Congenital heart defects US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Congenital heart defects. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Congenital heart defects US Medical PG Question 1: A 2-year-old boy is presented to the pediatrician due to poor weight gain and easy fatigability. His mother states that the patient barely engages in any physical activity as he becomes short of breath easily. The prenatal and birth histories are insignificant. Past medical history includes a few episodes of upper respiratory tract infection that were treated successfully. The patient is in the 10th percentile for weight and 40th percentile for height. The vital signs include: heart rate 122/min and respirations 32/min. Cardiac auscultation reveals clear lungs and a grade 2/6 holosystolic murmur loudest at the left lower sternal border. The remainder of the physical examination is negative for clubbing, cyanosis, and peripheral edema. Which of the following is the most likely diagnosis in this patient?
- A. Tetralogy of Fallot (TOF)
- B. Atrial septal defect (ASD)
- C. Coarctation of aorta
- D. Ventricular septal defect (VSD) (Correct Answer)
- E. Patent ductus arteriosus (PDA)
Congenital heart defects Explanation: ***Ventricular septal defect (VSD)***
- A **holosystolic murmur** loudest at the **left lower sternal border**, poor weight gain, and easy fatigability in a 2-year-old are classic signs of a **VSD**.
- The symptoms arise from significant **left-to-right shunting**, leading to pulmonary overcirculation and heart failure symptoms.
*Tetralogy of Fallot (TOF)*
- TOF typically presents with **cyanosis** and **TET spells**, which are absent in this patient.
- The murmur in TOF is usually an **ejection systolic murmur**, not holosystolic, and often associated with a single loud S2.
*Atrial septal defect (ASD)*
- An ASD typically presents with a **fixed, split S2** and an **ejection systolic murmur** at the upper left sternal border due to increased flow across the pulmonic valve.
- Symptoms like poor weight gain and easy fatigability are less common in early childhood unless the shunt is very large.
*Coarctation of aorta*
- This condition is characterized by **femoral-radial delay** and **differential blood pressures** between the upper and lower extremities.
- The murmur is typically heard in the **back** or subclavicular region, and symptoms usually include poor feeding, lethargy, and sometimes heart failure.
*Patent ductus arteriosus (PDA)*
- PDA is classically associated with a **continuous "machinery-like" murmur** loudest below the left clavicle.
- While it can cause poor weight gain and fatigability, the type of murmur described is not consistent with a PDA.
Congenital heart defects US Medical PG Question 2: A 38-year-old woman, gravida 2, para 1, at 24 weeks' gestation comes to the physician for a routine prenatal evaluation. She has no history of major medical illness and takes no medications. Fetal ultrasonography shows a cardiac defect resulting from abnormal development of the endocardial cushions. This defect is most likely to result in which of the following?
- A. Transposition of the great vessels
- B. Atrioventricular septal defect (Correct Answer)
- C. Dextrocardia
- D. Patent foramen ovale
- E. Sinus venosus defect
Congenital heart defects Explanation: ***Atrioventricular septal defect***
- **Endocardial cushion defects** are a hallmark of atrioventricular septal defects, leading to a common atrioventricular valve and an interatrial and/or interventricular communication.
- This defect commonly presents in individuals with **Down syndrome (Trisomy 21)**, though it can occur in isolation.
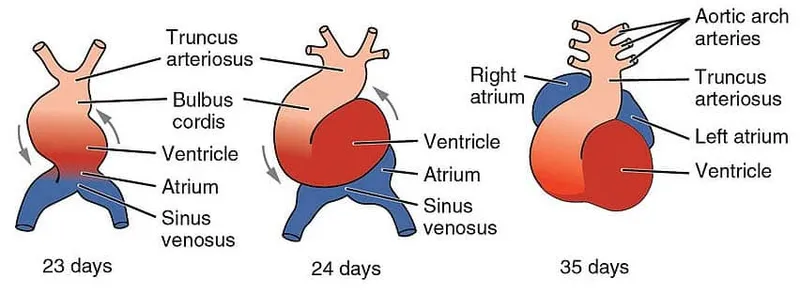
*Transposition of the great vessels*
- This defect results from abnormal **spiraling of the conotruncal septum**, not from endocardial cushion malformation.
- It leads to the **aorta arising from the right ventricle** and the **pulmonary artery from the left ventricle**, a circulation incompatible with life without a shunt.
*Dextrocardia*
- **Dextrocardia** is a condition where the heart is located on the right side of the chest, usually due to abnormal embryonic folding, and is not directly caused by endocardial cushion defects.
- It can occur as an isolated finding or as part of a more complex syndrome like **Kartagener syndrome**.
*Patent foramen ovale*
- A **patent foramen ovale** is a common remnant of fetal circulation, occurring when the foramen ovale fails to close after birth.
- It is a defect of the **atrial septum secondary to incomplete fusion between the septum primum and septum secundum**, not an endocardial cushion defect.
*Sinus venosus defect*
- A **sinus venosus defect** is a type of atrial septal defect occurring near the entrance of the superior or inferior vena cava.
- It is caused by **abnormal development of the sinus venosus** and is not directly related to endocardial cushion malformation.
Congenital heart defects US Medical PG Question 3: A 9-year-old boy is brought to the office due to exertional dyspnea and fatigability. He tires easily when walking or playing. His parents say that he was diagnosed with a congenital heart disease during his infancy, but they refused any treatment. They do not remember much about his diagnosis. The patient also had occasional respiratory infections throughout childhood that did not require hospitalization. He takes no medications. The patient has no family history of heart disease. His vital signs iclude: heart rate 98/min, respiratory rate 16/min, temperature 37.2°C (98.9°F), and blood pressure of 110/80 mm Hg. Physical examination shows toe cyanosis and clubbing but no finger abnormalities. Cardiac auscultation reveals a continuous machine-like murmur. All extremity pulses are full and equal. Which of the following is the most likely diagnosis?
- A. Tetralogy of Fallot
- B. Coarctation of the aorta
- C. Ventricular septal defect
- D. Atrial septal defect
- E. Patent ductus arteriosus (Correct Answer)
Congenital heart defects Explanation: ***Patent ductus arteriosus***
- A **patent ductus arteriosus (PDA)** can cause differential cyanosis and clubbing (lower extremities more affected than upper) due to preferential flow of deoxygenated blood through the PDA to the descending aorta.
- The classic **continuous machine-like murmur** auscultated in the precordium is highly characteristic of a PDA.
*Tetralogy of Fallot*
- Patients typically present with **cyanosis and clubbing of all four extremities** due to right-to-left shunting at the ventricular level, not isolated toe cyanosis.
- While it can cause exertional dyspnea, the murmur is typically a **systolic ejection murmur** from pulmonary stenosis, not a continuous machine-like murmur.
*Coarctation of the aorta*
- This condition presents with **differential blood pressures and pulses** between the upper and lower extremities, with elevated upper extremity pressures.
- It does not typically cause cyanosis or a continuous machine-like murmur.
*Ventricular septal defect*
- A **ventricular septal defect (VSD)** typically causes a **holosystolic murmur** loudest at the lower left sternal border.
- Cyanosis develops late due to Eisenmenger syndrome, and if it occurs, it's typically central, affecting all extremities.
*Atrial septal defect*
- An **atrial septal defect (ASD)** usually presents with a **fixed split S2** and a **systolic ejection murmur** at the upper left sternal border due to increased flow across the pulmonic valve.
- Significant cyanosis is rare and occurs only in advanced stages with Eisenmenger syndrome, affecting all extremities if present.
Congenital heart defects US Medical PG Question 4: A 4-year-old Caucasian male suffers from cyanosis and dyspnea relieved by squatting. Which of the following abnormalities is most likely present?
- A. Atrial septal defect
- B. Coarctation of the aorta
- C. Bicuspid aortic valve
- D. Ventricular septal defect
- E. Tetralogy of Fallot (Correct Answer)
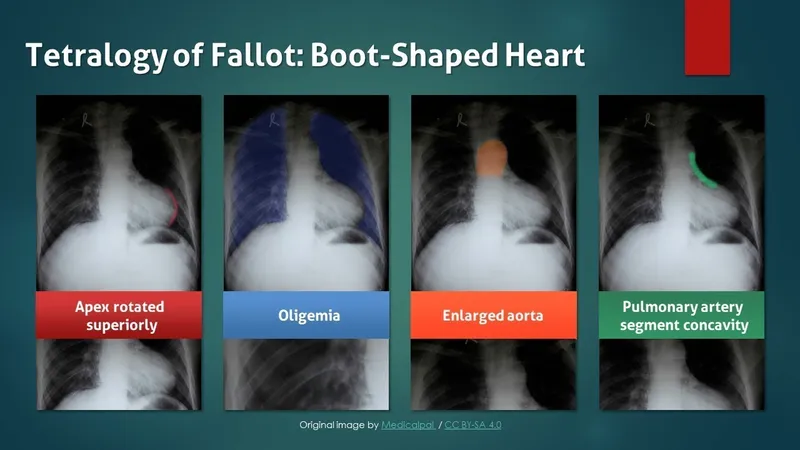
Congenital heart defects Explanation: ***Tetralogy of Fallot***
- **Cyanosis** and **dyspnea relieved by squatting** are the hallmark clinical features of **Tetralogy of Fallot**, making this the correct diagnosis.
- The condition consists of four anatomic abnormalities: **ventricular septal defect (VSD)**, **right ventricular outflow tract obstruction**, **right ventricular hypertrophy**, and **overriding aorta**.
- The right-to-left shunt across the VSD causes **deoxygenated blood** to enter systemic circulation, producing **cyanosis**.
- **Squatting increases systemic vascular resistance (SVR)**, which decreases the right-to-left shunt, improves pulmonary blood flow, and relieves cyanosis and dyspnea during **"tet spells"**.
*Atrial septal defect*
- ASDs typically cause **left-to-right shunts** and are **acyanotic lesions**.
- Patients may be asymptomatic or present with **exertional dyspnea** and **fatigue** in later childhood or adulthood.
- Cyanosis would only occur if **Eisenmenger syndrome** develops (reversal to right-to-left shunt due to pulmonary hypertension), which is rare at age 4 and does not improve with squatting.
*Coarctation of the aorta*
- This is an **acyanotic** lesion characterized by **narrowing of the descending aorta**.
- Classic findings include **upper extremity hypertension**, **diminished or delayed femoral pulses**, and **lower extremity hypotension**.
- Does not cause cyanosis or squatting relief.
*Bicuspid aortic valve*
- A common **acyanotic** congenital abnormality that may lead to **aortic stenosis** or **regurgitation** over time.
- Usually asymptomatic in childhood; may present with **murmur**, chest pain, or syncope in adulthood.
- Does not cause cyanosis or relief with squatting.
*Ventricular septal defect*
- Isolated VSDs typically cause **left-to-right shunts** and are **acyanotic**.
- May present with **heart failure symptoms** (tachypnea, poor feeding, failure to thrive) in infancy if the defect is large.
- Cyanosis occurs only if **Eisenmenger syndrome** develops (usually takes years to decades), and symptoms are not relieved by squatting.
Congenital heart defects US Medical PG Question 5: A 3-year-old boy is brought to the physician because of recurrent nosebleeds and fatigue for the past 2 months. He also frequently complains his head hurts. The patient has met all motoric milestones for his age but does not like to run because his legs start to hurt if he does. He is at the 40th percentile for both height and weight. His temperature is 37.0°C (98.6°F), pulse is 125/min, respirations are 32/min, and blood pressure in the right arm is 130/85 mm Hg. A grade 2/6 systolic murmur is heard in the left paravertebral region. Further evaluation of this patient is most likely to show which of the following findings?
- A. Inferior rib notching
- B. Delayed pulse in lower extremities (Correct Answer)
- C. Interarm difference in tissue oxygenation
- D. Pulmonary valve stenosis
- E. Left-axis deviation on ECG
Congenital heart defects Explanation: ***Delayed pulse in lower extremities***
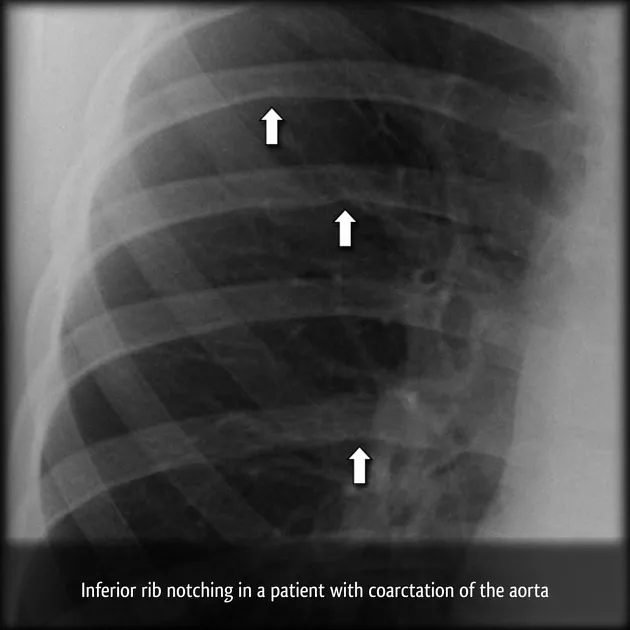
- The patient's symptoms, including **recurrent nosebleeds**, **headaches**, **leg pain with activity**, **hypertension** (especially in the right arm), and a **systolic murmur in the left paravertebral region**, are highly suggestive of **coarctation of the aorta**.
- A key physical finding in coarctation of the aorta is a **delayed and diminished femoral pulse** compared to the radial pulse due to obstruction of blood flow to the lower body.
*Inferior rib notching*
- This finding is characteristic of **collateral circulation** developing around a coarctation in older children and adults, as the **intercostal arteries** become enlarged to supply blood to the lower body.
- While associated with coarctation, it is typically seen on **chest X-rays** in older patients and is less likely to be present or pronounced in a 3-year-old.
*Interarm difference in tissue oxygenation*
- While coarctation can cause an **interarm blood pressure difference**, it typically does not directly cause a significant interarm difference in **tissue oxygenation** unless severe unilateral subclavian artery involvement is present, which is not the primary mechanism.
- The primary oxygenation concern in coarctation is usually related to overall cardiac output or systemic effects rather than a localized interarm difference.
*Pulmonary valve stenosis*
- **Pulmonary valve stenosis** would typically present with a **systolic ejection murmur** heard best at the left upper sternal border, often radiating to the back.
- It does not explain the specific constellation of symptoms such as **hypertension in the upper extremities**, **leg pain with activity**, or differential pulses characteristic of coarctation of the aorta.
*Left-axis deviation on ECG*
- **Left-axis deviation** on an ECG is often associated with conditions causing **left ventricular hypertrophy** or conduction defects.
- While severe coarctation can lead to left ventricular hypertrophy, left-axis deviation is not a specific or direct diagnostic finding for coarctation and is less characteristic than the described physical exam findings.
Congenital heart defects US Medical PG Question 6: A 1-year-old infant is brought to the emergency department by his parents because of fever and rapid breathing for the past 2 days. He had a mild seizure on the way to the emergency department and developed altered sensorium. His mother states that the patient has had recurrent respiratory infections since birth. He was delivered vaginally at term and without complications. He is up to date on his vaccines and has met all developmental milestones. His temperature is 37.0°C (98.6°F), pulse rate is 200/min, and respirations are 50/min. He is lethargic, irritable, and crying excessively. Physical examination is notable for a small head, an elongated face, broad nose, low set ears, and cleft palate. Cardiopulmonary exam is remarkable for a parasternal thrill, grade IV pansystolic murmur, and crackles over both lung bases. Laboratory studies show hypocalcemia and lymphopenia. Blood cultures are drawn and broad-spectrum antibiotics are started, and the child is admitted to the pediatric intensive care unit. The intensivist suspects a genetic abnormality and a fluorescence in situ hybridization (FISH) analysis is ordered which shows 22q11.2 deletion. Despite maximal therapy, the infant succumbs to his illness. The parents of the child request an autopsy. Which of the following findings is the most likely to be present on autopsy?
- A. Aplastic thymus (Correct Answer)
- B. Hypercellular bone marrow
- C. Accessory spleen
- D. Hypertrophy of Hassall's corpuscles
- E. Absent follicles in the lymph nodes
Congenital heart defects Explanation: ***Aplastic thymus***
- This infant's presentation with 22q11.2 deletion, recurrent respiratory infections, hypocalcemia, and congenital heart disease (parasternal thrill, pansystolic murmur) is classic for **DiGeorge syndrome**.
- **DiGeorge syndrome** is characterized by thymic aplasia or hypoplasia, leading to **T-cell immunodeficiency**, and parathyroid hypoplasia, resulting in **hypocalcemia**.
*Hypercellular bone marrow*
- **Hypercellular bone marrow** indicates increased hematopoietic activity and is not a characteristic finding in DiGeorge syndrome.
- In immunodeficiency states like DiGeorge, the bone marrow itself is often normal or may show lymphoid depletion.
*Accessory spleen*
- **Accessory spleen** is a common congenital anomaly and is not specifically associated with DiGeorge syndrome or its immunodeficiency.
- While it can occur in individuals with DiGeorge syndrome, it is not a direct pathological consequence of the 22q11.2 deletion.
*Hypertrophy of Hassall's corpuscles*
- **Hassall's corpuscles** are found in the medulla of the thymus, and their hypertrophy would indicate an active or hyperplastic thymus, which is contrary to the **thymic aplasia/hypoplasia** seen in DiGeorge syndrome.
- In DiGeorge syndrome, the thymus is either absent or severely underdeveloped.
*Absent follicles in the lymph nodes*
- **Absent follicles in the lymph nodes** would indicate a B-cell deficiency, as follicles are primarily composed of B lymphocytes.
- DiGeorge syndrome primarily affects **T-cell development** due to thymic abnormalities, not B-cell development or lymph node follicular formation directly.
Congenital heart defects US Medical PG Question 7: A 25-year-old woman, gravida 2, para 1, comes to the physician for her initial prenatal visit at 18 weeks’ gestation. She is a recent immigrant from Thailand. Her history is significant for anemia since childhood that has not required any treatment. Her mother and husband have anemia, as well. She has no history of serious illness and takes no medications. Her vital signs are within normal limits. Fundal height measures at 22 weeks. Ultrasound shows polyhydramnios and pleural and peritoneal effusion in the fetus with fetal subcutaneous edema. Which of the following is the most likely clinical course for this fetus?
- A. Neonatal death
- B. Normal development with regular blood transfusion
- C. Asymptomatic anemia
- D. Intrauterine fetal demise (Correct Answer)
- E. Carrier state
Congenital heart defects Explanation: ***Intrauterine fetal demise***
- The ultrasound findings of **polyhydramnios**, **pleural and peritoneal effusion**, and **fetal subcutaneous edema** are classic signs of **hydrops fetalis**.
- In a patient from Thailand with a history of lifelong anemia and a family history of anemia, these findings are highly suggestive of **alpha-thalassemia major (Hb Barts disease)**, which is almost always lethal in utero or shortly after birth.
*Neonatal death*
- While many cases of **hydrops fetalis** due to **alpha-thalassemia major** result in neonatal death, the severe findings often lead to **intrauterine fetal demise** before viability or at term.
- The combination of severe fetal compromise (multiple effusions, edema) and polyhydramnios often indicates a very poor prognosis and high likelihood of demise prior to full term delivery.
*Normal development with regular blood transfusion*
- This is typical for less severe forms of **thalassemia**, such as **beta-thalassemia major**, but not for **alpha-thalassemia major (Hb Barts disease)**, which is characterized by the complete absence of alpha-globin chains.
- **Hb Barts disease** is incompatible with life due to severe tissue hypoxia, as this hemoglobin has an extremely high affinity for oxygen and cannot release it to tissues effectively.
*Asymptomatic anemia*
- **Asymptomatic anemia** is generally associated with milder forms of anemia, such as alpha-thalassemia trait (two gene deletion) or beta-thalassemia minor.
- The severe manifestations of **hydrops fetalis** clearly indicate a profound, life-threatening condition for the fetus, not asymptomatic anemia.
*Carrier state*
- A **carrier state** (e.g., alpha-thalassemia trait) would typically involve mild or no anemia and would not cause **hydrops fetalis** in the fetus.
- The significant fetal pathology rules out a simple carrier state for the fetus; this fetus is severely affected by a major genetic disorder.
Congenital heart defects US Medical PG Question 8: A 74-year-old man presents with complaints of sudden severe crushing retrosternal pain. The pain radiated to his left arm shortly after it began, and he was subsequently rushed to the emergency department for evaluation. His troponins and creatine kinase-MB (CK-MB) were elevated. Unfortunately, the patient died within the next 2 hours and an autopsy was performed immediately. The gross examination of the heart will show?
- A. White, patchy, non-contractile scar
- B. Normal heart tissue (Correct Answer)
- C. Pallor of the infarcted tissue
- D. Abundant neutrophils
- E. Red granulation tissue surrounding the infarction
Congenital heart defects Explanation: ***Normal heart tissue***
- At **0-4 hours** following a myocardial infarction, the heart muscle shows **no gross changes** on autopsy examination.
- Although **coagulative necrosis** begins at the cellular level within minutes, these microscopic changes are **not visible** to the naked eye during gross examination.
- The patient died within **2 hours** of symptom onset, which falls within this early window where the heart appears **grossly normal** despite the acute infarction.
- Elevated **cardiac enzymes** (troponins, CK-MB) confirm myocardial injury has occurred, but gross pathological changes lag behind biochemical and microscopic changes.
*Pallor of the infarcted tissue*
- **Pallor** (pale discoloration) of infarcted myocardium typically becomes visible on gross examination at **4-12 hours** post-infarction.
- At 2 hours, this change has not yet developed sufficiently to be visible on gross inspection.
- Pallor results from **edema** and the accumulation of dead cells, which takes several hours to manifest grossly.
*White, patchy, non-contractile scar*
- A **white fibrotic scar** is characteristic of a **healed myocardial infarction**, which takes **several weeks to months** to form.
- This represents complete replacement of necrotic tissue by **collagenous scar tissue** (fibrosis).
- This is a chronic finding, not an acute one.
*Abundant neutrophils*
- **Neutrophil infiltration** is a microscopic finding that typically begins around **12-24 hours** after infarction, becoming abundant over the following days.
- Even when present, neutrophils are not visible on **gross examination**—they require microscopic evaluation.
- At 2 hours post-infarction, neutrophils have not yet migrated to the infarcted area.
*Red granulation tissue surrounding the infarction*
- **Granulation tissue** formation begins around **3-7 days** after infarction and involves proliferation of **capillaries** and **fibroblasts**.
- Grossly, this appears as a **hyperemic border** with central yellow softening.
- This represents the healing phase and would not be present within 2 hours of symptom onset.
Congenital heart defects US Medical PG Question 9: A 20-year-old man comes to the emergency room because of palpitations and mild dyspnea for the last 2 hours. He has had similar episodes in the past that resolved within 20 minutes, but they have been worsening since he started training for his first marathon 1 month ago. Ten years ago, he was treated for streptococcal pharyngitis with a 10-day course of penicillin. His maternal uncle passed away unexpectedly from a heart condition at age 40. He is 180 cm (5 ft 11 in) tall and weighs 85 kg (187 lb); BMI is 26.2 kg/m2. His temperature is 36.5°C (97.7°F), pulse is 70/min, respirations are 18/min, and blood pressure is 132/60 mm Hg. On examination, there is a decrescendo early diastolic murmur heard best along the left sternal border. His head slightly bobs about every second. The remainder of the examination shows no abnormalities. Which of the following is most likely to be present?
- A. Bicuspid aortic valve (Correct Answer)
- B. Antistreptolysin O antibodies
- C. Asymmetric septal hypertrophy
- D. Valve vegetation
- E. Myxomatous degeneration
Congenital heart defects Explanation: ***Bicuspid aortic valve***
- The patient presents with classic signs of **aortic regurgitation**, including a **decrescendo early diastolic murmur** and **De Musset's sign** (head bobbing). In a young individual, a **bicuspid aortic valve** is the most common congenital cause of aortic valve disease, often leading to regurgitation or stenosis over time.
- The patient's history of palpitations and dyspnea, worsening with exertion, suggests significant hemodynamic compromise related to chronic aortic insufficiency, which can develop secondary to a bicuspid valve.
*Antistreptolysin O antibodies*
- While the patient had a history of **streptococcal pharyngitis** 10 years ago, there are no other signs of **acute rheumatic fever** or **rheumatic heart disease**, such as migratory polyarthritis, chorea, or erythema marginatum.
- The murmur described is typical of aortic regurgitation without specific features pointing to rheumatic involvement, which typically affects the **mitral valve** first.
*Asymmetric septal hypertrophy*
- **Asymmetric septal hypertrophy** is characteristic of **hypertrophic cardiomyopathy**, which would typically present with a **systolic murmur** that increases with Valsalva maneuver, not an early diastolic murmur.
- While sudden cardiac death in a young relative might suggest hypertrophic cardiomyopathy, the physical exam findings here are inconsistent with that diagnosis.
*Valve vegetation*
- **Valve vegetations** are associated with **infective endocarditis** and would typically present with fever, new or worsening murmur, and signs of systemic infection, none of which are noted in this patient.
- The patient's symptoms are chronic and episodic, not acute, subacute, or associated with infectious signs.
*Myxomatous degeneration*
- **Myxomatous degeneration** primarily affects the **mitral valve**, leading to **mitral valve prolapse** and subsequent regurgitation, which would produce a **mid-systolic click** followed by a late systolic murmur.
- This condition is not typically associated with an early diastolic murmur characteristic of aortic regurgitation.
Congenital heart defects US Medical PG Question 10: A 14-year-old Caucasian female with a family history of familial hypercholesterolemia commits suicide by drug overdose. Her family decides to donate her organs, and her heart is removed for donation. After removing the heart, the cardiothoracic surgeon notices flat yellow spots on the inside of her aorta. Which of the following cell types predominate in these yellow spots?
- A. Fibroblasts
- B. T-cells
- C. Macrophages (Correct Answer)
- D. Neutrophils
- E. Endothelium
Congenital heart defects Explanation: ***Correct: Macrophages***
- The "flat yellow spots" on the aorta in a familial hypercholesterolemia patient are characteristic of **fatty streaks**, the earliest lesions of atherosclerosis.
- These fatty streaks are primarily composed of **lipid-laden macrophages**, also known as **foam cells**, which have ingested oxidized low-density lipoprotein (LDL).
- In familial hypercholesterolemia, elevated LDL levels accelerate the formation of these macrophage-rich lesions even in young patients.
*Incorrect: Fibroblasts*
- While fibroblasts are involved in the later stages of **atherosclerotic plaque formation** by synthesizing collagen and forming a fibrous cap, they are not the predominant cell type in early fatty streaks.
- Their presence signifies a more advanced, **fibrotic lesion**, not the initial yellow spots.
*Incorrect: T-cells*
- T-cells are involved in the inflammatory response in **atherosclerosis** and are found within plaques, but they are not the dominant cell type forming the bulk of the initial lipid accumulation in fatty streaks.
- They contribute to the **immune-mediated aspects** of plaque progression.
*Incorrect: Neutrophils*
- Neutrophils are primarily involved in **acute inflammation** and bacterial infections.
- They are generally not a prominent cell type in either early or advanced **atherosclerotic lesions** under normal circumstances.
*Incorrect: Endothelium*
- Endothelial cells line the lumen of blood vessels and are crucial in the **initiation of atherosclerosis** by becoming dysfunctional and allowing LDL entry.
- However, they do not constitute the "yellow spots" themselves, which are subendothelial accumulations of lipids and immune cells.
More Congenital heart defects US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.