Pericardial diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pericardial diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pericardial diseases US Medical PG Question 1: A 62-year-old woman presents to the emergency department with a 2-hour history of sharp chest pain. She says that the pain is worse when she inhales and is relieved by sitting up and leaning forward. Her past medical history is significant for rheumatoid arthritis, myocardial infarction status post coronary artery bypass graft, and radiation for breast cancer 20 years ago. Physical exam reveals a rubbing sound upon cardiac auscultation as well as increased jugular venous distention on inspiration. Pericardiocentesis is performed revealing grossly bloody fluid. Which of the following is most specifically associated with this patient's presentation?
- A. Myocardial infarction
- B. Malignancy (Correct Answer)
- C. Uremia
- D. Rheumatoid arthritis
- E. Viral illness
Pericardial diseases Explanation: ***Malignancy***
- The presence of **grossly bloody (hemorrhagic) pericardial fluid** is the key finding that most specifically points to **malignancy** as the underlying cause.
- **Hemorrhagic pericardial effusion** is most commonly associated with: (1) malignancy, (2) tuberculosis, or (3) trauma. Given the patient's **history of radiation therapy for breast cancer 20 years ago**, malignancy (either metastatic breast cancer or radiation-induced secondary malignancy) is the most likely cause.
- Clinical features like **chest pain** worse on inspiration and relieved by leaning forward, a **pericardial friction rub**, and **increased jugular venous distention on inspiration (Kussmaul sign)** indicate pericarditis with possible cardiac tamponade.
*Myocardial infarction*
- While myocardial infarction can lead to pericarditis (acute post-MI pericarditis or delayed Dressler's syndrome), the pericardial fluid is typically **serous or serosanguinous, not grossly bloody**.
- The patient's history of prior MI and CABG makes this less likely to be the cause of this acute presentation with hemorrhagic effusion.
- Post-MI pericarditis usually occurs within days to weeks after the MI event.
*Uremia*
- **Uremic pericarditis** occurs in patients with severe kidney failure (uremia) and typically presents with **serofibrinous exudate**, not grossly bloody effusion.
- There is no clinical indication of renal failure or uremia in this patient's presentation.
*Rheumatoid arthritis*
- **Rheumatoid pericarditis** can occur in patients with RA, but the pericardial effusion is usually **sterile and serofibrinous**, rarely resulting in frankly hemorrhagic fluid.
- While this patient has RA, the **grossly bloody fluid** and **history of breast cancer radiation** make malignancy a much more specific and likely diagnosis.
*Viral illness*
- **Viral pericarditis** is a common cause of acute pericarditis and typically presents with chest pain and a pericardial friction rub.
- However, viral pericarditis usually produces **serous or serofibrinous effusions, not grossly bloody fluid**.
- There is no mention of prodromal viral symptoms, and the hemorrhagic nature of the fluid strongly argues against a viral etiology.
Pericardial diseases US Medical PG Question 2: A 72-year-old man presents to the emergency department because of difficulty breathing and sharp chest pain. The chest pain increases in intensity with lying down, and it radiates to the scapular ridge. Approximately 3 weeks ago, he had an anterior ST-elevation myocardial infarction, which was treated with intravenous alteplase. He was discharged home in a stable condition. Current vital signs include a temperature of 38.1 (100.5°F), blood pressure of 131/91 mm Hg, and pulse of 99/min. On examination, heart sounds are distant and a scratching sound is heard on the left sternal border. ECG reveals widespread concave ST elevations in the precordial leads and PR depressions in leads V2-V6. Which of the following is the most likely cause of this patient condition?
- A. Recurrent infarction
- B. Myocarditis
- C. Aortic dissection
- D. Dressler’s syndrome (Correct Answer)
- E. Ventricular aneurysm
Pericardial diseases Explanation: ***Dressler’s syndrome***
- This syndrome, also known as **post-myocardial infarction syndrome**, typically presents weeks to months after an MI and is characterized by pleuritic chest pain, fever, and pericardial friction rub.
- The **widespread ST elevations (concave)** and **PR depressions** on ECG are classic findings of pericarditis, which is the underlying pathology of Dressler's syndrome.
*Recurrent infarction*
- While an MI can cause chest pain, the pain associated with infarction is typically **retrosternal, crushing**, and does not improve with leaning forward or worsen with lying down.
- ECG findings of recurrent MI would show **convex ST elevations** in a specific coronary artery territory, not widespread concave ST elevation.
*Myocarditis*
- Myocarditis can cause chest pain, fever, and ECG changes (including ST elevations), but it is primarily an **inflammation of the heart muscle** often due to viral infection.
- In this case, the **pericardial friction rub** and history of recent MI strongly point towards pericardial inflammation, not primarily myocardial inflammation.
*Aortic dissection*
- Aortic dissection presents with **severe, tearing chest pain** that often radiates to the back, but it typically has an abrupt onset and is not associated with a pericardial friction rub or widespread ST elevations.
- The ECG findings of pericarditis do not support acute aortic dissection.
*Ventricular aneurysm*
- A ventricular aneurysm is a late complication of MI and can lead to symptoms like heart failure or arrhythmias, but it does **not typically cause acute pericarditic chest pain** or associated ECG findings.
- While it can cause persistent ST elevation, it would not be widespread and concave, and it wouldn't be associated with a friction rub.
Pericardial diseases US Medical PG Question 3: A 36-year-old woman presents to the emergency department with chest discomfort and fatigue. She reports that her symptoms began approximately 1 week ago and are associated with shortness of breath, swelling of her legs, and worsening weakness. She’s been having transitory fevers for about 1 month and denies having similar symptoms in the past. Medical history is significant for systemic lupus erythematosus (SLE) treated with hydroxychloroquine. She had a SLE flare approximately 2 weeks prior to presentation, requiring a short course of prednisone. Physical exam was significant for a pericardial friction rub. An electrocardiogram showed widespread ST-segment elevation and PR depression. After extensive work-up, she was admitted for further evaluation, treatment, and observation. Approximately 2 days after admission she became unresponsive. Her temperature is 100°F (37.8°C), blood pressure is 75/52 mmHg, pulse is 120/min, and respirations are 22/min. Heart sounds are muffled. Which of the following is a clinical finding that will most likely be found in this patient?
- A. Warm extremities
- B. Pericardial knock
- C. Decreased systolic blood pressure by 8 mmHg with inspiration
- D. Jugular venous distension (Correct Answer)
- E. Unequal blood pressure measurements between both arms
Pericardial diseases Explanation: ***Jugular venous distension***
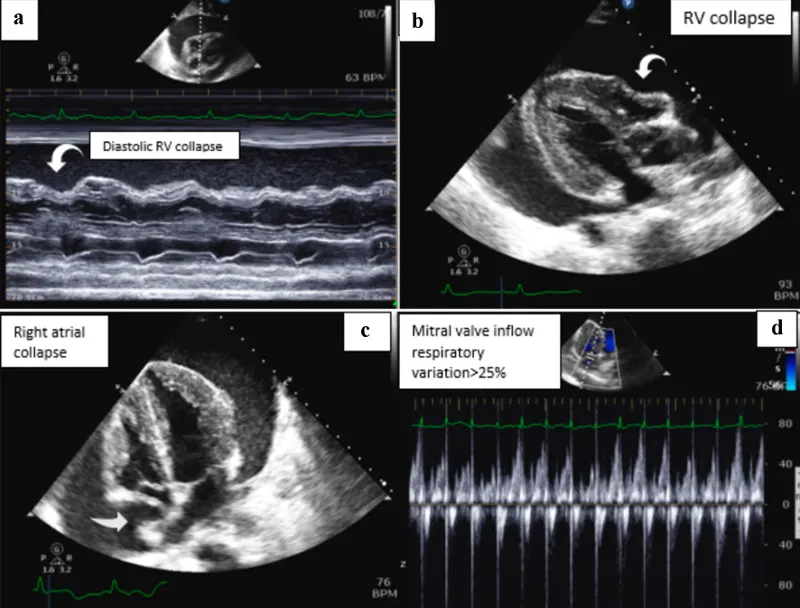
- The patient's presentation with **muffled heart sounds**, **hypotension**, and a **pericardial friction rub** points towards **cardiac tamponade**, a medical emergency caused by fluid accumulation in the pericardial sac.
- **Jugular venous distension** is a key component of **Beck's triad** (along with muffled heart sounds and hypotension) and indicates increased right atrial pressure due to restricted ventricular filling.
*Warm extremities*
- **Warm extremities** are more characteristic of **vasodilatory shock** (e.g., septic shock), where peripheral vasodilation leads to increased skin temperature.
- In **cardiac tamponade**, reduced cardiac output typically results in **cool and clammy extremities** due to compensatory peripheral vasoconstriction.
*Pericardial knock*
- A **pericardial knock** is an early diastolic sound often heard in **constrictive pericarditis**, caused by the sudden cessation of ventricular filling.
- While the patient has pericardial involvement, the acute presentation with signs of shock is more consistent with **cardiac tamponade**, rather than chronic constriction.
*Decreased systolic blood pressure by 8 mmHg with inspiration*
- **Pulsus paradoxus** (a decrease in systolic blood pressure of **>10 mmHg with inspiration**) is a hallmark sign of **cardiac tamponade**.
- While this patient likely has pulsus paradoxus, the value of **8 mmHg falls below the diagnostic threshold** of 10 mmHg and would not be considered pathological pulsus paradoxus.
- **Jugular venous distension** is a more reliable and clinically obvious finding in cardiac tamponade.
*Unequal blood pressure measurements between both arms*
- **Unequal blood pressure measurements between the arms** (>10-15 mmHg difference) are characteristic of conditions like **aortic dissection** or **subclavian artery stenosis**.
- This finding is not typically associated with **cardiac tamponade**, which affects global cardiac function.
Pericardial diseases US Medical PG Question 4: A 77-year-old woman presents to her physician because of fatigue and progressive dyspnea despite receiving optimal treatment for heart failure. Her medical history is positive for heart failure, active tuberculosis, and chronic renal failure, for which she has been in long-term hemodialysis (13 years). The woman currently takes rifampin and isoniazid. Her physical exam shows the presence of hepatomegaly and jugular venous distention that fails to subside on inspiration (Kussmaul's sign) and an impalpable apical impulse. Her pulse is 122/min, respiratory rate 16/min, temperature 36.0°C (97.4°F), and blood pressure 120/60 mm Hg. Her cardiac monitor shows a prominent y descent in her jugular venous pulse. A cardiac ultrasound shows pericardial calcifications and small tubular-shaped ventricles. Which of the following is the most likely cause of this patient's current condition?
- A. Constrictive pericarditis (Correct Answer)
- B. Dilated cardiomyopathy
- C. Atrial fibrillation
- D. Restrictive cardiomyopathy
- E. Hypertrophic cardiomyopathy
Pericardial diseases Explanation: ***Constrictive pericarditis***
- The patient presents with **fatigue, dyspnea, hepatomegaly, jugular venous distention with Kussmaul's sign**, and an **impalpable apical impulse**, all classic signs of **right-sided heart failure** due to impaired ventricular filling.
- The history of **tuberculosis** and **chronic renal failure** (risk factors for pericardial disease), along with **pericardial calcifications** and **small, tubular-shaped ventricles** on ultrasound, strongly points to constrictive pericarditis.
*Dilated cardiomyopathy*
- This condition is characterized by **ventricular dilation** and **systolic dysfunction**, leading to signs of both left and right heart failure.
- The ultrasound finding of **small, tubular-shaped ventricles** contradicts the definition of dilated cardiomyopathy.
*Atrial fibrillation*
- While atrial fibrillation can cause **palpitations, fatigue, and dyspnea**, it is an arrhythmia primarily affecting cardiac rhythm.
- It does not directly explain the **pericardial calcifications, Kussmaul's sign**, or the specific ventricular morphology seen on ultrasound.
*Restrictive cardiomyopathy*
- This condition involves increased **ventricular stiffness**, leading to impaired diastolic filling and typically presents with signs of **diastolic heart failure**.
- Although it can cause similar symptoms to constrictive pericarditis, it is primarily a **myocardial** disease and would not typically show **pericardial calcifications** on imaging.
*Hypertrophic cardiomyopathy*
- This involves **thickening of the ventricular walls**, often leading to **outflow tract obstruction** and **diastolic dysfunction**.
- The imaging showing **small, tubular-shaped ventricles** and **pericardial calcifications** are inconsistent with hypertrophic cardiomyopathy, which would show thickened myocardium.
Pericardial diseases US Medical PG Question 5: A 42-year-old woman presents with complaints of a sharp, stabbing pain in her chest upon coughing and inhalation. She says that the pain started acutely 2 days ago and has progressively worsened. Her past medical history is significant for a rash on her face, joint pains, and fatigue for the past few weeks. The patient is afebrile and her vital signs are within normal limits. On physical examination, there is a malar macular rash that spares the nasolabial folds. There is a friction rub at the cardiac apex that does not vary with respiration. Which of the following additional physical examination signs would most likely be present in this patient?
- A. Mid-systolic click
- B. Displaced apical impulse
- C. Chest pain that improves with leaning forward (Correct Answer)
- D. High-pitched diastolic murmur
- E. Pain improvement with inspiration
Pericardial diseases Explanation: ***Chest pain that improves with leaning forward***
- The patient's symptoms (malar rash, joint pains, fatigue, chest pain worse with coughing/inhalation, and an apical friction rub) are highly suggestive of **pericarditis secondary to Systemic Lupus Erythematosus (SLE)**.
- Pain from pericarditis is classically **relieved by leaning forward** as this position decreases the pressure on the inflamed pericardium.
*Mid-systolic click*
- A mid-systolic click is characteristic of **mitral valve prolapse**, which is not directly indicated by the patient's presenting symptoms or primary diagnosis of pericarditis.
- While SLE can be associated with various cardiac manifestations, a mid-systolic click is not a direct presentation of acute pericarditis.
*Displaced apical impulse*
- A displaced apical impulse typically suggests **ventricular enlargement** or conditions that shift the heart, such as a large **pericardial effusion**.
- While pericarditis can lead to effusion, the presence of a friction rub and acute onset does not immediately imply a significant enough effusion to displace the apical impulse.
*High-pitched diastolic murmur*
- A high-pitched diastolic murmur is characteristic of **aortic regurgitation** or, less commonly, **pulmonic regurgitation**.
- These are valvular abnormalities not directly linked to the acute pericarditis described in the patient's presentation.
*Pain improvement with inspiration*
- **Pleuritic chest pain**, often seen in conditions like pleurisy or pulmonary embolism, *worsens* with inspiration, not improves.
- The patient's pain worsening with inhalation rules out improvement with inspiration as a likely sign.
Pericardial diseases US Medical PG Question 6: A 41-year-old woman presents to the emergency room with chest pain. She has had progressive substernal chest pain accompanied by weakness and mild shortness of breath for the past 2 hours. Her past medical history is notable for poorly controlled systemic lupus erythematosus (SLE), Sjogren syndrome, and interstitial lung disease. She was hospitalized last year with pericarditis presumed to be from SLE. Her temperature is 98.6°F (37°C), blood pressure is 106/56 mmHg, pulse is 132/min, and respirations are 26/min. On exam, the skin overlying the internal jugular vein fills at 9 cm above the sternal angle and distant heart sounds are appreciated. There is no friction rub. She is given 1000cc of intravenous fluids with no appreciable change in her blood pressure. An electrocardiogram in this patient would most likely reveal which of the following findings?
- A. Polymorphic P waves
- B. ST elevations in leads II, III, and aVF
- C. Peaked T waves
- D. Wide QRS complexes with no P waves
- E. Electrical alternans (Correct Answer)
Pericardial diseases Explanation: ***Electrical alternans***
- The patient's symptoms (chest pain, shortness of breath, **hypotension**, **tachycardia**, **elevated JVP**, and **distant heart sounds**) in the context of a history of **pericarditis** and **SLE** are highly suggestive of **cardiac tamponade.**
- **Electrical alternans**, characterized by alternating QRS complex heights due to the swinging motion of the heart in a large pericardial effusion, is a classic EKG finding for cardiac tamponade.
- This finding reflects the mechanical swinging of the heart within the pericardial fluid, causing beat-to-beat variation in QRS amplitude.
*Polymorphic P waves*
- **Polymorphic P waves** (multifocal atrial tachycardia) occur when there are at least three different P wave morphologies on the EKG, indicating multiple ectopic atrial foci.
- This is typically seen in patients with severe lung disease or other conditions causing increased atrial stretch, but it is not a direct consequence or typical finding of cardiac tamponade.
*ST elevations in leads II, III, and aVF*
- **ST elevations in leads II, III, and aVF** indicate an **inferior myocardial infarction**, which is caused by coronary artery occlusion.
- While chest pain is present, the patient's other signs (elevated JVP, distant heart sounds, hypotension not responding to fluids, history of pericarditis/SLE) point away from an acute MI and strongly towards cardiac tamponade.
*Peaked T waves*
- **Peaked T waves** are characteristic of **hyperkalemia**, a condition of excessively high potassium levels in the blood.
- While hyperkalemia can cause cardiac symptoms, it does not typically present with the specific hemodynamic compromise and physical exam findings (elevated JVP, distant heart sounds) described, which are classic for cardiac tamponade.
*Wide QRS complexes with no P waves*
- **Wide QRS complexes with no P waves** are characteristic of a **ventricular arrhythmia**, such as ventricular tachycardia or idioventricular rhythm.
- While the patient is hypotensive and tachycardic, the presenting symptoms and physical exam findings are not directly indicative of a primary ventricular arrhythmia, but rather suggest an extracardiac compression of the heart due to tamponade.
Pericardial diseases US Medical PG Question 7: A 34-year-old Caucasian female presents at the ER with fever and sharp pain in her chest upon coughing and inhalation. Three weeks earlier she presented to her rheumatologist with a butterfly rash, joint pain and fatigue and was given a diagnosis of systemic lupus erythematosus. A friction rub is present upon physical exam. Which of the following do you most suspect in this patient?
- A. Pericardial tamponade
- B. Pericarditis (Correct Answer)
- C. Acute myocardial infarction
- D. Pulmonary hypertension
- E. Interstitial lung disease
Pericardial diseases Explanation: ***Pericarditis***
- The patient's symptoms of **sharp chest pain** worsened by coughing and inhalation, along with a **friction rub** upon examination, are classic signs of pericarditis.
- Her recent diagnosis of **systemic lupus erythematosus (SLE)** makes pericarditis a highly suspect complication, as SLE can affect the pericardium.
*Pericardial tamponade*
- While pericarditis can lead to tamponade, the clinical presentation here (chest pain, friction rub) more strongly points to **inflammation of the pericardium** rather than the signs of **hemodynamic compromise** seen in tamponade (e.g., muffled heart sounds, hypotension, jugular venous distention).
- There are no specific signs of **Beck's triad** (hypotension, muffled heart sounds, JVD) which would indicate tamponade.
*Acute myocardial infarction*
- The described **sharp chest pain worsened by inspiration and coughing** is atypical for myocardial infarction, which usually involves crushing or pressure-like pain.
- The presence of a **friction rub** is highly characteristic of pericarditis, not an MI.
*Pulmonary hypertension*
- Pulmonary hypertension typically presents with **dyspnea, fatigue, and signs of right-sided heart failure**, none of which are highlighted in this patient's acute presentation.
- **Chest pain** in pulmonary hypertension is usually exertion-related or due to right ventricular ischemia, not pleuritic.
*Interstitial lung disease*
- Interstitial lung disease primarily causes **progressive dyspnea and cough**, often with crackles on auscultation.
- The acute, pleuritic chest pain and **friction rub** are not characteristic findings of interstitial lung disease.
Pericardial diseases US Medical PG Question 8: A 73-year-old man with coronary artery disease and hypertension is brought to the emergency department by ambulance 90 minutes after the acute onset of substernal chest pain and dyspnea. He has smoked 2 packs of cigarettes daily for 52 years. Shortly after arriving at the hospital, he loses consciousness and is pulseless. Despite attempts at cardiopulmonary resuscitation, he dies. Examination of the heart at autopsy shows complete occlusion of the left anterior descending artery with a red thrombus overlying a necrotic plaque. Which of the following pathophysiologic mechanisms is most likely responsible for this patient's acute coronary condition?
- A. Influx of lipids into the endothelium
- B. Secretion of matrix metalloproteinases (Correct Answer)
- C. Release of platelet-derived growth factor
- D. Type III collagen deposition
- E. Proliferation of smooth muscle cells
Pericardial diseases Explanation: ***Secretion of matrix metalloproteinases***
- **Matrix metalloproteinases (MMPs)** degrade the **extracellular matrix** within the fibrous cap of an atherosclerotic plaque, leading to its **destabilization and rupture**.
- Plaque rupture then exposes the highly thrombogenic lipid core, initiating thrombus formation and acute coronary events like the **red thrombus** seen in the **left anterior descending artery (LAD)**.
*Influx of lipids into the endothelium*
- This process is characteristic of the **initial stages of atherosclerosis**, leading to **fatty streak formation**, not the acute plaque rupture and thrombosis described.
- While essential for plaque development, lipid influx alone does not directly explain aggressive plaque rupture and acute thrombus formation.
*Release of platelet-derived growth factor*
- **Platelet-derived growth factor (PDGF)** is primarily involved in **smooth muscle cell proliferation** and migration, contributing to plaque growth and thickening.
- Its role is more chronic and proliferative, not immediate plaque destabilization and rupture leading to acute thrombosis.
*Type III collagen deposition*
- **Type III collagen** is characteristic of early, developing atherosclerotic plaques and granulation tissue, contributing to plaque stability.
- Plaque vulnerability associated with rupture involves a **thin fibrous cap** with reduced **collagen content**, often due to increased collagen degradation.
*Proliferation of smooth muscle cells*
- **Smooth muscle cell proliferation** occurs during chronic atherosclerosis, contributing to the **fibrous cap formation** and overall plaque stability.
- In the context of acute plaque rupture, it is the *erosion* of the fibrous cap, often due to degradation, rather than proliferation, that is the immediate cause.
Pericardial diseases US Medical PG Question 9: A 51-year-old woman with hyperlipidemia comes to the physician because of weakness for one month. At the end of the day, she feels too fatigued to cook dinner or carry a laundry basket up the stairs. She also complains of double vision after she reads for long periods of time. All of her symptoms improve with rest. Her only medication is pravastatin. Physical examination shows drooping of the upper eyelids. Strength is initially 5/5 in the upper and lower extremities but decreases to 4/5 after a few minutes of sustained resistance. Sensation to light touch is intact and deep tendon reflexes are normal. Which of the following best describes the pathogenesis of this patient's condition?
- A. Type II hypersensitivity reaction (Correct Answer)
- B. Anterior horn cell destruction
- C. Impaired acetylcholine release
- D. Peripheral nerve demyelination
- E. Adverse drug effect
Pericardial diseases Explanation: ***Type II hypersensitivity reaction***
- This patient's symptoms of **fatigue** and **muscle weakness** that worsen with activity and improve with rest (**fatigable weakness**), along with **ptosis** (drooping eyelids) and **diplopia** (double vision), are classic for **myasthenia gravis**.
- Myasthenia gravis is an **autoimmune disease** characterized by autoantibodies that target and destroy **acetylcholine receptors** at the neuromuscular junction, leading to impaired signal transmission. This is a classic example of a **Type II hypersensitivity reaction**, where antibodies directly mediate cellular destruction or dysfunction.
*Anterior horn cell destruction*
- **Anterior horn cell destruction**, as seen in **amyotrophic lateral sclerosis (ALS)**, typically presents with both upper and lower motor neuron signs, such as **spasticity**, **hyperreflexia**, **fasciculations**, and **muscle atrophy**.
- In ALS, there is progressive weakness but typically **without fatigability** and oculomotor symptoms (ptosis, diplopia) are less common or occur late in the disease.
*Impaired acetylcholine release*
- **Impaired acetylcholine release** is characteristic of **Lambert-Eaton myasthenic syndrome (LEMS)**, which is often associated with small cell lung cancer.
- Unlike myasthenia gravis, LEMS typically shows **improvement in muscle strength with sustained activity** (due to increased presynaptic acetylcholine release), rather than worsening.
*Peripheral nerve demyelination*
- **Peripheral nerve demyelination** is the hallmark of conditions like **Guillain-Barré syndrome (GBS)** or **chronic inflammatory demyelinating polyneuropathy (CIDP)**.
- These conditions usually present with **sensory deficits**, **areflexia**, and **ascending paralysis/weakness**, which are absent in this patient.
*Adverse drug effect*
- While **statins** can cause **myopathy** (muscle pain and weakness), this typically involves diffuse muscle aches and elevated **creatine kinase** levels, and does not typically present with the classic fatigable weakness, ptosis, and diplopia seen here.
- The specific pattern of fatigable weakness improving with rest and affecting specific muscle groups (e.g., ocular muscles) points away from a simple statin-induced myopathy.
Pericardial diseases US Medical PG Question 10: A 47-year-old woman presents to her physician for difficulty swallowing. She states that she intentionally delayed seeing a physician for this issue. She says her primary issue with swallowing is that her mouth always feels dry so she has difficulty chewing food to the point that it can be swallowed. On physical examination, her oral mucosa appears dry. Both of her eyes also appear dry. Several enlarged lymph nodes are palpated. Which of the following patterns of reactive lymphadenitis is most commonly associated with this patient’s presentation?
- A. Sinus hyperplasia
- B. Follicular hyperplasia (Correct Answer)
- C. Diffuse hyperplasia
- D. Mixed B and T cell hyperplasia
- E. Paracortical hyperplasia
Pericardial diseases Explanation: ***Follicular hyperplasia***
- The patient's symptoms of **dry mouth (xerostomia)** and **dry eyes (xerophthalmia)** strongly suggest **Sjögren syndrome**. This autoimmune disease selectively affects **exocrine glands**, particularly the salivary and lacrimal glands.
- Lymphoid hyperplasia, especially **follicular hyperplasia**, is a common feature in Sjögren syndrome due to chronic B-cell activation, which is linked to a higher risk of developing **MALT lymphoma**.
*Sinus hyperplasia*
- **Sinus hyperplasia**, also known as **reticular hyperplasia**, is characterized by an increase in the number and size of macrophages within the subcapsular and medullary sinuses of lymph nodes.
- It is typically associated with **lymph nodes draining a site of malignancy** or conditions involving histiocytic proliferation.
*Diffuse hyperplasia*
- **Diffuse hyperplasia** involves a generalized expansion of all lymphoid components within the lymph node, without a predominance of any specific area.
- This pattern is less specific and can be seen in various **chronic inflammatory conditions** or reactive processes, but it is not the most characteristic pattern for Sjögren syndrome.
*Mixed B and T cell hyperplasia*
- While both B and T cells are involved in immune responses, **mixed B and T cell hyperplasia** refers to the expansion of both populations in a less defined pattern than follicular or paracortical types.
- Conditions like **toxoplasmosis** can present with mixed hyperplasia, but it is not the classic pattern seen in Sjögren syndrome.
*Paracortical hyperplasia*
- **Paracortical hyperplasia** involves the expansion of the paracortical areas of the lymph node, which are rich in T-lymphocytes.
- This pattern is typically seen in response to **viral infections** (e.g., infectious mononucleosis) or certain drug reactions, where T-cell activation is a prominent feature.
More Pericardial diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.