Free radical injury US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Free radical injury. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Free radical injury US Medical PG Question 1: A 33-year-old woman is brought to the emergency department 30 minutes after being rescued from a fire in her apartment. She reports nausea, headache, and dizziness. Physical examination shows black discoloration of her oral mucosa. Pulse oximetry shows an oxygen saturation of 99% on room air. The substance most likely causing symptoms in this patient primarily produces toxicity by which of the following mechanisms?
- A. Inhibition of mitochondrial complex V
- B. Degradation of 2,3-bisphosphoglycerate
- C. Oxidation of Fe2+
- D. Rise in serum pH
- E. Competitive binding to heme (Correct Answer)
Free radical injury Explanation: ***Competitive binding to heme***
- The patient's symptoms (nausea, headache, dizziness, black oral mucosa) and history of being rescued from a fire strongly suggest **carbon monoxide (CO) poisoning** [1].
- **Carbon monoxide** primarily exerts its toxicity by competitively binding to the **heme iron** in hemoglobin with an affinity 200-250 times greater than oxygen, forming **carboxyhemoglobin (COHb)** and displacing oxygen [2].
*Inhibition of mitochondrial complex V*
- **Cyanide poisoning** inhibits **mitochondrial complex IV (cytochrome c oxidase)**, not complex V, leading to impaired cellular respiration.
- While both cyanide and CO poisoning can occur in fires, CO is more common due to incomplete combustion, and the specific presentation points toward CO.
*Degradation of 2,3-bisphosphoglycerate*
- **2,3-BPG** is an important regulator of oxygen affinity for hemoglobin, promoting oxygen release to tissues [2]. Its degradation would increase hemoglobin's affinity for oxygen, thus reducing oxygen unloading, but this is not the primary mechanism of toxicity for CO or common fire-related toxins.
- No common toxin directly causes widespread degradation of 2,3-BPG as its primary mechanism of acute toxicity or symptoms.
*Oxidation of Fe2+*
- The oxidation of **ferrous iron (Fe2+)** to **ferric iron (Fe3+)** in hemoglobin leads to the formation of **methemoglobin**, which cannot bind oxygen. This occurs in **methemoglobinemia** induced by certain drugs or toxins (e.g., nitrites, dapsone).
- While **methemoglobinemia** impairs oxygen transport, it does not explain the black oral mucosa or the strong association with fire smoke toxicity in the context of CO.
*Rise in serum pH*
- A rise in serum pH (alkalosis) is not a direct or primary mechanism of toxicity for common fire-related toxins like carbon monoxide or cyanide.
- Most severe forms of toxicity, including CO and cyanide poisoning, tend to cause **lactic acidosis** due to cellular hypoxia and anaerobic metabolism, leading to a
**decrease** in serum pH.
Free radical injury US Medical PG Question 2: A 72-year-old man has been recently diagnosed with stage 3 squamous cell carcinoma of the oral cavity. After the necessary laboratory workup, concurrent chemoradiation therapy has been planned. Radiation therapy is planned to take place over 7 weeks and he will receive radiation doses daily, Monday–Friday, in 2.0 Gy fractions. For concurrent chemotherapy, he will receive intravenous cisplatin at a dosage of 50 mg/m2 weekly for 7 weeks. Which of the following best explains the mechanism of action of the antineoplastic drug that the patient will receive?
- A. Free radical-mediated lipid peroxidation
- B. Inhibition of polymerization of tubulin
- C. Inhibition of topoisomerase 1
- D. Inhibition of topoisomerase 2
- E. Formation of interstrand DNA cross-links (Correct Answer)
Free radical injury Explanation: ***Formation of interstrand DNA cross-links***
- **Cisplatin** is a **platinum-based chemotherapeutic agent** that acts by forming **interstrand and intrastrand DNA cross-links**.
- These cross-links interfere with **DNA replication and transcription**, leading to **DNA damage** and ultimately **apoptosis** in cancer cells.
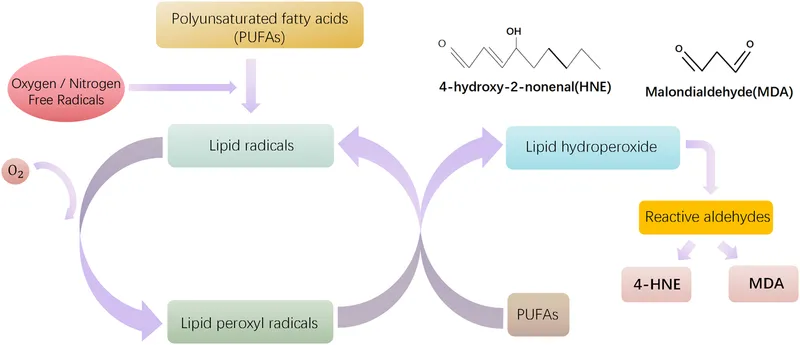
*Free radical-mediated lipid peroxidation*
- While some chemotherapeutic agents, like **anthracyclines**, can induce **free radical formation** and subsequent damage, this is not the primary mechanism of action for cisplatin.
- **Lipid peroxidation** primarily affects cell membranes, whereas cisplatin's main target is DNA.
*Inhibition of polymerization of tubulin*
- This mechanism of action is characteristic of **vinca alkaloids** (e.g., vincristine, vinblastine) and **taxanes** (e.g., paclitaxel, docetaxel), which disrupt microtubule formation and function.
- Cisplatin does not target **tubulin polymerization**.
*Inhibition of topoisomerase 1*
- **Topoisomerase 1 inhibitors** such as **irinotecan** and **topotecan** prevent DNA unwinding by stabilizing the cleavable complex, leading to DNA breaks.
- This is not how cisplatin exerts its therapeutic effects.
*Inhibition of topoisomerase 2*
- **Topoisomerase 2 inhibitors** like **etoposide** and **doxorubicin** interfere with DNA replication and repair by preventing the religation of DNA strands.
- Cisplatin's mechanism is distinct from topoisomerase inhibition.
Free radical injury US Medical PG Question 3: A healthy 34-year-old woman comes to the physician for advice on UV protection. She works as an archaeologist and is required to work outside for extended periods of time. She is concerned about premature skin aging. The physician recommends sun-protective clothing and sunscreen. In order to protect effectively against photoaging, the sunscreen should contain which of the following active ingredients?
- A. Zinc oxide (Correct Answer)
- B. Vitamin E
- C. Para-aminobenzoic acid
- D. Trimethoprim/sulfamethoxazole
- E. Trolamine salicylate
Free radical injury Explanation: **Zinc oxide**
- **Zinc oxide** is a physical sunscreen that provides broad-spectrum protection by **blocking both UVA and UVB rays**.
- **UVA rays** are primarily responsible for **photoaging**, and physical blockers like zinc oxide are highly effective against them.
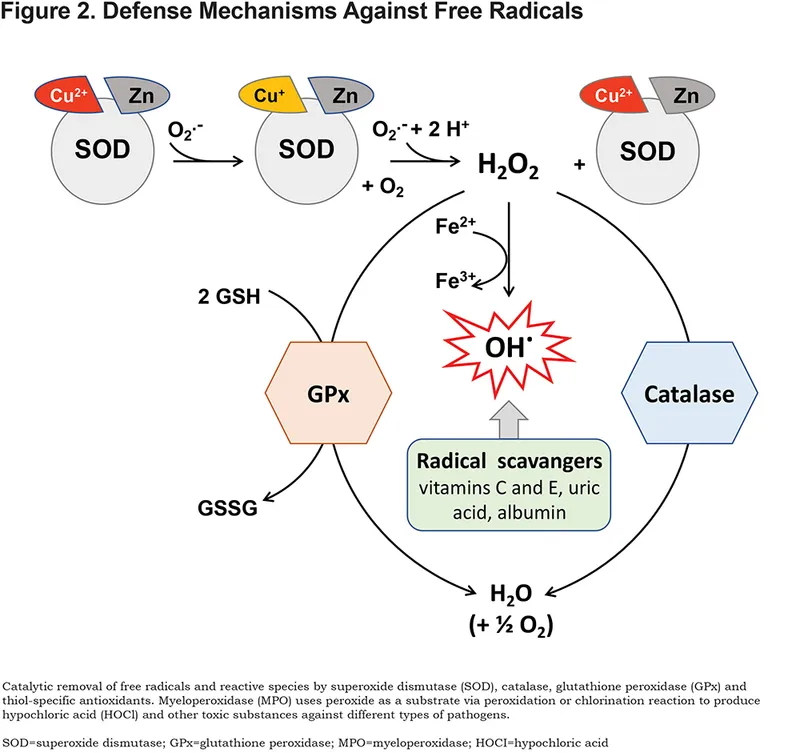
*Vitamin E*
- **Vitamin E** is an antioxidant that helps prevent cellular damage from free radicals, but it does **not provide direct protection against UV radiation** as a primary sunscreen ingredient.
- While commonly used in skincare for its **antioxidant properties**, it is not an active UV-blocking agent.
*Para-aminobenzoic acid*
- **Para-aminobenzoic acid (PABA)** is an older chemical sunscreen ingredient that primarily **blocks UVB rays**.
- It is often **associated with allergic reactions** and photosensitivity, and does not offer sufficient UVA protection for broad-spectrum coverage.
*Trimethoprim/sulfamethoxazole*
- **Trimethoprim/sulfamethoxazole** is an antibiotic combination used to treat various infections and has **no role in UV protection**.
- It is a medication and not an ingredient found in sunscreens for UV blocking.
*Trolamine salicylate*
- **Trolamine salicylate** is a topical analgesic ingredient often found in pain-relief creams and is **not an active sunscreen agent**.
- It has **no UV filtering properties** and does not protect against sun damage or photoaging.
Free radical injury US Medical PG Question 4: A 25-year-old woman presents to the ED with nausea, vomiting, diarrhea, abdominal pain, and hematemesis after ingesting large quantities of a drug. Which of the following pairs a drug overdose with the correct antidote for this scenario?
- A. Iron; deferoxamine (Correct Answer)
- B. Organophosphate; physostigmine
- C. Atropine; fomepizole
- D. Aspirin; N-acetylcysteine
- E. Acetaminophen; naloxone
Free radical injury Explanation: ***Iron; deferoxamine***
- The symptoms of **nausea, vomiting, diarrhea, abdominal pain, and hematemesis** are classic signs of **iron overdose**, which causes direct corrosive injury to the GI mucosa.
- **Deferoxamine** is a **chelating agent** specifically used to bind iron ions and facilitate their excretion, thus reversing iron toxicity.
*Organophosphate; physostigmine*
- **Organophosphate poisoning** presents with a **cholinergic crisis** (SLUDGE: salivation, lacrimation, urination, defecation, GI upset, emesis, miosis), but **hematemesis** is not a primary feature.
- **Physostigmine** is an acetylcholinesterase inhibitor used for atropine overdose, not organophosphate poisoning; **atropine** and **pralidoxime** are the antidotes for organophosphate.
*Atropine; fomepizole*
- **Atropine overdose** causes **anticholinergic symptoms** (dry mouth, blurred vision, tachycardia, urinary retention, delirium), not GI irritation and hematemesis.
- **Fomepizole** is an antidote for **methanol** or **ethylene glycol poisoning**, not atropine.
*Aspirin; N-acetylcysteine*
- **Aspirin overdose** (salicylate toxicity) results in **tinnitus, hyperventilation, metabolic acidosis, and altered mental status**, but **hematemesis** is less common than with iron.
- **N-acetylcysteine** is the antidote for acetaminophen overdose, not aspirin; aspirin overdose is treated with **alkalinization of urine** and **hemodialysis**.
*Acetaminophen; naloxone*
- **Acetaminophen overdose** primarily causes **hepatic toxicity**, initially presenting with non-specific GI symptoms, but **hematemesis** is atypical, and the main concern is liver damage.
- **Naloxone** is an opioid antagonist used to reverse opioid overdose, not acetaminophen.
Free radical injury US Medical PG Question 5: After being warned by the locals not to consume the freshwater, a group of American backpackers set off on a week-long hike into a region of the Ecuadorean Amazon forest known for large gold mines. The group of hikers stopped near a small stream and used the water they filtered from the stream to make dinner. Within the next half hour, the hikers began to experience headaches, vertigo, visual disturbances, confusion, tachycardia, and altered levels of consciousness. Which of the following enzymes was most likely inhibited in this group of hikers?
- A. NADH dehydrogenase
- B. ATP synthase
- C. Cytochrome c oxidase (Correct Answer)
- D. Cytochrome bc1 complex
- E. Succinate dehydrogenase
Free radical injury Explanation: ***Cytochrome c oxidase***
- The symptoms described (headaches, vertigo, visual disturbances, confusion, tachycardia, altered consciousness occurring within 30 minutes) are characteristic of **acute cyanide poisoning**.
- **Cyanide** is commonly found in water near **gold mining operations**, where it is used in the gold extraction process and can contaminate local water sources.
- **Cyanide** is a potent inhibitor of **cytochrome c oxidase** (Complex IV) in the electron transport chain, binding to the heme iron (Fe³⁺) and preventing oxygen utilization, leading to **histotoxic hypoxia**.
- This results in cellular energy failure, particularly affecting high-energy-demand organs like the brain and heart, explaining the acute neurological and cardiovascular symptoms.
*NADH dehydrogenase*
- While NADH dehydrogenase (Complex I) is a component of the electron transport chain, it is not the primary target of **cyanide poisoning**.
- Inhibitors of Complex I include rotenone and barbiturates, which cause different clinical presentations and do not produce the rapid onset of symptoms seen with cyanide.
*ATP synthase*
- **ATP synthase** (Complex V) synthesizes ATP using the proton gradient, but it is not directly inhibited by **cyanide**.
- Inhibitors of ATP synthase, such as oligomycin, prevent ATP synthesis by blocking the enzyme directly, whereas cyanide acts upstream at Complex IV.
*Cytochrome bc1 complex*
- The **cytochrome bc1 complex** (Complex III) is involved in electron transfer and proton pumping, but it is not the primary enzyme inhibited by **cyanide**.
- Inhibitors of Complex III include antimycin A, which would disrupt the electron transport chain but do not cause the characteristic rapid-onset symptoms of cyanide poisoning.
*Succinate dehydrogenase*
- **Succinate dehydrogenase** (Complex II) participates in both the citric acid cycle and the electron transport chain, but it is not targeted by **cyanide**.
- Inhibitors of Complex II, such as malonate, competitively block succinate oxidation but do not produce the acute systemic toxicity characteristic of cyanide poisoning.
Free radical injury US Medical PG Question 6: A 7-year-old boy is brought to the pediatrician by his parents for concern of general fatigue and recurrent abdominal pain. You learn that his medical history is otherwise unremarkable and that these symptoms started about 3 months ago after they moved to a different house. Based on clinical suspicion labs are obtained that reveal a microcytic anemia with high-normal levels of ferritin. Examination of a peripheral blood smear shows findings that are demonstrated in the figure provided. Which of the following is the most likely mechanism responsible for the anemia in this patient?
- A. Deletion of beta hemoglobin gene
- B. Chronic loss of blood through GI tract
- C. Inhibition of ALA dehydratase and ferrochelatase (Correct Answer)
- D. Inflammation due to occult abdominal malignancy
- E. X-linked mutation of ALA synthetase
Free radical injury Explanation: ***Inhibition of ALA dehydratase and ferrochelatase***
- The patient's symptoms (fatigue, abdominal pain), microcytic anemia with high-normal ferritin, and the presence of **basophilic stippling** in the peripheral blood smear (visible in the provided image as small, dark blue granules within red blood cells) are highly suggestive of **lead poisoning**.
- **Lead toxicity** primarily inhibits two key enzymes in heme synthesis: **aminolevulinate dehydratase (ALA dehydratase)** and **ferrochelatase**. This inhibition leads to impaired heme production, resulting in microcytic anemia, and accumulation of heme precursors, contributing to symptoms. The **high-normal ferritin** despite microcytic anemia is crucial as it rules out iron deficiency and points towards a heme synthesis disorder. The move to a new house 3 months ago suggests a new exposure to lead.
*Deletion of beta hemoglobin gene*
- This describes **beta-thalassemia**, which also causes microcytic anemia. However, beta-thalassemia is a genetic disorder usually presenting earlier in life or with a family history, and typically does not present with **abdominal pain** or **basophilic stippling** as its primary distinguishing feature in this context. Ferritin levels would also vary.
- While beta-thalassemia can cause microcytic anemia, a positive family history and specific hemoglobin electrophoresis findings would be expected, rather than recent onset symptoms linked to a new environment and prominent basophilic stippling.
*Chronic loss of blood through GI tract*
- **Chronic GI blood loss** would lead to **iron deficiency anemia**. While this would cause microcytic anemia, it would be characterized by **low ferritin levels** (as iron stores are depleted), not high-normal ferritin.
- The presence of basophilic stippling is not a typical finding in simple iron deficiency anemia.
*Inflammation due to occult abdominal malignancy*
- **Anemia of chronic disease** due to inflammation (e.g., from malignancy) can be microcytic or normocytic, but it is typically associated with **elevated ferritin** as ferritin is an acute phase reactant. However, this diagnosis would not explain the prominent **basophilic stippling** seen in the peripheral smear.
- Occult malignancy would likely present with other constitutional symptoms and the mechanism of anemia is related to a functional iron deficiency, not a direct inhibition of heme synthesis enzymes like in lead poisoning.
*X-linked mutation of ALA synthetase*
- An **X-linked mutation of ALA synthetase** (the rate-limiting enzyme in heme synthesis) is characteristic of **X-linked sideroblastic anemia**. This condition leads to ring sideroblasts in the bone marrow and typically presents with a microcytic or normocytic anemia.
- While it involves heme synthesis dysfunction, it's a genetic disorder, often congenital, and the sudden onset of symptoms linked to a new environment, along with the distinct feature of basophilic stippling, makes lead poisoning a more likely diagnosis in this specific clinical scenario. Furthermore, in sideroblastic anemia, iron accumulates in mitochondria, but the primary clinical picture and direct enzyme inhibition mechanism differ from lead poisoning.
Free radical injury US Medical PG Question 7: An 84-year-old man is brought to the physician by the staff of a group home where he resides because of worsening confusion and decreased urinary output. His nurse reports that the patient has not been drinking much for the last 3 days. Examination shows a decreased skin turgor and dry oral mucosa. His pulse is 105/min and blood pressure is 100/65 mm Hg. His serum creatinine is 3.1 mg/dL and a urea nitrogen is 42 mg/dL. Urine studies show multiple brownish granular casts. Which of the following processes is most likely involved in the pathogenesis of this patient's condition?
- A. Immune complex deposition in mesangium
- B. Leukocytic infiltration of renal interstitium
- C. Necrosis of renal papillae
- D. Necrosis of tubular epithelial cells (Correct Answer)
- E. Disruption of glomerular podocytes
Free radical injury Explanation: ***Necrosis of tubular epithelial cells***
- The patient presents with classic signs of **acute kidney injury (AKI)**, including confusion, decreased urinary output, decreased skin turgor, dry oral mucosa, tachycardia, hypotension, elevated creatinine (3.1 mg/dL), and urea nitrogen (42 mg/dL).
- The presence of **brownish granular casts** in the urine is highly suggestive of **acute tubular necrosis (ATN)**, secondary to ischemia caused by severe dehydration and hypoperfusion.
*Immune complex deposition in mesangium*
- This typically points to a **glomerular pathology**, such as IgA nephropathy or post-infectious glomerulonephritis.
- These conditions would usually present with **hematuria** and **proteinuria**, not necessarily brownish granular casts or the acute dehydration found here.
*Leukocytic infiltration of renal interstitium*
- This finding is characteristic of **acute interstitial nephritis**, which is often caused by drug hypersensitivity or infection.
- The clinical presentation with dehydration and granular casts is not typical for acute interstitial nephritis.
*Necrosis of renal papillae*
- **Renal papillary necrosis** is often associated with analgesic abuse, sickle cell disease, diabetes, or obstruction.
- While it can cause AKI, it typically presents with **flank pain** and **hematuria**, and the urine sediment would show ghost cells or fragments of necrotic papillae, not specifically brownish granular casts.
*Disruption of glomerular podocytes*
- **Podocyte disruption** is seen in primary glomerular diseases like minimal change disease or focal segmental glomerulosclerosis.
- These conditions primarily cause **nephrotic syndrome** (heavy proteinuria, edema), which is not the main presentation here.
Free radical injury US Medical PG Question 8: A 72-year-old female is brought to the emergency department by ambulance because she was unable to walk. She says that she cut her leg while falling about a week ago. Since then, the wound has started draining fluid and become progressively more painful. She is found to have necrotizing fasciitis and is taken emergently to the operating room. Histological examination of cells along the fascial planes reveal cells undergoing necrosis. Which of the following represents the earliest sign that a cell has progressed to irreversible damage in this patient?
- A. Fragmentation of the nucleus
- B. Membrane blebbing from organelles
- C. Chromatin dissolution and disappearance
- D. Ribosomal detachment from the endoplasmic reticulum
- E. Condensation of DNA into a basophilic mass (Correct Answer)
Free radical injury Explanation: ***Condensation of DNA into a basophilic mass***
- **Karyopyknosis**, or the **condensation of nuclear chromatin into a dense, shrunken mass**, is an early microscopic sign of irreversible cell injury leading to necrosis. It indicates the cell has committed to a death pathway.
- This nuclear change is characterized by the nucleus appearing as a **small, dense, and deeply basophilic structure** due to chromatin clumping.
*Fragmentation of the nucleus*
- **Karyorrhexis**, the fragmentation of the pyknotic nucleus, occurs *after* karyopyknosis, indicating a later stage of irreversible injury.
- This process involves the breakdown of the condensed nuclear fragments, leading to their subsequent disappearance.
*Membrane blebbing from organelles*
- **Membrane blebbing** can occur in both reversible and irreversible injury, but its presence on *organelles* specifically doesn't necessarily represent the *earliest* sign of irreversible damage compared to nuclear changes.
- While significant blebbing points towards severe damage, **nuclear changes** are often considered more definitive early markers of irreversible commitment.
*Chromatin dissolution and disappearance*
- **Karyolysis**, the dissolution and fading of the nucleus due to enzymatic degradation, represents a *later* stage of irreversible injury, occurring after karyopyknosis and karyorrhexis.
- In this stage, the nucleus eventually completely disappears, leaving only an anucleated ghost cell.
*Ribosomal detachment from the endoplasmic reticulum*
- **Ribosomal detachment** from the endoplasmic reticulum is an early sign of **reversible cell injury**, leading to decreased protein synthesis.
- It indicates initial cellular stress but not necessarily a commitment to irreversible damage or necrosis.
Free radical injury US Medical PG Question 9: An 87-year-old woman is admitted to the intensive care unit after a neighbor found her lying on the floor at her home. Her respirations are 13/min and shallow. Despite appropriate therapy, the patient dies. Gross examination of the brain at autopsy shows neovascularization and liquefactive necrosis without cavitation in the distribution of the left middle cerebral artery. Histological examination of a brain tissue sample from the left temporal lobe shows proliferation of neural cells that stain positive for glial fibrillary acidic protein. Based on these findings, approximately how much time has most likely passed since the initial injury in this patient?
- A. 2 days
- B. 2 hours
- C. 10 days (Correct Answer)
- D. 25 days
- E. 12 hours
Free radical injury Explanation: ***10 days***
- **Neovascularization** and the absence of cavitation with **liquefactive necrosis** are indicative of a subacute phase of ischemic injury, typically seen around 1-3 weeks.
- The proliferation of **glial fibrillary acidic protein (GFAP)** positive neural cells (astrocytes) signifies **astrogliosis**, a repair response common after approximately one week, peaking around 2-3 weeks post-injury.
*2 days*
- At 2 days, the primary histological findings would be **neutrophilic infiltration** and initial stages of neuronal necrosis.
- **Neovascularization** and significant astrogliosis are generally not prominent until later in the recovery phase.
*2 hours*
- Within 2 hours, there would be minimal to no gross changes, and microscopic examination might show only **red neurons** (eosinophilic neurons with pyknotic nuclei) reflecting early irreversible neuronal damage.
- There would be no signs of inflammation, tissue breakdown, or repair processes like neovascularization or astrogliosis.
*25 days*
- By 25 days (approximately 3-4 weeks), **cavitation** with a **cystic astrocytic glial scar** would likely be prominent at the site of liquefactive necrosis, which is explicitly stated as absent in the question.
- While astrogliosis would still be present, the lack of cavitation points to an earlier stage of repair.
*12 hours*
- At 12 hours, gross changes are typically still absent or subtle, and microscopic findings would primarily involve **edema** and early signs of neuronal injury (e.g., changes in Nissl bodies, mild eosinophilia).
- Inflammatory cell infiltration and reparative processes like neovascularization or astrogliosis would not yet be significant.
Free radical injury US Medical PG Question 10: A 34-year-old woman comes to the physician a week after noticing a lump in her left breast. Three months ago, she was discharged from the hospital after treatment of multiple injuries sustained in a motor vehicle collision. Her only medication is an oral contraceptive. Her mother died of ovarian cancer. Examination shows a 2.5-cm, nontender mass in the upper outer quadrant of the left breast. Mammography shows a circumscribed radiolucent lesion with a rim of peripheral calcification. A photomicrograph of tissue from a biopsy of the mass is shown. Which of the following is the most likely cause of the breast swelling?
- A. Defect in DNA repair
- B. Obstruction of lactiferous ducts
- C. Stimulation of estrogen receptors
- D. Thrombophlebitis of subcutaneous veins
- E. Release of cytoplasmic triglycerides (Correct Answer)
Free radical injury Explanation: ***Release of cytoplasmic triglycerides***
- This patient's history of **trauma** followed by a new breast lump and mammographic findings of a **circumscribed radiolucent lesion with peripheral calcification** are classic for **fat necrosis**. The image shows necrotic fat cells, inflammatory infiltrates, and foamy macrophages, consistent with fat necrosis.
- Fat necrosis occurs when **adipocytes** are damaged, causing the release of **triglycerides** and free fatty acids. These then incite an inflammatory response, followed by calcification and fibrosis.
*Defect in DNA repair*
- A defect in DNA repair is associated with an increased risk of **malignancy**, such as breast cancer, especially given the family history of ovarian cancer (BRCA gene mutations). However, the histologic image and the description of a **radiolucent lesion with rim calcification** are not characteristic of malignancy.
- While the family history is relevant for cancer risk, the clinical and histological findings point away from a primary malignancy and towards a benign reactive process.
*Obstruction of lactiferous ducts*
- Obstruction of lactiferous ducts typically leads to conditions like **mastitis**, **duct ectasia**, or **galactocele**. These would present with different radiographic features, often with inflammation or fluid-filled cysts, and different histological patterns.
- The image does not show features of ductal obstruction, such as dilated ducts, inspissated secretions, or periductal inflammation characteristic of duct ectasia.
*Stimulation of estrogen receptors*
- Stimulation of estrogen receptors is relevant in conditions like **fibroadenoma**, **fibrocystic changes**, or certain types of **breast cancer**. While the patient is on oral contraceptives (estrogenic), the clinical picture and biopsy findings are not consistent with these estrogen-mediated conditions.
- Fibroadenomas often appear as well-defined masses on mammography but histologically consist of glandular and stromal proliferation, which is not seen here. Fibrocystic changes involve cysts and fibrosis.
*Thrombophlebitis of subcutaneous veins*
- Thrombophlebitis of subcutaneous veins, also known as **Mondor's disease**, presents as a palpable cord-like structure with pain and tenderness localized along the affected vein. It typically resolves spontaneously.
- This condition is unlikely given the description of a **2.5-cm, nontender mass** and the specific histological findings of necrotic fat and inflammation, which are not characteristic of venous thrombosis.
More Free radical injury US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.