Hypertensive heart disease US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hypertensive heart disease. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hypertensive heart disease US Medical PG Question 1: A 53-year-old woman visits her physician with complaints of shortness of breath and fatigue over the last few weeks. Her past medical history includes hypertension diagnosed 20 years ago. She takes hydrochlorothiazide and losartan daily. Her mother died at the age of 54 from a stroke, and both of her grandparents suffered from cardiovascular disease. She has a 13 pack-year history of smoking and drinks alcohol occasionally. Her blood pressure is 150/120 mm Hg, pulse is 95/min, respiratory rate is 22/min, and temperature is 36.7°C (98.1°F). On physical examination, she has bibasilar rales, distended jugular veins, and pitting edema in both lower extremities. Her pulse is irregularly irregular and her apical pulse is displaced laterally. Fundoscopy reveals ‘copper wiring’ and ‘cotton wool spots’. Which of the following echocardiographic findings will most likely be found in this patient?
- A. Ejection fraction: 55% with dilated chambers and thin walls
- B. Ejection fraction: 60% with normal left ventricular wall thickness
- C. Ejection fraction: 65% with rapid early diastolic filling and slow late diastolic filling
- D. Ejection fraction: 40% with increased left ventricular wall thickness (Correct Answer)
- E. Ejection fraction: 80% with regurgitant aortic valve
Hypertensive heart disease Explanation: ***Ejection fraction: 40% with increased left ventricular wall thickness***
- This patient presents with **chronic, poorly controlled hypertension** (20-year history, BP 150/120, hypertensive retinopathy with copper wiring and cotton wool spots) leading to **decompensated heart failure**.
- Clinical signs of heart failure include **shortness of breath, fatigue, bibasilar rales, jugular venous distension, and bilateral pitting edema**.
- The **irregularly irregular pulse suggests atrial fibrillation**, a common complication of hypertensive heart disease and left atrial enlargement.
- The **laterally displaced apical pulse** indicates left ventricular enlargement, and combined with **reduced ejection fraction (40%)** confirms **heart failure with reduced ejection fraction (HFrEF)**.
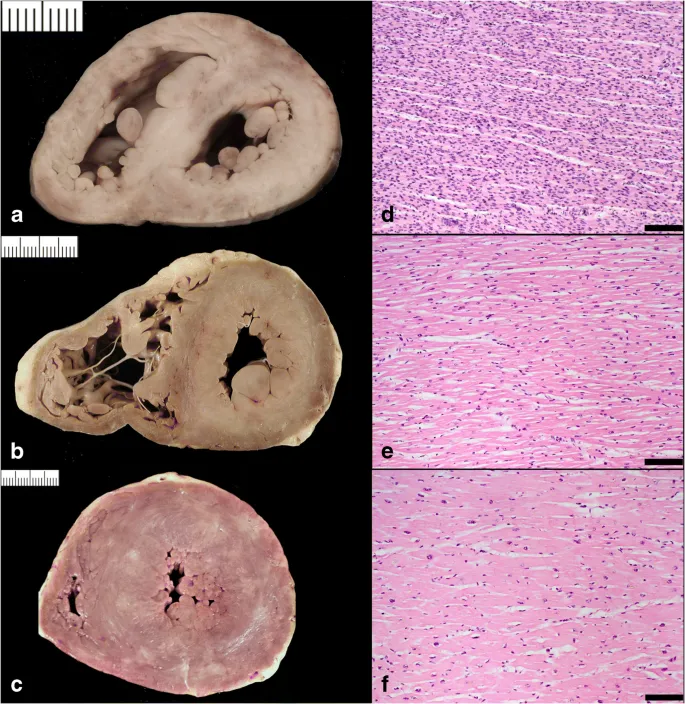
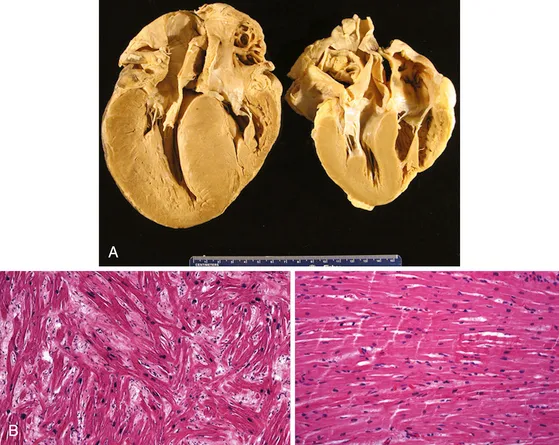
- In **advanced hypertensive heart disease**, the ventricle may show **mixed/eccentric hypertrophy** with both **increased wall thickness** (from chronic pressure overload) and **chamber dilatation** (from decompensation), resulting in reduced systolic function.
- This represents **stage D hypertensive heart disease** with progression from concentric LVH to eccentric remodeling with systolic dysfunction.
*Ejection fraction: 55% with dilated chambers and thin walls*
- An EF of 55% is **borderline normal/preserved** and would be inconsistent with the **severely reduced systolic function** suggested by the clinical presentation of decompensated heart failure.
- **Dilated chambers with thin walls** is the classic pattern of **non-ischemic dilated cardiomyopathy**, which typically presents with **EF <40%**, not 55%.
- While this patient may have some chamber dilatation, the combination of long-standing hypertension with preserved/increased wall thickness makes this less likely than hypertensive heart disease.
*Ejection fraction: 60% with normal left ventricular wall thickness*
- An EF of 60% is **normal** and **normal LV wall thickness** would not explain the clinical picture.
- This finding would be incompatible with the **severe decompensated heart failure** evident from bibasilar rales, JVD, and pitting edema.
- The **laterally displaced apical pulse and irregularly irregular rhythm** indicate significant cardiac remodeling, not a structurally normal heart.
*Ejection fraction: 65% with rapid early diastolic filling and slow late diastolic filling*
- An EF of 65% indicates **preserved systolic function**, which contradicts the clinical evidence of **systolic heart failure** (laterally displaced apex, severe volume overload).
- While **diastolic dysfunction** can occur in hypertensive heart disease, the described filling pattern doesn't clearly indicate the **impaired relaxation** pattern (reduced E/A ratio) typically seen in hypertensive heart disease.
- The severity of this patient's presentation (bibasilar rales, JVD, peripheral edema) suggests **systolic dysfunction**, not isolated diastolic dysfunction.
*Ejection fraction: 80% with regurgitant aortic valve*
- An EF of 80% is **supranormal/hyperdynamic** and inconsistent with the clinical presentation of **decompensated heart failure**.
- While **chronic aortic regurgitation** can cause LV dilatation and eventual heart failure, it typically presents with a **wide pulse pressure** and **bounding pulses**, and the history strongly points to **hypertensive etiology** rather than primary valvular disease.
- Aortic regurgitation would not explain the **hypertensive retinopathy** or the **20-year history of hypertension** as the primary pathology.
Hypertensive heart disease US Medical PG Question 2: A 70-year-old man presented to a medical clinic for a routine follow-up. He has had hypertension for 20 years and is currently on multiple anti-hypertensive medications. The blood pressure is 150/100 mm Hg. The remainder of the examinations were within normal limits. Echocardiography showed some changes in the left ventricle. What is the most likely reason for the change?
- A. Disordered growth of the cardiac cells
- B. Increase in number of normal cardiac cells
- C. Replacement of cardiac cells into stronger red fiber skeletal cells
- D. Decrease in cardiac cell size
- E. Increase in cardiac cell size (Correct Answer)
Hypertensive heart disease Explanation: ***Increase in cardiac cell size***
- Chronic **hypertension** increases the afterload on the left ventricle, causing the cardiac muscle cells (myocytes) to **hypertrophy** (increase in size) to generate greater force to eject blood.
- This adaptive change is a compensatory mechanism to maintain cardiac output against increased systemic vascular resistance.
*Disordered growth of the cardiac cells*
- This description typically refers to **dysplasia**, which involves abnormal cell growth and organization, often raising suspicion for pre-cancerous conditions.
- Cardiac muscle cells, being terminally differentiated, do not commonly undergo dysplastic changes in response to hypertension.
*Increase in number of normal cardiac cells*
- An increase in the number of cells is known as **hyperplasia**, a process that occurs in tissues with high regenerative capacity.
- Mature **cardiac myocytes** have very limited proliferative capacity, so an increase in their number is not the primary mechanism of ventricular adaptation to hypertension.
*Replacement of cardiac cells into stronger red fiber skeletal cells*
- This scenario describes **metaplasia**, where one differentiated cell type is replaced by another.
- Such a transformation from cardiac muscle to skeletal muscle cells does not occur in response to hypertension and is biologically impossible within the heart.
*Decrease in cardiac cell size*
- A decrease in cell size, or **atrophy**, occurs due to decreased workload, nutrition, or hormonal stimulation.
- In hypertension, the workload on the heart is significantly increased, leading to hypertrophy rather than atrophy.
Hypertensive heart disease US Medical PG Question 3: An 80-year-old African American male presents complaining of worsening shortness of breath that occurs during his weekly round of golf. He also notes he has been waking up at night "choking and gasping for air", though he has been able to gain some relief by propping his head on a stack of pillows before he goes to bed. Upon auscultation, a low frequency, early diastolic gallop is heard over the apex while the patient rests in the left lateral decubitus position. This finding is most consistent with which of the following?
- A. Left ventricular concentric hypertrophy
- B. Right atrial hypertrophy
- C. Mitral stenosis
- D. Left atrial hypertrophy
- E. Left ventricular eccentric hypertrophy (Correct Answer)
Hypertensive heart disease Explanation: ***Left ventricular eccentric hypertrophy***
- The symptoms of **dyspnea on exertion** and **paroxysmal nocturnal dyspnea** (relieved by propping up pillows) are classic for **left-sided heart failure**.
- An **early diastolic gallop** (S3 heart sound) heard best at the apex in the left lateral decubitus position is indicative of **volume overload** and a failing, dilated left ventricle, consistent with eccentric hypertrophy.
*Left ventricular concentric hypertrophy*
- Concentric hypertrophy is typically associated with **pressure overload** (e.g., hypertension, aortic stenosis) and often presents with a **late diastolic gallop (S4)** due to a stiff, non-compliant ventricle.
- While it can lead to heart failure, the presence of an **S3 gallop** points more strongly to a dilated, volume-overloaded ventricle.
*Right atrial hypertrophy*
- Right atrial hypertrophy results from **right ventricular dysfunction** or conditions like **pulmonary hypertension** and would manifest with symptoms of right heart failure (e.g., peripheral edema, jugular venous distention), not primarily left-sided symptoms.
- It is not directly associated with a left ventricular early diastolic gallop.
*Mitral stenosis*
- Mitral stenosis typically causes a **mid-diastolic murmur** with an opening snap, and its symptoms are usually related to elevated left atrial pressure leading to pulmonary congestion and dyspnea.
- An **S3 gallop** is not characteristic of mitral stenosis; it's more specific for left ventricular systolic dysfunction.
*Left atrial hypertrophy*
- Left atrial hypertrophy (enlargement) commonly results from conditions like **mitral valve disease** or **left ventricular diastolic dysfunction** but does not directly cause an S3 gallop.
- While it contributes to symptoms of left heart failure, it's a consequence rather than the primary cause of an S3.
Hypertensive heart disease US Medical PG Question 4: A 67-year-old male with a history of poorly controlled hypertension, COPD, and diabetes presents to his cardiologist for a routine appointment. He reports that he has no current complaints and has not noticed any significant changes in his health. On exam, the cardiologist hears an extra heart sound in late diastole that immediately precedes S1. This heart sound is most associated with which of the following?
- A. Left ventricular hypertrophy (Correct Answer)
- B. Increased filling pressures
- C. Mitral regurgitation
- D. Mitral stenosis
- E. Ventricular dilation
Hypertensive heart disease Explanation: ***Left ventricular hypertrophy***
- An **S4 heart sound** in late diastole, immediately preceding S1, is typically heard with a **stiff, non-compliant left ventricle**, which is characteristic of **left ventricular hypertrophy**.
- The patient's history of **poorly controlled hypertension and diabetes** are significant risk factors for developing left ventricular hypertrophy.
*Increased filling pressures*
- While increased filling pressures can occur in heart failure, an **S4** specifically indicates **diastolic dysfunction due to a hypertrophied ventricle**, not merely high filling pressures.
- An **S3 heart sound** is more commonly associated with increased filling pressures and **ventricular dilation in systolic dysfunction**.
*Mitral regurgitation*
- **Mitral regurgitation** is typically characterized by a **holosystolic murmur**, which is a different auscultatory finding.
- While chronic mitral regurgitation can lead to ventricular hypertrophy, the **S4 sound** itself reflects the underlying **stiffness of the ventricle**, not directly the valvular insufficiency.
*Mitral stenosis*
- **Mitral stenosis** is characterized by an **opening snap** followed by a **mid-diastolic rumble**, which is distinct from an S4 heart sound.
- It involves a narrowed mitral valve orifice, causing impedance to blood flow from the left atrium to the left ventricle.
*Ventricular dilation*
- **Ventricular dilation** is typically associated with an **S3 heart sound**, which occurs in early diastole during rapid ventricular filling.
- An **S4** signifies a **non-compliant, stiff ventricle** (often hypertrophied), rather than a dilated one.
Hypertensive heart disease US Medical PG Question 5: A 42-year-old woman comes to the physician because of a 12 month history of progressive fatigue and shortness of breath with exertion. Five years ago, she emigrated from Eastern Europe. She has smoked one pack of cigarettes daily for 20 years. She has a history of using methamphetamines and cocaine but quit 5 years ago. Vital signs are within normal limits. Physical examination shows jugular venous pulsations 9 cm above the sternal angle. The lungs are clear to auscultation. There is a normal S1 and a loud, split S2. An impulse can be felt with the fingers left of the sternum. The abdomen is soft and nontender. The fingertips are enlarged and the nails are curved. There is pitting edema around the ankles bilaterally. An x-ray of the chest shows pronounced central pulmonary arteries and a prominent right heart border. Which of the following is most likely to confirm the diagnosis?
- A. CT angiography
- B. Serologic testing
- C. Doppler echocardiography
- D. High-resolution CT of the lung
- E. Right-heart catheterization (Correct Answer)
Hypertensive heart disease Explanation: ***Right-heart catheterization***
- This is the **gold standard** for diagnosing **pulmonary hypertension** by directly measuring pulmonary artery pressure, pulmonary wedge pressure, and cardiac output. The patient's symptoms (fatigue, shortness of breath, loud split S2, prominent right heart border, JVP elevation, peripheral edema, digital clubbing) strongly suggest pulmonary hypertension.
- It helps classify the type of pulmonary hypertension and guides treatment strategies, as **mean pulmonary artery pressure (mPAP) > 20 mmHg** at rest is diagnostic.
*CT angiography*
- Primarily used to diagnose **pulmonary embolism** or to evaluate for chronic thromboembolic pulmonary hypertension (CTEPH). While helpful in some cases of pulmonary hypertension, it does not directly measure pressures.
- It would show emboli or chronic organized thrombi if present but doesn't provide the hemodynamic data needed to confirm the severity and type of pulmonary hypertension.
*Serologic testing*
- Used to identify underlying systemic diseases (e.g., **autoimmune conditions like scleroderma**) that can cause pulmonary hypertension. However, it does not directly confirm the diagnosis of pulmonary hypertension itself.
- While it may uncover **etiological factors**, serological markers are not diagnostic for the presence or severity of pulmonary hypertension.
*Doppler echocardiography*
- A crucial initial screening tool that **estimates pulmonary artery pressure** and assesses right ventricular function, often prompting further investigation for pulmonary hypertension.
- While highly suggestive, it is **indirect and an estimation**, and thus not considered definitive for confirming the diagnosis or for precise hemodynamic measurements.
*High-resolution CT of the lung*
- Used to evaluate for **interstitial lung disease** or other parenchymal lung conditions that can cause secondary pulmonary hypertension.
- It provides detailed images of the lung parenchyma but does not directly measure pulmonary pressures or confirm the diagnosis of pulmonary hypertension.
Hypertensive heart disease US Medical PG Question 6: An investigator is studying the physiological response during congestive heart failure exacerbations in patients with systolic heart failure. A hormone released by ventricular cardiomyocytes in response to increased wall stress is isolated from a patient's blood sample. The intracellular mechanism by which this hormone acts is most similar to the effect of which of the following substances?
- A. Aldosterone
- B. Platelet-derived growth factor
- C. Nitric oxide (Correct Answer)
- D. Angiotensin II
- E. Human chorionic gonadotropin
Hypertensive heart disease Explanation: ***Nitric oxide***
- The hormone described is likely **Brain Natriuretic Peptide (BNP)**, released from ventricular cardiomyocytes in response to **increased wall stress** during heart failure. BNP acts by increasing intracellular **cGMP** to cause vasodilation and natriuresis.
- **Nitric oxide (NO)** also works by stimulating **guanylyl cyclase** to increase intracellular cGMP, leading to smooth muscle relaxation and vasodilation, thus mimicking the intracellular mechanism of BNP.
*Aldosterone*
- **Aldosterone** is a steroid hormone that acts on intracellular mineralocorticoid receptors, altering gene expression to promote **sodium reabsorption** and potassium excretion.
- This mechanism is distinct from the **second messenger system** involving cGMP.
*Platelet-derived growth factor*
- **Platelet-derived growth factor (PDGF)** binds to cell surface receptor tyrosine kinases, initiating a signaling cascade that primarily involves **phosphorylation** and leads to cell growth and proliferation.
- This mechanism is different from the direct activation of **guanylyl cyclase** by BNP.
*Angiotensin II*
- **Angiotensin II** primarily acts on G protein-coupled receptors (GPCRs), leading to vasoconstriction, aldosterone release, and other effects, often through **IP3/DAG** or **cAMP** pathways.
- Its intracellular signaling mechanism is not primarily centered on **cGMP**.
*Human chorionic gonadotropin*
- **Human chorionic gonadotropin (hCG)** is a glycoprotein hormone that binds to **G protein-coupled receptors (GPCRs)**, primarily stimulating the production of **cAMP** as a second messenger.
- While it uses a second messenger system, the specific pathway (cAMP) differs from the **cGMP** pathway activated by BNP.
Hypertensive heart disease US Medical PG Question 7: A 75-year-old woman presents to her physician with a cough and shortness of breath. She says that cough gets worse at night and her shortness of breath occurs with moderate exertion or when lying flat. She says these symptoms have been getting worse over the last 6 months. She mentions that she has to use 3 pillows while sleeping in order to relieve her symptoms. She denies any chest pain, chest tightness, or palpitations. Past medical history is significant for hypertension and diabetes mellitus type 2. Her medications are amiloride, glyburide, and metformin. Family history is significant for her father who also suffered diabetes mellitus type 2 before his death at 90 years old. The patient says she drinks alcohol occasionally but denies any smoking history. Her blood pressure is 130/95 mm Hg, temperature is 36.5°C (97.7°F), and heart rate is 100/min. On physical examination, she has a sustained apical impulse, a normal S1 and S2, and a loud S4 without murmurs. There are bilateral crackles present bilaterally. A chest radiograph shows a mildly enlarged cardiac silhouette. A transesophageal echocardiogram is performed and shows a normal left ventricular ejection fraction. Which of the following myocardial changes is most likely present in this patient?
- A. Macrophages with hemosiderin
- B. Asymmetric hypertrophy of the interventricular septum
- C. Ventricular hypertrophy with sarcomeres duplicated in series
- D. Ventricular hypertrophy with sarcomeres duplicated in parallel (Correct Answer)
- E. Granuloma consisting of lymphocytes, plasma cells and macrophages surrounding necrotic tissue
Hypertensive heart disease Explanation: ***Ventricular hypertrophy with sarcomeres duplicated in parallel***
- This patient presents with symptoms and signs consistent with **diastolic heart failure** due to **hypertension**, including exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, S4 gallop, and preserved ejection fraction on echocardiogram.
- **Chronic hypertension** causes increased **afterload**, leading to **concentric left ventricular hypertrophy** where new sarcomeres are added in **parallel**, thickening the ventricular wall, and contributing to impaired relaxation and diastolic dysfunction.
*Macrophages with hemosiderin*
- **Hemosiderin-laden macrophages ("heart failure cells")** are typically found in the **lungs** in cases of chronic **pulmonary congestion** due to **left-sided heart failure**.
- While pulmonary congestion is present, this option describes a finding in the **lungs**, not the specific myocardial change causing the heart failure.
*Asymmetric hypertrophy of the interventricular septum*
- This is a hallmark feature of **hypertrophic cardiomyopathy (HCM)**, an inherited genetic disorder, often causing **dynamic left ventricular outflow tract obstruction**.
- There are no other features suggestive of HCM in this patient; her symptoms are more consistent with **hypertensive heart disease**.
*Ventricular hypertrophy with sarcomeres duplicated in series*
- Duplication of sarcomeres **in series** leads to **eccentric hypertrophy**, which is typically seen in conditions of **volume overload**, such as **dilated cardiomyopathy** or **aortic regurgitation**.
- This patient's presentation with **preserved ejection fraction** and chronic hypertension points towards **pressure overload** and concentric hypertrophy, not eccentric hypertrophy.
*Granuloma consisting of lymphocytes, plasma cells and macrophages surrounding necrotic*
- This description is characteristic of a **granuloma** seen in conditions like **tuberculosis** or **cardiac sarcoidosis**, the latter of which can cause restrictive cardiomyopathy.
- While sarcoidosis can cause heart failure, the patient's long-standing **hypertension** is a much more common and direct cause of her reported symptoms and findings.
Hypertensive heart disease US Medical PG Question 8: A 65-year-old man presents to the physician for the evaluation of increasing dyspnea and swelling of the lower extremities over the past year. He has no cough. He also complains of frequent awakenings at night and excessive daytime sleepiness. He has no history of a serious illness. He takes no medications other than zolpidem before sleep. He is a 35-pack-year smoker. His blood pressure is 155/95 mm Hg. His BMI is 37 kg/m2. Oropharyngeal examination shows a small orifice and an enlarged tongue and uvula. The soft palate is low-lying. The examination of the nasal cavity shows no septal deviation or polyps. Symmetric pitting edema is seen below the knee, bilaterally. The lungs are clear to auscultation. Echocardiography shows a mildly dilated right ventricle and an elevated systolic pulmonary artery pressure with no abnormalities of the left heart. A ventilation-perfusion scan shows no abnormalities. Which of the following is the most likely cause of this patient’s symptoms?
- A. Chronic obstructive pulmonary disease
- B. Pulmonary thromboembolism
- C. Idiopathic pulmonary artery hypertension
- D. Obstructive sleep apnea (Correct Answer)
- E. Heart failure with a preserved ejection fraction
Hypertensive heart disease Explanation: ***Obstructive sleep apnea***
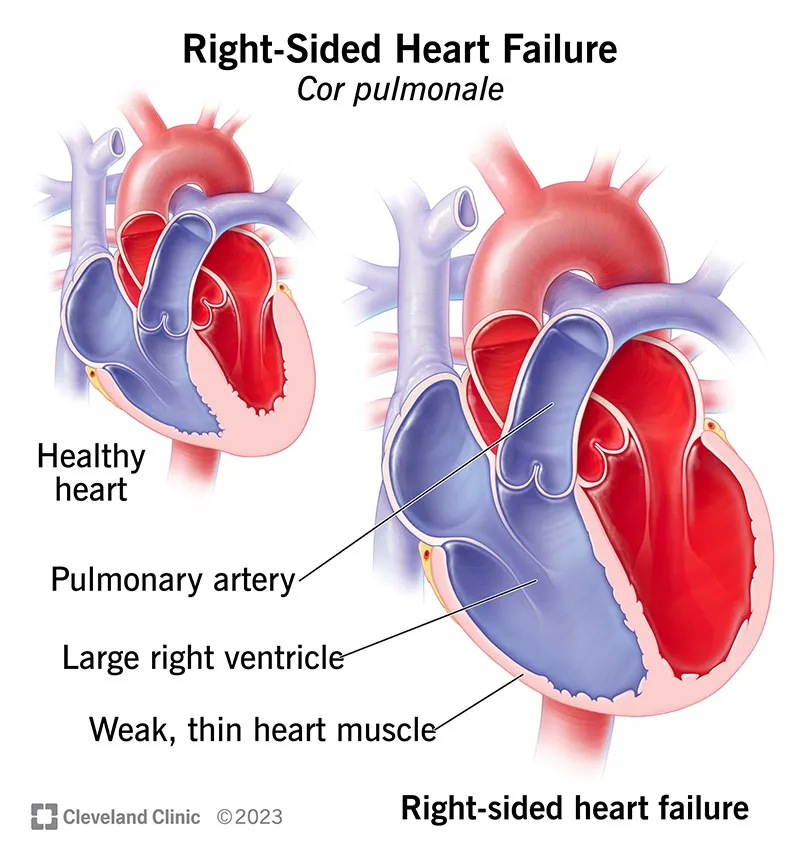
- This patient's symptoms of **dyspnea, lower extremity swelling, frequent nocturnal awakenings, and excessive daytime sleepiness**, in conjunction with **obesity (BMI 37)**, **hypertension**, and specific **oropharyngeal abnormalities** (small orifice, enlarged tongue and uvula, low-lying soft palate), are highly suggestive of **obstructive sleep apnea (OSA)**.
- The echocardiographic findings of a **mildly dilated right ventricle** and **elevated systolic pulmonary artery pressure** (cor pulmonale) without left heart abnormalities are a common consequence of chronic hypoxia and hypercapnia associated with severe OSA.
*Chronic obstructive pulmonary disease*
- While the patient is a 35-pack-year smoker, the absence of a **cough** and **clear lungs to auscultation** make COPD less likely.
- A Ventilation-Perfusion scan showing **no abnormalities** further decreases the likelihood of significant parenchymal lung disease often seen in COPD.
*Pulmonary thromboembolism*
- Although dyspnea is a symptom of pulmonary thromboembolism, the **insidious onset over a year** and the absence of acute symptoms like pleuritic chest pain or hemoptysis make it unlikely.
- A **normal ventilation-perfusion scan** effectively rules out significant pulmonary thromboembolism.
*Idiopathic pulmonary artery hypertension*
- This diagnosis typically presents with **progressive dyspnea** and signs of **right heart failure**, similar to the patient's presentation.
- However, the patient's severe **risk factors for OSA (obesity, oropharyngeal features)** provide a more specific and likely underlying cause for the observed pulmonary hypertension, rather than idiopathic.
*Heart failure with a preserved ejection fraction*
- This condition is characterized by dyspnea and edema with normal or near-normal left ventricular ejection fraction.
- However, the echocardiogram specifically states **no abnormalities of the left heart**, which would typically show some signs of diastolic dysfunction in HFpEF. The primary findings point to right heart strain.
Hypertensive heart disease US Medical PG Question 9: A patient with a history of Tetralogy of Fallot is being evaluated for long-term complications. This patient is at greatest risk of damage to which of the following cardiovascular structures?
- A. Cardiac septum
- B. Coronary artery
- C. Temporal artery
- D. Pulmonary valve (Correct Answer)
- E. Cardiac conduction system
Hypertensive heart disease Explanation: ***Pulmonary valve***
- Patients with **Tetralogy of Fallot** often have severe **pulmonary stenosis**, which can lead to significant long-term damage and insufficiency of the pulmonary valve, frequently requiring replacement.
- The elevated right ventricular pressure from **outflow obstruction** and the **ventricular septal defect** alter flow dynamics, putting continuous strain on the pulmonary valve and the right ventricular outflow tract.
*Cardiac septum*
- While a **ventricular septal defect (VSD)** is a key feature of Tetralogy of Fallot, it is a structural anomaly present from birth and usually does not *suffer additional damage* over time in the same way a valve does, although its size can impact shunt dynamics.
- Damage to the septum itself (beyond the initial defect) is not the primary long-term risk for this cardiovascular structure in Tetralogy of Fallot.
*Coronary artery*
- Anomalies of the **coronary arteries** can occur in Tetralogy of Fallot but are not consistently present and are not the primary structure at greatest risk of *damage* as a direct consequence of the typical hemodynamics of the condition.
- Coronary artery disease is generally a later-life atherosclerotic process and not directly linked to the congenital defect itself.
*Temporal artery*
- The **temporal artery** is an extracardiac artery and is not a cardiovascular structure at risk of damage in Tetralogy of Fallot.
- Conditions like giant cell arteritis affect the temporal artery, which is unrelated to this congenital heart defect.
*Cardiac conduction system*
- While there is a risk of **arrhythmias** in patients with Tetralogy of Fallot, particularly with surgical repairs, the direct *damage* to the cardiac conduction system itself from the pathophysiology is not the greatest risk compared to the structural deterioration of the pulmonary valve.
- Scarring from corrective surgery can predispose to conduction abnormalities, but the primary pathology and greatest unaddressed risk is often related to the right ventricular outflow tract and pulmonary valve.
Hypertensive heart disease US Medical PG Question 10: A 36-year-old healthy man presents to his physician to discuss his concerns about developing heart disease. His father, grandfather, and older brother had heart problems, and he has become increasingly worried he might be at risk. He takes no medications and his past medical history is only significant for an appendectomy at 20 years ago. He is married happily with 2 young children and works as a hotel manager and exercises occasionally in the hotel gym. He drinks 3–5 alcoholic beverages per week but denies smoking and illicit drug use. Today his blood pressure is 146/96 mm Hg, pulse rate is 80/min, and respiratory rate is 16/min. He has a body mass index of 26.8 kg/m2. His physical examination is otherwise unremarkable. Laboratory tests show:
Laboratory test
Serum glucose (fasting) 88 mg/dL
Serum electrolytes
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum creatinine 0.8 mg/dl
Blood urea nitrogen 10 mg/dl
Cholesterol, total 350 mg/dL
HDL-cholesterol 40 mg/dL
LDL-cholesterol 280 mg/dL
Triglycerides 130 mg/dL
Besides appropriate medications for his cholesterol and a follow-up for his hypertension, which of the following supplements is thought to provide a protective cardiovascular effect?
- A. Folic acid (Correct Answer)
- B. Thiamine
- C. Vitamin K
- D. Vitamin B12
- E. Vitamin E
Hypertensive heart disease Explanation: ***Folic acid***
- Folic acid (Vitamin B9) is involved in the metabolism of **homocysteine**, and elevated homocysteine levels are associated with increased cardiovascular risk.
- **Historically**, it was hypothesized that lowering homocysteine with folic acid would reduce cardiovascular events.
- However, **large randomized controlled trials (HOPE-2, NORVIT, VISP) have failed to demonstrate cardiovascular benefit** from folic acid supplementation despite successfully lowering homocysteine levels.
- Among the options listed, folic acid was the supplement most **historically thought** to provide cardiovascular protection, though current evidence does not support routine supplementation for this purpose.
- **Current guidelines do NOT recommend** folic acid supplementation for cardiovascular disease prevention in the general population.
*Thiamine*
- **Thiamine** (Vitamin B1) is crucial for carbohydrate metabolism and nerve function.
- Thiamine deficiency can lead to **beriberi** (including wet beriberi with cardiac manifestations), but supplementation in individuals without deficiency provides **no cardiovascular protection**.
*Vitamin K*
- **Vitamin K** is essential for blood clotting and bone metabolism, and may play a role in preventing vascular calcification.
- However, there is **insufficient evidence** to recommend vitamin K supplementation for cardiovascular protection in clinical practice.
*Vitamin B12*
- **Vitamin B12** is important for nerve function, red blood cell formation, and homocysteine metabolism.
- Like folic acid, B12 was studied for cardiovascular protection through homocysteine reduction, but **clinical trials failed to show benefit**.
- Routine B12 supplementation for cardiovascular protection in individuals with normal B12 levels is **not recommended**.
*Vitamin E*
- **Vitamin E** is an antioxidant that was extensively studied for cardiovascular protection in the 1990s-2000s.
- **Large clinical trials (HOPE, GISSI) conclusively showed NO cardiovascular benefit** from vitamin E supplementation, and some studies suggested potential harm at high doses.
- Vitamin E supplementation for cardiovascular disease prevention is **not recommended**.
More Hypertensive heart disease US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.