseous necrosis
- C. Gangrenous necrosis
- D. Coagulative necrosis
- E. Fat necrosis
Hyperplasia and metaplasia Explanation: ***Liquefactive necrosis***
- This is the characteristic type of necrosis seen in the **central nervous system** following an ischemic insult like a stroke.
- The brain tissue is rapidly digested by hydrolytic enzymes, forming a **cyst-like cavity** filled with fluid (hence "hypoattenuation" on CT), reflecting the accumulation of necrotic cellular debris.
*Caseous necrosis*
- This is a form of cell death typically associated with **tuberculous infections** and some fungal infections.
- It results in the formation of a cheesy, friable material consisting of fragmented cells and granular debris, which is not characteristic of stroke.
*Gangrenous necrosis*
- This type of necrosis is typically seen in the **extremities** and is often associated with a loss of blood supply and subsequent bacterial infection.
- It involves tissue death due to ischemia, often accompanied by signs of putrefaction, making it distinct from a brain infarct.
*Coagulative necrosis*
- This is the most common type of necrosis and occurs in solid organs (e.g., heart, kidney) due to **ischemia**, preserving the architectural outlines of the dead cells for a period.
- Unlike the brain, where rapid liquefaction occurs, coagulative necrosis is not the primary form of cell death observed in the central nervous system after an ischemic stroke.
*Fat necrosis*
- This occurs in **adipose tissue**, usually due to trauma or enzymatic digestion (e.g., in pancreatitis).
- It involves the breakdown of fats into fatty acids, which then combine with calcium to form chalky white areas, which is not relevant to a cerebral infarct.
Hyperplasia and metaplasia US Medical PG Question 10: A 38-year-old man is admitted to the hospital because of fever, yellowing of the skin, and nausea for 1 day. He recently returned from a backpacking trip to Brazil and Paraguay, during which he had a 3-day episode of high fever that resolved spontaneously. Physical examination shows jaundice, epigastric tenderness, and petechiae over his trunk. Five hours after admission, he develops dark brown emesis and anuria. Despite appropriate lifesaving measures, he dies. Postmortem liver biopsy shows eosinophilic degeneration of hepatocytes with condensed nuclear chromatin. This patient’s hepatocytes were most likely undergoing which of the following processes?
- A. Regeneration
- B. Steatosis
- C. Necrosis
- D. Apoptosis (Correct Answer)
- E. Proliferation
Hyperplasia and metaplasia Explanation: ***Apoptosis***
- The patient's symptoms (fever, jaundice, epigastric tenderness, petechiae, dark emesis, anuria) and history of travel to endemic areas are highly suggestive of **Yellow Fever**.
- **Eosinophilic degeneration of hepatocytes with condensed nuclear chromatin**, described as **Councilman bodies** or **apoptotic bodies**, is a characteristic histological finding in Yellow Fever and indicates programmed cell death.
*Regeneration*
- This process involves the replacement of damaged tissue with new, healthy tissue, which would contradict the patient's rapidly deteriorating condition and death.
- While regeneration can occur in the liver, the described histological findings of **eosinophilic degeneration** and **condensed nuclear chromatin** are indicative of cell death, not repair.
*Steatosis*
- **Steatosis** refers to the accumulation of fat droplets within hepatocytes, which is usually seen in conditions like alcoholic liver disease or non-alcoholic fatty liver disease.
- This is not consistent with the eosinophilic degeneration and condensed chromatin described, which point to a different type of cellular injury.
*Necrosis*
- **Necrosis** is a form of unregulated cell death often associated with inflammation and cellular swelling; the description of **eosinophilic degeneration** and **condensed nuclear chromatin** points specifically to apoptotic cell death rather than necrotic changes which would typically include cell swelling and rupture.
- While Yellow Fever does cause significant liver damage leading to cell death, the specific histological features (e.g., Councilman bodies) are characteristic of **apoptosis**, not typically seen in necrosis.
*Proliferation*
- **Proliferation** refers to an increase in the number of cells, typically in response to a stimulus or as part of a disease process like cancer.
- The patient's rapid decline and the histological findings of dying cells (eosinophilic degeneration, condensed chromatin) are antithetical to cellular proliferation.
More Hyperplasia and metaplasia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.