Cell injury

On this page
🔬 The Cellular Damage Spectrum: From Stress to Destruction
Cells face constant threats-ischemia, toxins, infections, trauma-and their responses determine whether tissues adapt, survive, or die. You'll discover how ATP depletion triggers metabolic collapse, why calcium influx becomes catastrophic, and how membrane damage seals a cell's fate. By recognizing injury patterns from reversible stress to irreversible necrosis and apoptosis, you'll connect molecular mechanisms to clinical presentations and learn when intervention can rescue dying tissue. This foundation transforms abstract pathology into actionable clinical reasoning across every organ system you'll encounter.
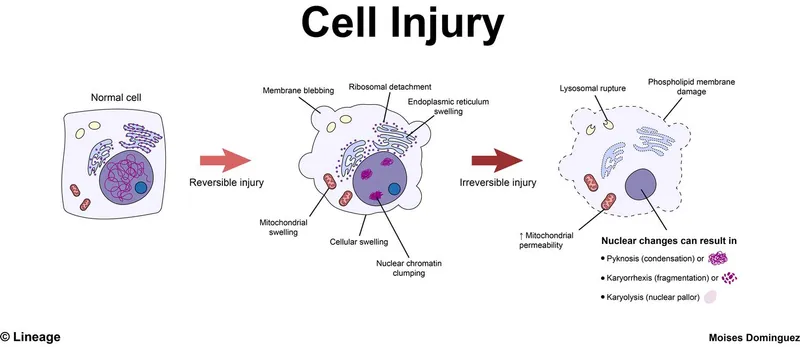
The cellular injury spectrum encompasses a continuum from mild stress responses that trigger protective adaptations, through severe reversible injury with potential for recovery, to irreversible damage culminating in cell death. This progression involves specific molecular checkpoints where intervention can alter outcomes.
📌 Remember: RAIN - Reversible injury shows ATP depletion, Increased calcium, Nuclear changes (chromatin clumping)
Cellular stress responses activate within seconds of injury onset, while irreversible changes typically occur after 30-60 minutes of severe stress. The point of no return occurs when mitochondrial membrane permeability becomes irreversibly compromised, leading to >50% ATP depletion and uncontrolled calcium influx.
⭐ Clinical Pearl: Myocardial cells become irreversibly injured after 20-40 minutes of complete ischemia, while neurons suffer irreversible damage within 3-5 minutes of oxygen deprivation
| Cell Type | Reversible Injury Threshold | Irreversible Injury Time | ATP Depletion Level | Calcium Increase | Recovery Potential |
|---|---|---|---|---|---|
| Neurons | 2-3 minutes | 3-5 minutes | >80% | 10-fold | Minimal |
| Cardiomyocytes | 15-20 minutes | 20-40 minutes | >70% | 5-fold | Moderate |
| Hepatocytes | 30-45 minutes | 60-90 minutes | >60% | 3-fold | High |
| Skeletal muscle | 60-120 minutes | 2-4 hours | >50% | 2-fold | Excellent |
| Fibroblasts | 2-4 hours | 6-8 hours | >40% | 2-fold | Excellent |
💡 Master This: Cellular injury severity correlates directly with ATP depletion percentage - <25% depletion allows full recovery, 25-50% causes reversible injury, >50% triggers irreversible damage
Understanding cellular injury mechanisms transforms clinical pattern recognition, enabling prediction of tissue recovery potential and optimal intervention timing across all medical specialties.
🔬 The Cellular Damage Spectrum: From Stress to Destruction
⚡ The Energy Crisis: ATP Depletion and Metabolic Collapse
Energy metabolism disruption follows a predictable sequence: oxidative phosphorylation failure → glycolytic compensation → lactate accumulation → pH reduction → enzyme dysfunction → membrane pump failure. This cascade occurs within minutes of severe injury onset.
📌 Remember: GLAD - Glycolysis increases, Lactate accumulates, ATP depletes, Damage becomes irreversible
The ATP/ADP ratio normally maintained at 10:1 drops to 1:1 during severe stress, triggering AMP-activated protein kinase (AMPK) activation within 30 seconds. AMPK activation initiates energy conservation mechanisms but cannot prevent injury progression if ATP synthesis remains compromised.
| Metabolic Parameter | Normal Value | Mild Stress | Severe Stress | Critical Level | Recovery Time |
|---|---|---|---|---|---|
| ATP concentration | 3-5 mM | 2-3 mM | 1-2 mM | <0.5 mM | 2-6 hours |
| ATP/ADP ratio | 10:1 | 5:1 | 2:1 | 1:1 | 4-8 hours |
| Lactate levels | 1-2 mM | 3-5 mM | 8-15 mM | >20 mM | 6-12 hours |
| Intracellular pH | 7.2 | 7.0 | 6.8 | <6.5 | 8-24 hours |
| Oxygen consumption | 100% | 150% | 50% | <10% | 12-48 hours |
Mitochondrial dysfunction represents the critical bottleneck in energy metabolism, with electron transport chain disruption reducing ATP synthesis by >80% within minutes of severe injury. Complex I and III represent the most vulnerable components, with reactive oxygen species generation increasing 10-fold during dysfunction.
💡 Master This: ATP depletion triggers Na+/K+-ATPase pump failure, causing cellular swelling within 5-10 minutes - the earliest morphological sign of cellular injury
Energy crisis resolution requires mitochondrial membrane potential restoration and oxidative phosphorylation recovery, processes that can take hours to days depending on injury severity and cellular repair capacity.
⚡ The Energy Crisis: ATP Depletion and Metabolic Collapse
🌊 Calcium Catastrophe: The Cellular Flood Gates
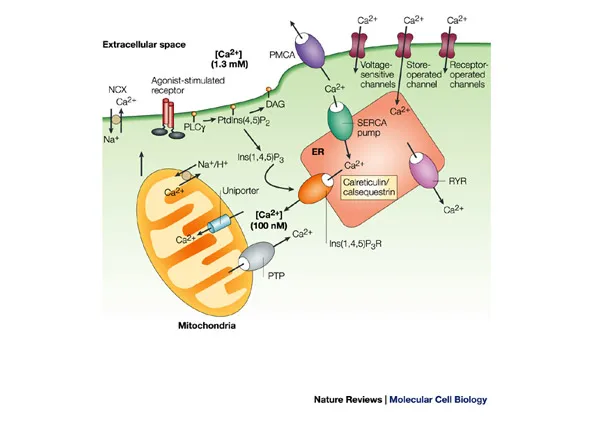
The calcium injury cascade follows a predictable pattern: pump failure → membrane permeabilization → massive influx → enzyme activation → structural destruction. This process becomes irreversible when cytosolic calcium exceeds 1-5 μM for more than 10-15 minutes.
📌 Remember: CALM - Calcium influx, Activates enzymes, Leads to Membrane destruction
Calcium-activated enzymes include phospholipase A2 (membrane destruction), calpains (cytoskeletal proteolysis), endonucleases (DNA fragmentation), and ATPases (further energy depletion). These enzymes become activated at calcium concentrations >500 nM, creating a self-perpetuating destruction cycle.
| Calcium Parameter | Normal Range | Early Injury | Severe Injury | Critical Level | Enzyme Activation |
|---|---|---|---|---|---|
| Cytosolic [Ca2+] | 50-100 nM | 200-500 nM | 1-5 μM | >10 μM | Progressive |
| ER [Ca2+] | 100-500 μM | 50-200 μM | <50 μM | Depleted | N/A |
| Mitochondrial [Ca2+] | 100-500 nM | 1-5 μM | >10 μM | >50 μM | Permeability transition |
| Pump activity | 100% | 50-70% | <20% | Absent | N/A |
| Membrane integrity | Intact | Mild damage | Severe damage | Disrupted | Complete |
Mitochondrial calcium overload triggers the mitochondrial permeability transition pore (mPTP) opening, causing immediate ATP synthesis cessation and cytochrome c release. This represents the definitive point of no return in cellular injury progression.
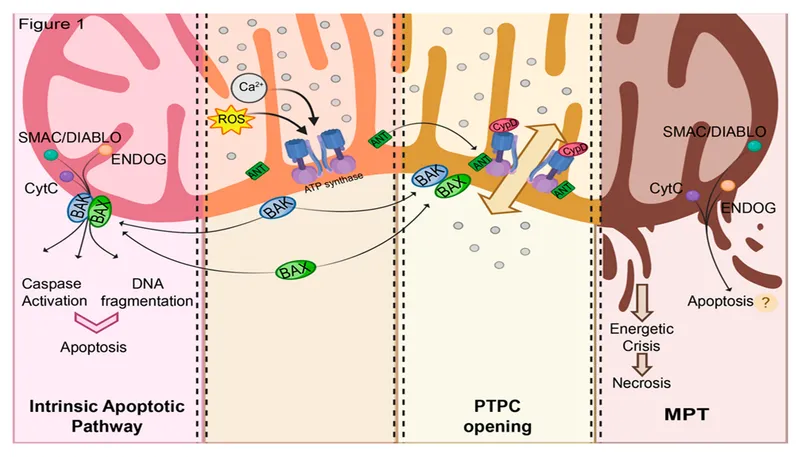
💡 Master This: Calcium influx creates a positive feedback loop - more calcium → more enzyme activation → more membrane damage → more calcium influx → irreversible cellular destruction
Calcium homeostasis restoration requires hours to days after injury resolution, with endoplasmic reticulum calcium stores requiring 24-48 hours for complete replenishment in surviving cells.
🌊 Calcium Catastrophe: The Cellular Flood Gates
🧬 Membrane Mayhem: The Cellular Fortress Under Siege
The membrane injury sequence follows: lipid peroxidation → protein denaturation → cytoskeletal disruption → permeability increase → structural collapse. This progression becomes irreversible when >30% of membrane phospholipids undergo oxidative damage.
📌 Remember: LIPS - Lipid peroxidation, Increased permeability, Protein damage, Structural collapse
Membrane lipid composition determines injury susceptibility, with polyunsaturated fatty acids being 100-fold more susceptible to oxidative damage than saturated fatty acids. Arachidonic acid and docosahexaenoic acid represent primary targets for free radical attack.
| Membrane Component | Normal Function | Injury Response | Damage Threshold | Recovery Time | Clinical Marker |
|---|---|---|---|---|---|
| Phospholipids | Barrier integrity | Peroxidation | >20% oxidized | 6-12 hours | Malondialdehyde |
| Membrane proteins | Transport/signaling | Denaturation | >50% inactive | 12-24 hours | Enzyme release |
| Cholesterol | Fluidity regulation | Oxidation | >30% modified | 24-48 hours | Oxysterols |
| Cytoskeleton | Structural support | Fragmentation | >40% disrupted | 48-72 hours | Spectrin breakdown |
| Glycocalyx | Cell recognition | Shedding | >60% lost | 72-96 hours | Syndecan-1 |
| %%{init: {'flowchart': {'htmlLabels': true}}}%% | |||||
| flowchart TD |
Start["🔬 Normal Membrane
• Intact bilayer• Homeostasis"]
Stress["⚠️ Oxidative Stress
• ROS formation• Radical attack"]
Lipid["🩹 Lipid Peroxidation
• Fatty acid chains• Malondialdehyde"]
Protein["🧬 Protein Damage
• Thiol oxidation• Enz. dysfunction"]
Level["📋 Damage Level
• Extent check• Impact severity"]
Repair["🩺 Repairable
• Mild injury• Viable state"]
Recovery["✅ Recovery
• Cell survives• Normal health"]
Irreversible["🩺 Irreversible
• Severe injury• Failed repair"]
Collapse["🩹 Memb. Collapse
• Loss of barrier• Ion leakage"]
Death["⚠️ Cell Death
• Necrosis onset• Apoptotic path"]
Start --> Stress Stress --> Lipid Lipid --> Protein Protein --> Level Level -->|LT 30%| Repair Level -->|GT 30%| Irreversible Repair --> Recovery Irreversible --> Collapse Collapse --> Death
style Start fill:#EEFAFF, stroke:#DAF3FF, stroke-width:1.5px, rx:12, ry:12, color:#0369A1 style Stress fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C style Lipid fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Protein fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Level fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Repair fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Recovery fill:#F6F5F5, stroke:#E7E6E6, stroke-width:1.5px, rx:12, ry:12, color:#525252 style Irreversible fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Collapse fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C style Death fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C
> ⭐ **Clinical Pearl**: **Lactate dehydrogenase (LDH)** elevation indicates membrane damage, with levels **>3x normal** suggesting significant cellular injury in clinical settings
Membrane repair mechanisms include **phospholipid synthesis**, **antioxidant enzyme activation**, and **heat shock protein** upregulation. These processes require **6-24 hours** for completion and consume **significant ATP** resources.
> 💡 **Master This**: Membrane damage creates **vicious cycles** - increased permeability → calcium influx → enzyme activation → more membrane damage → further permeability increase
Advanced membrane injury triggers **membrane blebbing**, **cytoplasmic extrusion**, and **organelle release** - morphological changes visible within **30-60 minutes** of irreversible injury onset.
---
🧬 Membrane Mayhem: The Cellular Fortress Under Siege
🎯 Pattern Recognition: The Cellular Injury Fingerprint
The cellular injury recognition framework uses systematic evaluation of: nuclear changes → cytoplasmic alterations → membrane modifications → organelle disruption. Each category provides specific diagnostic information about injury severity and reversibility.
📌 Remember: NICE - Nuclear changes (chromatin clumping), Increased cell size, Cytoplasmic eosinophilia, Enzyme release
Nuclear changes represent the most reliable indicators of injury severity: chromatin margination (reversible), pyknosis (condensation), karyorrhexis (fragmentation), and karyolysis (dissolution). These changes follow a predictable temporal sequence over 2-24 hours.
| Morphological Change | Timing | Reversibility | Molecular Basis | Clinical Significance | Diagnostic Confidence |
|---|---|---|---|---|---|
| Cellular swelling | 5-15 minutes | Reversible | Na+/K+ pump failure | Early injury marker | High |
| Chromatin clumping | 30-60 minutes | Reversible | Ionic shifts | Metabolic stress | High |
| Cytoplasmic eosinophilia | 1-2 hours | Irreversible | Protein denaturation | Severe injury | Very high |
| Nuclear pyknosis | 2-6 hours | Irreversible | DNA condensation | Cell death | Very high |
| Membrane blebbing | 4-8 hours | Irreversible | Cytoskeletal collapse | Advanced necrosis | Very high |
⭐ Clinical Pearl: Cytoplasmic eosinophilia appears 1-2 hours after irreversible injury onset and indicates >70% probability of cell death in tissue sections
Organelle-specific patterns provide mechanistic insights: mitochondrial swelling (energy failure), endoplasmic reticulum dilation (protein synthesis disruption), lysosomal rupture (membrane instability). Each pattern correlates with specific injury mechanisms.
💡 Master This: Pattern timing enables injury age determination - acute changes (<6 hours) show swelling and chromatin clumping, while chronic changes (>24 hours) show nuclear fragmentation and cytoplasmic loss
Advanced pattern recognition incorporates immunohistochemical markers: cleaved caspase-3 (apoptosis), HMGB1 (necrosis), LC3 (autophagy), enabling molecular-level injury classification with >95% diagnostic accuracy.
🎯 Pattern Recognition: The Cellular Injury Fingerprint
⚖️ Therapeutic Intervention: The Cellular Rescue Protocols
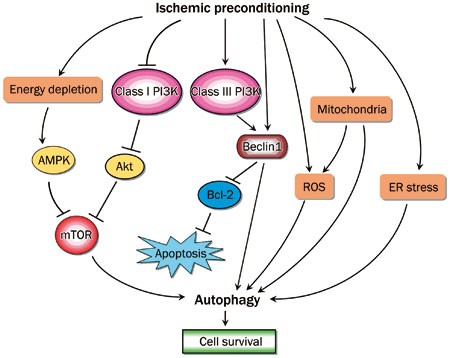
The cellular rescue protocol hierarchy prioritizes: energy restoration → calcium control → membrane stabilization → antioxidant protection → repair enhancement. Each intervention level requires specific timing and molecular targets for optimal efficacy.
📌 Remember: CREAM - Calcium blockers, Reperfusion, Energy substrates, Antioxidants, Membrane stabilizers
Energy restoration interventions include glucose supplementation, insulin therapy, mitochondrial substrates, and ATP precursors. These interventions show maximum efficacy when initiated within 15-30 minutes of injury onset.
| Intervention Category | Optimal Timing | Mechanism | Efficacy Window | Success Rate | Clinical Application |
|---|---|---|---|---|---|
| Calcium channel blockers | 0-30 minutes | Prevent Ca2+ influx | 60 minutes | 60-80% | Stroke, MI |
| Antioxidants | 0-45 minutes | Scavenge free radicals | 90 minutes | 40-70% | Reperfusion injury |
| Energy substrates | 0-60 minutes | Restore ATP synthesis | 120 minutes | 50-75% | Shock, ischemia |
| Membrane stabilizers | 30-120 minutes | Prevent lipid peroxidation | 180 minutes | 30-60% | Multi-organ failure |
| Growth factors | 2-24 hours | Enhance repair | 7 days | 20-50% | Chronic injury |
| %%{init: {'flowchart': {'htmlLabels': true}}}%% | |||||
| flowchart TD |
ID["🚨 Injury Detection
• Identify harm• Initial trigger"]
TA["📋 Timing Assessment
• Evaluate onset• Duration check"]
AI["⚠️ Acute Intervention
• Immediate care• Rapid response"]
EC["💊 Calcium Control
• Energy balance• Control levels"]
HS["✅ High Success
• Optimal outcome• Recovery likely"]
DL["🩺 Damage Limitation
• Reduce spread• Manage injury"]
MS["💊 Membrane Stability
• Cell protection• Guard membrane"]
MS_OUT["✅ Moderate Success
• Partial repair• Stable status"]
RE["🩹 Repair Enhancement
• Tissue healing• Chronic phase"]
GF["💊 Growth Factor
• Therapy admin• Promote growth"]
LS["✅ Limited Success
• Late stage• Poor prognosis"]
ID --> TA TA -->|< 30 min| AI TA -->|30-120 min| DL TA -->|> 120 min| RE
AI --> EC --> HS DL --> MS --> MS_OUT RE --> GF --> LS
style ID fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C style TA fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style AI fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C style EC fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style HS fill:#F6F5F5, stroke:#E7E6E6, stroke-width:1.5px, rx:12, ry:12, color:#525252 style DL fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style MS fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style MS_OUT fill:#F6F5F5, stroke:#E7E6E6, stroke-width:1.5px, rx:12, ry:12, color:#525252 style RE fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style GF fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style LS fill:#F6F5F5, stroke:#E7E6E6, stroke-width:1.5px, rx:12, ry:12, color:#525252
> ⭐ **Clinical Pearl**: **Combination therapy** targeting multiple pathways simultaneously increases cellular survival by **30-50%** compared to single-agent interventions
**Calcium control strategies** include **channel blockers** (verapamil, nifedipine), **chelators** (EGTA, BAPTA), and **pump enhancers** (milrinone). These interventions must be initiated **before** massive calcium influx occurs to maintain efficacy.
> 💡 **Master This**: **Therapeutic window** duration varies by cell type - neurons (**3-6 hours**), cardiomyocytes (**6-12 hours**), hepatocytes (**12-24 hours**) - requiring tissue-specific intervention protocols
Advanced intervention strategies include **preconditioning protocols**, **remote ischemic conditioning**, and **pharmacological conditioning** that can extend therapeutic windows by **2-4 fold** through endogenous protective mechanism activation.
---
⚖️ Therapeutic Intervention: The Cellular Rescue Protocols
🔗 Multi-System Integration: The Cellular Injury Network
The cellular injury communication network operates through: damage-associated molecular patterns (DAMPs) → inflammatory mediator release → systemic circulation → distant organ activation → amplification cascades. This network can transform localized injury into systemic disease within hours.
📌 Remember: DAMPS - Damage signals, Amplification cascades, Multi-organ effects, Pathway interactions, Systemic responses
DAMP molecules include HMGB1 (nuclear protein), ATP (energy molecule), DNA fragments, heat shock proteins, and S100 proteins. These molecules activate pattern recognition receptors on immune cells and endothelial cells throughout the body.
| DAMP Molecule | Cellular Source | Receptor Target | Systemic Effect | Peak Release Time | Clinical Marker |
|---|---|---|---|---|---|
| HMGB1 | Nuclear release | TLR2/4, RAGE | Inflammation | 6-24 hours | Sepsis severity |
| ATP | Mitochondrial leak | P2X7, P2Y | Platelet activation | 1-6 hours | Thrombosis risk |
| DNA fragments | Nuclear breakdown | TLR9, cGAS-STING | Interferon response | 2-12 hours | Autoimmunity |
| HSP70 | Stress response | TLR2/4 | Cytoprotection | 4-48 hours | Recovery marker |
| S100A8/A9 | Neutrophil release | TLR4, RAGE | Neutrophil recruitment | 2-8 hours | Tissue damage |
| %%{init: {'flowchart': {'htmlLabels': true}}}%% | |||||
| flowchart TD |
Injury["💥 Cellular Injury
• Local tissue damage• Triggering event"]
DAMP["📡 DAMP Release
• Danger signals• Molecular patterns"]
Receptor["🔑 Receptors
• Cell activation• PRR signaling"]
ResponseType{"⚖️ Response Type
• Immune balance• Host reaction"}
Repair["🛠️ Repair
• Healing mechanisms• Local control"]
Recovery["✅ Recovery
• Tissue restoration• Return to baseline"]
Inflam["🔥 Inflammation
• Systemic ⬆️• Cytokine storm"]
MODS["⚠️ Organs
• Dysfunction• Multi-organ hit"]
Disease["🩺 Systemic Disease
• Chronic state• Critical illness"]
Injury --> DAMP DAMP --> Receptor Receptor --> ResponseType
ResponseType -->|Protective| Repair Repair --> Recovery
ResponseType -->|Excessive| Inflam Inflam --> MODS MODS --> Disease
style Injury fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style DAMP fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style Receptor fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8 style ResponseType fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Repair fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style Recovery fill:#F6F5F5, stroke:#E7E6E6, stroke-width:1.5px, rx:12, ry:12, color:#525252 style Inflam fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C style MODS fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C style Disease fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8
> ⭐ **Clinical Pearl**: **HMGB1 levels >10 ng/mL** predict **multi-organ dysfunction** development with **85%** accuracy in critically ill patients
**Organ crosstalk networks** demonstrate how **hepatic injury** affects **renal function** through **inflammatory mediators**, **cardiac injury** influences **pulmonary function** through **neurohormonal activation**, and **intestinal injury** impacts **systemic immunity** through **barrier dysfunction**.
> 💡 **Master This**: **Network amplification** occurs when **>20%** of cells in an organ undergo injury simultaneously, triggering **systemic DAMP release** that can cause **distant organ dysfunction** within **6-12 hours**
Advanced network understanding reveals **therapeutic targets** for **multi-organ protection**: **DAMP inhibitors** (HMGB1 antibodies), **receptor antagonists** (TLR4 blockers), and **network modulators** (complement inhibitors) that can prevent **systemic injury propagation**.
---
🔗 Multi-System Integration: The Cellular Injury Network
🎯 Clinical Mastery Arsenal: The Cellular Injury Toolkit
Essential Cellular Injury Numbers for clinical practice:
- ATP depletion >50% = irreversible injury threshold
- Calcium >1 μM = enzyme activation level
- LDH >3x normal = significant membrane damage
- Troponin elevation = cardiomyocyte injury within 3-6 hours
- Therapeutic window = 30 minutes for optimal intervention
📌 Remember: MASTER - Membrane damage (LDH), ATP depletion (lactate), Stress markers (troponin), Timing (therapeutic window), Enzymes (calcium-activated), Recovery potential
| Clinical Scenario | Key Markers | Timing | Intervention | Success Rate | Monitoring |
|---|---|---|---|---|---|
| Myocardial infarction | Troponin, CK-MB | 3-6 hours | Reperfusion | 85-95% | Serial enzymes |
| Stroke | CT/MRI changes | 3-4.5 hours | Thrombolysis | 60-80% | Neurological exam |
| Hepatic injury | ALT, AST | 6-12 hours | Supportive care | 70-90% | Liver function |
| Renal injury | Creatinine, BUN | 12-24 hours | Fluid management | 60-85% | Urine output |
| Multi-organ failure | Multiple markers | 24-48 hours | Organ support | 30-60% | SOFA score |
- Step 1: Identify injury timing and severity markers
- Step 2: Assess reversibility potential using cellular indicators
- Step 3: Determine therapeutic window and intervention options
- Step 4: Monitor recovery markers and adjust therapy
- Step 5: Predict complications using network understanding
⭐ Clinical Pearl: Serial marker monitoring every 6-12 hours during the first 48 hours provides the most accurate assessment of cellular injury progression and recovery potential
💡 Master This: Cellular injury mastery enables prediction of patient outcomes, complication risk, and recovery potential through systematic application of molecular principles to clinical practice
Advanced Integration Tools include biomarker panels for multi-organ assessment, imaging protocols for real-time injury monitoring, and therapeutic algorithms for personalized intervention based on individual cellular injury patterns.
This cellular injury knowledge transforms clinical decision-making across all specialties, from emergency medicine rapid assessment to critical care organ support strategies, providing the mechanistic foundation for evidence-based patient care.
🎯 Clinical Mastery Arsenal: The Cellular Injury Toolkit
Practice Questions: Cell injury
Test your understanding with these related questions
Which transport mechanism is primarily responsible for calcium reabsorption in the proximal tubule?













