Ischemic heart disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ischemic heart disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ischemic heart disease US Medical PG Question 1: A 42-year-old woman presents to the urgent care clinic with recurrent chest pain and pressure radiating to her jaw. ECG is obtained and shows ST-segment elevation, but her cardiac enzymes are repeatedly found to be within normal ranges. She has a heart rate of 82/min and a blood pressure of 128/76 mm Hg. Physical examination reveals regular heart sounds with no friction rub. Which of the following options is an acceptable treatment regimen for this patient’s suspected condition?
- A. Calcium channel blockers and nitrates (Correct Answer)
- B. Nitrates only
- C. Beta-blockers, nitrates and aspirin
- D. Aspirin and clopidogrel
- E. Aspirin, clopidogrel, beta-blockers, and nitrates
Ischemic heart disease Explanation: **Calcium channel blockers and nitrates**
- This patient likely has **Prinzmetal's angina** (vasospastic angina), characterized by recurrent chest pain, ST-segment elevation on ECG, and normal cardiac enzymes, consistent with **coronary artery spasm**.
- **Calcium channel blockers** (e.g., diltiazem, amlodipine) and **nitrates** are the cornerstone of treatment, as they directly relax coronary arteries and prevent spasms.
*Nitrates only*
- While **nitrates** can alleviate acute symptoms of Prinzmetal's angina by vasodilation, they are generally **insufficient for long-term prevention** of recurrent spasms.
- **Calcium channel blockers** are crucial for sustained prophylaxis against vasospasm.
*Beta-blockers, nitrates and aspirin*
- **Beta-blockers** are generally **contraindicated** in Prinzmetal's angina as they can worsen **coronary artery spasm** by blocking beta-2 mediated vasodilation, leading to unopposed alpha-adrenergic vasoconstriction.
- **Aspirin** is not the primary treatment for vasospastic angina, as the pain is due to spasm rather than thrombotic occlusion.
*Aspirin and clopidogrel*
- **Aspirin** and **clopidogrel** are **antiplatelet agents** primarily used to prevent thrombus formation in atherosclerotic coronary artery disease.
- They are not indicated as a first-line treatment for Prinzmetal's angina, where chest pain is due to **coronary vasospasm**, not platelet aggregation.
*Aspirin, clopidogrel, beta-blockers, and nitrates*
- This combination includes several treatments that are either **ineffective** or **harmful** for Prinzmetal's angina.
- **Beta-blockers** are contraindicated, and **antiplatelet agents** (aspirin, clopidogrel) are not primary treatments for vasospasm.
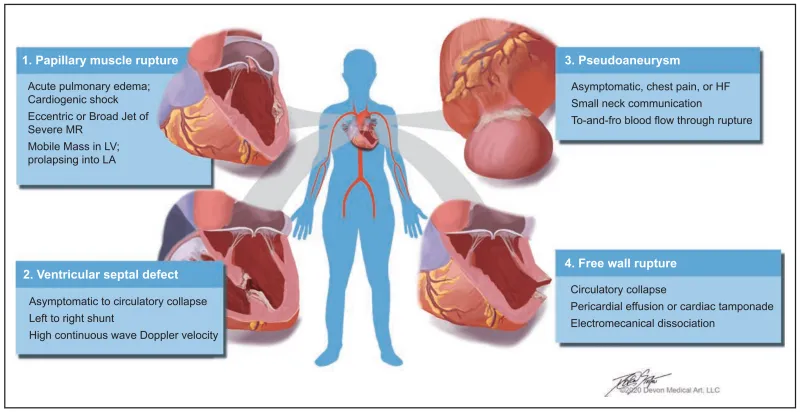
Ischemic heart disease US Medical PG Question 2: A 76-year-old man is admitted to the hospital for evaluation of sudden-onset chest pain. Three days after admission, he develops severe shortness of breath. Despite appropriate care, the patient dies. The heart at autopsy is shown. Which of the following most likely contributed to this patient's cause of death?
- A. Rupture of the interventricular septum
- B. Pseudoaneurysmal dilation of the left ventricle
- C. Exudative inflammation of the pericardium
- D. Occlusion of the posterior descending artery (Correct Answer)
- E. Bacterial infection of the mitral valve endocardium
Ischemic heart disease Explanation: ***Occlusion of the posterior descending artery***
- The image suggests a **large inferoposterior myocardial infarction**, impacting the posterior descending artery (PDA) territory, which supplies the posterior 1/3 of the interventricular septum and inferior wall of the left ventricle.
- An extensive infarction three days prior could lead to **cardiac rupture** or severe heart failure, resulting in sudden death.
*Rupture of the interventricular septum*
- A septal rupture can lead to a **ventricular septal defect**, causing a left-to-right shunt and heart failure, which might manifest as shortness of breath.
- This complication typically occurs within the first week following an **anterior or inferior myocardial infarction**, but the image points more directly to the cause of the infarction itself.
*Pseudoaneurysmal dilation of the left ventricle*
- A pseudoaneurysm is an **incomplete myocardial rupture** contained by pericardial adhesions, which can develop days to weeks post-MI and may rupture.
- While a life-threatening complication, the image primarily shows the infarct and not a distinct pseudoaneurysm.
*Exudative inflammation of the pericardium*
- **Fibrinous pericarditis** is common after transmural MI (Dressler syndrome or early pericarditis) and causes chest pain but rarely leads to death.
- It does not typically cause acute severe shortness of breath leading to death within three days in this context.
*Bacterial infection of the mitral valve endocardium*
- **Infective endocarditis** affects valve function and can cause heart failure, but it's typically a subacute process with systemic symptoms like fever.
- The presented acute timeline and image findings are not consistent with primary infective endocarditis as the cause of sudden death following acute chest pain.
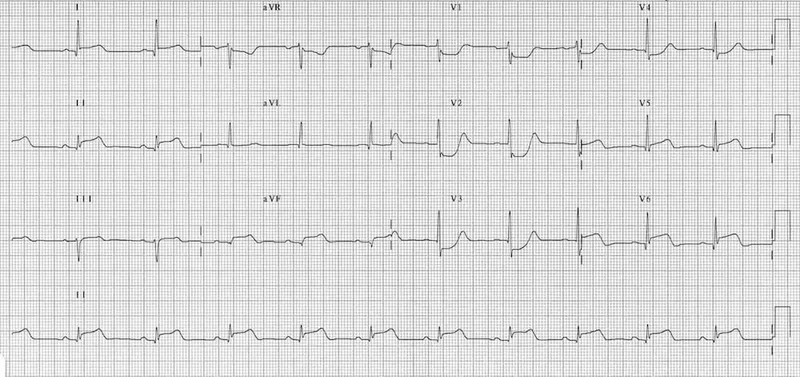
Ischemic heart disease US Medical PG Question 3: A 58-year-old man comes to the emergency department for complaints of crushing chest pain for 4 hours. He was shoveling snow outside when the pain started. It is rated 7/10 and radiates to his left arm. An electrocardiogram (ECG) demonstrates ST-segment elevation in leads V2-4. He subsequently undergoes percutaneous coronary intervention (PCI) and is discharged with aspirin, clopidogrel, carvedilol, atorvastatin, and lisinopril. Five days later, the patient is brought to the emergency department by his wife with complaints of dizziness. He reports lightheadedness and palpitations for the past 2 hours but otherwise feels fine. His temperature is 99.7°F (37.6°C), blood pressure is 95/55 mmHg, pulse is 105/min, and respirations are 17/min. A pulmonary artery catheter is performed and demonstrates an increase in oxygen concentration at the pulmonary artery. What finding would you expect in this patient?
- A. Widespread ST-segment elevations
- B. Harsh, loud, holosystolic murmur at the lower left sternal border (Correct Answer)
- C. Pulseless electrical activity
- D. Drop of systolic blood pressure by 20 mmHg during inspiration
- E. Normal findings
Ischemic heart disease Explanation: ***Harsh, loud, holosystolic murmur at the lower left sternal border***
- This patient's presentation, including recent **anterior STEMI**, dizziness, lightheadedness, palpitations, hypotension, tachycardia, and **increased oxygen saturation in the pulmonary artery** (oxygen "step-up" indicating a left-to-right shunt), is highly suggestive of **ventricular septal rupture (VSR)**.
- VSR is a **mechanical complication** of MI that typically occurs **3-7 days post-infarction** when the necrotic myocardium is weakest.
- A **VSR** causes a **harsh, loud, holosystolic murmur** best heard at the **lower left sternal border** due to turbulent blood flow through the septal defect from the left ventricle to the right ventricle.
- The left-to-right shunt results in oxygenated blood from the left ventricle mixing with deoxygenated blood in the right ventricle, causing the characteristic oxygen saturation step-up detected by pulmonary artery catheterization.
*Widespread ST-segment elevations*
- Widespread ST-segment elevations are characteristic of **acute pericarditis**, which typically presents with **pleuritic chest pain** that improves when leaning forward and a **friction rub**, not the hemodynamic compromise described here.
- While **Dressler syndrome** (post-MI pericarditis) can occur weeks after MI, the acute hemodynamic instability, left-to-right shunt evidence, and 5-day timeframe point to VSR rather than pericarditis.
*Pulseless electrical activity*
- **Pulseless electrical activity (PEA)** indicates cardiac arrest with organized electrical activity but no mechanical cardiac output, resulting in an **unpalpable pulse**.
- The patient has a documented pulse of **105/min**, which directly contradicts PEA.
- A patient in PEA would be unconscious and unable to report symptoms for 2 hours.
*Drop of systolic blood pressure by 20 mmHg during inspiration*
- A drop in systolic blood pressure >10 mmHg during inspiration (**pulsus paradoxus**) is characteristic of **cardiac tamponade** or severe obstructive airway disease.
- While **free wall rupture** leading to tamponade is another mechanical complication post-MI, the **oxygen saturation step-up** in the pulmonary artery is pathognomonic for an **intracardiac shunt** (VSR), not tamponade.
- Tamponade would show equalization of diastolic pressures across all chambers, not increased PA oxygen saturation.
*Normal findings*
- The patient presents with clear evidence of hemodynamic compromise: **hypotension (95/55 mmHg)**, **tachycardia (105/min)**, dizziness, and lightheadedness.
- The **oxygen saturation step-up** in the pulmonary artery is an objective abnormal finding indicating an intracardiac left-to-right shunt.
- Therefore, normal findings are incompatible with this clinical presentation.
Ischemic heart disease US Medical PG Question 4: A 78-year-old man with a history of myocardial infarction status post coronary artery bypass grafting and a 60-pack-year history of smoking is found deceased in his apartment after not returning calls to his family for the last 2 days. The man was last known to be alive 3 days ago, when his neighbor saw him getting his mail. The family requests an autopsy. On autopsy, the man is found to have a 100% blockage of his left anterior descending artery of his heart and likely passed from sudden cardiac death 2 days prior. Which of the following findings is expected to be found on histologic examination of his damaged myocardium?
- A. Fat saponification
- B. Cellular debris and lymphocytes
- C. Cystic cavitation
- D. Cellular debris and macrophages
- E. Uniform binding of acidophilic dyes (Correct Answer)
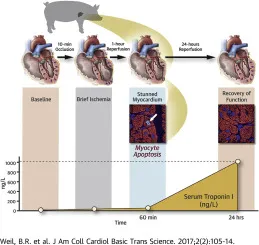
Ischemic heart disease Explanation: ***Uniform binding of acidophilic dyes***
- This finding, often described as **coagulative necrosis**, is characteristic of myocardial infarction 1-3 days after onset, as enzymes denature and bind to eosin more uniformly.
- The patient was found deceased 2 days after his suspected death, placing the myocardial changes within this timeframe.
*Fat saponification*
- **Fat saponification** is a type of fat necrosis, typically seen in the pancreas or breast, resulting from the enzymatic destruction of fat cells.
- It does not occur in the myocardium following an ischemic event.
*Cellular debris and lymphocytes*
- **Lymphocytes** are generally not the predominant inflammatory cells in the initial stages of a myocardial infarction.
- While cellular debris would be present, the primary inflammatory infiltrate in the first 3 days after an MI is typically **neutrophils**, not lymphocytes.
*Cystic cavitation*
- **Cystic cavitation** is a characteristic feature of liquefactive necrosis, which occurs in the brain following an ischemic stroke, but not in the heart.
- The heart undergoes **coagulative necrosis** after an MI.
*Cellular debris and macrophages*
- **Macrophages** become prominent later in the healing process of a myocardial infarction, typically starting around **3-7 days** after the event.
- At the 2-day mark, the dominant cells would still be neutrophils and necrotic myocytes.
Ischemic heart disease US Medical PG Question 5: A 57-year-old man presents to his primary care provider because of chest pain for the past 3 weeks. The chest pain occurs after climbing more than 2 flight of stairs or walking for more than 10 minutes and resolves with rest. He is obese, has a history of type 2 diabetes mellitus, and has smoked 15-20 cigarettes a day for the past 25 years. His father died from a myocardial infarction at 52 years of age. Vital signs reveal a temperature of 36.7 °C (98.06°F), a blood pressure of 145/93 mm Hg, and a heart rate of 85/min. The physical examination is unremarkable. Which of the following best represents the most likely etiology of the patient’s condition?
- A. Hypertrophy of the interventricular septum
- B. Multivessel atherosclerotic disease with or without a nonocclusive thrombus
- C. Intermittent coronary vasospasm with or without coronary atherosclerosis
- D. Fixed, atherosclerotic coronary stenosis (> 70%) (Correct Answer)
- E. Sudden disruption of an atheromatous plaque, with a resulting occlusive thrombus
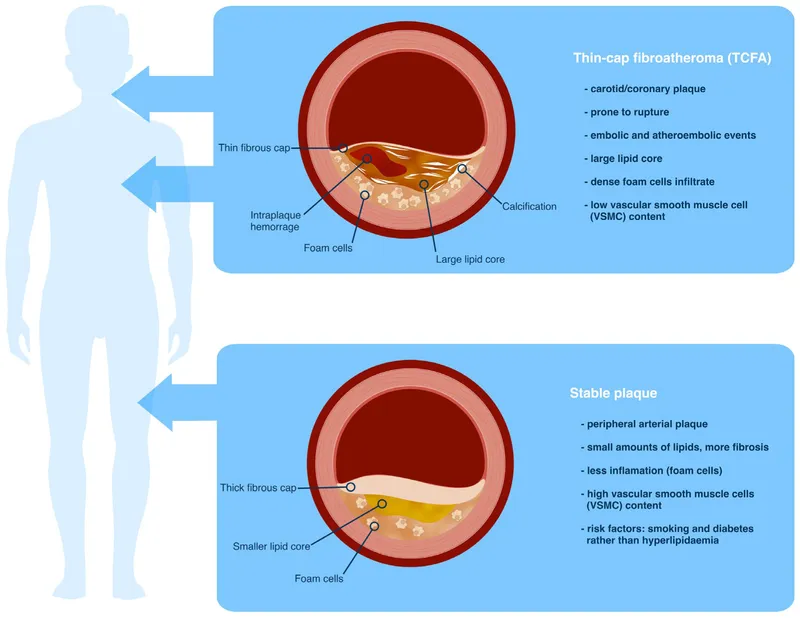
Ischemic heart disease Explanation: ***Fixed, atherosclerotic coronary stenosis (> 70%)***
- The patient's presentation with **exertional chest pain** that resolves with rest (stable angina), along with multiple **cardiovascular risk factors** (obesity, type 2 diabetes mellitus, smoking, family history of early MI, hypertension), strongly points towards **stable ischemic heart disease**.
- This clinical picture is typically caused by a **fixed, hemodynamically significant stenosis** in one or more coronary arteries, usually greater than 70%, that limits blood flow during increased demand.
*Multivessel atherosclerotic disease with or without a nonocclusive thrombus*
- While the patient likely has **multivessel atherosclerosis**, the phrase "with or without a nonocclusive thrombus" leans towards **unstable angina** or NSTEMI, which typically involves a sudden change in symptoms or rest angina.
- The patient's symptoms are **stable and reproducible** with exertion, resolving with rest, which is characteristic of stable angina rather than a thrombotic event.
*Sudden disruption of an atheromatous plaque, with a resulting occlusive thrombus*
- This mechanism describes an **acute coronary syndrome (ACS)**, such as an **ST-elevation myocardial infarction (STEMI)** or **non-ST-elevation myocardial infarction (NSTEMI)**.
- ACS typically presents with new-onset, worsening, or rest angina, which is different from the stable, exertional pattern described in the patient.
*Intermittent coronary vasospasm with or without coronary atherosclerosis*
- **Coronary vasospasm** (e.g., Prinzmetal angina) typically causes chest pain that occurs **at rest**, often at night or in the early morning, and is not necessarily related to exertion.
- While the patient could have underlying atherosclerosis, the **predictable exertional nature** of his symptoms makes vasospasm less likely as the primary etiology.
*Hypertrophy of the interventricular septum*
- **Interventricular septal hypertrophy** is characteristic of **hypertrophic cardiomyopathy (HCM)**, which can cause exertional chest pain due to outflow tract obstruction or myocardial ischemia.
- However, HCM is less likely to be the primary etiology in a 57-year-old with multiple classic **atherosclerotic risk factors** and no mention of a heart murmur or family history of HCM.
Ischemic heart disease US Medical PG Question 6: A 50-year-old man presents the emergency department for intense chest pain, profuse sweating, and shortness of breath. The onset of these symptoms was 3 hours ago. The chest pain began after a heated discussion with a colleague at the community college where he is employed. Upon arrival, he is found conscious and responsive; the vital signs include a blood pressure of 130/80 mm Hg, a heart rate at 90/min, a respiratory rate at 20/min, and a body temperature of 36.4°C (97.5°F). His medical history is significant for hypertension diagnosed 7 years ago, which is well-controlled with a calcium channel blocker. The initial electrocardiogram (ECG) shows ST-segment depression in multiple consecutive leads, an elevated cardiac troponin T level, and normal kidney function. Which of the following would you expect to find in this patient?
- A. Subendocardial necrosis (Correct Answer)
- B. Transmural necrosis
- C. Incomplete occlusion of a coronary artery
- D. Coronary artery spasm
- E. Ventricular pseudoaneurysm
Ischemic heart disease Explanation: ***Subendocardial necrosis***
- This patient's presentation with **ST-segment depression** and **elevated troponin T** indicates a **Non-ST-segment Elevation Myocardial Infarction (NSTEMI)**, which typically results from subendocardial ischemia and necrosis.
- Subendocardial tissue is most vulnerable to ischemia due to its high oxygen demand and distal location from the coronary arteries, making it the first region to suffer damage when oxygen supply is compromised.
*Transmural necrosis*
- **Transmural necrosis** is characteristic of a **ST-segment Elevation Myocardial Infarction (STEMI)**, which presents with persistent **ST-segment elevation** on ECG.
- This patient's ECG shows **ST-segment depression**, ruling out transmural involvement at the time of presentation.
*Incomplete occlusion of a coronary artery*
- While an NSTEMI usually involves an **incomplete occlusion** or **critical stenosis** of a coronary artery, the question asks what would be *found* in the patient's heart tissue, not the mechanism.
- The direct tissue consequence of incomplete occlusion leading to NSTEMI is **subendocardial necrosis**, which is a more specific answer about the pathological finding.
*Coronary artery spasm*
- Although **coronary artery spasm (Prinzmetal angina)** can cause chest pain and ECG changes, it typically presents with **transient ST-segment elevation** (not depression) and often resolves spontaneously.
- The elevated troponin T indicates myocardial necrosis, which is not typically a feature of uncomplicated coronary artery spasm, and the duration of symptoms (3 hours) suggests a more sustained event than a transient spasm.
*Ventricular pseudoaneurysm*
- A **ventricular pseudoaneurysm** is a **late complication of myocardial infarction**, typically occurring weeks to months after the acute event, due to rupture of the ventricular free wall contained by pericardium.
- Given the 3-hour symptom onset, it is highly unlikely to be present in the acute phase of myocardial infarction.
Ischemic heart disease US Medical PG Question 7: An 18-year-old man presents with a sudden loss of consciousness while playing college football. There was no history of a concussion. Echocardiography shows left ventricular hypertrophy and increased thickness of the interventricular septum. Which is the most likely pathology underlying the present condition?
- A. Autoimmunity of myocardial fibers
- B. Drug abuse
- C. Viral infection
- D. Mutation in the myosin heavy chain (Correct Answer)
- E. Streptococcal infection
Ischemic heart disease Explanation: ***Mutation in the myosin heavy chain***
- The presentation of **sudden loss of consciousness** (syncope) in a young athlete with **left ventricular hypertrophy** and **interventricular septal thickening** is classic for **hypertrophic cardiomyopathy (HCM)**.
- HCM is most commonly caused by **autosomal dominant mutations in genes** encoding sarcomeric proteins, with **beta-myosin heavy chain mutations** being the most frequent.
*Autoimmunity of myocardial fibers*
- Autoimmune conditions affecting the heart, such as **myocarditis** or **lupus carditis**, typically present with symptoms like **chest pain**, **dyspnea**, or signs of **heart failure**, which are not described here.
- While they can lead to cardiac dysfunction, they are less likely to cause isolated severe hypertrophy and sudden syncope in a young asymptomatic individual as the initial presentation.
*Drug abuse*
- **Stimulant drug abuse** (e.g., cocaine, amphetamines) can cause cardiomyopathy and arrhythmias, potentially leading to syncope.
- However, the specific echocardiographic findings of **marked septal hypertrophy** are not characteristic of drug-induced cardiomyopathy, which often manifests as **dilated cardiomyopathy** or global ventricular dysfunction.
*Viral infection*
- **Viral myocarditis** can cause cardiac inflammation, leading to **dilated cardiomyopathy** or arrhythmias, and can present with sudden cardiac death.
- While viral myocarditis can lead to some degree of hypertrophy, the prominent and isolated **asymmetric septal hypertrophy** and the chronic nature implied by the structural changes are less typical of acute or resolving viral infection.
*Streptococcal infection*
- **Rheumatic heart disease**, a sequela of **Streptococcus pyogenes infection**, primarily causes **valvular damage** (especially mitral stenosis or regurgitation) and less commonly diffuse myocardial involvement.
- It does not typically present with isolated severe **left ventricular hypertrophy** and **interventricular septal thickening** as the primary cardiac pathology leading to sudden syncope.
Ischemic heart disease US Medical PG Question 8: A 74-year-old man presents with complaints of sudden severe crushing retrosternal pain. The pain radiated to his left arm shortly after it began, and he was subsequently rushed to the emergency department for evaluation. His troponins and creatine kinase-MB (CK-MB) were elevated. Unfortunately, the patient died within the next 2 hours and an autopsy was performed immediately. The gross examination of the heart will show?
- A. White, patchy, non-contractile scar
- B. Normal heart tissue (Correct Answer)
- C. Pallor of the infarcted tissue
- D. Abundant neutrophils
- E. Red granulation tissue surrounding the infarction
Ischemic heart disease Explanation: ***Normal heart tissue***
- At **0-4 hours** following a myocardial infarction, the heart muscle shows **no gross changes** on autopsy examination.
- Although **coagulative necrosis** begins at the cellular level within minutes, these microscopic changes are **not visible** to the naked eye during gross examination.
- The patient died within **2 hours** of symptom onset, which falls within this early window where the heart appears **grossly normal** despite the acute infarction.
- Elevated **cardiac enzymes** (troponins, CK-MB) confirm myocardial injury has occurred, but gross pathological changes lag behind biochemical and microscopic changes.
*Pallor of the infarcted tissue*
- **Pallor** (pale discoloration) of infarcted myocardium typically becomes visible on gross examination at **4-12 hours** post-infarction.
- At 2 hours, this change has not yet developed sufficiently to be visible on gross inspection.
- Pallor results from **edema** and the accumulation of dead cells, which takes several hours to manifest grossly.
*White, patchy, non-contractile scar*
- A **white fibrotic scar** is characteristic of a **healed myocardial infarction**, which takes **several weeks to months** to form.
- This represents complete replacement of necrotic tissue by **collagenous scar tissue** (fibrosis).
- This is a chronic finding, not an acute one.
*Abundant neutrophils*
- **Neutrophil infiltration** is a microscopic finding that typically begins around **12-24 hours** after infarction, becoming abundant over the following days.
- Even when present, neutrophils are not visible on **gross examination**—they require microscopic evaluation.
- At 2 hours post-infarction, neutrophils have not yet migrated to the infarcted area.
*Red granulation tissue surrounding the infarction*
- **Granulation tissue** formation begins around **3-7 days** after infarction and involves proliferation of **capillaries** and **fibroblasts**.
- Grossly, this appears as a **hyperemic border** with central yellow softening.
- This represents the healing phase and would not be present within 2 hours of symptom onset.
Ischemic heart disease US Medical PG Question 9: A 49-year-old man with a past medical history of hypertension on amlodipine presents to your office to discuss ways to lessen his risk of complications from heart disease. After a long discussion, he decides to significantly decrease his intake of trans fats in an attempt to lower his risk of coronary artery disease. Which type of prevention is this patient initiating?
- A. Secondary prevention
- B. Delayed prevention
- C. Quaternary prevention
- D. Tertiary prevention
- E. Primary prevention (Correct Answer)
Ischemic heart disease Explanation: ***Primary prevention***
- This patient is initiating primary prevention by **modifying lifestyle choices** (decreasing trans fats) to **prevent the initial onset of coronary artery disease**, as he has a risk factor (hypertension) but no established heart disease.
- Primary prevention focuses on **preventing disease before it occurs** through health promotion and risk reduction.
*Secondary prevention*
- Secondary prevention involves **early detection and treatment of existing disease** to prevent progression or recurrence.
- Examples include **screening tests** like mammography or **medications for individuals already diagnosed** with a condition.
*Delayed prevention*
- This is **not a recognized category** of prevention in public health or medical practice.
- Prevention stages are typically classified as primary, secondary, tertiary, and sometimes quaternary.
*Quaternary prevention*
- Quaternary prevention aims to **protect patients from medical interventions** that may cause harm, such as over-medicalization or unnecessary procedures.
- It focuses on **reducing the burden of iatrogenic disease** and ensuring appropriate care.
*Tertiary prevention*
- Tertiary prevention focuses on **reducing the impact of an existing disease** or disability through rehabilitation and managing complications.
- It applies to patients who **already have an established disease** and seeks to improve their quality of life and functionality.
Ischemic heart disease US Medical PG Question 10: A 36-year-old healthy man presents to his physician to discuss his concerns about developing heart disease. His father, grandfather, and older brother had heart problems, and he has become increasingly worried he might be at risk. He takes no medications and his past medical history is only significant for an appendectomy at 20 years ago. He is married happily with 2 young children and works as a hotel manager and exercises occasionally in the hotel gym. He drinks 3–5 alcoholic beverages per week but denies smoking and illicit drug use. Today his blood pressure is 146/96 mm Hg, pulse rate is 80/min, and respiratory rate is 16/min. He has a body mass index of 26.8 kg/m2. His physical examination is otherwise unremarkable. Laboratory tests show:
Laboratory test
Serum glucose (fasting) 88 mg/dL
Serum electrolytes
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum creatinine 0.8 mg/dl
Blood urea nitrogen 10 mg/dl
Cholesterol, total 350 mg/dL
HDL-cholesterol 40 mg/dL
LDL-cholesterol 280 mg/dL
Triglycerides 130 mg/dL
Besides appropriate medications for his cholesterol and a follow-up for his hypertension, which of the following supplements is thought to provide a protective cardiovascular effect?
- A. Folic acid (Correct Answer)
- B. Thiamine
- C. Vitamin K
- D. Vitamin B12
- E. Vitamin E
Ischemic heart disease Explanation: ***Folic acid***
- Folic acid (Vitamin B9) is involved in the metabolism of **homocysteine**, and elevated homocysteine levels are associated with increased cardiovascular risk.
- **Historically**, it was hypothesized that lowering homocysteine with folic acid would reduce cardiovascular events.
- However, **large randomized controlled trials (HOPE-2, NORVIT, VISP) have failed to demonstrate cardiovascular benefit** from folic acid supplementation despite successfully lowering homocysteine levels.
- Among the options listed, folic acid was the supplement most **historically thought** to provide cardiovascular protection, though current evidence does not support routine supplementation for this purpose.
- **Current guidelines do NOT recommend** folic acid supplementation for cardiovascular disease prevention in the general population.
*Thiamine*
- **Thiamine** (Vitamin B1) is crucial for carbohydrate metabolism and nerve function.
- Thiamine deficiency can lead to **beriberi** (including wet beriberi with cardiac manifestations), but supplementation in individuals without deficiency provides **no cardiovascular protection**.
*Vitamin K*
- **Vitamin K** is essential for blood clotting and bone metabolism, and may play a role in preventing vascular calcification.
- However, there is **insufficient evidence** to recommend vitamin K supplementation for cardiovascular protection in clinical practice.
*Vitamin B12*
- **Vitamin B12** is important for nerve function, red blood cell formation, and homocysteine metabolism.
- Like folic acid, B12 was studied for cardiovascular protection through homocysteine reduction, but **clinical trials failed to show benefit**.
- Routine B12 supplementation for cardiovascular protection in individuals with normal B12 levels is **not recommended**.
*Vitamin E*
- **Vitamin E** is an antioxidant that was extensively studied for cardiovascular protection in the 1990s-2000s.
- **Large clinical trials (HOPE, GISSI) conclusively showed NO cardiovascular benefit** from vitamin E supplementation, and some studies suggested potential harm at high doses.
- Vitamin E supplementation for cardiovascular disease prevention is **not recommended**.
More Ischemic heart disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.