Infective endocarditis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Infective endocarditis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Infective endocarditis US Medical PG Question 1: A 27-year-old man who recently emigrated as a refugee from Somalia presents with fever, weight loss, fatigue, and exertional chest pain. He says his symptoms began 3 weeks ago and that his appetite has decreased and he has lost 3 kg (6.6 lb) in the last 3 weeks. He denies any history of cardiac disease. His past medical history is unremarkable. The patient admits that he has always lived in poor hygienic conditions in overcrowded quarters and in close contact with cats. His vital signs include: blood pressure 120/60 mm Hg, pulse 90/min, and temperature 38.0°C (100.4°F). Physical examination reveals generalized pallor. A cardiac examination reveals an early diastolic murmur loudest at the left third intercostal space. Abdominal examination reveals a tender and mildly enlarged spleen. Prominent axillary lymphadenopathy is noted. Laboratory investigations reveal a WBC count of 14,500/μL with 5% bands and 93% polymorphonuclear cells. An echocardiogram reveals a 5-mm vegetation on the aortic valve with moderate regurgitation. Three sets of blood cultures are taken over 24 hours followed by empiric antibiotic therapy with gentamicin and vancomycin. The blood cultures show no growth after 5 days. Following a week of empiric therapy, the patient continues to deteriorate. Which of the following would most likely confirm the diagnosis in this patient?
- A. Epstein-Barr virus heterophile antibody
- B. Peripheral blood smear
- C. Q fever serology
- D. Bartonella serology (Correct Answer)
- E. HIV polymerase chain reaction
Infective endocarditis Explanation: **Bartonella serology**
- The patient's history of **poor hygiene**, **cat exposure**, culture-negative endocarditis with **aortic valve vegetation**, and **axillary lymphadenopathy** are highly suggestive of **Bartonella endocarditis**.
- **Bartonella henselae**, the causative agent of **cat scratch disease**, can cause indolent, culture-negative endocarditis, and serology is a key diagnostic tool.
*Epstein-Barr virus heterophile antibody*
- This test is primarily used to diagnose **infectious mononucleosis**, which typically presents with **pharyngitis, lymphadenopathy**, and **fatigue**.
- While fatigue and lymphadenopathy are present, the patient's **fever, weight loss, exertional chest pain**, and **endocarditis** are not typical features of mononucleosis.
*Peripheral blood smear*
- A peripheral blood smear is used to identify **hematological abnormalities** like **anemia, leukemia**, or **parasitic infections** (e.g., malaria).
- While **generalized pallor** suggests anemia, it would not directly confirm the cause of the **culture-negative endocarditis** or explain the specific constellation of symptoms.
*Q fever serology*
- **Q fever**, caused by **Coxiella burnetii**, can cause **culture-negative endocarditis**, particularly in patients with pre-existing valvular disease.
- However, the strong history of **cat exposure** and **axillary lymphadenopathy** in this case makes **Bartonella** a more probable diagnosis given the available information.
*HIV polymerase chain reaction*
- **HIV infection** can lead to various opportunistic infections and systemic symptoms like **weight loss, fever**, and **lymphadenopathy**.
- While HIV can predispose to endocarditis, the specific clinical picture with **cat exposure** and **culture-negative endocarditis** points more directly to **Bartonella infection** rather than primary HIV as the cause of the endocarditis.
Infective endocarditis US Medical PG Question 2: A 24-year-old male is brought into the emergency department complaining of chills, headaches, and malaise for several days. He also states that he experiences shortness of breath when climbing two flights of stairs in his home. He admits to occasionally using intravenous drugs during the previous year. On exam, his vital signs are temperature 39.2° C, heart rate 108/min, blood pressure 124/82 mm Hg, respiratory rate 20/min, and oxygen saturation 98% on room air. A holosystolic murmur is heard near the lower left sternal border. An echocardiogram confirms vegetations on the tricuspid valve. What is the most likely causative organism of this patient's condition?
- A. Candida albicans
- B. Staphylococcus aureus (Correct Answer)
- C. Streptococcus mutans
- D. Staphylococcus epidermidis
- E. Streptococcus bovis
Infective endocarditis Explanation: ***Staphylococcus aureus***
- This patient's history of **intravenous drug use** and the finding of **tricuspid valve vegetations** are highly characteristic of **infectious endocarditis** caused by *Staphylococcus aureus.*
- *S. aureus* is the most common pathogen in IV drug users due to its prevalence on the skin and ability to adhere to and colonize damaged heart valves.
*Candida albicans*
- While *Candida albicans* can cause endocarditis, especially in immunocompromised individuals or those with central venous catheters, it is **less common** than *S. aureus* in IV drug users and does not typically present with the same high frequency.
- Fungal endocarditis often has a more **subacute course** and can be associated with larger vegetations.
*Streptococcus mutans*
- *Streptococcus mutans* is a common cause of **dental caries** and is associated with infective endocarditis, particularly in patients with pre-existing valvular heart disease and poor dental hygiene, affecting the **mitral or aortic valves**.
- It is **not typically associated** with endocarditis in intravenous drug users.
*Staphylococcus epidermidis*
- *Staphylococcus epidermidis* is a common cause of **prosthetic valve endocarditis** but is less frequently involved in native valve endocarditis, especially in IV drug users, compared to *S. aureus*.
- It is a **coagulase-negative staphylococcus** and a common skin commensal.
*Streptococcus bovis*
- *Streptococcus bovis* (now *Streptococcus gallolyticus*) endocarditis is strongly associated with **colorectal cancer** or other gastrointestinal pathologies.
- This patient has no features suggestive of gastrointestinal disease, making *S. bovis* an **unlikely causative agent**.
Infective endocarditis US Medical PG Question 3: A 37-year-old man presents to the emergency department for a persistent fever. The patient states he has felt unwell for the past week and has felt subjectively febrile. The patient has a past medical history of a suicide attempt and alcohol abuse. He is not currently taking any medications. The patient admits to using heroin and cocaine and drinking 5-8 alcoholic drinks per day. His temperature is 103°F (39.4°C), blood pressure is 92/59 mmHg, pulse is 110/min, respirations are 20/min, and oxygen saturation is 96% on room air. Cardiopulmonary exam is notable for a systolic murmur heard best along the left sternal border. Dermatologic exam reveals scarring in the antecubital fossa. Which of the following is the next best step in management?
- A. CT scan
- B. Ultrasound
- C. Chest radiograph
- D. Blood cultures (Correct Answer)
- E. Vancomycin and gentamicin
Infective endocarditis Explanation: ***Blood cultures***
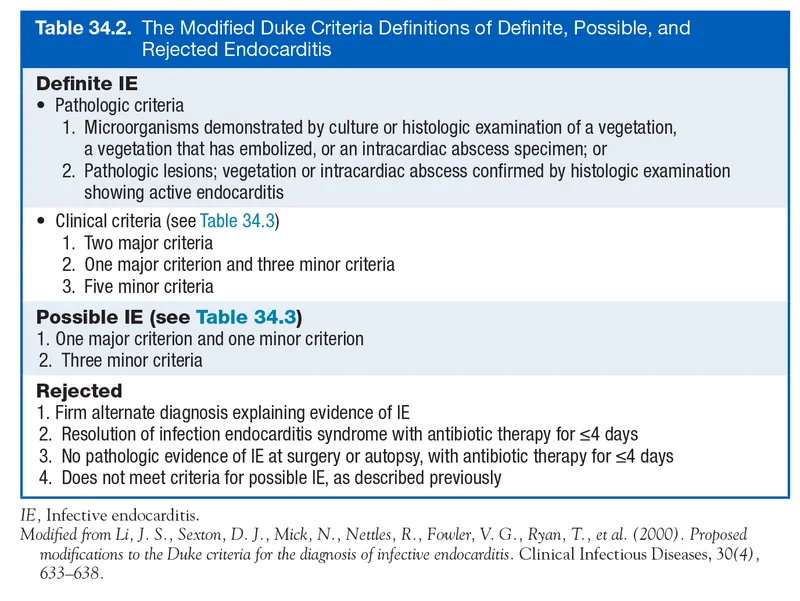
- The patient's history of **intravenous drug use (IVDU)**, persistent fever, and a **new systolic murmur** strongly suggest **infective endocarditis**.
- **Blood cultures** are crucial for identifying the causative organism and guiding appropriate antibiotic therapy, serving as the cornerstone of diagnosis in suspected endocarditis.
*CT scan*
- While CT scans can be useful for identifying complications of endocarditis (e.g., septic emboli in the brain or lungs), they are **not the initial diagnostic step** for identifying the source of infection.
- CT scans expose the patient to **radiation** and are more expensive, making them less suitable as a first step compared to blood cultures.
*Ultrasound*
- An **echocardiogram** (a type of ultrasound) is essential for visualizing vegetations on heart valves, but it is typically performed *after* blood cultures reveal bacteremia to confirm the diagnosis and assess severity.
- A general ultrasound of other body areas would be non-specific and **unlikely to pinpoint the cause** of persistent fever in this clinical context.
*Chest radiograph*
- A chest radiograph can identify **pulmonary infiltrates** or **septic emboli in the lungs**, which are potential complications of right-sided endocarditis (common in IVDU).
- However, a chest radiograph **does not identify the causative organism** or confirm the primary diagnosis of endocarditis, making it a secondary investigation.
*Vancomycin and gentamicin*
- This combination represents a broad-spectrum antibiotic regimen often used for **empiric treatment of infective endocarditis**, particularly in IVDU patients due to concerns for MRSA or resistant streptococcal species.
- While ultimately necessary, administering antibiotics *before* obtaining **blood cultures** can significantly reduce the yield of cultures and hinder definitive diagnosis and tailored treatment.
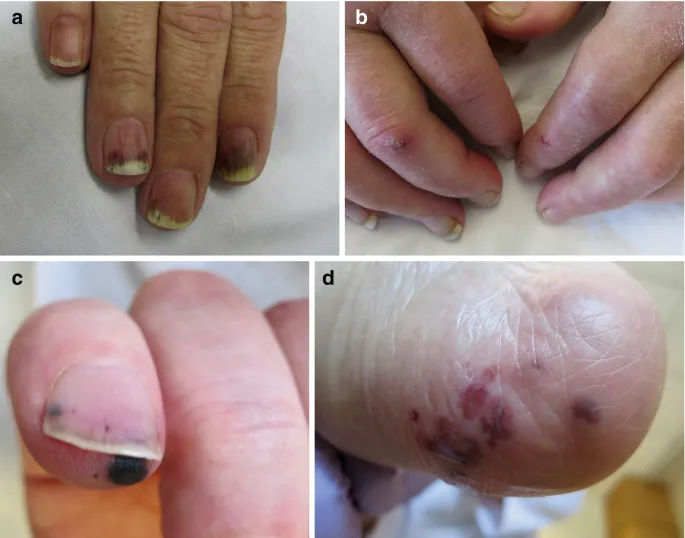
Infective endocarditis US Medical PG Question 4: A 24-year-old man presents with low-grade fever and shortness of breath for the last 3 weeks. Past medical history is significant for severe mitral regurgitation status post mitral valve replacement five years ago. His temperature is 38.3°C (101.0°F) and respiratory rate is 18/min. Physical examination reveals vertical hemorrhages under his nails, multiple painless erythematous lesions on his palms, and two tender, raised nodules on his fingers. Cardiac auscultation reveals a new-onset 2/6 holosystolic murmur loudest at the apex with the patient in the left lateral decubitus position. A transesophageal echocardiogram reveals vegetations on the prosthetic valve. Blood cultures reveal catalase-positive, gram-positive cocci. Which of the following characteristics is associated with the organism most likely responsible for this patient’s condition?
- A. Coagulase positive
- B. DNAse positive
- C. Hemolysis
- D. Novobiocin sensitive (Correct Answer)
- E. Optochin sensitive
Infective endocarditis Explanation: ***Novobiocin sensitive***
- The patient has **prosthetic valve endocarditis** caused by a **catalase-positive, gram-positive coccus**, which is most likely **_Staphylococcus epidermidis_** due to its association with foreign bodies and prosthetic devices.
- _Staphylococcus epidermidis_ is a **coagulase-negative staphylococcus** that is **novobiocin sensitive**, helping to differentiate it from other coagulase-negative staphylococci like **_Staphylococcus saprophyticus_** (novobiocin resistant).
- Although this is late prosthetic valve endocarditis (5 years post-surgery), _S. epidermidis_ remains a common pathogen due to biofilm formation on prosthetic materials.
*Coagulase positive*
- **Coagulase-positive** gram-positive cocci, such as **_Staphylococcus aureus_**, are a common cause of endocarditis, especially in intravenous drug users and can also cause prosthetic valve endocarditis.
- However, the correct answer requires identifying the characteristic that differentiates the most likely organism, and **coagulase-negative** staphylococci like _S. epidermidis_ are more characteristically associated with prosthetic device infections due to their biofilm-forming capabilities.
- A positive coagulase test differentiates _S. aureus_ from coagulase-negative staphylococci.
*DNAse positive*
- **DNAse positivity** is characteristic of **_Staphylococcus aureus_** and group A beta-hemolytic streptococci (_Streptococcus pyogenes_).
- While _S. aureus_ can cause prosthetic valve endocarditis, the question asks for the characteristic most associated with the likely organism, which in the context of prosthetic devices is typically **_S. epidermidis_** (DNAse negative).
*Hemolysis*
- **Hemolysis patterns** are primarily used to differentiate **streptococcal species**, not staphylococci. For example, **beta-hemolytic streptococci** cause complete hemolysis.
- While some staphylococci can show hemolytic activity, it is not a primary characteristic used to differentiate between the most likely staphylococcal causes of prosthetic valve endocarditis.
*Optochin sensitive*
- **Optochin sensitivity** is a key characteristic used to identify **_Streptococcus pneumoniae_**.
- _S. pneumoniae_ is **catalase-negative**, while the described organism is **catalase-positive**, ruling out _S. pneumoniae_ as the causative agent.
Infective endocarditis US Medical PG Question 5: A 38-year-old female presents to the emergency room with fevers, fatigue, and anorexia for over a month. Past medical history includes mild mitral valve prolapse. She underwent an uncomplicated tooth extraction approximately 6 weeks ago. Her vital signs include a temperature of 100.8 F, pulse of 83, blood pressure of 110/77, and SpO2 of 97% on room air. On exam, you note a grade III/VI holosystolic murmur at the apex radiating to the axilla as well as several red, painful nodules on her fingers. Which of the following is the next best course of action?
- A. Blood cultures are not needed. Start empiric antibiotics
- B. Start anticoagulation with heparin
- C. Consult cardiothoracic surgery for mitral valve replacement
- D. Obtain blood cultures x3 sites over 24 hours and start antibiotics after culture results are available
- E. Obtain blood cultures x3 sites over 1 hour and start empiric antibiotics (Correct Answer)
Infective endocarditis Explanation: ***Obtain blood cultures x3 sites over 1 hour and start empiric antibiotics***
- The patient's presentation with **fever, fatigue, anorexia, new murmur, and painful finger nodules (Osler's nodes)** after a recent dental procedure strongly suggests **infective endocarditis**. Prompt initiation of **empiric antibiotics** after obtaining adequate blood cultures is crucial to improve outcomes and prevent further complications like septic emboli or valvular damage.
- Obtaining **multiple blood cultures rapidly (e.g., three sets over 1 hour)** from different sites maximizes the chance of isolating the causative organism before antibiotics are given, enabling targeted therapy later, while minimizing delay to treatment.
*Blood cultures are not needed. Start empiric antibiotics*
- **Blood cultures are essential** for diagnosing infective endocarditis, identifying the causative organism, and guiding appropriate antibiotic therapy. Skipping blood cultures could lead to inappropriate antibiotic selection and treatment failure.
- While empiric antibiotics are warranted, they should always be initiated **after blood cultures** have been drawn to avoid sterilizing the blood and making microbial identification difficult.
*Start anticoagulation with heparin*
- **Anticoagulation is generally contraindicated** in infective endocarditis due to the increased risk of hemorrhagic complications, especially in cases of septic emboli to the brain.
- While patients with endocarditis can form vegetations that may embolize, the risks of **bleeding outweigh the benefits** of routine anticoagulation.
*Consult cardiothoracic surgery for mitral valve replacement*
- While **mitral valve prolapse** is a risk factor for endocarditis and severe valvular damage may eventually require surgery, primary management involves **antibiotic therapy**.
- Surgical intervention is typically reserved for cases with **severe valvular regurgitation/stenosis leading to heart failure**, uncontrolled infection despite antibiotics, or recurrent emboli, and is not the immediate next step.
*Obtain blood cultures x3 sites over 24 hours and start antibiotics after culture results are available*
- Waiting for **24 hours to collect blood cultures** would significantly delay the initiation of antibiotics, which is dangerous in a potentially life-threatening infection like endocarditis.
- Delaying antibiotics until **culture results are available** could take several days, leading to worsening infection, organ damage, and increased mortality. **Empiric antibiotics** must be started promptly after initial blood collection.
Infective endocarditis US Medical PG Question 6: Blood cultures are sent to the laboratory. Intravenous antibiotic therapy is started. Transesophageal echocardiography shows a large, oscillating vegetation attached to the tricuspid valve. There are multiple small vegetations attached to tips of the tricuspid valve leaflets. There is moderate tricuspid regurgitation. The left side of the heart and the ejection fraction are normal. Which of the following is the most likely causal organism of this patient's condition?
- A. Streptococcus sanguinis
- B. Staphylococcus aureus (Correct Answer)
- C. Enterococcus faecalis
- D. Neisseria gonorrhoeae
- E. Staphylococcus epidermidis
Infective endocarditis Explanation: ***Staphylococcus aureus***
- **_Staphylococcus aureus_** is the most common cause of **acute infective endocarditis**, particularly in intravenous drug users, which often affects the **tricuspid valve**.
- The presence of large, oscillating vegetations and **multiple small vegetations** on the tricuspid valve strongly suggests an aggressive infection, typical of _S. aureus_.
*Streptococcus sanguinis*
- _Streptococcus sanguinis_ is a common cause of **subacute infective endocarditis** in patients with pre-existing valvular disease but rarely causes acute, aggressive right-sided endocarditis.
- It's typically associated with **dental procedures** and usually affects the left side of the heart.
*Enterococcus faecalis*
- _Enterococcus faecalis_ can cause endocarditis, often associated with **genitourinary or gastrointestinal procedures**, and typically affects older men.
- While it can cause virulent endocarditis, it is less commonly associated with acute right-sided disease in this demographic compared to _S. aureus_.
*Neisseria gonorrhoeae*
- **_Neisseria gonorrhoeae_** is a rare cause of endocarditis, usually seen in younger, sexually active individuals, and often involves the aortic valve.
- While it can be acute, it is an extremely uncommon cause of **tricuspid valve endocarditis**.
*Staphylococcus epidermidis*
- **_Staphylococcus epidermidis_** is primarily associated with **prosthetic valve endocarditis** or foreign bodies, often presenting as a subacute infection.
- It rarely causes natural valve endocarditis, especially acute right-sided disease in this context.
Infective endocarditis US Medical PG Question 7: A 27-year-old man presents to the emergency department with weakness and a fever for the past week. The patient is homeless and has a past medical history of alcohol and IV drug abuse. His temperature is 102°F (38.9°C), blood pressure is 107/68 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a tremulous patient with antecubital scars and a murmur over the left lower sternal border. Blood cultures are drawn and the patient is started on vancomycin and ceftriaxone and is admitted to the ICU. The patient's fever and symptoms do not improve despite antibiotic therapy for which the initial identified organism is susceptible. Cultures currently reveal MRSA as one of the infective organisms. Which of the following is the best next step in management?
- A. Transesophageal echocardiography (Correct Answer)
- B. Obtain new blood cultures
- C. CT scan of the chest
- D. Nafcillin and piperacillin-tazobactam
- E. Vancomycin and gentamicin
Infective endocarditis Explanation: ***Transesophageal echocardiography***
- The patient's history of **IV drug abuse**, **fever**, **new murmur**, and identification of **MRSA** strongly suggest **infective endocarditis**.
- A Transesophageal echocardiography (TEE) is the **most sensitive and specific imaging modality** to detect vegetations, abscesses, or valvular damage, which is crucial for guiding further management.
*Obtain new blood cultures*
- While repeating blood cultures can be useful to confirm eradication or identify new pathogens, the initial blood cultures already revealed MRSA, which is a common cause of **endocarditis in IV drug users**.
- The immediate priority given the lack of improvement and high suspicion of endocarditis is to visualize the heart valves for vegetations.
*CT scan of the chest*
- A CT scan of the chest would be useful to look for complications such as **septic emboli in the lungs** or other pulmonary pathologies.
- However, it would not provide the detailed visualization of heart valves necessary to diagnose or rule out valvular vegetations characteristic of endocarditis.
*Nafcillin and piperacillin-tazobactam*
- **Nafcillin** is active against **methicillin-susceptible Staphylococcus aureus (MSSA)**, but the patient's cultures already identified **MRSA**.
- **Piperacillin-tazobactam** is a broad-spectrum antibiotic but not a first-line treatment for MRSA infections and would not be appropriate given the identified pathogen.
*Vancomycin and gentamicin*
- The patient is already on **Vancomycin**, which is appropriate for MRSA, but adding **gentamicin** without clear indication would not be the best next step.
- While gentamicin is sometimes used as an adjunct in specific endocarditis regimens (e.g., enterococcal), the primary concern here is the lack of clinical improvement despite appropriate MRSA coverage, pointing towards a structural cardiac issue.
Infective endocarditis US Medical PG Question 8: A 51-year-old man comes to the physician for 2 months of intermittent low-grade fever, malaise, and joint pain. He has a history of recurrent dental abscesses requiring drainage but has otherwise been healthy. His temperature is 38.3°C (100.9°F) and pulse is 112/min. Physical examination shows a new holosystolic murmur in the left midclavicular line that radiates to the axilla. There are linear reddish-brown lesions underneath the nail beds and tender violaceous nodules on the bilateral thenar eminences. Two sets of blood cultures grow Streptococcus mutans. A transthoracic echocardiogram shows moderate regurgitation of the mitral valve. Which of the following mechanisms is most likely directly involved in the pathogenesis of this patient's valvular condition?
- A. Coagulative necrosis
- B. Leaflet calcification and fibrosis
- C. Antibody cross-reaction
- D. Fibrin clot formation (Correct Answer)
- E. Sterile platelet thrombi deposition
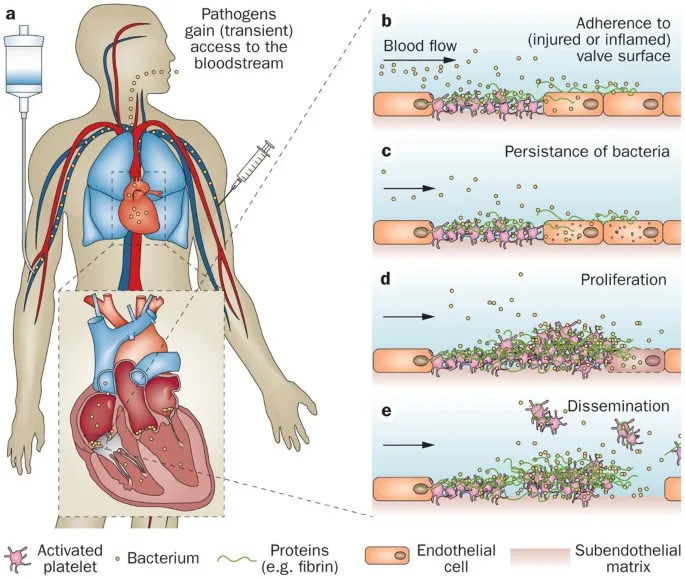
Infective endocarditis Explanation: ***Fibrin clot formation***
- This patient has **infective endocarditis**, characterized by **vegetations** on the heart valves. These vegetations are composed of platelets, fibrin, microorganisms, and inflammatory cells.
- The formation of these vegetations involves the deposition of **fibrin and platelets** on damaged endothelial surfaces, which then become a nidus for bacterial colonization, specifically *Streptococcus mutans* in this case.
*Coagulative necrosis*
- **Coagulative necrosis** is a type of cell death typically seen in ischemic conditions (e.g., myocardial infarction, renal infarcts) where the cell architecture is preserved for a period.
- It is not the primary mechanism for valvular damage and vegetation formation in **infective endocarditis**.
*Leaflet calcification and fibrosis*
- **Calcification and fibrosis** of valve leaflets are characteristic features of chronic degenerative valvular diseases, such as **aortic stenosis** in older age or chronic rheumatic heart disease.
- While chronic inflammation can lead to fibrosis, the acute pathophysiology of infective endocarditis is dominated by vegetation formation and destruction rather than primary calcification.
*Antibody cross-reaction*
- **Antibody cross-reaction** is the mechanism responsible for **rheumatic fever**, where antibodies against streptococcal M proteins cross-react with cardiac tissue antigens (molecular mimicry), leading to valvular damage.
- Although *Streptococcus* is involved, the signs and symptoms (new murmur, fever, splinter hemorrhages, Osler nodes, and positive blood cultures) are classic for **infective endocarditis**, not acute rheumatic fever.
*Sterile platelet thrombi deposition*
- **Sterile platelet thrombi deposition** occurs in **nonbacterial thrombotic endocarditis (NBTE)**, also known as marantic endocarditis, often associated with hypercoagulable states or malignancy.
- While it involves platelet deposition, the key difference here is the presence of **positive blood cultures** with *Streptococcus mutans*, indicating an active infection, not a sterile process.
Infective endocarditis US Medical PG Question 9: A 61-year-old man with a history of stage IIIa lung adenocarcinoma that has been treated with wedge resection and chemotherapy presents to the primary care clinic. He is largely asymptomatic, but he demonstrates a persistent microcytic anemia despite iron supplementation. Colonoscopy performed 3 years earlier was unremarkable. His past medical history is significant for diabetes mellitus type II, hypertension, acute lymphoblastic leukemia as a child, and hypercholesterolemia. He currently smokes 1 pack of cigarettes per day, drinks a glass of pinot grigio per day, and currently denies any illicit drug use. His vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 126/74 mm Hg; heart rate, 87/min; and respiratory rate, 17/min. On physical examination, his pulses are bounding, complexion is pale, but breath sounds remain clear. Oxygen saturation was initially 91% on room air, with a new oxygen requirement of 2 L by nasal cannula. Which of the following lab values would suggest anemia of chronic disease as the underlying etiology?
- A. Decreased serum iron and transferrin, decreased ferritin, normal serum transferrin receptor
- B. Increased serum iron and transferrin, increased ferritin, normal serum transferrin receptor
- C. Decreased serum iron, increased transferrin, decreased ferritin, increased serum transferrin receptor
- D. Decreased serum iron and transferrin, increased ferritin, normal serum transferrin receptor (Correct Answer)
- E. Decreased serum iron, decreased transferrin, increased ferritin, increased serum transferrin receptor
Infective endocarditis Explanation: ***Decreased serum iron and transferrin, increased ferritin, normal serum transferrin receptor***
- In **anemia of chronic disease (ACD)**, inflammation leads to increased **hepcidin** levels, which blocks iron release from stores and reduces iron absorption, resulting in **decreased serum iron and transferrin** (which reflects transferrin saturation).
- The inflammatory state also causes **ferritin** (an acute phase reactant and iron storage protein) to be **increased** or normal, as iron is sequestered. **Serum transferrin receptor** levels are typically normal, differentiating it from iron deficiency anemia.
*Decreased serum iron and transferrin, decreased ferritin, normal serum transferrin receptor*
- This pattern, particularly the **decreased ferritin**, is more indicative of **iron deficiency anemia**, where the body's iron stores are depleted.
- In iron deficiency, the body attempts to increase iron absorption and mobilization, thus ferritin would be low.
*Increased serum iron and transferrin, increased ferritin, normal serum transferrin receptor*
- This combination is not typical for any common anemia. **Increased serum iron and transferrin** might suggest iron overload conditions, but not iron-restricted erythropoiesis.
- While ferritin can be increased in chronic disease, the increased serum iron and transferrin are contradictory to ACD.
*Decreased serum iron, increased transferrin, decreased ferritin, increased serum transferrin receptor*
- This constellation, especially the **increased transferrin** and **decreased ferritin**, is characteristic of **iron deficiency anemia**.
- **Increased serum transferrin receptor** is a hallmark of iron deficiency, as cells upregulate receptors to capture more iron when deficient.
*Decreased serum iron, decreased transferrin, increased ferritin, increased serum transferrin receptor*
- While **decreased serum iron, decreased transferrin** (low transferrin saturation), and **increased ferritin** can be seen in ACD, the presence of an **increased serum transferrin receptor** is inconsistent.
- An increased serum transferrin receptor is usually a marker for increased erythropoietic activity or iron deficiency, which is not the primary mechanism of ACD.
Infective endocarditis US Medical PG Question 10: A 14-year-old Caucasian female with a family history of familial hypercholesterolemia commits suicide by drug overdose. Her family decides to donate her organs, and her heart is removed for donation. After removing the heart, the cardiothoracic surgeon notices flat yellow spots on the inside of her aorta. Which of the following cell types predominate in these yellow spots?
- A. Fibroblasts
- B. T-cells
- C. Macrophages (Correct Answer)
- D. Neutrophils
- E. Endothelium
Infective endocarditis Explanation: ***Correct: Macrophages***
- The "flat yellow spots" on the aorta in a familial hypercholesterolemia patient are characteristic of **fatty streaks**, the earliest lesions of atherosclerosis.
- These fatty streaks are primarily composed of **lipid-laden macrophages**, also known as **foam cells**, which have ingested oxidized low-density lipoprotein (LDL).
- In familial hypercholesterolemia, elevated LDL levels accelerate the formation of these macrophage-rich lesions even in young patients.
*Incorrect: Fibroblasts*
- While fibroblasts are involved in the later stages of **atherosclerotic plaque formation** by synthesizing collagen and forming a fibrous cap, they are not the predominant cell type in early fatty streaks.
- Their presence signifies a more advanced, **fibrotic lesion**, not the initial yellow spots.
*Incorrect: T-cells*
- T-cells are involved in the inflammatory response in **atherosclerosis** and are found within plaques, but they are not the dominant cell type forming the bulk of the initial lipid accumulation in fatty streaks.
- They contribute to the **immune-mediated aspects** of plaque progression.
*Incorrect: Neutrophils*
- Neutrophils are primarily involved in **acute inflammation** and bacterial infections.
- They are generally not a prominent cell type in either early or advanced **atherosclerotic lesions** under normal circumstances.
*Incorrect: Endothelium*
- Endothelial cells line the lumen of blood vessels and are crucial in the **initiation of atherosclerosis** by becoming dysfunctional and allowing LDL entry.
- However, they do not constitute the "yellow spots" themselves, which are subendothelial accumulations of lipids and immune cells.
More Infective endocarditis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.