Cellular adaptations (atrophy, hypertrophy) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cellular adaptations (atrophy, hypertrophy). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 1: A 45-year-old man presents with a hereditary condition affecting iron metabolism. The condition is caused by mutations in a gene that normally stimulates hepatic production of hepcidin, a hormone that downregulates iron absorption by inhibiting ferroportin (an iron transporter) on enterocytes. Due to this genetic defect, the patient has developed iron overload. He presents with skin hyperpigmentation, fatigue, joint pain, and diabetes mellitus. Laboratory studies show elevated serum ferritin and transferrin saturation. The patient is also developing early signs of cardiovascular complications from iron deposition. What would be the first cardiac manifestation in this patient?
- A. Preload: decreased, cardiac contractility: unchanged, afterload: increased (Correct Answer)
- B. Preload: decreased, cardiac contractility: decreased, afterload: decreased
- C. Preload: increased, cardiac contractility: increased, afterload: increased
- D. Preload: increased, cardiac contractility: decreased, afterload: increased
- E. Preload: increased, cardiac contractility: increased, afterload: decreased
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Preload: decreased, cardiac contractility: unchanged, afterload: increased***
- The first cardiac manifestation of **hereditary hemochromatosis** is typically **restrictive cardiomyopathy**, where iron deposition causes myocardial stiffening and impaired diastolic relaxation.
- In early restrictive disease, the stiff ventricle has **impaired filling**, leading to **reduced end-diastolic volume (decreased preload)** despite elevated filling pressures.
- **Systolic contractility remains initially unchanged** as the primary defect is diastolic dysfunction, not systolic failure.
- **Afterload is increased** due to compensatory peripheral vasoconstriction and reduced stroke volume triggering baroreceptor responses.
- This pattern reflects pure diastolic dysfunction with preserved systolic function (HFpEF pattern).
*Preload: decreased, cardiac contractility: decreased, afterload: decreased*
- While preload may be decreased, **reduced afterload** is inconsistent with restrictive cardiomyopathy, which typically shows compensatory vasoconstriction, not vasodilation.
- **Decreased contractility** occurs in later stages when iron toxicity directly damages myofibrils, progressing to dilated cardiomyopathy, but is not the initial presentation.
*Preload: increased, cardiac contractility: increased, afterload: increased*
- **Increased contractility** is not seen in iron-induced cardiac disease; iron deposition impairs, rather than enhances, myocardial function.
- This pattern would suggest a hyperdynamic state (e.g., sepsis, hyperthyroidism) which is unrelated to hemochromatosis.
*Preload: increased, cardiac contractility: decreased, afterload: increased*
- This combination describes **advanced or dilated cardiomyopathy** where the heart fails to pump effectively, causing volume overload and elevated preload.
- While this can occur in later stages of hemochromatosis, the **first cardiac manifestation** is restrictive (diastolic) dysfunction, not dilated (systolic) dysfunction.
- Decreased contractility develops after prolonged iron exposure damages contractile proteins.
*Preload: increased, cardiac contractility: increased, afterload: decreased*
- This pattern describes hyperdynamic circulation with reduced systemic vascular resistance, which does not occur in iron overload cardiomyopathy.
- Iron deposition causes myocardial stiffness and eventual contractile dysfunction, never enhanced contractility.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 2: A 12-year-old boy is brought to the physician because of difficulty in walking for 5 months. His mother reports that he has trouble keeping his balance and walking without support. Over the past year, he has started to have difficulty seeing in the dark and his hearing has been impaired. Examination shows marked scaling of the skin on the face and feet and a shortened 4th toe. Muscle strength is 3/5 in the lower extremities and 4/5 in the upper extremities. Sensation to pinprick is symmetrically decreased over the legs. Fundoscopy shows peripheral pigment deposits and retinal atrophy. His serum phytanic acid concentration is markedly elevated. The patient's condition is most likely caused by a defect in which of the following cellular structures?
- A. Proteasomes
- B. Peroxisomes (Correct Answer)
- C. Smooth endoplasmic reticulum
- D. Mitochondria
- E. Myofilaments
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Peroxisomes***
- The constellation of symptoms including **difficulty walking and maintaining balance**, **impaired night vision and hearing**, **scaling skin**, **distal muscle weakness**, **ataxia**, **peripheral neuropathy**, **pigmentary retinopathy**, and **markedly elevated serum phytanic acid** is characteristic of **Refsum disease**.
- **Refsum disease** is an autosomal recessive disorder caused by a defect in **peroxisomal alpha-oxidation** (specifically phytanoyl-CoA hydroxylase deficiency), leading to the accumulation of phytanic acid in tissues.
- Phytanic acid is a branched-chain fatty acid derived from dietary sources (dairy products, ruminant fats) that cannot undergo beta-oxidation and requires alpha-oxidation in peroxisomes.
*Proteasomes*
- **Proteasomes** are responsible for the degradation of ubiquitinated proteins, important for cellular protein homeostasis.
- Defects in proteasomes are associated with various conditions like **neurodegenerative diseases** (e.g., Parkinson's), but not with the specific symptoms of phytanic acid accumulation.
*Smooth endoplasmic reticulum*
- The **smooth endoplasmic reticulum** is involved in **lipid synthesis**, detoxification, and calcium storage.
- While lipid metabolism is affected in Refsum disease, the primary defect is in the degradation of branched-chain fatty acids like phytanic acid, which occurs in **peroxisomes**, not the smooth ER.
*Mitochondria*
- **Mitochondria** are the primary sites of **ATP production** through oxidative phosphorylation and are involved in fatty acid beta-oxidation.
- While some metabolic disorders affect mitochondria, **phytanic acid accumulation** specifically points to a peroxisomal defect because phytanic acid cannot undergo beta-oxidation due to its 3-methyl branch and requires alpha-oxidation, which is a peroxisomal process.
*Myofilaments*
- **Myofilaments** (actin and myosin) are the contractile proteins within muscle cells.
- While muscle weakness is a symptom, the underlying cause is not a primary defect in myofilaments themselves, but rather the **neurological and systemic effects** of phytanic acid accumulation affecting peripheral nerves and muscle innervation.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 3: A 70-year-old man presented to a medical clinic for a routine follow-up. He has had hypertension for 20 years and is currently on multiple anti-hypertensive medications. The blood pressure is 150/100 mm Hg. The remainder of the examinations were within normal limits. Echocardiography showed some changes in the left ventricle. What is the most likely reason for the change?
- A. Disordered growth of the cardiac cells
- B. Increase in number of normal cardiac cells
- C. Replacement of cardiac cells into stronger red fiber skeletal cells
- D. Decrease in cardiac cell size
- E. Increase in cardiac cell size (Correct Answer)
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Increase in cardiac cell size***
- Chronic **hypertension** increases the afterload on the left ventricle, causing the cardiac muscle cells (myocytes) to **hypertrophy** (increase in size) to generate greater force to eject blood.
- This adaptive change is a compensatory mechanism to maintain cardiac output against increased systemic vascular resistance.
*Disordered growth of the cardiac cells*
- This description typically refers to **dysplasia**, which involves abnormal cell growth and organization, often raising suspicion for pre-cancerous conditions.
- Cardiac muscle cells, being terminally differentiated, do not commonly undergo dysplastic changes in response to hypertension.
*Increase in number of normal cardiac cells*
- An increase in the number of cells is known as **hyperplasia**, a process that occurs in tissues with high regenerative capacity.
- Mature **cardiac myocytes** have very limited proliferative capacity, so an increase in their number is not the primary mechanism of ventricular adaptation to hypertension.
*Replacement of cardiac cells into stronger red fiber skeletal cells*
- This scenario describes **metaplasia**, where one differentiated cell type is replaced by another.
- Such a transformation from cardiac muscle to skeletal muscle cells does not occur in response to hypertension and is biologically impossible within the heart.
*Decrease in cardiac cell size*
- A decrease in cell size, or **atrophy**, occurs due to decreased workload, nutrition, or hormonal stimulation.
- In hypertension, the workload on the heart is significantly increased, leading to hypertrophy rather than atrophy.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 4: A 19-year-old Caucasian male collapsed from sudden cardiac arrest while playing in a college basketball game. Attempts at resuscitation were unsuccessful. Post-mortem pathologic and histologic examination found asymmetric left ventricular hypertrophy and myocardial disarray. Assuming this was an inherited condition, the relevant gene most likely affects which of the following structures?
- A. Cardiac cell sarcomere proteins (Correct Answer)
- B. Membrane potassium channel proteins
- C. Membrane sodium channels
- D. Ryanodine receptors
- E. Autoimmune beta-cell antibodies
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Cardiac cell sarcomere proteins***
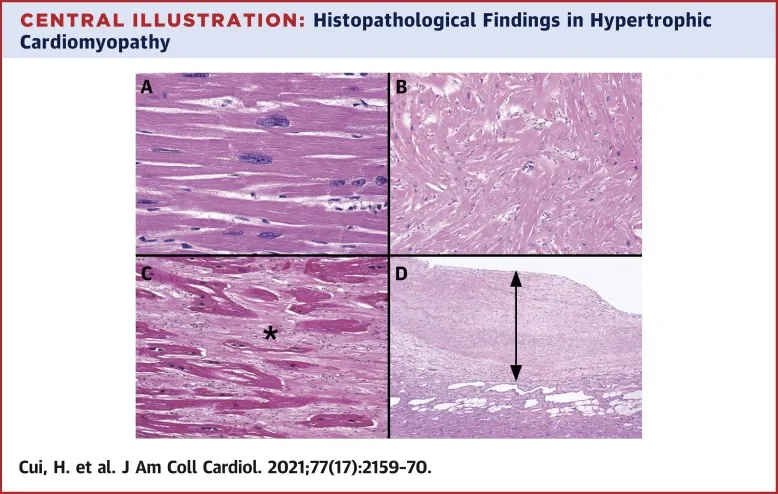
- The clinical presentation of **sudden cardiac arrest** in a young athlete, along with post-mortem findings of **asymmetric left ventricular hypertrophy** and **myocardial disarray**, are classic for **hypertrophic cardiomyopathy (HCM)**.
- HCM is most commonly caused by mutations in genes encoding **sarcomeric proteins**, leading to abnormal myocardial structure and function.
*Membrane potassium channel proteins*
- Mutations in voltage-gated **potassium channels** are typically associated with cardiac arrhythmias such as **long QT syndrome** and **short QT syndrome**.
- These conditions primarily affect cardiac electrical activity and do not directly cause asymmetric left ventricular hypertrophy or myocardial disarray.
*Membrane sodium channels*
- Defects in **sodium channels** are predominantly linked to conditions like **Brugada syndrome** and certain forms of **long QT syndrome**.
- These channelopathies are characterized by specific ECG abnormalities and increased risk of sudden cardiac death due to arrhythmias, but not structural heart disease like HCM.
*Ryanodine receptors*
- Mutations in the **ryanodine receptor 2 (RyR2) gene** are associated with **catecholaminergic polymorphic ventricular tachycardia (CPVT)**.
- CPVT causes life-threatening arrhythmias, particularly during exercise or emotional stress, but it does not typically present with the structural cardiac abnormalities of HCM.
*Autoimmune beta-cell antibodies*
- **Autoimmune beta-cell antibodies** are characteristic of **Type 1 diabetes mellitus**, an autoimmune disease affecting the pancreas.
- These antibodies are unrelated to cardiac structural or electrical abnormalities and would not explain sudden cardiac arrest with left ventricular hypertrophy and myocardial disarray.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 5: An 85-year-old woman presents to her physician with complaints of significant weakness and weight loss. She recently has been diagnosed with stage IV breast cancer for which she currently is receiving treatment. She mentions that, despite taking a diet rich in protein and calories, she continues to lose weight. On physical examination, her vital signs are stable, but muscle wasting is clearly evident in her upper limbs, lower limbs, and face. The physician explains to her that her advanced cancer is the most important cause for the weight loss and muscle wasting. This cachexia is mediated by the proteolysis-inducing factor released from cancer cells. Which of the following effects is produced by this factor?
- A. Activation of hormone-sensitive lipase in adipose tissue
- B. Suppression of the appetite center in the hypothalamus
- C. Stimulation of apoptosis
- D. Increased release of tumor necrosis factor (TNF) from macrophages
- E. Activation of NF-κB (Correct Answer)
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Activation of NF-κB***
- Proteolysis-inducing factor (PIF) released from cancer cells leads to the **activation of NF-κB** in muscle cells.
- This activation results in an increased expression of **ubiquitin-proteasome pathway** components, which promotes protein degradation and muscle wasting in **cancer cachexia**.
*Activation of hormone-sensitive lipase in adipose tissue*
- While **cachexia** involves fat loss, PIF's primary effect on muscle wasting is through protein degradation, not direct activation of hormone-sensitive lipase.
- **Hormone-sensitive lipase** is mainly activated by catecholamines and cortisol during stress.
*Suppression of the appetite center in the hypothalamus*
- **Anorexia** (loss of appetite) is a component of cachexia, but PIF directly mediates muscle breakdown rather than directly suppressing hypothalamic appetite centers.
- Various cytokines like IL-1, IL-6, and TNF-α, as well as neurotransmitters, influence appetite.
*Stimulation of apoptosis*
- While **apoptosis** can contribute to cell loss in various contexts, PIF's main mechanism for muscle wasting is through the **ubiquitin-proteasome system**, not primarily by inducing apoptosis.
- Muscle atrophy in cachexia is often characterized more by protein breakdown than widespread myocyte death via apoptosis.
*Increased release of tumor necrosis factor (TNF) from macrophages*
- **TNF-α** is a major cytokine implicated in cachexia, but PIF itself is an independent factor released by tumor cells.
- PIF can act synergistically with cytokines like TNF-α to exacerbate muscle wasting, but it does not primarily cause the release of TNF-α from macrophages.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 6: A 48-year-old man has smoked approximately 3 packs of cigarettes per day for the past 12 years. Which of the following pathologic changes is most likely to occur in his bronchial epithelium?
- A. Metaplasia (Correct Answer)
- B. Hyperplasia
- C. Hypertrophy
- D. Dysplasia
- E. Atrophy
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Metaplasia***
- Chronic irritation from **cigarette smoking** can cause the **bronchial epithelium** to change from ciliated columnar to stratified squamous, a process known as **metaplasia**.
- This adaptation makes the tissue more resistant to injury but results in the loss of important protective functions like **mucociliary clearance**.
*Hyperplasia*
- **Hyperplasia** involves an increase in the number of cells in a tissue or organ, often in response to increased demand or chronic stimulation.
- While smoking can cause hyperplasia of goblet cells and mucous glands in the bronchi, the direct epithelial change in response to chronic irritation is more specifically **metaplasia**.
*Hypertrophy*
- **Hypertrophy** is an increase in the size of individual cells, leading to an increase in the size of the organ or tissue.
- This is not the primary adaptive change seen in the bronchial epithelium in response to chronic smoking; instead, cells change their type.
*Dysplasia*
- **Dysplasia** refers to disorderly cell growth, often characterized by variations in cell size, shape, and organization; it is considered a precursor to cancer.
- While chronic smoking can eventually lead to dysplasia and then carcinoma, the initial and most common adaptive change in the bronchial epithelium is **metaplasia**.
*Atrophy*
- **Atrophy** is a decrease in cell size or number, leading to a reduction in the size of an organ or tissue, usually due to decreased workload, nutrition, or blood supply.
- This is not a typical response of the bronchial epithelium to chronic irritation from smoking, which tends to induce proliferative or adaptive changes.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 7: As part of a clinical research study, microscopic analysis of tissues obtained from surgical specimens is performed. Some of these tissues have microscopic findings of an increase in the size of numerous cells within the tissue with an increase in the amount of cytoplasm, but the nuclei are uniform in size. Which of the following processes shows such microscopic findings?
- A. Liver following partial resection
- B. Female breasts at puberty
- C. Ovaries following menopause
- D. Uterine myometrium in pregnancy (Correct Answer)
- E. Cervix with chronic inflammation
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Uterine myometrium in pregnancy***
- During pregnancy, the uterine myometrial cells undergo significant **hypertrophy** (increase in cell size) in response to hormonal stimulation, primarily *estrogen* and *progesterone*.
- This leads to a marked increase in the amount of **cytoplasm** and overall cell size, while maintaining relatively **uniform nuclei**, which precisely matches the microscopic findings described.
- The smooth muscle cells can increase **10-40 fold** in size, making this the classic example of physiologic hypertrophy.
- Note: Hyperplasia (increased cell number) also occurs but is less prominent; the microscopic findings described emphasize the hypertrophic changes.
*Liver following partial resection*
- The liver primarily undergoes **hyperplasia** (increase in cell number) to regenerate following partial resection.
- While some hypertrophy occurs, the dominant microscopic finding is an increase in hepatocyte **number** through proliferation rather than a marked increase in individual cell size and cytoplasm as the primary feature.
*Female breasts at puberty*
- Breast development at puberty involves both **hyperplasia** of the glandular epithelium and ductal structures and **adipose tissue deposition**, driven by *estrogen* and *progesterone*.
- The findings described (marked increase in cell size and cytoplasm with uniform nuclei) are more characteristic of the extreme cell hypertrophy seen in the gravid uterus rather than the mixed growth and differentiation patterns of pubertal breast development.
*Ovaries following menopause*
- Following menopause, the ovaries undergo **atrophy**, meaning a decrease in size and cellular activity due to declining hormonal production.
- This process involves a **decrease in cell size** and number, which is the opposite of the microscopic findings described in the question.
*Cervix with chronic inflammation*
- Chronic inflammation in the cervix can cause various changes, including **squamous metaplasia** (transformation of columnar epithelium to squamous epithelium) or an influx of inflammatory cells.
- While there might be some reactive cellular changes, it does not typically involve a widespread, uniform increase in cell size and cytoplasm within existing cells as described, but rather a change in cell type or infiltration by inflammatory cells.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 8: A 52-year-old female was found upon mammography to have branching calcifications in the right lower breast. Physical exam revealed a palpable nodularity in the same location. A tissue biopsy was taken from the lesion, and the pathology report diagnosed the lesion as comedocarcinoma. Which of the following histological findings is most likely present in the lesion?
- A. Disordered glandular cells invading the ductal basement membrane
- B. Pleomorphic cells surrounding areas of comedonecrosis (Correct Answer)
- C. Extensive lymphocytic infiltrate
- D. Halo cells in epidermal tissue
- E. Orderly rows of cells surrounding lobules
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Pleomorphic cells surrounding areas of comedonecrosis***
- **Comedocarcinoma** specifically refers to a high-grade subtype of **ductal carcinoma in situ (DCIS)** characterized by **central necrosis (comedonecrosis)** surrounded by **pleomorphic epithelial cells**.
- The presence of branching calcifications on mammography is also a classic sign often associated with **comedonecrosis** within the ducts.
*Disordered glandular cells invading the ductal basement membrane*
- This description is characteristic of **invasive ductal carcinoma**, where malignant cells breach the basement membrane and infiltrate surrounding tissues, which is not stated in the diagnosis of comedocarcinoma.
- Comedocarcinoma is a form of **carcinoma in situ**, meaning the cancerous cells are confined within the ductal system and have not yet invaded the basement membrane.
*Extensive lymphocytic infiltrate*
- While immune cell infiltrates can be seen in various cancers, an **extensive lymphocytic infiltrate** is more characteristic of conditions like **medullary carcinoma** of the breast or specific immune responses, not a defining feature of comedocarcinoma.
- It does not directly relate to the characteristic histological appearance of **comedonecrosis** and **pleomorphic cells** seen in comedocarcinoma.
*Halo cells in epidermal tissue*
- **Halo cells** (koilocytes) are characteristic of **human papillomavirus (HPV) infection** and are found in **cervical or anal squamous lesions**, not typically in breast tissue.
- This finding is completely unrelated to breast pathology and specifically to comedocarcinoma.
*Orderly rows of cells surrounding lobules*
- This description is more indicative of **lobular carcinoma in situ (LCIS)** or some benign proliferative lesions, where cellular architecture tends to maintain some order.
- **Comedocarcinoma** involves disordered, pleomorphic cells within ducts, often with central necrosis, and does not form orderly rows surrounding lobules.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 9: A 16-year-old boy is brought to the emergency department 20 minutes after collapsing while playing basketball. There is no personal or family history of serious illness. On arrival, there is no palpable pulse and no respiratory effort is seen. He is declared dead. The family agrees to an autopsy. Which of the following is most likely to be found in this patient?
- A. Defect in the atrial septum
- B. Interventricular septal hypertrophy (Correct Answer)
- C. Pericardial fluid collection
- D. Postductal narrowing of the aorta
- E. Atheromatous plaque rupture
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Interventricular septal hypertrophy***
- This presentation is highly suggestive of **hypertrophic cardiomyopathy (HCM)**, which is characterized by **left ventricular hypertrophy**, especially of the interventricular septum, leading to outflow obstruction and sudden cardiac arrest, particularly in young athletes.
- **Sudden collapse during strenuous exercise** in a young, otherwise healthy individual with no prior history of illness is a classic presentation of HCM.
*Defect in the atrial septum*
- An **atrial septal defect (ASD)** typically presents with a **murmur** and may lead to heart failure or pulmonary hypertension later in life, but it is an unlikely cause of sudden death in an adolescent during exercise.
- While it can cause cardiac symptoms, sudden collapse without prior symptoms is uncommon, and the primary pathological finding would be a hole, not hypertrophy.
*Pericardial fluid collection*
- A significant pericardial fluid collection that causes sudden collapse would indicate **pericardial tamponade**, which is usually associated with clear signs of circulatory collapse (e.g., **Beck's triad** - muffled heart sounds, jugular venous distension, hypotension) and is often due to trauma, infection, or malignancy, which are not suggested here.
- The sudden, unheralded nature of collapse during exercise points away from conditions that typically have more gradual onset or preceding symptoms.
*Postductal narrowing of the aorta*
- **Coarctation of the aorta** can cause hypertension and may lead to heart failure or aortic rupture, but it typically presents with **blood pressure discrepancies** between the upper and lower extremities and a characteristic murmur, not sudden cardiac death during exercise without prior symptoms.
- While it can be severe, sudden death usually results from complications like aortic dissection or rupture after a period of untreated hypertension, not acute collapse in a seemingly healthy individual.
*Atheromatous plaque rupture*
- **Atherosclerosis** and plaque rupture are the underlying cause of most **myocardial infarctions** in adults, but they are extremely rare in a 16-year-old without significant risk factors or a history of lipid disorders.
- The patient's age and lack of predisposing factors make this an improbable finding for sudden cardiac death.
Cellular adaptations (atrophy, hypertrophy) US Medical PG Question 10: A 60-year-old African American woman presents to her family physician with shortness of breath on exertion. She also describes shortness of breath when she lies down to go to bed at night, as well as recent swelling in her ankles. Past medical history is significant for long-standing hypertension, for which she takes amlodipine and lisinopril. Her temperature is 36.8°C (98.2°F), the heart rate is 90/min, the respiratory rate is 15/min, and the blood pressure is 135/80 mm Hg. The physical exam is significant for JVD, lower extremity pitting edema, laterally displaced PMI, left ventricular heave, bilateral pulmonary crackles, and an S4 heart sound. Chest X-ray demonstrates pulmonary vascular congestion, Kerley B lines, and cardiomegaly. Echocardiogram demonstrates a preserved ejection fraction. Kidney biopsy would likely demonstrate which of the following?
- A. Thinning of the intima and media
- B. Onion-skinning
- C. Nodular sclerosis
- D. Intimal thickening and medial hypertrophy (Correct Answer)
- E. Fibrinoid necrosis
Cellular adaptations (atrophy, hypertrophy) Explanation: ***Intimal thickening and medial hypertrophy***
* The patient's presentation of **heart failure with preserved ejection fraction (HFpEF)**, long-standing **hypertension**, and findings like left ventricular heave and S4 heart sound strongly suggest **hypertensive cardiomyopathy**, which in turn causes **hypertensive nephrosclerosis**.
* **Hypertensive nephrosclerosis** is characterized by **intimal thickening** and **medial hypertrophy** of renal arterioles, leading to **ischemia** and atrophy of glomeruli and tubules.
*Thinning of the intima and media*
* This is not a characteristic pathological change seen in hypertensive nephrosclerosis.
* In hypertension, the vessel walls typically undergo thickening due to **hypertrophy** and **hyperplasia** of smooth muscle cells and increased extracellular matrix, not thinning.
*Onion-skinning*
* **"Onion-skinning"** is a hallmark feature of **malignant hypertension**, characterized by concentric laminar thickening of the arteriolar walls.
* The patient's blood pressure (135/80 mmHg) is not consistent with malignant hypertension, which would typically involve much higher blood pressure readings.
*Nodular sclerosis*
* **Nodular sclerosis** (also known as **Kimmelstiel-Wilson lesions**) is characteristic of **diabetic nephropathy**, not primarily hypertensive nephrosclerosis.
* While diabetes and hypertension often co-exist, the prompt in this case points more directly to long-standing hypertension as the primary cause of renal damage.
*Fibrinoid necrosis*
* **Fibrinoid necrosis** of arterioles is also associated with **malignant hypertension** and some forms of vasculitis.
* This patient's blood pressure is controlled (135/80 mmHg) and does not indicate the severe, rapid increase in blood pressure seen in malignant hypertension.
More Cellular adaptations (atrophy, hypertrophy) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.