Myocarditis and cardiomyopathies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Myocarditis and cardiomyopathies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Myocarditis and cardiomyopathies US Medical PG Question 1: A 43-year-old woman presents to her primary care provider with shortness of breath. She reports a 4-month history of progressively worsening difficulty breathing with associated occasional chest pain. She is a long-distance runner but has had trouble running recently due to her breathing difficulties. Her past medical history is notable for well-controlled hypertension for which she takes hydrochlorothiazide. She had a tibial osteosarcoma lesion with pulmonary metastases as a child and successfully underwent chemotherapy and surgical resection. She has a 10 pack-year smoking history but quit 15 years ago. She drinks a glass of wine 3 times per week. Her temperature is 98.6°F (37°C), blood pressure is 140/85 mmHg, pulse is 82/min, and respirations are 18/min. On exam, she has increased work of breathing with a normal S1 and loud P2. An echocardiogram in this patient would most likely reveal which of the following?
- A. Biventricular dilatation with a decreased ejection fraction
- B. Left ventricular dilatation with an incompetent aortic valve
- C. Left atrial dilatation with mitral valve stenosis
- D. Right ventricular hypertrophy with a dilated pulmonary artery (Correct Answer)
- E. Left ventricular hypertrophy with a bicuspid aortic valve
Myocarditis and cardiomyopathies Explanation: The patient's history of **pulmonary metastases** (even successfully treated) and a **loud P2 heart sound** suggest **pulmonary hypertension**, which leads to increased afterload on the right ventricle. [1] **Pulmonary hypertension** causes the **right ventricle to hypertrophy** to overcome the elevated pulmonary arterial pressure, and the **pulmonary artery itself often dilates** due to the sustained high pressure. [1] [2] This describes **dilated cardiomyopathy**, which typically presents with **symptoms of heart failure** but doesn't specifically explain the **loud P2**, which points to pulmonary hypertension. [2]
Myocarditis and cardiomyopathies US Medical PG Question 2: A 72-year-old African American man presents with progressive fatigue, difficulty breathing on exertion, and lower extremity swelling for 3 months. The patient was seen at the emergency department 2 times before. The first time was because of back pain, and the second was because of fever and cough. He took medications at the emergency room, but he refused to do further tests recommended to him. He does not smoke or drink alcohol. His family history is irrelevant. His vital signs include a blood pressure of 110/80 mm Hg, temperature of 37.2°C (98.9°F), and regular radial pulse of 90/min. On physical examination, the patient looks pale, and his tongue is enlarged. Jugular veins become distended on inspiration. Pitting ankle edema is present on both sides. Bilateral basal crackles are audible on the chest auscultation. Hepatomegaly is present on abdominal palpation. Chest X-ray shows osteolytic lesions of the ribs. ECG shows low voltage waves and echocardiogram shows a speckled appearance of the myocardium with diastolic dysfunction and normal appearance of the pericardium. Which of the following best describes the mechanism of this patient’s illness?
- A. Thickening of the parietal pericardium with dystrophic calcification
- B. Calcification of the aortic valve orifice with obstruction of the left ventricular outflow tract
- C. Concentric hypertrophy of the myocytes with thickening of the interventricular septum
- D. Diastolic cardiac dysfunction with reciprocal variation in ventricular filling with respiration
- E. Deposition of an extracellular fibrillar protein that stains positive for Congo red in the myocardium (Correct Answer)
Myocarditis and cardiomyopathies Explanation: - ***Deposition of an extracellular fibrillar protein that stains positive for Congo red in the myocardium***
- The patient's presentation with **progressive fatigue, dyspnea, edema, enlarged tongue, jugular venous distention with inspiration** (Kussmaul's sign), **basal crackles, hepatomegaly, osteolytic lesions, low voltage on ECG, and a speckled appearance of the myocardium on echocardiogram with diastolic dysfunction** is highly suggestive of **amyloidosis**.
- **Amyloidosis** involves the deposition of misfolded, insoluble **fibrillar proteins** in various tissues, including the heart, leading to restrictive cardiomyopathy. These amyloid deposits typically stain **positive with Congo red** and demonstrate **apple-green birefringence** under polarized light.
- *Thickening of the parietal pericardium with dystrophic calcification*
- This description is characteristic of **constrictive pericarditis**, which can cause symptoms similar to restrictive cardiomyopathy (e.g., Kussmaul's sign, edema).
- However, the echocardiogram in this patient shows a **speckled appearance of the myocardium** and a **normal pericardium**, ruling out constrictive pericarditis.
- *Calcification of the aortic valve orifice with obstruction of the left ventricular outflow tract*
- This describes **aortic stenosis**, which would lead to signs of left ventricular outflow obstruction, such as a systolic murmur and possibly left ventricular hypertrophy.
- While it can cause dyspnea and fatigue, it does not typically explain the **speckled myocardium**, **enlarged tongue**, or **osteolytic lesions** seen in this patient.
- *Concentric hypertrophy of the myocytes with thickening of the interventricular septum*
- This is characteristic of **hypertensive heart disease** or **hypertrophic cardiomyopathy**.
- While these conditions can cause diastolic dysfunction, they typically do not present with **osteolytic lesions**, **enlarged tongue**, or the **speckled appearance of the myocardium** on echocardiography that is seen in amyloidosis.
- *Diastolic cardiac dysfunction with reciprocal variation in ventricular filling with respiration*
- While **diastolic cardiac dysfunction** is present, this option is too general and describes a physiological consequence rather than the underlying mechanism for the constellation of symptoms.
- **Reciprocal variation in ventricular filling with respiration** can be seen in both restrictive cardiomyopathy and constrictive pericarditis but does not explain the specific findings of **osteolytic lesions** or **enlarged tongue**, which point towards a systemic infiltrative disease like amyloidosis.
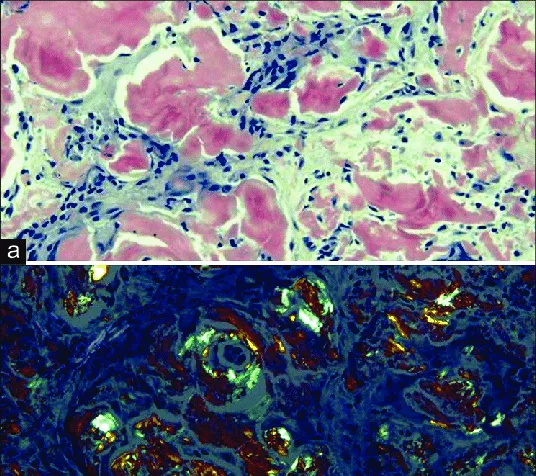
Myocarditis and cardiomyopathies US Medical PG Question 3: A 49-year-old man presents to his physician complaining of weakness and fatigue. On exam, you note significant peripheral edema. Transthoracic echocardiogram is performed and reveals a preserved ejection fraction with impaired diastolic relaxation. A representative still image is shown in Image A. Which of the following is likely the cause of this patient's symptoms?
- A. Hemochromatosis (Correct Answer)
- B. Heavy, long-term alcohol consumption
- C. History of myocardial infarction
- D. History of a recent viral infection
- E. Previous treatment with doxorubicin
Myocarditis and cardiomyopathies Explanation: ***Hemochromatosis***
- **Hemochromatosis** can lead to **restrictive cardiomyopathy** due to iron deposition in the myocardium, causing **diastolic dysfunction** with a **preserved ejection fraction**.
- The symptoms of **weakness**, **fatigue**, and **peripheral edema** are consistent with **heart failure** secondary to this cardiac impairment.
*Heavy, long-term alcohol consumption*
- **Alcoholic cardiomyopathy** typically presents as **dilated cardiomyopathy**, characterized by **systolic dysfunction** and a **reduced ejection fraction**, which contradicts the preserved ejection fraction seen in this patient.
- While chronic alcohol use can cause heart failure symptoms, the specific echocardiographic findings do not align with this etiology.
*History of myocardial infarction*
- A **myocardial infarction** commonly leads to **systolic dysfunction** or **ischemic cardiomyopathy**, resulting in a **reduced ejection fraction** due to scar tissue formation and impaired contractility.
- The patient's preserved ejection fraction and primary diastolic relaxation abnormality make this diagnosis less likely.
*History of a recent viral infection*
- A recent viral infection can cause **viral myocarditis**, which typically leads to **dilated cardiomyopathy** and **systolic dysfunction** with a **reduced ejection fraction**.
- The observed preserved ejection fraction and isolated diastolic relaxation impairment are not characteristic features of acute viral myocarditis.
*Previous treatment with doxorubicin*
- **Doxorubicin** (an anthracycline) is a well-known cardiotoxic agent that causes **dilated cardiomyopathy** with a **reduced ejection fraction**, primarily affecting **systolic function**.
- The patient's preserved ejection fraction makes doxorubicin-induced cardiotoxicity an unlikely cause of his current presentation.
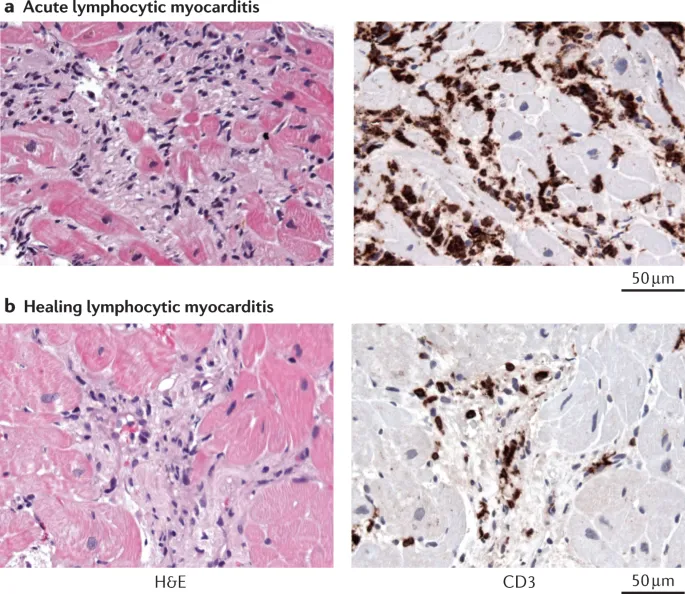
Myocarditis and cardiomyopathies US Medical PG Question 4: A 22-year-old male varsity athlete visits the on-campus health services for shortness of breath, fatigue, and lower limb edema with onset 1 week after mild upper respiratory tract infection. Upon physical examination, his blood pressure is 100/68 mm Hg, heart rate is 120/min, respiratory rate is 23/min, and temperature is 36.4°C (97.5°F). He is referred to the nearest hospital, where his systolic pressure drops below 90 mm Hg with an S3 gallop, and he needs inotropic support in the critical care unit. A chest radiograph shows an enlarged heart, clear lungs, and effacement of the right costodiaphragmatic angle. A subsequent esophageal echocardiogram reveals severe dilation of all heart cavities, an ejection fraction of 23%, and mitral regurgitation. His family and personal history are unremarkable; therefore, an endomyocardial biopsy (EMB) is ordered. Which of the following microscopic findings would you expect in this specimen?
- A. Infiltration with neutrophils
- B. Infiltration with lymphocytes (Correct Answer)
- C. Infiltration with granulomas
- D. Infiltration with eosinophils
- E. Infiltration with giant cells
Myocarditis and cardiomyopathies Explanation: ***Infiltration with lymphocytes***
- The patient's presentation with **heart failure symptoms** following an **upper respiratory tract infection**, coupled with **dilated cardiomyopathy** and **reduced ejection fraction**, strongly suggests **viral myocarditis**.
- **Lymphocytic infiltration** of the myocardium is the hallmark microscopic finding in **viral myocarditis**, representing the immune response to viral infection of cardiac myocytes.
*Infiltration with neutrophils*
- **Neutrophilic infiltrates** are typically characteristic of **acute bacterial infections** or **ischemic injury** within the myocardium, rather than post-viral myocarditis.
- While neutrophils may be present early in severe inflammatory responses, they are not the predominant or defining feature of **viral myocarditis**.
*Infiltration with granulomas*
- The presence of **granulomas** in the myocardium is indicative of conditions such as **sarcoidosis**, **tuberculosis**, or **giant cell myocarditis**, none of which fit the patient's acute post-viral presentation.
- These conditions typically have a more insidious onset or different systemic manifestations.
*Infiltration with eosinophils*
- **Eosinophilic infiltration** of the myocardium is characteristic of **hypersensitivity myocarditis** (often drug-induced) or **parasitic infections** like trichinellosis, which are not suggested by the patient's history.
- **Eosinophilic myocarditis** can also occur in various systemic diseases but is not associated with routine viral infections.
*Infiltration with giant cells*
- **Giant cells** in the myocardium are the defining feature of **giant cell myocarditis**, a rare and aggressive form of myocarditis distinct from typical viral myocarditis.
- **Giant cell myocarditis** often has a fulminant course and is usually characterized by more widespread myocyte necrosis and a poorer prognosis, and while it could be considered in severe cases, lymphocytic infiltration is more common after a viral illness.
Myocarditis and cardiomyopathies US Medical PG Question 5: A 28-year-old man presents to the clinic with increasing shortness of breath, mild chest pain at rest, and fatigue. He normally lives a healthy lifestyle with moderate exercise and an active social life, but recently he has been too tired to do much. He reports that he is generally healthy and on no medications but did have a ‘cold’ 2 weeks ago. He does not smoke, besides occasional marijuana with friends, and only drinks socially. His father has hypertension, hyperlipidemia, and lung cancer after a lifetime of smoking, and his mother is healthy. He also has one older brother with mild hypertension. His pulse is 104/min, the respiratory rate 23/min, the blood pressure 105/78 mm Hg, and the temperature 37.1°C (98.8°F). On physical examination, he is ill-appearing and has difficulty completing sentences. On auscultation he has a third heart sound, and his point of maximal impact is displaced laterally. He has 2+ pitting edema of the lower extremities up to the knees. An ECG is obtained and shows premature ventricular complexes and mildly widened QRS complexes. An echocardiogram is also performed and shows global hypokinesis with a left ventricle ejection fraction of 39%. Of the following, what is the most likely cause of his symptoms?
- A. Amyloidosis
- B. Cocaine abuse
- C. Unstable angina
- D. Coxsackievirus infection (Correct Answer)
- E. Acute myocardial infarction
Myocarditis and cardiomyopathies Explanation: ***Coxsackievirus infection***
- The patient's recent **viral prodrome** ("cold" 2 weeks ago) followed by rapid onset of heart failure symptoms, including **dilated cardiomyopathy** (global hypokinesis, EF 39%), is highly suggestive of **viral myocarditis**, with Coxsackievirus being a common cause.
- Findings like a **third heart sound (S3)**, **displaced point of maximal impact (PMI)**, **2+ pitting edema**, and ECG abnormalities (PVCs, widened QRS) are consistent with **heart failure** secondary to myocardial damage.
*Amyloidosis*
- **Amyloidosis** typically causes **restrictive cardiomyopathy** or stiff heart syndrome, not dilated cardiomyopathy with global hypokinesis, and often presents in older patients with systemic involvement.
- While it can cause heart failure, the sudden onset after a viral illness in a young patient makes it less likely.
*Cocaine abuse*
- **Cocaine abuse** can lead to cardiomyopathy, but it usually presents acutely with vasospasm and myocardial infarction, or chronic cardiomyopathy.
- The patient's history of only occasional marijuana use and social drinking does not support significant substance abuse as the primary cause here.
*Unstable angina*
- **Unstable angina** is characterized by chest pain due to myocardial ischemia, but it does not directly explain global hypokinesis, a low ejection fraction, or the systemic signs of heart failure (edema, S3).
- The symptoms are more consistent with myocardial dysfunction rather than transient ischemia.
*Acute myocardial infarction*
- While an **acute myocardial infarction (MI)** can cause heart failure, the patient's symptoms are more diffuse (global hypokinesis rather than regional wall motion abnormalities expected in an MI) and developed over two weeks after a viral illness.
- An MI would typically present with more acute and severe chest pain, and the ECG findings (PVCs, widened QRS) are not definitive for an acute infarct without ST elevation or significant Q waves.
Myocarditis and cardiomyopathies US Medical PG Question 6: A 14-year-old boy who has been otherwise healthy presents to his doctor complaining of feeling easily winded and light-headed at basketball practice. He has never felt this way before and is frustrated because he is good enough to make varsity this year. He denies smoking, alcohol, or recreational drug use. His mother is very worried because her oldest son and brother had both died suddenly while playing sports despite being otherwise healthy. The transthoracic echocardiogram confirms the suspected diagnosis, which demonstrates a preserved ejection fraction and systolic anterior motion of the mitral valve. The patient is advised that he will need to stay hydrated and avoid intense exercise, and he will likely need an ICD due to his family history. Which of the following physical exam findings is consistent with this patient’s most likely diagnosis?
- A. Tricuspid regurgitation
- B. Systolic ejection murmur that radiates to the carotids
- C. S3 heart sound
- D. Mitral regurgitation
- E. Systolic ejection murmur that worsens with the Valsalva maneuver (Correct Answer)
Myocarditis and cardiomyopathies Explanation: ***Systolic ejection murmur that worsens with the Valsalva maneuver***
- The patient's presentation with **syncope/lightheadedness during exertion**, family history of **sudden cardiac death in athletes**, and echocardiogram findings of **systolic anterior motion (SAM) of the mitral valve** are classic for **hypertrophic cardiomyopathy (HCM)**.
- The murmur of HCM is typically a **systolic ejection murmur** that **worsens with maneuvers that decrease preload**, such as the **Valsalva maneuver** or standing, because this reduction in ventricular volume exacerbates the left ventricular outflow tract (LVOT) obstruction.
*Tricuspid regurgitation*
- This is typically associated with **right heart failure** or **pulmonary hypertension**, which are not indicated by the patient's symptoms or echo findings.
- While it can be heard as a **systolic murmur**, it usually accentuates with inspiration (Carvallo's sign) and does not worsen with the Valsalva maneuver in the context of hypertrophic cardiomyopathy.
*Systolic ejection murmur that radiates to the carotids*
- A systolic ejection murmur radiating to the carotids is characteristic of **aortic stenosis**, which involves a fixed obstruction of the aortic valve.
- While both HCM and aortic stenosis cause systolic murmurs, HCM's murmur has different auscultatory behavior with preload-altering maneuvers (worsening with Valsalva) compared to aortic stenosis (which often softens or is unchanged).
*S3 heart sound*
- An **S3 heart sound** is typically a low-pitched diastolic sound associated with **volume overload** and **heart failure with reduced ejection fraction**, indicating rapid ventricular filling into a dilated ventricle.
- The patient's echocardiogram shows a **preserved ejection fraction**, and his symptoms are related to outflow obstruction, not volume overload.
*Mitral regurgitation*
- While **mitral regurgitation (MR)** can occur in HCM due to systolic anterior motion (SAM) of the mitral valve causing malcoaptation, the primary murmur heard due to the **LVOT obstruction** is a **systolic ejection murmur**.
- The murmur of MR is typically a **holosystolic murmur** that radiates to the axilla and usually **softens with the Valsalva maneuver** as reduced preload can decrease the severity of regurgitation.
Myocarditis and cardiomyopathies US Medical PG Question 7: An 18-year-old boy is brought to the emergency department by his parents because he suddenly collapsed while playing football. His parents mention that he had complained of dizziness while playing before, but never fainted in the middle of a game. On physical examination, the blood pressure is 130/90 mm Hg, the respirations are 15/min, and the pulse is 110/min. The chest is clear, but a systolic ejection murmur is present. The remainder of the examination revealed no significant findings. An electrocardiogram is ordered, along with an echocardiogram. He is diagnosed with hypertrophic cardiomyopathy and the physician lists all the precautions he must follow. Which of the following drugs will be on the list of contraindicated substances?
- A. Βeta-blockers
- B. Dobutamine
- C. Nitrates (Correct Answer)
- D. Calcium channel blockers
- E. Potassium channel blockers
Myocarditis and cardiomyopathies Explanation: ***Nitrates***
- **Nitrates** cause **vasodilation**, which decreases **preload** and worsens **left ventricular outflow tract obstruction (LVOTO)** in **hypertrophic cardiomyopathy (HCM)**, potentially leading to syncope or sudden death.
- Reduced preload exacerbates the dynamic obstruction, causing a critical drop in cardiac output.
- **Commonly encountered substances** patients must avoid include nitroglycerin, isosorbide, and **phosphodiesterase-5 inhibitors** (sildenafil, tadalafil) which potentiate nitrate effects.
- This is a critical counseling point for HCM patients in everyday life.
*Beta-blockers*
- **Beta-blockers** are **first-line treatment** for **hypertrophic cardiomyopathy (HCM)** as they reduce heart rate, improve diastolic filling, and decrease contractility, thereby reducing **LVOTO**.
- They alleviate symptoms and reduce the risk of sudden cardiac death in HCM.
*Dobutamine*
- **Dobutamine** is a **beta-1 adrenergic agonist** that increases contractility and heart rate, which would worsen **LVOTO** in HCM.
- While also contraindicated in HCM, dobutamine is only used in **controlled hospital settings** for stress testing or hemodynamic support, not a substance patients encounter in daily life.
- The question focuses on outpatient counseling about substances to avoid in everyday situations.
*Calcium channel blockers*
- **Non-dihydropyridine calcium channel blockers** (verapamil, diltiazem) are used in **HCM management**, particularly in patients who cannot tolerate beta-blockers.
- They improve **diastolic function** and reduce **LVOTO** by decreasing contractility and heart rate.
- **Caution:** Dihydropyridines (nifedipine, amlodipine) can worsen obstruction and should be avoided.
*Potassium channel blockers*
- **Antiarrhythmics** like **amiodarone** (potassium channel blocker) are used in **HCM** patients for atrial or ventricular arrhythmias.
- Not contraindicated; therapeutically indicated for rhythm management.
Myocarditis and cardiomyopathies US Medical PG Question 8: A 51-year-old man comes to the physician because of progressively worsening dyspnea on exertion and fatigue for the past 2 months. Cardiac examination shows no murmurs or bruits. Coarse crackles are heard at the lung bases bilaterally. An ECG shows an irregularly irregular rhythm with absent p waves. An x-ray of the chest shows globular enlargement of the cardiac shadow with prominent hila and bilateral fluffy infiltrates. Transthoracic echocardiography shows a dilated left ventricle with an ejection fraction of 40%. Which of the following is the most likely cause of this patient's condition?
- A. Acute psychological stress
- B. Deposition of misfolded proteins
- C. Inherited β-myosin heavy chain mutation
- D. Uncontrolled essential hypertension
- E. Tachycardia-induced cardiomyopathy secondary to atrial fibrillation (Correct Answer)
Myocarditis and cardiomyopathies Explanation: ***Tachycardia-induced cardiomyopathy secondary to atrial fibrillation***
- The patient presents with **progressively worsening dyspnea on exertion** and **fatigue**, along with signs of **heart failure** (globular cardiac shadow, prominent hila, bilateral fluffy infiltrates).
- The **ECG finding of an irregularly irregular rhythm with absent P waves** is characteristic of **atrial fibrillation**, and a dilated left ventricle with an **ejection fraction of 40%** indicates **dilated cardiomyopathy**, which can be caused by chronic tachycardia in atrial fibrillation.
*Acute psychological stress*
- Acute psychological stress can lead to **Takotsubo cardiomyopathy** (stress-induced cardiomyopathy), which typically presents with **transient left ventricular apical ballooning** and preserved basal contractility, not necessarily a globally dilated left ventricle in this context.
- While it can cause heart failure symptoms, the **chronic nature** of the symptoms (2 months) and the presence of **atrial fibrillation** make it a less likely primary cause here.
*Deposition of misfolded proteins*
- **Amyloidosis**, characterized by the deposition of misfolded proteins, primarily causes **restrictive cardiomyopathy**, leading to impaired diastolic filling rather than primarily systolic dysfunction with a dilated ventricle.
- While amyloidosis can manifest with HF symptoms, the echocardiographic finding of a **dilated left ventricle** and the strong evidence for atrial fibrillation contributing to tachycardia-induced cardiomyopathy make this less likely.
*Inherited β-myosin heavy chain mutation*
- This mutation is classically associated with **hypertrophic cardiomyopathy**, characterized by **left ventricular hypertrophy** and impaired diastolic function, often with a normal or increased ejection fraction initially.
- The patient's echocardiogram shows a **dilated left ventricle** with reduced ejection fraction, which is inconsistent with typical hypertrophic cardiomyopathy.
*Uncontrolled essential hypertension*
- Chronic uncontrolled hypertension typically leads to **hypertensive heart disease**, initially causing **left ventricular hypertrophy** and eventual **diastolic dysfunction**, before progressing to dilated cardiomyopathy in very advanced stages.
- While possible, the prominent **irregularly irregular rhythm with absent P waves** guiding towards atrial fibrillation as a direct cause of tachycardia-induced cardiomyopathy makes it a more specific and likely cause in this scenario.
Myocarditis and cardiomyopathies US Medical PG Question 9: A 16-year-old boy is brought to the emergency department 20 minutes after collapsing while playing basketball. There is no personal or family history of serious illness. On arrival, there is no palpable pulse and no respiratory effort is seen. He is declared dead. The family agrees to an autopsy. Which of the following is most likely to be found in this patient?
- A. Defect in the atrial septum
- B. Interventricular septal hypertrophy (Correct Answer)
- C. Pericardial fluid collection
- D. Postductal narrowing of the aorta
- E. Atheromatous plaque rupture
Myocarditis and cardiomyopathies Explanation: ***Interventricular septal hypertrophy***
- This presentation is highly suggestive of **hypertrophic cardiomyopathy (HCM)**, which is characterized by **left ventricular hypertrophy**, especially of the interventricular septum, leading to outflow obstruction and sudden cardiac arrest, particularly in young athletes.
- **Sudden collapse during strenuous exercise** in a young, otherwise healthy individual with no prior history of illness is a classic presentation of HCM.
*Defect in the atrial septum*
- An **atrial septal defect (ASD)** typically presents with a **murmur** and may lead to heart failure or pulmonary hypertension later in life, but it is an unlikely cause of sudden death in an adolescent during exercise.
- While it can cause cardiac symptoms, sudden collapse without prior symptoms is uncommon, and the primary pathological finding would be a hole, not hypertrophy.
*Pericardial fluid collection*
- A significant pericardial fluid collection that causes sudden collapse would indicate **pericardial tamponade**, which is usually associated with clear signs of circulatory collapse (e.g., **Beck's triad** - muffled heart sounds, jugular venous distension, hypotension) and is often due to trauma, infection, or malignancy, which are not suggested here.
- The sudden, unheralded nature of collapse during exercise points away from conditions that typically have more gradual onset or preceding symptoms.
*Postductal narrowing of the aorta*
- **Coarctation of the aorta** can cause hypertension and may lead to heart failure or aortic rupture, but it typically presents with **blood pressure discrepancies** between the upper and lower extremities and a characteristic murmur, not sudden cardiac death during exercise without prior symptoms.
- While it can be severe, sudden death usually results from complications like aortic dissection or rupture after a period of untreated hypertension, not acute collapse in a seemingly healthy individual.
*Atheromatous plaque rupture*
- **Atherosclerosis** and plaque rupture are the underlying cause of most **myocardial infarctions** in adults, but they are extremely rare in a 16-year-old without significant risk factors or a history of lipid disorders.
- The patient's age and lack of predisposing factors make this an improbable finding for sudden cardiac death.
Myocarditis and cardiomyopathies US Medical PG Question 10: A 73-year-old man with coronary artery disease and hypertension is brought to the emergency department by ambulance 90 minutes after the acute onset of substernal chest pain and dyspnea. He has smoked 2 packs of cigarettes daily for 52 years. Shortly after arriving at the hospital, he loses consciousness and is pulseless. Despite attempts at cardiopulmonary resuscitation, he dies. Examination of the heart at autopsy shows complete occlusion of the left anterior descending artery with a red thrombus overlying a necrotic plaque. Which of the following pathophysiologic mechanisms is most likely responsible for this patient's acute coronary condition?
- A. Influx of lipids into the endothelium
- B. Secretion of matrix metalloproteinases (Correct Answer)
- C. Release of platelet-derived growth factor
- D. Type III collagen deposition
- E. Proliferation of smooth muscle cells
Myocarditis and cardiomyopathies Explanation: ***Secretion of matrix metalloproteinases***
- **Matrix metalloproteinases (MMPs)** degrade the **extracellular matrix** within the fibrous cap of an atherosclerotic plaque, leading to its **destabilization and rupture**.
- Plaque rupture then exposes the highly thrombogenic lipid core, initiating thrombus formation and acute coronary events like the **red thrombus** seen in the **left anterior descending artery (LAD)**.
*Influx of lipids into the endothelium*
- This process is characteristic of the **initial stages of atherosclerosis**, leading to **fatty streak formation**, not the acute plaque rupture and thrombosis described.
- While essential for plaque development, lipid influx alone does not directly explain aggressive plaque rupture and acute thrombus formation.
*Release of platelet-derived growth factor*
- **Platelet-derived growth factor (PDGF)** is primarily involved in **smooth muscle cell proliferation** and migration, contributing to plaque growth and thickening.
- Its role is more chronic and proliferative, not immediate plaque destabilization and rupture leading to acute thrombosis.
*Type III collagen deposition*
- **Type III collagen** is characteristic of early, developing atherosclerotic plaques and granulation tissue, contributing to plaque stability.
- Plaque vulnerability associated with rupture involves a **thin fibrous cap** with reduced **collagen content**, often due to increased collagen degradation.
*Proliferation of smooth muscle cells*
- **Smooth muscle cell proliferation** occurs during chronic atherosclerosis, contributing to the **fibrous cap formation** and overall plaque stability.
- In the context of acute plaque rupture, it is the *erosion* of the fibrous cap, often due to degradation, rather than proliferation, that is the immediate cause.
More Myocarditis and cardiomyopathies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.