Rheumatic heart disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Rheumatic heart disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Rheumatic heart disease US Medical PG Question 1: A 53-year-old female presents with worsening shortness of breath with activity. Physical exam reveals a diastolic murmur with an opening snap. The patient’s medical history is significant for a left hip replacement 10 years ago, and she vaguely recalls an extended period of illness as a child described as several severe episodes of sore throat followed by rash, fever, and joint pains. Administration of which of the following treatments at that time would have been most effective in reducing her risk of developing cardiac disease?
- A. Ciprofloxacin
- B. Vancomycin
- C. Penicillin (Correct Answer)
- D. Acyclovir
- E. Aspirin
Rheumatic heart disease Explanation: ***Penicillin***
- The patient's childhood history of recurrent sore throats, rash, fever, and joint pains is highly suggestive of **rheumatic fever**, a sequela of untreated **Group A Streptococcal (GAS) pharyngitis**.
- **Penicillin** is the most effective antibiotic for treating GAS pharyngitis and preventing subsequent rheumatic fever and its associated **valvular heart disease**, such as the **mitral stenosis** suggested by the diastolic murmur and opening snap.
*Ciprofloxacin*
- **Ciprofloxacin** is a fluoroquinolone antibiotic primarily used for gram-negative bacterial infections and some gram-positive infections, but it is **not the first-line treatment for GAS pharyngitis**.
- Its broad spectrum and potential side effects make it unsuitable for routine use in preventing rheumatic fever.
*Vancomycin*
- **Vancomycin** is a powerful antibiotic reserved for serious infections caused by gram-positive bacteria, particularly **MRSA** and **_Clostridioides difficile_**.
- While it has activity against GAS, it is **not appropriate for treating GAS pharyngitis** due to its reserved status for resistant infections, requirement for IV administration, and potential side effects, making it unsuitable for preventing rheumatic fever.
*Acyclovir*
- **Acyclovir** is an antiviral medication used to treat herpes simplex and varicella-zoster virus infections.
- It has **no antibacterial activity** and would be completely ineffective in treating GAS pharyngitis or preventing rheumatic heart disease.
*Aspirin*
- **Aspirin** is an anti-inflammatory and antiplatelet agent used to manage symptoms of rheumatic fever like **arthralgia** and fever, but it **does not treat the underlying streptococcal infection**.
- While it can alleviate some acute symptoms, it **does not prevent the development of permanent cardiac damage**.
Rheumatic heart disease US Medical PG Question 2: A 63-year-old man comes to the physician for evaluation of fever and a nonproductive cough for the past 2 weeks. During this period, he has also had fatigue, myalgia, and difficulty breathing. Five weeks ago, he underwent an aortic prosthetic valve replacement due to high-grade aortic stenosis. The patient has a history of hypertension, asthma, and type 2 diabetes mellitus. A colonoscopy 2 years ago was normal. The patient has smoked one pack of cigarettes daily for the past 40 years. He has never used illicit drugs. Current medications include aspirin, warfarin, lisinopril, metformin, inhaled albuterol, and a multivitamin. The patient appears lethargic. Temperature is 38.6°C (101.5°F), pulse is 105/min, and blood pressure is 140/60 mm Hg. Rales are heard on auscultation of the lungs. A grade 2/6, diastolic blowing murmur is heard over the left sternal border and radiates to the right sternal border. A photograph of his right index finger is shown. Laboratory studies show a leukocyte count of 13,800/mm3 and an erythrocyte sedimentation rate of 48 mm/h. Which of the following is the most likely causal organism?
- A. Staphylococcus epidermidis (Correct Answer)
- B. Enterococcus faecalis
- C. Streptococcus gallolyticus
- D. Streptococcus pyogenes
- E. Viridans streptococci
Rheumatic heart disease Explanation: ***Staphylococcus epidermidis***
- This patient's **recent prosthetic valve replacement** makes him highly susceptible to infective endocarditis caused by *Staphylococcus epidermidis*, a common pathogen in **nosocomial infections** and on implanted devices.
- **Early prosthetic valve endocarditis** (within 2 months post-surgery, as in this case at 5 weeks) is most commonly caused by coagulase-negative staphylococci, particularly *S. epidermidis*, which colonize the valve during the perioperative period.
- The symptoms of fever, cough, fatigue, myalgia, difficulty breathing, and a new diastolic murmur, along with peripheral manifestations (shown in the photograph) and elevated inflammatory markers, are all consistent with infective endocarditis.
*Enterococcus faecalis*
- While *Enterococcus faecalis* can cause endocarditis, it is more commonly associated with **gastrointestinal or genitourinary procedures**, which are not indicated here.
- No recent urinary tract infection or GI instrumentation (colonoscopy was 2 years ago) points away from this organism.
*Streptococcus gallolyticus*
- Previously known as *Streptococcus bovis*, this organism is strongly associated with **colon cancer, inflammatory bowel disease, and colonic polyps**.
- The patient had a normal colonoscopy recently (2 years ago), making this less likely.
*Streptococcus pyogenes*
- *Streptococcus pyogenes* is known for causing **pharyngitis, scarlet fever, and rheumatic fever**, but it is a relatively uncommon cause of infective endocarditis, especially on prosthetic valves.
- There is no history of a recent streptococcal infection to suggest this pathogen.
*Viridans streptococci*
- **Viridans streptococci** are the most common cause of **native valve endocarditis**, often following dental procedures, but are less common in early prosthetic valve endocarditis compared to *S. epidermidis*.
- This patient had a prosthetic valve replacement 5 weeks ago, pointing more towards a nosocomial organism like *S. epidermidis*.
Rheumatic heart disease US Medical PG Question 3: A 35-year-old African-American female presents to the emergency room complaining of chest pain. She also complains of recent onset arthritis and increased photosensitivity. Physical examination reveals bilateral facial rash. Which of the following is most likely to be observed in this patient?
- A. Pain improves with inspiration
- B. High-pitched diastolic murmur
- C. Fixed and split S2
- D. Mid-systolic click
- E. Pain relieved by sitting up and leaning forward (Correct Answer)
Rheumatic heart disease Explanation: ***Pain relieved by sitting up and leaning forward***
- This patient's symptoms (chest pain, arthritis, photosensitivity, facial rash) are highly suggestive of **systemic lupus erythematosus (SLE)**.
- Among the cardiac manifestations of SLE, **pericarditis** is common. The chest pain of pericarditis is typically relieved by sitting up and leaning forward, as this decreases pressure on the inflamed pericardial sac.
*Pain improves with inspiration*
- This describes **pleuritic chest pain**, which is often associated with conditions like pleurisy or pneumothorax, where inspiration causes stretching of inflamed pleura.
- While pleurisy can occur in SLE, the relief by sitting up and leaning forward is a more classic sign of pericarditis.
*High-pitched diastolic murmur*
- A high-pitched diastolic murmur is characteristic of **aortic regurgitation** or **pulmonic regurgitation**.
- While SLE can cause valvular heart disease (e.g., Libman-Sacks endocarditis, often leading to mitral valve involvement), aortic or pulmonic regurgitation is not the most typical acute cardiac finding associated with these specific chest pain characteristics.
*Fixed and split S2*
- A fixed and split S2 is a classic finding in an **atrial septal defect (ASD)**.
- While rare, SLE can be associated with some congenital heart abnormalities or pulmonary hypertension, but ASD is not a typical direct complication leading to this S2 finding in the context of acute chest pain.
*Mid-systolic click*
- A mid-systolic click is characteristic of **mitral valve prolapse (MVP)**.
- Mitral valve abnormalities, including MVP and mitral regurgitation (due to Libman-Sacks endocarditis), are relatively common in SLE. However, the chest pain associated with pericarditis (relieved by sitting up) is a more direct and common finding given the constellation of symptoms than a mid-systolic click alone.
Rheumatic heart disease US Medical PG Question 4: A 47-year-old woman comes to the physician because of a 6-week history of fatigue and low-grade fever. She has no history of serious illness except for a bicuspid aortic valve, diagnosed 10 years ago. She does not use illicit drugs. Her temperature is 37.7°C (99.9°F). Physical examination shows petechiae under the fingernails and multiple tender, red nodules on the fingers. A new grade 2/6 diastolic murmur is heard at the right second intercostal space. Which of the following is the most likely causal organism?
- A. Staphylococcus epidermidis
- B. Streptococcus pyogenes
- C. Streptococcus sanguinis (Correct Answer)
- D. Streptococcus pneumoniae
- E. Enterococcus faecalis
Rheumatic heart disease Explanation: ***Streptococcus sanguinis***
- The patient's presentation with **fatigue, low-grade fever, petechiae, tender nodules (Osler nodes)**, and a **new diastolic murmur** in a patient with a **bicuspid aortic valve** is highly suggestive of **infective endocarditis**.
- **Streptococcus sanguinis** (and other viridans streptococci) are common causes of subacute bacterial endocarditis, often associated with **oral flora** and pre-existing valvular heart disease.
*Staphylococcus epidermidis*
- This organism is a common cause of **prosthetic valve endocarditis** and **nosocomial infections** but is less likely to cause endocarditis in a native valve without a history of recent surgery or intravenous lines.
- While it can cause endocarditis, the clinical features here, especially the lack of recent medical interventions, point away from *S. epidermidis* as the primary cause.
*Streptococcus pyogenes*
- **Streptococcus pyogenes** is primarily known for causing **strep throat, scarlet fever, and rheumatic fever**, which can lead to rheumatic heart disease but rarely causes acute or subacute infective endocarditis directly.
- It typically causes more acute and severe infections, which doesn't align with the 6-week history of low-grade fever and fatigue.
*Streptococcus pneumoniae*
- **Streptococcus pneumoniae** is a common cause of **pneumonia, meningitis, and otitis media** but is an uncommon cause of infective endocarditis, accounting for a very small percentage of cases.
- Endocarditis due to *S. pneumoniae* tends to be **acute and fulminant**, often associated with severe systemic illness, which is not fully consistent with the subacute presentation here.
*Enterococcus faecalis*
- **Enterococcus faecalis** is a common cause of **nosocomial urinary tract infections** and can cause endocarditis, especially in older patients or those with gastrointestinal or genitourinary procedures.
- While it's a possibility for endocarditis, the oral flora association with viridans streptococci (like *S. sanguinis*) in the context of a bicuspid aortic valve makes it a more direct fit.
Rheumatic heart disease US Medical PG Question 5: A 20-year-old man comes to the emergency room because of palpitations and mild dyspnea for the last 2 hours. He has had similar episodes in the past that resolved within 20 minutes, but they have been worsening since he started training for his first marathon 1 month ago. Ten years ago, he was treated for streptococcal pharyngitis with a 10-day course of penicillin. His maternal uncle passed away unexpectedly from a heart condition at age 40. He is 180 cm (5 ft 11 in) tall and weighs 85 kg (187 lb); BMI is 26.2 kg/m2. His temperature is 36.5°C (97.7°F), pulse is 70/min, respirations are 18/min, and blood pressure is 132/60 mm Hg. On examination, there is a decrescendo early diastolic murmur heard best along the left sternal border. His head slightly bobs about every second. The remainder of the examination shows no abnormalities. Which of the following is most likely to be present?
- A. Bicuspid aortic valve (Correct Answer)
- B. Antistreptolysin O antibodies
- C. Asymmetric septal hypertrophy
- D. Valve vegetation
- E. Myxomatous degeneration
Rheumatic heart disease Explanation: ***Bicuspid aortic valve***
- The patient presents with classic signs of **aortic regurgitation**, including a **decrescendo early diastolic murmur** and **De Musset's sign** (head bobbing). In a young individual, a **bicuspid aortic valve** is the most common congenital cause of aortic valve disease, often leading to regurgitation or stenosis over time.
- The patient's history of palpitations and dyspnea, worsening with exertion, suggests significant hemodynamic compromise related to chronic aortic insufficiency, which can develop secondary to a bicuspid valve.
*Antistreptolysin O antibodies*
- While the patient had a history of **streptococcal pharyngitis** 10 years ago, there are no other signs of **acute rheumatic fever** or **rheumatic heart disease**, such as migratory polyarthritis, chorea, or erythema marginatum.
- The murmur described is typical of aortic regurgitation without specific features pointing to rheumatic involvement, which typically affects the **mitral valve** first.
*Asymmetric septal hypertrophy*
- **Asymmetric septal hypertrophy** is characteristic of **hypertrophic cardiomyopathy**, which would typically present with a **systolic murmur** that increases with Valsalva maneuver, not an early diastolic murmur.
- While sudden cardiac death in a young relative might suggest hypertrophic cardiomyopathy, the physical exam findings here are inconsistent with that diagnosis.
*Valve vegetation*
- **Valve vegetations** are associated with **infective endocarditis** and would typically present with fever, new or worsening murmur, and signs of systemic infection, none of which are noted in this patient.
- The patient's symptoms are chronic and episodic, not acute, subacute, or associated with infectious signs.
*Myxomatous degeneration*
- **Myxomatous degeneration** primarily affects the **mitral valve**, leading to **mitral valve prolapse** and subsequent regurgitation, which would produce a **mid-systolic click** followed by a late systolic murmur.
- This condition is not typically associated with an early diastolic murmur characteristic of aortic regurgitation.
Rheumatic heart disease US Medical PG Question 6: An autopsy of a patient's heart who recently died in a motor vehicle accident shows multiple nodules near the line of closure on the ventricular side of the mitral valve leaflet. Microscopic examination shows that these nodules are composed of immune complexes, mononuclear cells, and thrombi interwoven with fibrin strands. These nodules are most likely to be found in which of the following patients?
- A. A 41-year-old female with a facial rash and nonerosive arthritis (Correct Answer)
- B. A 6-year-old female with subcutaneous nodules and erythema marginatum
- C. A 62-year-old male with Cardiobacterium hominis bacteremia
- D. A 54-year-old male who recently underwent dental surgery
- E. A 71-year-old male with acute-onset high fever and nail bed hemorrhages
Rheumatic heart disease Explanation: ***A 41-year-old female with a facial rash and nonerosive arthritis***
- The description of nodules composed of **immune complexes, mononuclear cells, and thrombi interwoven with fibrin strands** on the **ventricular side of the mitral valve leaflets** is classic for **Libman-Sacks endocarditis**.
- **Libman-Sacks endocarditis** is strongly associated with **systemic lupus erythematosus (SLE)**, which commonly presents with a **malar rash** and **nonerosive arthritis** in young to middle-aged women.
*A 6-year-old female with subcutaneous nodules and erythema marginatum*
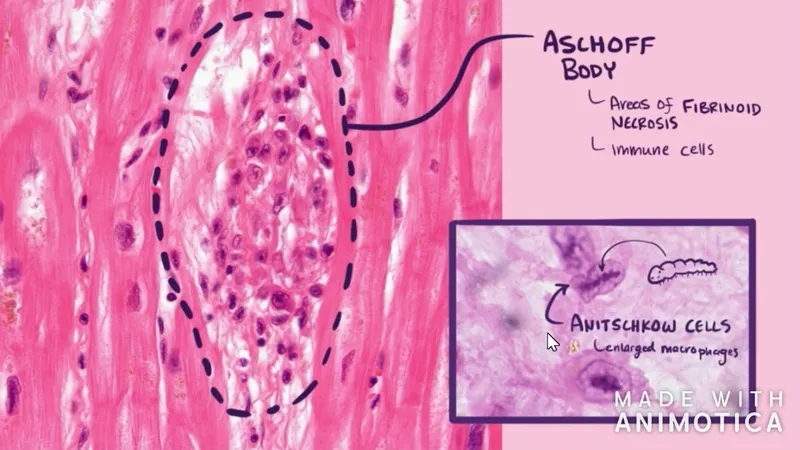
- This presentation is characteristic of **acute rheumatic fever**, which causes **Aschoff bodies** (fibrinoid necrosis surrounded by inflammatory cells) in the heart.
- While it affects heart valves, the characteristic lesions are **fibrinous vegetations along the lines of closure** (Rheumatic Heart Disease) rather than immune complex-rich nodules on the ventricular surface described, and it is most commonly associated with **streptococcal infection**, not immune complexes as the primary driver.
*A 62-year-old male with Cardiobacterium hominis bacteremia*
- **Cardiobacterium hominis** is a HACEK group organism that can cause **subacute infective endocarditis**.
- Infective endocarditis involves vegetations composed of **microorganisms, fibrin, inflammatory cells, and red blood cells**, which typically occur on the **atrial side of the mitral valve** or the **ventricular side of the aortic valve**, and the primary component is bacteria, not immune complexes.
*A 54-year-old male who recently underwent dental surgery*
- Recent dental surgery is a common risk factor for **infective endocarditis**, often caused by **viridans group streptococci**.
- The lesions in infective endocarditis are primarily composed of **bacterial colonies and fibrin**, and they typically develop on the **atrial side of the mitral valve** (high-pressure side) and are destructive, differing from the immune complex-rich, non-destructive nodules of Libman-Sacks endocarditis.
*A 71-year-old male with acute-onset high fever and nail bed hemorrhages*
- **Acute-onset high fever** and **nail bed hemorrhages (splinter hemorrhages)** are signs of **acute infective endocarditis**, often caused by virulent organisms like *Staphylococcus aureus*.
- Although vegetation can occur on the heart valves, the composition is primarily bacterial colonies and inflammatory cells, and the primary location is usually the **aortic or mitral valve**, typically in areas of turbulent flow or previous damage, differing microscopically from Libman-Sacks endocarditis.
Rheumatic heart disease US Medical PG Question 7: A 16-year-old female is seen at her outpatient primary medical doctor's office complaining of a sore throat. Further history reveals that she has no cough and physical exam is notable for tonsillar exudates. Vitals in the office reveal HR 88, RR 16, and T 102.1. Using the Centor criteria for determining likelihood of Group A beta-hemolytic strep pharyngitis, the patient has a score of 3. A review of the primary literature yields the findings in Image A. What is the specificity of the Centor criteria using a score of 3 as a cutoff value?
- A. 41/46 = 89%
- B. Not enough information has been provided
- C. 45/50 = 90%
- D. 41/50 = 82% (Correct Answer)
- E. 9/54 = 17%
Rheumatic heart disease Explanation: ***41/50 = 82%***
- Specificity = **True Negatives / (True Negatives + False Positives)**
- With a Centor score cutoff of ≥3 as "positive" for GABHS pharyngitis, those without disease who score <3 are **true negatives (TN = 41)**
- Those without disease who score ≥3 are **false positives (FP = 9)**
- Therefore: Specificity = 41 / (41 + 9) = **41/50 = 82%**
*41/46 = 89%*
- This represents **Negative Predictive Value (NPV)**, not specificity
- NPV = TN / (TN + FN) = 41 / (41 + 5) = 41/46 = 89%
- NPV reflects the probability that a patient with a negative test (Centor score <3) truly lacks GABHS disease
- While clinically useful, this is not what the question asks for
*Not enough information has been provided*
- Incorrect: the referenced data table provides all necessary values
- **True negatives = 41** and **false positives = 9** allow direct calculation of specificity
- No additional information is required
*45/50 = 90%*
- This represents **Sensitivity**, not specificity
- Sensitivity = TP / (TP + FN) = 45 / (45 + 5) = **45/50 = 90%**
- Sensitivity reflects the proportion of true disease-positive patients who score ≥3 on the Centor criteria
- This is a different diagnostic parameter from specificity
*9/54 = 17%*
- This calculation uses an incorrect denominator (54 = TP + FP = 45 + 9)
- 9/50 = 18% would represent the **false positive rate (1 − specificity)**
- 9/54 = FP/(TP + FP), which is the **false discovery rate (1 − PPV)**, not specificity
- Does not correspond to specificity or any standard diagnostic parameter with the denominator shown
Rheumatic heart disease US Medical PG Question 8: A 27-year-old woman comes to the physician because of a 3-day history of a sore throat and fever. Her temperature is 38.5°C (101.3°F). Examination shows edematous oropharyngeal mucosa and enlarged tonsils with purulent exudate. There is tender cervical lymphadenopathy. If left untreated, which of the following conditions is most likely to occur in this patient?
- A. Rheumatic fever (Correct Answer)
- B. Rheumatoid arthritis
- C. Erythema multiforme
- D. Toxic shock syndrome
- E. Post-streptococcal glomerulonephritis
Rheumatic heart disease Explanation: ***Rheumatic fever***
- The patient presents with classic symptoms of **streptococcal pharyngitis** (sore throat, fever, tonsillar exudate, tender cervical lymphadenopathy), which, if left untreated, is a major risk factor for developing **acute rheumatic fever**.
- **Acute rheumatic fever** is a serious inflammatory disease that can affect the **heart valves**, joints, brain, and skin, occurring in approximately **3% of untreated cases** of Group A Streptococcal pharyngitis.
*Rheumatoid arthritis*
- This is a **chronic autoimmune inflammatory disease** primarily affecting the synovial joints, not typically associated with an acute streptococcal infection.
- It involves a different pathophysiological mechanism and is not a direct complication of untreated streptococcal pharyngitis.
*Erythema multiforme*
- This is an **acute, self-limiting skin condition** often triggered by infections (e.g., Herpes simplex virus) or medications, resulting in target lesions.
- While infections can cause it, **streptococcal pharyngitis** is not a common or direct cause, and it's not a systemic complication similar to rheumatic fever.
*Toxic shock syndrome*
- This is a **rapidly progressing infectious disease** characterized by fever, rash, hypotension, and multi-organ failure, most often caused by toxins produced by *Staphylococcus aureus* or *Streptococcus pyogenes*.
- While *Streptococcus pyogenes* (Group A Strep) can cause it, toxic shock syndrome is an **acute complication** rather than a late sequela of untreated infection, making **rheumatic fever** the more characteristic delayed complication.
*Post-streptococcal glomerulonephritis*
- While this is another serious immune-mediated complication of **streptococcal infections**, it **more commonly follows skin infections (impetigo)** than pharyngitis.
- **Rheumatic fever** is the most characteristic and clinically significant late complication of untreated streptococcal **pharyngitis** specifically, with greater emphasis in clinical practice due to its potential for permanent cardiac valve damage.
Rheumatic heart disease US Medical PG Question 9: A 43-year-old woman presents to the emergency department complaining of palpitations, dry cough, and shortness of breath for 1 week. She immigrated to the United States from Korea at the age of 20. She says that her heart is racing and she has never felt these symptoms before. Her cough is dry and is associated with shortness of breath that occurs with minimal exertion. Her past medical history is otherwise unremarkable. She has no allergies and is not currently taking any medications. She is a nonsmoker and an occasional drinker. She denies illicit drug use. Her blood pressure is 100/65 mm Hg, pulse is 76/min, respiratory rate is 23/min, and temperature is 36.8°C (98.2°F). Her physical examination is significant for bibasilar lung crackles and a non-radiating, low-pitched, mid-diastolic rumbling murmur best heard at the apical region. In addition, she has jugular vein distention and bilateral pitting edema in her lower extremities. Which of the following best describes the infectious agent that led to this patient’s condition?
- A. A bacterium that induces partial lysis of red cells with hydrogen peroxide
- B. A bacterium that requires an anaerobic environment to grow properly
- C. A bacterium that does not lyse red cells
- D. A bacterium that induces heme degradation of the red cells of a blood agar plate
- E. A bacterium that induces complete lysis of the red cells of a blood agar plate with an oxygen-sensitive cytotoxin (Correct Answer)
Rheumatic heart disease Explanation: ***A bacterium that induces complete lysis of the red cells of a blood agar plate with an oxygen-sensitive cytotoxin***
- This describes **Group A Streptococcus (GAS)**, specifically *Streptococcus pyogenes*, which causes **rheumatic fever** leading to **mitral stenosis**. Mitral stenosis is characterized by a **mid-diastolic rumbling murmur** at the apex, left atrial enlargement causing **palpitations**, and **pulmonary congestion** leading to dyspnea, cough, and bibasilar crackles.
- The delayed onset of symptoms (immigrated at 20, symptoms at 43) is typical for **rheumatic heart disease**, where repeated GAS infections in childhood/adolescence lead to valve damage that manifests years later. GAS produces **streptolysin O**, an **oxygen-labile cytotoxin** responsible for **beta-hemolysis** (complete lysis) on blood agar.
*A bacterium that induces partial lysis of red cells with hydrogen peroxide*
- This describes **alpha-hemolytic** bacteria like *Streptococcus pneumoniae* or *Viridans streptococci*, which cause **partial hemolysis** (greenish discoloration) on blood agar due to **hydrogen peroxide** production.
- While *Viridans streptococci* can cause **infective endocarditis**, the clinical picture of **rheumatic mitral stenosis** is more consistent with a history of recurrent streptococcal pharyngitis (GAS).
*A bacterium that requires an anaerobic environment to grow properly*
- This description typically refers to **anaerobic bacteria**, such as *Clostridium* or *Bacteroides* species.
- These bacteria are generally not associated with the primary cause of acute rheumatic fever or the subsequent development of chronic valvular heart disease like mitral stenosis.
*A bacterium that does not lyse red cells*
- This describes **gamma-hemolytic** (non-hemolytic) bacteria, such as *Enterococcus faecalis* or some *Staphylococcus* species.
- These organisms do not cause the characteristic hemolysis seen with the streptococci responsible for rheumatic fever.
*A bacterium that induces heme degradation of the red cells of a blood agar plate*
- This description is **too vague** and does not specifically identify the organism. While heme degradation occurs with various types of hemolysis, the key distinguishing feature of **Group A Streptococcus** is **complete lysis (beta-hemolysis)** combined with production of the **oxygen-sensitive toxin streptolysin O**.
- This option lacks the specificity needed to identify GAS as the causative agent of rheumatic fever. Both alpha- and beta-hemolytic organisms can degrade heme, but only beta-hemolytic GAS causes rheumatic heart disease.
Rheumatic heart disease US Medical PG Question 10: A 51-year-old woman with hyperlipidemia comes to the physician because of weakness for one month. At the end of the day, she feels too fatigued to cook dinner or carry a laundry basket up the stairs. She also complains of double vision after she reads for long periods of time. All of her symptoms improve with rest. Her only medication is pravastatin. Physical examination shows drooping of the upper eyelids. Strength is initially 5/5 in the upper and lower extremities but decreases to 4/5 after a few minutes of sustained resistance. Sensation to light touch is intact and deep tendon reflexes are normal. Which of the following best describes the pathogenesis of this patient's condition?
- A. Type II hypersensitivity reaction (Correct Answer)
- B. Anterior horn cell destruction
- C. Impaired acetylcholine release
- D. Peripheral nerve demyelination
- E. Adverse drug effect
Rheumatic heart disease Explanation: ***Type II hypersensitivity reaction***
- This patient's symptoms of **fatigue** and **muscle weakness** that worsen with activity and improve with rest (**fatigable weakness**), along with **ptosis** (drooping eyelids) and **diplopia** (double vision), are classic for **myasthenia gravis**.
- Myasthenia gravis is an **autoimmune disease** characterized by autoantibodies that target and destroy **acetylcholine receptors** at the neuromuscular junction, leading to impaired signal transmission. This is a classic example of a **Type II hypersensitivity reaction**, where antibodies directly mediate cellular destruction or dysfunction.
*Anterior horn cell destruction*
- **Anterior horn cell destruction**, as seen in **amyotrophic lateral sclerosis (ALS)**, typically presents with both upper and lower motor neuron signs, such as **spasticity**, **hyperreflexia**, **fasciculations**, and **muscle atrophy**.
- In ALS, there is progressive weakness but typically **without fatigability** and oculomotor symptoms (ptosis, diplopia) are less common or occur late in the disease.
*Impaired acetylcholine release*
- **Impaired acetylcholine release** is characteristic of **Lambert-Eaton myasthenic syndrome (LEMS)**, which is often associated with small cell lung cancer.
- Unlike myasthenia gravis, LEMS typically shows **improvement in muscle strength with sustained activity** (due to increased presynaptic acetylcholine release), rather than worsening.
*Peripheral nerve demyelination*
- **Peripheral nerve demyelination** is the hallmark of conditions like **Guillain-Barré syndrome (GBS)** or **chronic inflammatory demyelinating polyneuropathy (CIDP)**.
- These conditions usually present with **sensory deficits**, **areflexia**, and **ascending paralysis/weakness**, which are absent in this patient.
*Adverse drug effect*
- While **statins** can cause **myopathy** (muscle pain and weakness), this typically involves diffuse muscle aches and elevated **creatine kinase** levels, and does not typically present with the classic fatigable weakness, ptosis, and diplopia seen here.
- The specific pattern of fatigable weakness improving with rest and affecting specific muscle groups (e.g., ocular muscles) points away from a simple statin-induced myopathy.
More Rheumatic heart disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.